Prevalence of Vertebral Fractures in CTPA’s in Adults Aged 75 and Older and Their Association with Subsequent Fractures and Mortality
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Data and Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Peck, W.A.; Burckhardt, P.; Christiansen, C.; Fleisch, H.A.; Genant, H.K.; Gennari, C.; Martin, T.J.; Martini, L.; Morita, R.; Ogata, E.; et al. Diagnosis, prophylaxis and treatment of osteoporosis. In Proceedings of the Fourth International Symposium on Osteoporosis and Consensus Development Conference, Hong Kong, China, 1–2 April 1993. [Google Scholar]
- National Institute for Health and Care Excellence (NICE) Impact. Report on Falls and Fragility Fractures. Available online: https://www.nice.org.uk/Media/Default/About/what-we-do/Into-practice/measuring-uptake/NICE-Impact-falls-and-fragility-fractures.pdf (accessed on 3 July 2019).
- Crandall, C.J.; Newberry, S.J.; Diamant, A.; Lim, Y.W.; Gellad, W.F.; Booth, M.J.; Motala, A.; Shekelle, P.G. Comparative effectiveness of pharmacologic treatments to prevent fractures: An updated systematic review. Ann. Intern. Med. 2014, 161, 711–723. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health and Care Excellent (NICE). Osteoporosis: Assessing the Risk of Fragility Fracture. Guidance and Guidelines. Available online: https://www.nice.org.uk/guidance/cg146 (accessed on 3 July 2019).
- Turner, D.A.; Khioe, R.F.S.; Shepstone, L.; Lenaghan, E.; Cooper, C.; Gittoes, N.; Harvey, N.C.; Holland, R.; Howe, A.; McCloskey, E.; et al. The Cost-Effectiveness of Screening in the Community to Reduce Osteoporotic Fractures in Older Women in the UK: Economic Evaluation of the SCOOP Study. J. Bone Miner. Res. 2018, 33, 845–851. [Google Scholar] [CrossRef] [PubMed]
- Ballane, G.; Cauley, J.A.; Luckey, M.M.; El-Hajj Fuleihan, G. Worldwide prevalence and incidence of osteoporotic vertebral fractures. Osteoporos Int. 2017, 28, 1531–1542. [Google Scholar] [CrossRef] [PubMed]
- Fink, H.A.; Milavetz, D.L.; Palermo, L.; Nevitt, M.C.; Cauley, J.A.; Genant, H.K.; Black, D.M.; Ensrud, L.E. What proportion of incident radiographic vertebral deformities is clinically diagnosed and vice versa? J. Bone Miner Res. 2005, 20, 1216–1222. [Google Scholar] [CrossRef]
- Bartalena, T.; Rinaldi, M.F.; Modolon, C.; Braccaioli, L.; Sverzellati, N.; Rossi, G.; Rimondi, E.; Busacca, M.; Albisinni, U.; Resnick, D. Incidental vertebral compression fractures in imaging studies: Lessons not learned by radiologists. World J. Radiol. 2010, 2, 399–404. [Google Scholar] [CrossRef]
- Jackson, S.A.; Tenenhouse, A.; Robertson, L. Vertebral fracture definition from population-based data: Preliminary results from the Canadian Multicenter Osteoporosis Study (CaMos). Osteoporos Int. 2000, 11, 680–687. [Google Scholar] [CrossRef]
- Grigoryan, M.; Guermazi, A.; Roemer, F.W.; Delmas, P.D.; Genant, H.K. Recognizing and reporting osteoporotic vertebral fractures. Eur. Spine J. 2003, 12, 104–112. [Google Scholar] [CrossRef]
- Genant, H.K.; Wu, C.Y.; Kuijk, C.V.; Nevitt, M.C. Vertebral fracture assessment using a semiquantitative technique. J. Bone Miner. Res. 1993, 8, 1137–1148. [Google Scholar] [CrossRef]
- Johnell, O.; Kanis, J.A.; Odén, A.; Sernbo, I.; Redlund-Johnell, I.; Patterson, C.; De Laet, C.; Jonsson, B. Fracture risk following an osteoporotic fracture. Osteoporos Int. 2004, 15, 175–179. [Google Scholar] [CrossRef]
- Ismail, A.A.; Neill, T.; Cooper, C.; Finn, J.D.; Bhalla, A.K.; Cannata, J.B.; Delmas, P.; Falch, J.A.; Felsch, B.; Hoszowski, K.; et al. Mortality Associated with Vertebral Deformity in Men and Women: Results from the European Prospective Osteoporosis Study (EPOS). Osteoporos Int. 1998, 8, 291–297. [Google Scholar] [CrossRef]
- Ensrud, K.E.; Thompson, D.E.; Cauley, J.A.; Nevitt, M.C.; Kado, D.M.; Hochberg, M.C.; Santora, A.C.; Black, D.M. Prevalent vertebral deformities predict mortality and hospitalization in older women with low bone mass. J. Am. Geriatr. Soc. 2015, 48, 241–249. [Google Scholar] [CrossRef] [PubMed]
- Grados, F.; Marcelli, C.; Dargent-Molina, P.; Roux, C.; Vergnol, J.F.; Meunier, P.J.; Fardellone, P. Prevalence of vertebral fractures in French women older than 75 years from the EPIDOS study. Bone 2004, 34, 362–367. [Google Scholar] [CrossRef] [PubMed]
- Woo, E.K.; Mansoubi, H.; Alyas, F. Incidental vertebral fractures on multidetector CT images of the chest: Prevalence and recognition. Clin. Radiol. 2008, 63, 160–164. [Google Scholar] [CrossRef] [PubMed]
- Carberry, G.A.; Pooler, B.D.; Binkley, N.; Lauder, T.B.; Bruce, R.J.; Pickhardt, P.J. Unreported Vertebral Body Compression Fractures at Abdominal Multidetector CT. Radiology 2013, 268, 120–126. [Google Scholar] [CrossRef]
- Bartalena, T.; Giannelli, G.; Rinaldi, M.F.; Rimondi, G.; Rinaldi, G.; Sverzellati, N.; Gavelli, G. Prevalence of thoracolumbar vertebral fractures on multidetector CT. Underreporting by radiologists. Eur. J. Radiol. 2009, 69, 555–559. [Google Scholar] [CrossRef]
- Williams, A.L.; Al-Busaidi, A.; Sparrow, P.J.; Adams, J.E.; Whitehouse, R.W. Under-reporting of osteoporotic vertebral fractures on computed tomography. Eur. J. Radiol. 2009, 69, 179–183. [Google Scholar] [CrossRef]
- Li, Y.; Yan, L.; Cai, S.; Wang, P.; Zhuang, H.; Yu, H. The prevalence and under-diagnosis of vertebral fractures on chest radiograph. BMC Musculoskelet Disord 2018, 19, 235. [Google Scholar] [CrossRef]
- Delmas, P.D.; Van Langerijt, L.D.; Watts, N.B.; Eastell, R.; Genant, H.; Grauer, A.; Cahall, D.L. Underdiagnosis of vertebral fractures is a worldwide problem: The IMPACT study. J. Bone Miner. Res. 2005, 20, 557–563. [Google Scholar] [CrossRef]
- Singh, I.; Anwar, A.; Rasuly, A.; Edwards, C.; Farooq, A.H.; Majeed, S.; Singh, N.; Waheed, A. Prevalence of fragility fractures according to quality and outcomes framework (QOF) of the general medical services (GMS) contract and quality initiatives to improve osteoporosis care in the general practice within Caerphilly County Borough, Wales, UK: A feasibility study. MOJ Gerontol. Ger. 2018, 3, 98–104. [Google Scholar]
- Rodrigues, A.M.; Eusébio, M.; Santos, M.J.; Gouveia, N.; Tavares, V.; Coelho, P.S.; Mendes, J.M.; Branco, J.C.; Canhão, H. The burden and undertreatment of fragility fractures among senior women. Arch. Osteoporos. 2018, 13, 22. [Google Scholar] [CrossRef]
- Anderson, K.D.; Ko, F.C.; Virdi, A.S.; Sumner, D.R.; Ross, R.D. Biomechanics of Implant Fixation in Osteoporotic Bone. Curr. Osteoporos. Rep. 2020. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health and Care Excellent (NICE). Percutaneous Vertebroplasty. Interventional Procedures Guidance. Available online: https://www.nice.org.uk/guidance/IPG12 (accessed on 4 July 2019).
| CTPA Reports | Total | % of Cohort | % of Fractures |
|---|---|---|---|
| Cohort size | 161 | / | / |
| Fracture present | 54 | 33.5% | / |
| Unreported fracture | 31 | 19.3% | 57.4% |
| Reported vertebral fracture: All terminology | 23 | 14.3% | 42.6% |
| Reported vertebral fracture: Term ‘fracture’ used | 14 | 8.7% | 25.9% |
| Vertebral Fracture | No Vertebral Fracture | p | |
|---|---|---|---|
| Subsequent fracture: Hip | 6/54 (11.1%) | 3/107 (2.8%) | 0.0303 |
| Subsequent fracture: Vertebral | 3/54 (5.6%) | 3/107 (2.8%) | 0.3843 |
| Subsequent fracture: Wrist | 2/54 (3.7%) | 3/107 (2.8%) | 0.7566 |
| Subsequent fracture: All | 12/54 (22.2%) | 11/107 (10.3%) | 0.0414 |
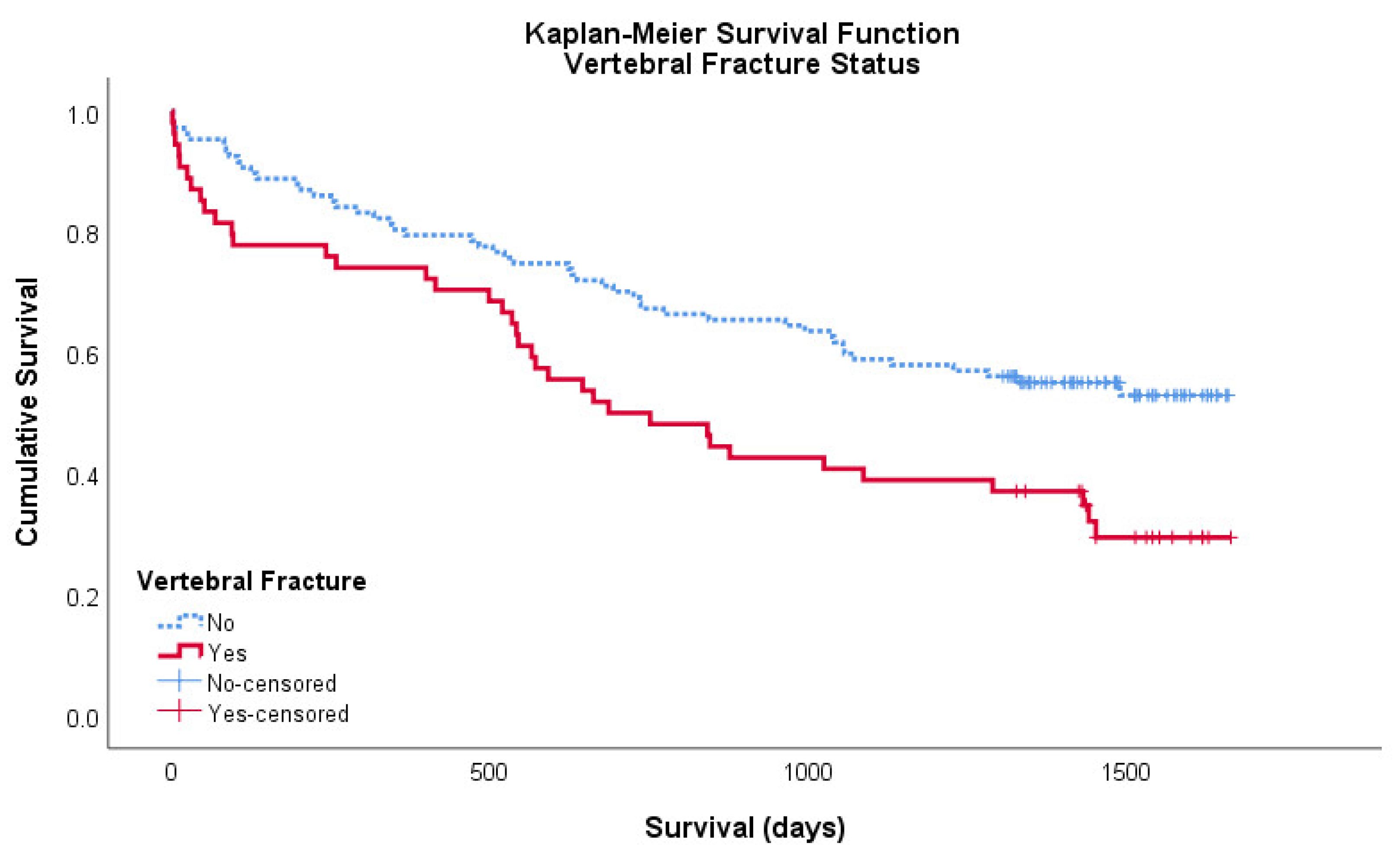
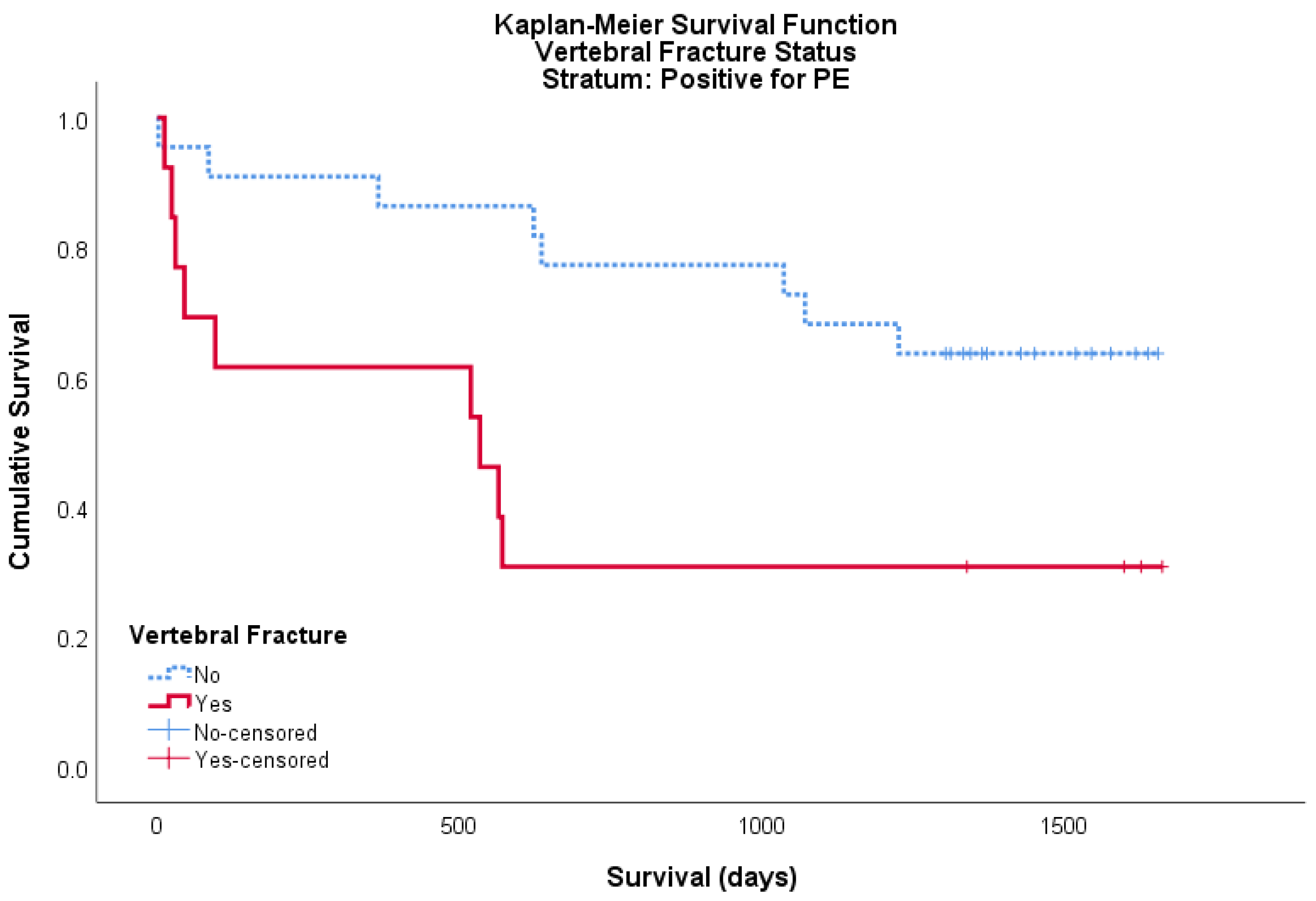
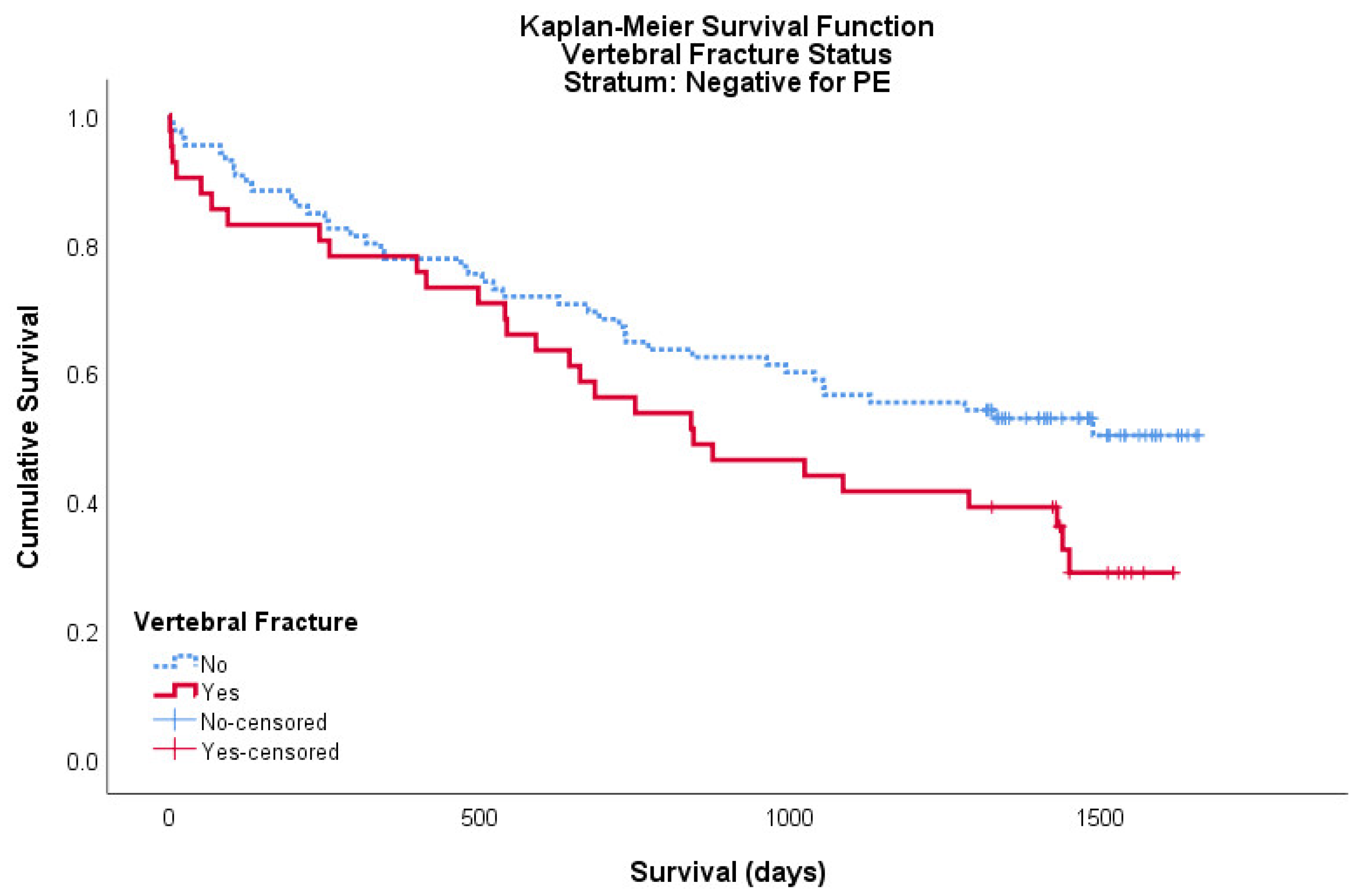
| Mortality by 26 June 2019 | 37/54 (68.5%) | 49/107 (45.8%) | 0.0063 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jones, L.; Singh, S.; Edwards, C.; Goyal, N.; Singh, I. Prevalence of Vertebral Fractures in CTPA’s in Adults Aged 75 and Older and Their Association with Subsequent Fractures and Mortality. Geriatrics 2020, 5, 56. https://doi.org/10.3390/geriatrics5030056
Jones L, Singh S, Edwards C, Goyal N, Singh I. Prevalence of Vertebral Fractures in CTPA’s in Adults Aged 75 and Older and Their Association with Subsequent Fractures and Mortality. Geriatrics. 2020; 5(3):56. https://doi.org/10.3390/geriatrics5030056
Chicago/Turabian StyleJones, Llewelyn, Sukhdev Singh, Chris Edwards, Nimit Goyal, and Inder Singh. 2020. "Prevalence of Vertebral Fractures in CTPA’s in Adults Aged 75 and Older and Their Association with Subsequent Fractures and Mortality" Geriatrics 5, no. 3: 56. https://doi.org/10.3390/geriatrics5030056
APA StyleJones, L., Singh, S., Edwards, C., Goyal, N., & Singh, I. (2020). Prevalence of Vertebral Fractures in CTPA’s in Adults Aged 75 and Older and Their Association with Subsequent Fractures and Mortality. Geriatrics, 5(3), 56. https://doi.org/10.3390/geriatrics5030056






