First-Hand Experience of Severe Dysphagia Following Brainstem Stroke: Two Qualitative Cases
Abstract
1. Introduction
2. Materials and Methods
“Case studies are the preferred method when (a) “how” or “why” questions are being posed, (b) the investigator has little control over events, and (c) the focus is on a contemporary phenomenon within a real-life context”.
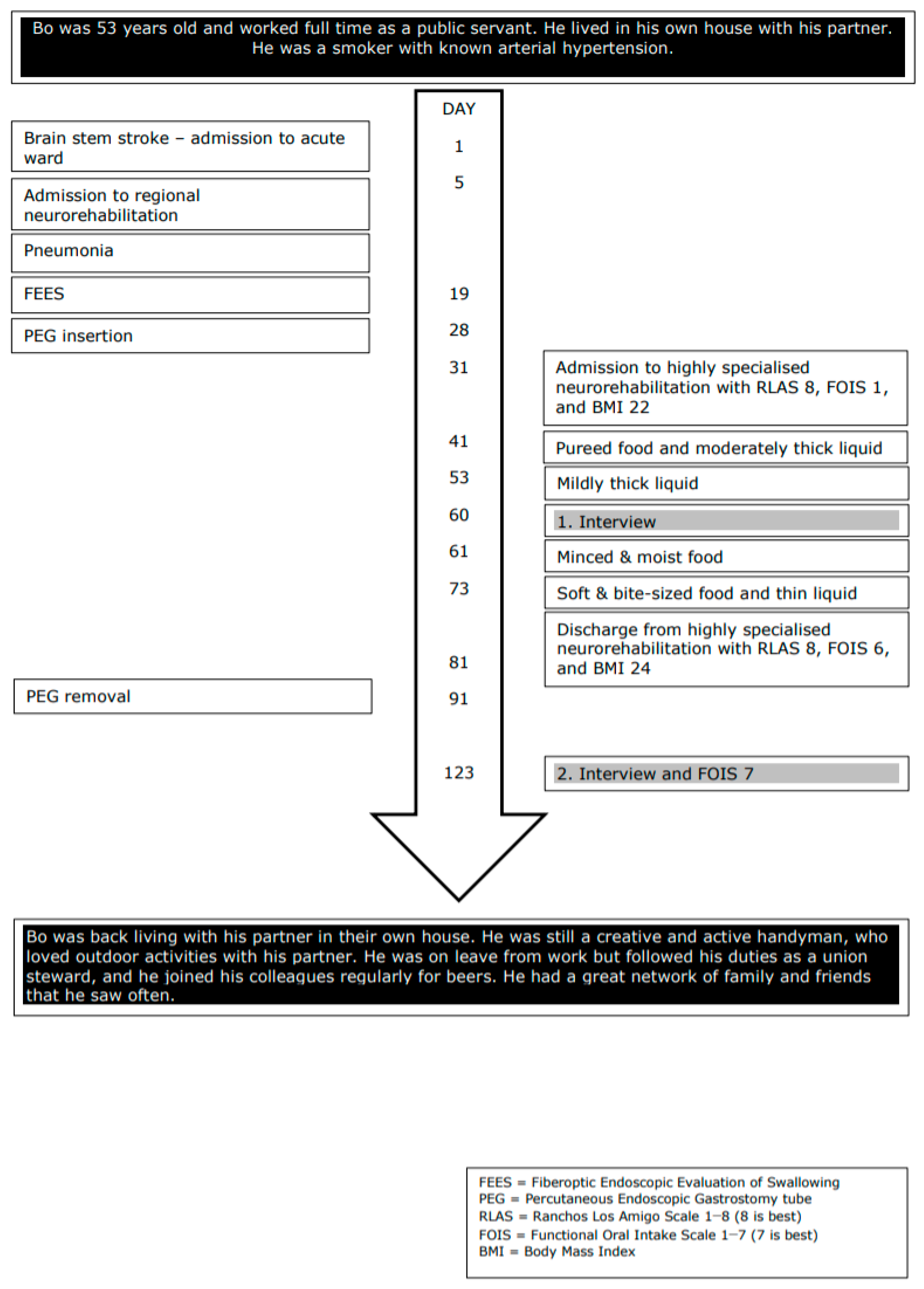
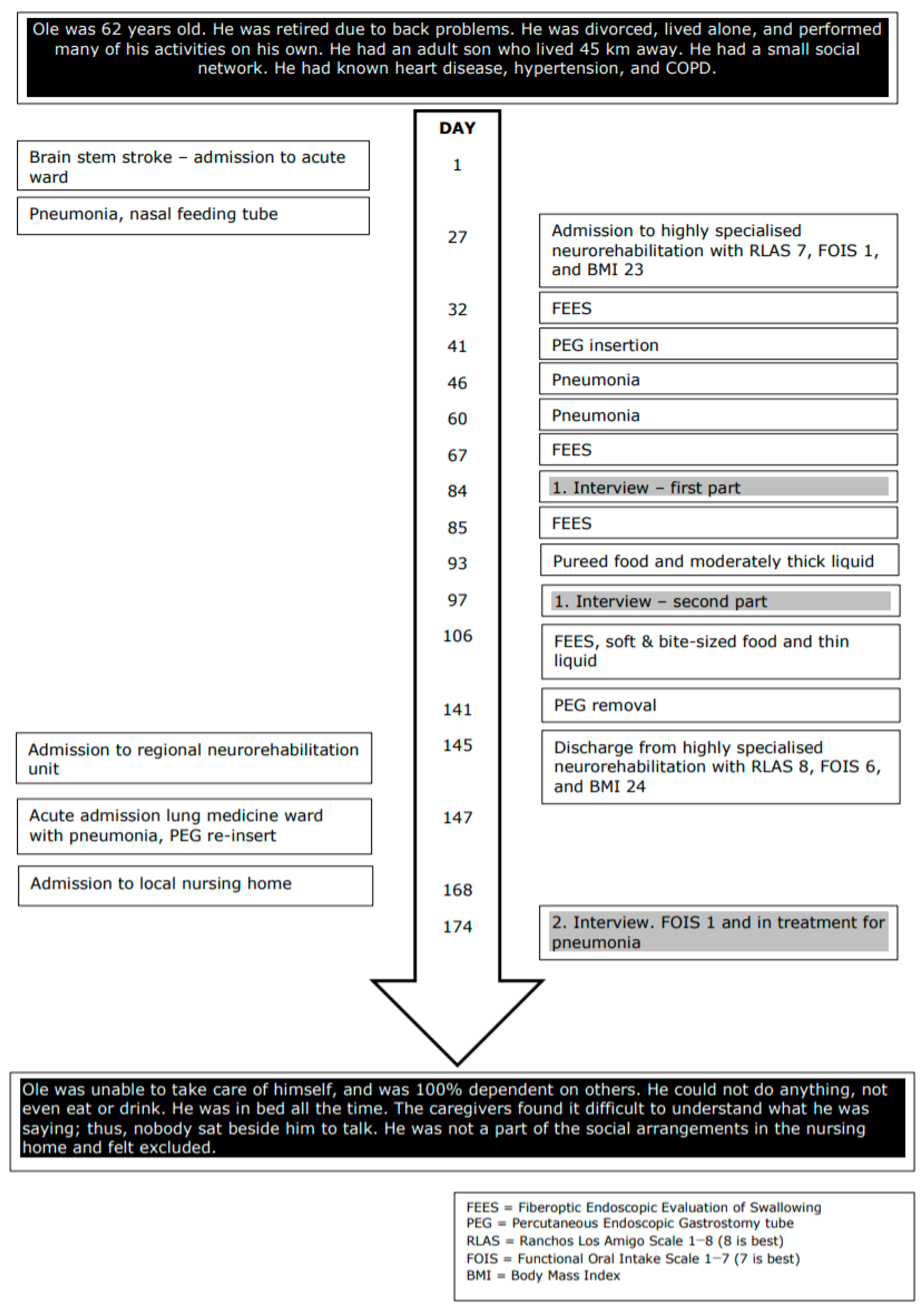
2.1. Sampling and Participants
2.2. Ethics
2.3. Data Collection
2.4. Data Analysis
3. Results
3.1. Mouth and Throat
3.1.1. Unusual Sensations and Feelings
“Clearing my voice ... I often did this ... and saliva was quite crazy in the beginning ... And then I couldn’t swallow either the mucus or the saliva. It all had to come out. It was damn annoying ... When it (the saliva) came, I spit it out. It’s rare that it all comes up”.(Ole)
“I think it’s disgusting when I start coughing in the middle of everything. I mostly eat by myself”.(Bo)
“Those who know me do understand what I am saying. But my voice, it has become more monotonous than it was before”.(Bo)
3.1.2. The Pleasure of Having Something Familiar in the Mouth
“The first portion of yogurt was like getting a better Christmas dinner”.(Bo)
“I haven’t tasted any proper food since I had the stroke … I rinse my mouth with soda and such like. It seems to help”.(Ole)
“It (the beer) no longer tastes good because it tastes like a “lazy beer” (without gas) when it is turning inside the mouth .... that is the same with red wine. The quality of the red wine has to be much better today than before, before I liked the taste of it”.(Bo)
3.1.3. Unfamiliar Objects “Invade” the Mouth
“I’ve tried that, but I don’t like it. They (therapists) put something in the gauze that I have to chew on and that I do not like. That’s the gauze I can’t have in my mouth, it’s something strange....”.(Ole)
“It was fried well, and it was just before it melted on the tongue. But chewing in gauze gives me a feeling of nausea”.(Ole)
“As a therapy, it is not horrible. But I can just taste their (therapists) rubber gloves and those tasted nasty”.(Ole)
3.2. Shared Dining
3.2.1. Eating Together
“I need to take my time and I have to concentrate on eating …… my wife quickly got used to it, so she knows very well that she should not talk to me when I have food in my mouth ... but it’s so annoying when you’re seeing other people. You may well be perceived as a little ignorant”.(Bo)
3.2.2. Social Interaction
“I have to concentrate when eating so it’s difficult to have a conversation at the same time… it’s very annoying when I eat with other people…. And others perceive me as snobbish”(Bo)
3.3. Recovery and Regression
“I do not talk with food in my mouth, and the meals at home have got another rhythm - eating and talking are separated”.(Bo)
“I’m not getting well by just lying down”.(Ole)
“My health is miserable… the damned pneumonia… it fills my head that I can’t get anything to eat and drink… it’s damn hot outside right now”(Ole)
4. Discussion
4.1. Limitations
4.2. Future Research
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Teasell, R.; Foley, N.; Doherty, T.; Finestone, H. Clinical characteristics of patients with brainstem strokes admitted to a rehabilitation unit. Arch. Phys. Med. Rehabil. 2002, 83, 1013–1016. [Google Scholar] [CrossRef] [PubMed]
- Miller, A.J. Neurophysiological basis of swallowing. Dysphagia 1986, 1, 91–100. [Google Scholar] [CrossRef]
- Horner, J.; Buoyer, F.G.; Alberts, M.J.; Helms, M.J. Dysphagia following brain-stem stroke: Clinical correlates and outcome. Arch. Neurol. 1991, 48, 1170–1173. [Google Scholar] [CrossRef] [PubMed]
- Meng, N.H.; Wang, T.G.; Lien, I.N. Dysphagia in patients with brainstem stroke: Incidence and outcome. Am. J. Phys. Med. Rehabil. 2000, 79, 170–175. [Google Scholar] [CrossRef]
- Turney, T.M.; Garraway, W.M.; Whisnant, J.P. The natural history of hemispheric and brainstem infarction in Rochester, Minnesota. Stroke 1984, 15, 790–793. [Google Scholar] [CrossRef]
- Klinke, M.E.; Wilson, M.E.; Hafsteinsdottir, T.B.; Jonsdottir, H. Recognizing new perspectives in eating difficulties following stroke: A concept analysis. Disabil. Rehabil. 2013, 35, 1491–1500. [Google Scholar] [CrossRef]
- Carlsson, E.; Ehrenberg, A.; Ehnfors, M. Stroke and eating difficulties: Long-term experiences. J. Clin. Nurs. 2004, 13, 825–834. [Google Scholar] [CrossRef]
- Perry, L.; McLaren, S. An exploration of nutrition and eating disabilities in relation to quality of life at 6 months post stroke. Health Soc. Care Community 2004, 12, 288–297. [Google Scholar] [CrossRef]
- Moloney, J.; Walsh, M. “I had no idea what a complicated business eating is...”: A qualitative study of the impact of dysphagia during stroke recovery. Disabil. Rehabil. 2018, 40, 1524–1531. [Google Scholar] [CrossRef]
- Martino, R.; Beaton, D.; Diamant, N.E. Perceptions of psychological issues related to dysphagia differ in acute and chronic patients. Dysphagia 2010, 25, 26–34. [Google Scholar] [CrossRef]
- Hellden, J.; Bergström, L.; Karlsson, S. Experiences of living with persisting post-stroke dysphagia and of dysphagia management—A qualitative study. Int. J. Qual. Stud. Health Well-Being 2018, 13, 1522194. [Google Scholar] [CrossRef] [PubMed]
- Stringer, S. Managing dysphagia in palliative care. Prof. Nurse 1999, 14, 489–492. [Google Scholar] [PubMed]
- Medin, J.; Larson, J.; von Arbin, M.; Wredling, R.; Tham, K. Striving for control in eating situations after stroke. Scand. J. Caring Sci. 2010, 24, 772–780. [Google Scholar] [CrossRef] [PubMed]
- Shune, S.E.; Linville, D. Understanding the dining experience of individuals with dysphagia in care facilities: A grounded theory analysis. Int. J. Nurs. Stud. 2019, 92, 144–153. [Google Scholar] [CrossRef] [PubMed]
- Dysfagi og aktivitetsproblemer med at synke-spise-drikke—Anbefalinger til ergoterapeutisk viden, færdigheder og kompetencer. Available online: https://www.etf.dk/uploads/uploads/public/documents/Faglige_selskaber/EFS_Dysfagi/anbefalinger_dysfagi_2019.pdf (accessed on 18 November 2019).
- Luker, J.; Lynch, E.; Bernhardsson, S. Stroke survivor’s experiences of physical rehabilitation: A systematic review of qualitative studies. Arch. Phys. Med. Rehabil. 2015, 96, 1698–1708. [Google Scholar] [CrossRef] [PubMed]
- Yin, R.K. Case Study Research: Design and Methods, 4th ed.; SAGE Publications, Inc.: Thousand Oaks, CA, USA, 2009. [Google Scholar]
- Merleau-Ponty, M. Kroppens Fænomenologi; Det lille forlag: Copenhagen, Denmark, 1994. [Google Scholar]
- Gallagher, S. How the Body Shapes the Mind; Oxford University Press: Oxford, UK, 2005. [Google Scholar]
- Gagnier, J.J.; Kienle, G.; Altman, D.G.; Moher, D.; Sox, H.; Riley, D. The CARE Guidelines: Consensus-based Clinical Case Reporting Guideline Development. BMJ Case Rep. 2013, 7, 223. [Google Scholar] [CrossRef]
- Kjaersgaard, A.; Nielsen, L.H.; Sjolund, B.H. Randomized trial of two swallowing assessment approaches in patients with acquired brain injury: Facial-oral tract therapy versus fibreoptic endoscopic evaluation of swallowing. Clin. Rehabil. 2014, 28, 243–253. [Google Scholar] [CrossRef]
- Kjaersgaard, A.; Nielsen, L.H.; Sjolund, B.H. Factors affecting return to oral intake in inpatient rehabilitation after acquired brain injury. Brain Inj. 2015, 29, 1094–1104. [Google Scholar] [CrossRef]
- Kjaersgaard, A.; Kristensen, H.K. Brain injury and severe eating difficulties at admission—Patient perspective nine to fifteen months after discharge: A pilot study. Brain Sci. 2017, 7, 96. [Google Scholar] [CrossRef]
- Patton, M. Qualitative Research and Evaluation Methods, 2nd ed.; SAGE Publications: Thousand Oaks, CA, USA, 2009. [Google Scholar]
- Puri, K.S.; Suresh, K.R.; Gogtay, N.J.; Thatte, U.M. Declaration of Helsinki, 2008: Implications for stakeholders in research. J. Postgrad. Med. 2009, 55, 131–134. [Google Scholar]
- Houlden, H.; Edwards, M.; McNeil, J.; Greenwood, R. Use of the Barthel index and the functional independence measure during early inpatient rehabilitation after single incident brain injury. Clin. Rehabil. 2006, 20, 153–159. [Google Scholar] [CrossRef] [PubMed]
- McHorney, C.A.; Robbins, J.; Lomax, K.; Rosenbek, J.C.; Chignell, K.; Kramer, A.E.; Bricker, D.E. The SWAL-QOL and SWAL-CARE outcomes tool for oropharyngeal dysphagia in adults: III. Documentation of reliability and validity. Dysphagia 2002, 17, 97–114. [Google Scholar] [CrossRef] [PubMed]
- Creswell, J.W. Qualitative procedures. Research Design, 3th ed; Creswell, J.W., Ed.; SAGE Publications: Thousand Oaks, CA, USA, 2009; pp. 173–202. [Google Scholar]
- Giorgi, A. The Descriptive Phenomenological Method in Psychology; Duquesne University Press: Pittsburg, PA, USA, 2009. [Google Scholar]
- Kvale, S.; Brinkmann, S. Interviews—Learning the Craft of Qualitative Research Interviewing, 2nd ed.; SAGE: Thousand Oaks, CA, USA, 2009; pp. 97–121. [Google Scholar]
- Kvale, S. The social construction of validity. Qual. Inq. 1995, 1, 19–40. [Google Scholar] [CrossRef]
- Graneheim, U.H.; Lundman, B. Qualitative content analysis in nursing research: Concepts, procedures and measures to achieve trustworthiness. Nurse Educ. Today 2004, 24, 105–112. [Google Scholar] [CrossRef] [PubMed]
- Hansen, T.S.; Jakobsen, D. A decision-algorithm defining the rehabilitation approach: ‘Facial oral tract therapy’®. Disabil. Rehabil. 2010, 32, 1447–1460. [Google Scholar] [CrossRef] [PubMed]
- Groher, M.E.; Crary, M.A. Dysphagia: Clinical Management in Adults and Children, 1st ed.; Mary Heights, Missouri: Mosby, Inc.: St. Louis, MO, USA, 2010. [Google Scholar]
- Gustafsson, B.; Tibbling, L. Dysphagia, an unrecognized handicap. Dysphagia 1991, 6, 193–199. [Google Scholar] [CrossRef] [PubMed]
- Gallagher, S.; Zahavi, D. The Phenomenological Mind; Routledge: London, UK; New York, NY, USA, 2008. [Google Scholar]
- Pallesen, H. Body, coping and self-identity. A qualitative 5-year follow-up study of stroke. Disabil. Rehabil. 2014, 36, 232–241. [Google Scholar] [CrossRef]
- Arntzen, C.; Borg, T.; Hamran, T. Long-term recovery trajectory after stroke: An ongoing negotiation between body, participation and self. Disabil. Rehabil. 2015, 37, 1626–1634. [Google Scholar] [CrossRef]
- Leder, D. The Absent Body; University of Chicago Press: Chicago, IL, USA, 1990. [Google Scholar]
- Thornquist, E. Movement and Interaction; The Sherborne Approach and Documentation; Universitetsforlaget: Oslo, Norway, 2012. [Google Scholar]
- Gallagher, S. Født med en krop. I. In Krop og Læring; Roessler, K.K., Ed.; Klim: Aarhus, Denmark, 2002. [Google Scholar]
- Hafsteinsdottir, T.B.; Grypdonck, M. Being a stroke patient: A review of the literature. J. Adv. Nurs. 1997, 26, 580–588. [Google Scholar] [CrossRef]
- Salter, K.I.; Hellings, C.; Foley, N.; Teasell, R. The experience of living with stroke: A qualitative meta-synthesis. J. Rehabil. Med. 2008, 40, 595–602. [Google Scholar] [CrossRef]
- Kessler, D.; Dubouloz, C.J.; Urbanowski, R.; Egan, M. Meaning perspective transformation following stroke: The process of change. Disabil. Rehabil. 2009, 31, 1056–1065. [Google Scholar] [CrossRef] [PubMed]
- Kubina, L.A.; Dubouloz, C.J.; Davis, C.G.; Kessler, D.; Egan, Y. The process of re-engagement in personally valued activities during the two years following stroke. Disabil. Rehabil. 2013, 35, 236–243. [Google Scholar] [CrossRef] [PubMed]
| Introduction |
|---|
| 1. General questions related to eating and drinking 2. The meaning of food and liquid prior to the injury 3. The meaning of food and liquid at the time of the interview and immediately after the injury 4. Are you currently experiencing any physical difficulties that may influence eating and drinking? How was it immediately after the injury? 5. Are you currently experiencing worries and if so, do they influence your mood in relation to eating and drinking? How was it immediately after the injury? 6. Your social life (meals with the family, work, leisure activities, parties, vacations, etc.)—how is it currently? How was it immediately after the injury? 7. Your experiences of obtaining food and drink via a feeding tube Closing interview (debriefing) |
| Step | Analytical Process | |
|---|---|---|
| 1 | The entire interview was read and reread to gain an overall picture | The first author transcribed each interview. Each interview transcript was then read by the other author, after which the interview was played again to ensure that the transcription was accurate |
| 2 | Natural “meaning units,” as they were expressed by the interviewees were identified by the researcher | The data were analysed in depth using a phenomenological method to trace thematic patterns of how the two informants experienced severe dysphagia during their inpatient neurorehabilitation and how they had recovered during the one month since discharge. This part of the analysis was first performed by both authors individually and subsequently by consensus of the two authors |
| 3 | The dominating themes in the meaning units were identified. The researcher attempted to form themes from the interviewed person’s point of view, as the researcher understood it | Meaning units were organized and gradually transformed into categories. Firstly, the data were separated for each informant, and secondly, similarities and differences were noted in an iterative process |
| 4 | The meaning units were questioned based on the research questions from the semi-structured interview guide | The data were described in a final set of themes and sub-themes that answered the research questions regarding how the two people with BSS experienced severe dysphagia during their inpatient neurorehabilitation and how they expressed their recovery approximately one month following discharge |
| 5 | The non-redundant themes were condensed into descriptive statements | The first draft of the final results was co-generated and discussed by both authors, after which it was considered to constitute essential knowledge |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kjaersgaard, A.; Pallesen, H. First-Hand Experience of Severe Dysphagia Following Brainstem Stroke: Two Qualitative Cases. Geriatrics 2020, 5, 15. https://doi.org/10.3390/geriatrics5010015
Kjaersgaard A, Pallesen H. First-Hand Experience of Severe Dysphagia Following Brainstem Stroke: Two Qualitative Cases. Geriatrics. 2020; 5(1):15. https://doi.org/10.3390/geriatrics5010015
Chicago/Turabian StyleKjaersgaard, Annette, and Hanne Pallesen. 2020. "First-Hand Experience of Severe Dysphagia Following Brainstem Stroke: Two Qualitative Cases" Geriatrics 5, no. 1: 15. https://doi.org/10.3390/geriatrics5010015
APA StyleKjaersgaard, A., & Pallesen, H. (2020). First-Hand Experience of Severe Dysphagia Following Brainstem Stroke: Two Qualitative Cases. Geriatrics, 5(1), 15. https://doi.org/10.3390/geriatrics5010015





