Foreign Body Ingestion: A Curious Case of the Missing Denture
Abstract
1. Introduction
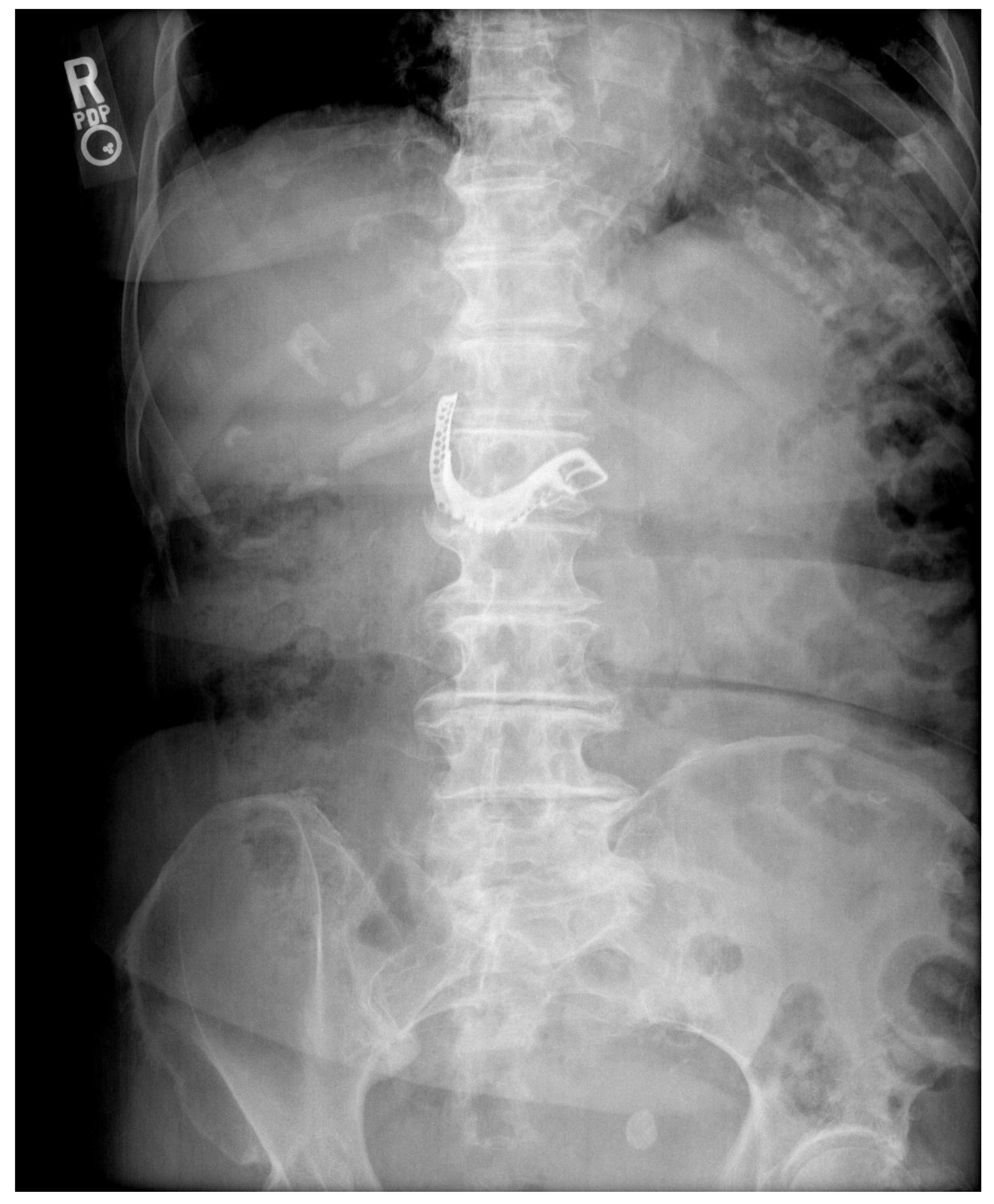
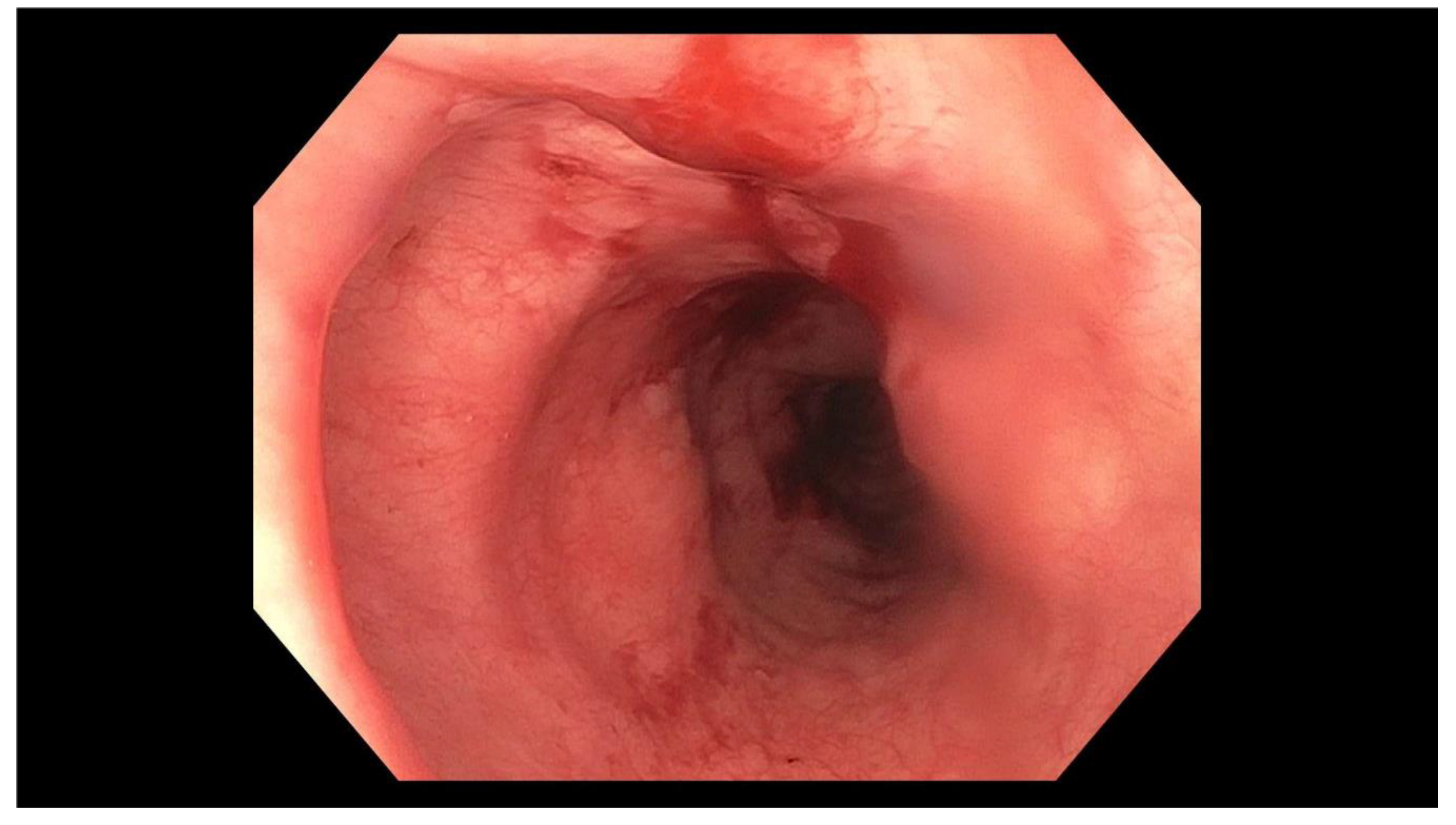
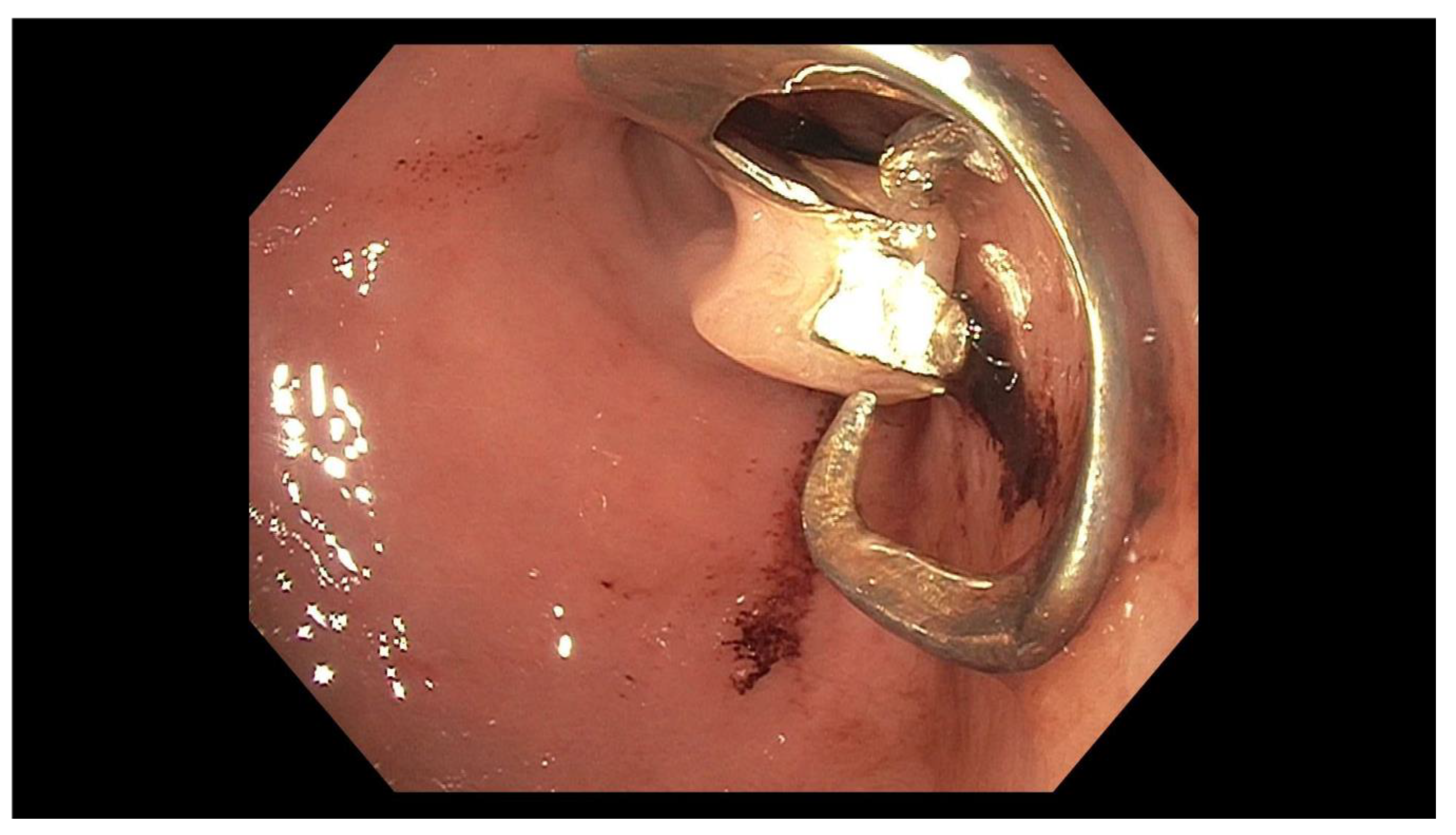
2. Case Report
3. Discussion
Author Contributions
Funding
Conflicts of Interest
Informed Consent
References
- Webb, W.A. Management of Foreign Bodies of the Upper Gastrointestinal Tract. Gastroenterology 1988, 94, 204–216. [Google Scholar] [CrossRef]
- Longstreth, G.F.; Longstreth, K.J.; Yao, J.F. Esophageal food impaction: Epidemiology and therapy. A retrospective, observational study. Gastrointest. Endosc. 2001, 53, 193–198. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.T.; Wong, R.K.H. Foreign Bodies. Gastrointest. Endosc. Clin. N. Am. 2007, 17, 361–382. [Google Scholar] [CrossRef]
- Ambe, P.; Weber, S.A.; Schauer, M.; Knoefel, W.T. Swallowed Foreign Bodies in Adults. Dtsch. Arztebl. Int. 2012, 109, 869–876. [Google Scholar] [CrossRef] [PubMed]
- Gutschow, C.A.; Leers, J.M.; Schroder, W.; Prenzel, K.L.; Fuchs, H.; Bollschweiler, E.; Bludau, M.; Holscher, A.H. Effect of aging on esophageal motility in patients with and without GERD. GMS Ger. Med. Sci. 2011, 9, 1–7. [Google Scholar]
- Bunker, P.G.; Aberdeen, S.D. The role of dentistry in problems of foreign bodies in the air and food passages. J. Am. Dent. Assoc. 1962, 64, 782–787. [Google Scholar] [CrossRef] [PubMed]
- Mizuno, K.; Takahashi, K.; Tominaga, K.; Nishigaki, Y.; Sato, H.; Ikarashi, S.; Hayashi, K.; Yamamoto, T.; Honda, Y.; Hashimoto, S.; et al. Endoscopic Removal of Ingested Dentures and Dental Instruments: A Retrospective Analysis. Gastroenterol. Res. Pract. 2016. [Google Scholar] [CrossRef] [PubMed]
- Libanio, D.; Garrido, M.; Jacome, F.; Dinis-Ribeiro, M.; Pedroto, I.; Marcos-Pinto, R. Foreign body ingestion and food impaction in adults: Better to scope than to wait. United Eur. Gastroenterol. J. 2018, 6, 974–980. [Google Scholar] [CrossRef] [PubMed]
- Chaves, D.M.; Ishioka, S.; Felix, V.N.; Sakai, P.; Gama-Rodrigues, J.J. Removal of a Foreign Body from the Upper Gastrointestinal Tract with a Flexible Endoscope: A Prospective Study. Endoscopy 2004, 36, 887–892. [Google Scholar] [CrossRef] [PubMed]

© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marquardt, P.; Derousseau, T.; Patel, N. Foreign Body Ingestion: A Curious Case of the Missing Denture. Geriatrics 2020, 5, 49. https://doi.org/10.3390/geriatrics5030049
Marquardt P, Derousseau T, Patel N. Foreign Body Ingestion: A Curious Case of the Missing Denture. Geriatrics. 2020; 5(3):49. https://doi.org/10.3390/geriatrics5030049
Chicago/Turabian StyleMarquardt, Patrick, Taylor Derousseau, and Neha Patel. 2020. "Foreign Body Ingestion: A Curious Case of the Missing Denture" Geriatrics 5, no. 3: 49. https://doi.org/10.3390/geriatrics5030049
APA StyleMarquardt, P., Derousseau, T., & Patel, N. (2020). Foreign Body Ingestion: A Curious Case of the Missing Denture. Geriatrics, 5(3), 49. https://doi.org/10.3390/geriatrics5030049




