Abstract
Background: Sexual dysfunction is a complication of transurethral resection of prostate (TURP). There is a lack of knowledge of the effect of discharge programs aiming at improving sexual function in older patients undergoing TURP. Objective: To investigate the effect of the nurse-led sexual health discharge program on the sexual function of older patients undergoing TURP. Methods: This randomized controlled clinical trial was conducted on 80 older patients undergoing TURP in an urban area of Iran. Samples were selected using a convenience method and were randomly assigned into intervention and control groups (n = 40 in each group). The sexual health discharge program was conducted by a nurse in three sessions of 30–45 min for the intervention group. Sexual function scores were measured using the International Index of Erectile Function (IIEF) Questionnaire, one and three months after the intervention. Results: The intervention significantly improved erectile function (p = 0.044), sexual desire (p = 0.01), satisfaction with sexual intercourse (p = 0.03), overall satisfaction with sexual function (p = 0.01), and the general score of sexual function (p = 0.038), three months after the program. In the first month after the intervention, except in sexual desire (p = 0.028), no statistically significant effect of the program was reported (p > 0.05). Conclusion: The nurse-led sexual health discharge program led to the improvement of the sexual function of older patients undergoing TURP over time. This program can be incorporated into routine discharge programs for the promotion of well-being in older patients.
1. Introduction
Benign prostatic hyperplasia (BPH) as an age-related process is characterized by the hypertrophy of the prostate gland [1] and negatively influences patients’ quality of life [2]. The aging process is associated with lower urinary tract symptoms independent of the enlargement of the prostate gland [3] and affects 28% of men aged more than 70 years [4].
Transurethral resection of prostate (TURP) is one of the conventional treatments of BPH [5] and can lead to complications such as early iatrogenic stress incontinence (30%–40%), stricture (2.2%–9.8%), erectile issues (3.4%–32%), and ejaculatory dysfunction (53%–75%) [6]. Additionally, patients often feel distress with regard to their sexual function and sexuality [7]. Therefore, management of their sexual dysfunction needs multi-dimensional programs consisting of physiological, psychological, and therapeutic interventions [8]. It has been shown that a 10-week group-based cognitive-behavioral program can improve the sexual function of patients after radical prostatectomy [9]. Additionally, continuous improvements in sexual outcomes after the use of the internet-based sexual counseling program in patients with prostate cancer have been reported [10].
Planning for the discharge process and transnational care to home is an important task of healthcare professionals, especially nurses [11]. The discharge program should be started upon admission, continued to the discharge and follow up visits [12], as well as should be specialized to each patient’s needs [13]. The discharge planning program has positive effects on mental health [11] and cardiovascular health [13]. It addition, it can reduce the readmission rate of patients to the hospital [14]. However, there is a lack of evidence surrounding the effect of the discharge program run by the nurse on sexual function among older patients with prostate disorders. Therefore, this study examined the effect of the nurse-led sexual health discharge program on the sexual function of older patients undergoing TURP.
2. Materials and Methods
2.1. Study Design
This randomized controlled trial with one intervention group and one control group was conducted from June 2017 to April 2018. The study process was depicted using the CONSORT flow diagram (Figure 1).
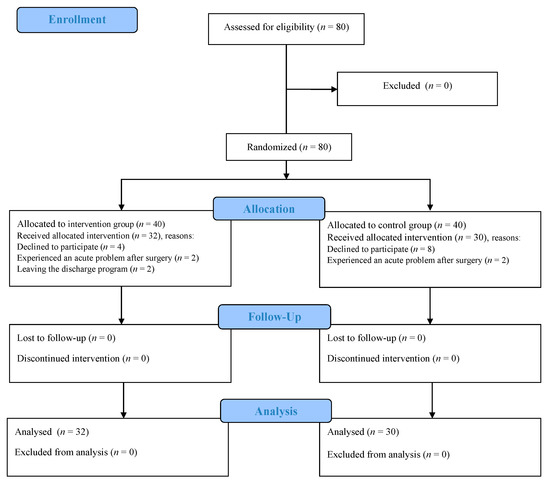
Figure 1.
The study process according to the CONSORT flow diagram.
Given a 15% chance of attrition rate, α = 0.05, and a power of 0.80, the sample size was estimated 40 people in each group. Accordingly, 80 older patients undergoing TURP were selected using a convenience sampling method from the urological ward of a referral teaching hospital in an urban area of Iran. They were randomly assigned to each group via a 4:4-block randomization method by a staff nurse who was unaware of the assignments through a system of sealed envelopes. Allocation codes were written on the separate pieces of paper, placed in sealed envelopes and in an opaque box. The envelopes were removed from the box to determine the patient’s group by the staff nurse. After opening them, they were put back into the box. The sampling was continued until that the samples in both groups was accomplished. Identity of research hindered blinding of the subjects to the group assignments. However, the data analyst (SF) was unaware of the group assignments and the codes assigned to each group was disclosed after accomplishing data analysis.
2.2. Setting and Participants
Inclusion criteria to recruit the participants were as follows: (i) older patients aged between 60 and 85 years; (ii) being married; (iii) no history of receiving sexual health education; (iv) no hypogonadism and neurological disorders such as multiple sclerosis and spinal cord injuries; (v) no history of the pelvic floor muscle surgery; (vi) no consumption of opioids, alcohol, anti-depressants, or anti-dementia drugs; (vii) no previous psychiatric disorder; and (viii) no history of coronary artery diseases, bypass graft surgery, and current atherosclerotic diseases. Unwillingness to participate in the study, not following up to the scheduled discharge program, and the experience of an acute health problem after surgery led to exclusion from the study.
2.3. Measures
Data were collected using a demographic data form and the International Index of Erectile Function (IIEF) Questionnaire.
- ○
- The demographic data form for gathering data on the older patients’ age, body mass index, education level, health insurance status, employment status, economic status, independence in the activities of daily living, and past medical history.
- ○
- The IIEF Questionnaire was developed and validated by Rosen in 1997. It is a self-report questionnaire of the male sexual function and consists of 15 questions with a 5-point Likert scale. The minimum and maximum scores were 15 and 75, respectively and a higher score indicated a better sexual performance. Severity of erectile dysfunction was classified as follows: 6–10 (severe), 11–16 (moderate), 17–21 (mild-to-moderate), 22–25 (mild), 26–30 (no dysfunction) [15]. More details on the number of items and relating scores were presented in Table 1.
 Table 1. Items and the scores of the International Index of Erectile Function (IIEF) Questionnaire.
Table 1. Items and the scores of the International Index of Erectile Function (IIEF) Questionnaire.
2.4. Validity and Reliability
For content validity, the demographic data form and the IIEF questionnaire were given to 10 specialists of nursing, reproductive health, and urology to seek their opinions. For reliability using internal consistency, the Cronbach’s alpha coefficient of the IIEF questionnaire was calculated and reported 0.97.
2.5. Ethical Considerations
Ethical permission was obtained from the ethics committee affiliated with university in which the second author (HS) worked (decree code: IR.TUMS.FNM.REC.1396.2300). The purpose and method of the discharge program were explained to the participants before commencing the study, and they were asked to sign the written consent form, if they were willing to take part in the study. They were assured of the possibility of withdrawal from the study without any effect on the process of care. Additionally, the older patients’ names remained confidential during the study and publication of findings. This clinical trial was registered on the website of registry of clinical trials under the code of IRCT20180917041052N1.
2.6. Intervention
The nurse-led sexual health discharge program was designed based on a thorough review of online literature and nursing textbooks [1,8], as well as consultation with experts in the fields of cancer nursing and urology.
Before the intervention, a demographic data form was completed and the sexual function of the older patients in the intervention and control groups was measured using the IIEF questionnaire. Next, the program was conducted for the intervention group in the urology ward by the first researcher (RB) who was a staff nurse and had required education and training regarding the pedagogical approach of sexual function during three teaching sessions as follows:
- ○
- The first session: Description of the anatomy and physiology of the urinary tract and prostate gland function, definition of BPH, causes, and clinical manifestations [1,8].
- ○
- The second session: Diagnosis of BPH, explanation of TURP as a treatment modality of BPH, probable complications of TURP including pain, infection, bleeding, urinary incontinence, and sexual dysfunction [1,16].
- ○
- The third session: Effect of fatigue on sexual function, the importance of managing urinary incontinence for improving sexual satisfaction, role of physical activity and exercise in the recovery of sexual performance, role of pelvic floor muscle exercises in the improvement of sexual function and activity through controlling urinary incontinence [8,17,18].
The duration of each education session varied from 30 to 45 min. It was presented to the older patients individually from admission until discharge from the hospital, face to face in their rooms, and with the consideration of the older patients’ sexual health level and past knowledge. Education was discontinued in the first hours after surgery and when they had pain, bleeding and anxiety. To ensure of the effectiveness of education and the older patients’ learning, their questions were answered through holding discussions. In addition, educational materials were provided to the older patients via an educational booklet.
For followed up, the first researcher made telephone calls every two weeks to answer the patients’ questions and monitor the implementation of the discharge program at home after discharge. In addition, the researcher’s telephone number was given to the participants for necessary contacts.
The control group only received routine care consisting of brief education by staff nurses in the ward regarding discharge care. Sexual function in both groups was measured one and three months after discharge using the questionnaires.
2.7. Data analysis
Descriptive (frequency, percentage, mean and standard deviation) and inferential statistics (Fisher exact test, independent t-test, paired-t test, and ANOVA test) were used for data analysis. Simple linear regression was used to assess differences in sexual function between the groups before, one month and three months after the intervention. To investigate the effect of time trends, intervention, and interactions between time and groups, the repeated measures of analyses of variance were used. All statistical analyses were performed using the SPSS software version 16 for Windows (SPSS Inc., Chicago, IL, USA) and p value less than 0.05 was considered statistically significant.
3. Results
The mean age of the older patients in the intervention and control groups was 64.13 ± 6.23 and 67.27 ± 6.80, respectively. The groups were homogenous in terms of age, body mass index, occupation status, health insurance, economic status, independence in the activity of daily living, history of hypertension, diabetes mellitus, heart failure, smoking, use of drugs for BPH and chronic obstructive pulmonary disease (COPD) (p > 0.05). However, there was a statistically significant difference between the groups in the education level (p = 0.018) (Table 2).

Table 2.
Demographic characteristics of the older patients in the groups.
Regarding the sexual function (Table 3), the mean and standard deviation of sexual performance in the intervention and control groups before the intervention were 45.12 ± 22.21 and 44.03 ± 24.34, respectively. There were no statistically significant differences between the groups in terms of sexual function categories and overall sexual function.

Table 3.
Comparison of sexual function before and after the intervention between the groups.
The mean score and standard deviation of the sexual function in the intervention and control groups one month after the intervention were reported 31.72 ± 22.38 and 21.03 ± 21.93, respectively. The program did not have any statistically significant effect on the older patients’ sexual function in this time period except on the sexual desire domain (p = 0.028).
Three months after the intervention, the mean scores of sexual function in the groups were reported 43.75 ± 22.62 and 29.60 ± 20.18, respectively. The assessment of sexual function between the groups three months after the intervention demonstrated that the scores of erectile function (p = 0.044), sexual desire (p = 0.01), satisfaction with sexual intercourse (p = 0.03), overall satisfaction (p = 0.01) domains, and also the overall score of sexual function (p = 0.038) had statistically significant differences. Therefore, the nurse-led sexual health discharge program had statistically significant effects on these domains over time. However, no statistically significant difference was found between the groups in orgasmic function (p = 0.331) (Table 3).
To examine and compare the sexual performance of the older patients before, one month and three months after the intervention in the groups, the analysis of variance with repeated measures showed that the intervention without the effect of time had no statistically significant effect on sexual function (p = 0.24), but a statistically significant effect was observed in examining the interaction between time and the intervention on sexual function (p = 0.04). This meant that for the intervention to create a positive effect on the older patients’ sexual function, time was required and positive results were obtained over a longer period of time (Table 4; Figure 2).

Table 4.
Effects of the intervention and time on the sexual function.
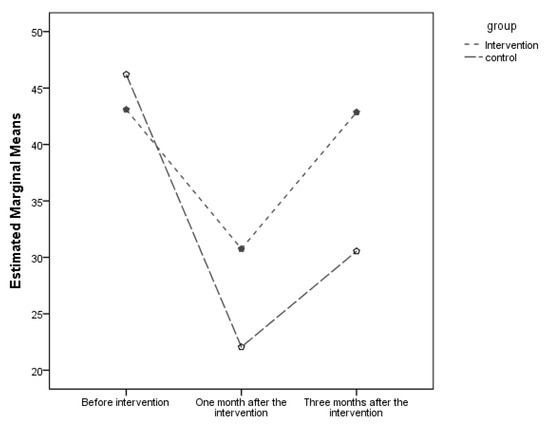
Figure 2.
Mean scores of sexual function at different times.
4. Discussion
The present study aimed to evaluate the older patients’ sexual function undergoing TURP after the implementation of the nurse-led discharge program. Regarding the comparison of sexual function before and three months after the intervention, the total mean score of sexual function in the intervention group was significantly higher than that of the control group. However, at the first month after the intervention, only improvements in sexual desire were observed in the intervention group. Statistically insignificant changes on other areas could be due to the physical consequences of surgery such as the presence of urinary catheter, pain, dysuria, bleeding of the urethra, and incontinence after TURP.
Regarding the role of physical activity in the improvement of physical and psychological sexual function, our study results supported the findings of Simon et al.’s study in the USA [19]. They found that exercise had a positive correlation with the sexual function of participants. In addition, the results of the present study were in line with those of Geraerts et al.’s (2016) study in Belgium [20] investigating the effect of pelvic floor muscle exercises on erectile dysfunction and ejaculation after radical prostatectomy, indicating the improvement of sexual function after the intervention.
Considering the psychological part of the educational discharge program, our findings were supported by those of Brotto et al. (2008) in Canada [21], indicating that the psychological education intervention significantly reduced women sexual dysfunction. In another study, Lassen et al. (2013) in Canada [22] showed that nursing discharge planning based on psycho-educational interventions had positive effects on patients’ sexual function after prostatectomy.
No study was found in the literature to assess the impact of the nurse-led discharge program on the sexual function with a focus on both physical and psychological aspects in older patients undergoing TURP. This study considered various physical and psychological factors influencing the sexual health of older patients. Therefore, it had a holistic perspective toward the discharge program to cover all dimensions influencing their sexual function [23].
A limitation of this study was that the researcher had no possibility to educate the older patients’ partners and spouses with regard to sexual function. Therefore, further studies are needed to assess the status and sexual satisfaction of their spouses and partners. In addition, the small sample size and a focus on older patients one month and three months after TURP could influence the generalizability of findings to patients in other age groups and in longer follow up periods. Due to the interaction between time and intervention on sexual function, future studies with a longer intervention duration are suggested to evaluate the effect of time on sexual function.
5. Conclusions
This was the first randomized controlled trial on the effect of the nurse-led discharge program on the sexual function of older patients undergoing TURP with a focus on both physical and psychological aspects influencing sexual function. The results of this trial showed that a nurse-led discharge program had a positive effect on the sexual function of older patients undergoing TURP. This program can be incorporated into routine discharge planning for the promotion of well-being in older patients. Nurses are suggested to perform a need assessment and design and implement discharge programs for improving the sexual health and quality of life of older patients undergoing invasive procedures such as TURP.
Author Contributions
Conceptualization: R.B., H.S., and M.V.; methodology: R.B., H.S., and M.V.; investigation & formal analysis: R.B., and S.F.; writing—original draft preparation: M.V., R.B., H.S., and S.A.; writing—review and editing: M.V., S.A.; project administration: M.V. and H.S. All authors have read and agreed to the published version of the manuscript.
Funding
This article was one part of the first author’ master thesis approved by Tehran University of Medical Sciences, Tehran, Iran (Decree number: IR.TUMS.FNM.REC.1396.2300). The university did not influence the design of the study, nor they influenced the collection of data, the data analysis and interpretation or the reporting of results.
Acknowledgments
The authors would like to thank all older patients for their cooperation with this study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Hinkle, J.L.; Cheever, K.H. Brunner & Suddarth’s Textbook of Medical-Surgical Nursing; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2013. [Google Scholar]
- Speakman, M.; Kirby, R.; Doyle, S.; Ioannou, C. Burden of male lower urinary tract symptoms (LUTS) suggestive of benign prostatic hyperplasia (BPH)–focus on the UK. BJU Inter. 2015, 115, 508–519. [Google Scholar] [CrossRef] [PubMed]
- Bushman, W. Etiology, epidemiology, and natural history. Urol. Clin. 2009, 36, 403–415. [Google Scholar] [CrossRef] [PubMed]
- Girman, C.J.; Jacobsen, S.J.; Guess, H.A.; Oesterling, J.E.; Chute, C.G.; Panser, L.A.; Lieber, M.M. Natural history of prostatism: Relationship among symptoms, prostate volume and peak urinary flow rate. J. Urol. 1995, 153, 1510–1515. [Google Scholar] [CrossRef]
- Milicevic, S. The impact of benign prostatic hyperplasia surgical treatment with turp method on the quality of life. Acta Inform. Med. 2011, 19, 142–145. [Google Scholar] [CrossRef] [PubMed]
- Rassweiler, J.; Teber, D.; Kuntz, R.; Hofmann, R. Complications of transurethral resection of the prostate (TURP)—incidence, management, and prevention. Eur. Urol. 2006, 50, 969–980. [Google Scholar] [CrossRef] [PubMed]
- Salonia, A.; Burnett, A.L.; Graefen, M.; Hatzimouratidis, K.; Montorsi, F.; Mulhall, J.P.; Stief, C. Prevention and management of postprostatectomy sexual dysfunctions part 2: Recovery and preservation of erectile function, sexual desire, and orgasmic function. Eur. Urol. 2012, 62, 273–286. [Google Scholar] [CrossRef] [PubMed]
- Kozier, B.; Erb, G.L.; Berman, A.; Snyder, S.; Frandsen, G. Kozier and Erb’s Fundamentals of Nursing: Concepts, Process, and Practice, 10th ed.; Pearson Australia: Melbourne, Australia, 2016. [Google Scholar]
- Molton, I.R.; Siegel, S.D.; Penedo, F.J.; Dahn, J.R.; Kinsinger, D.; Traeger, L.N.; Antoni, M.H. Promoting recovery of sexual functioning after radical prostatectomy with group-based stress management: The role of interpersonal sensitivity. J. Psychosom. Res. 2008, 64, 527–536. [Google Scholar] [CrossRef] [PubMed]
- Schover, L.R.; Canada, A.L.; Yuan, Y.; Sui, D.; Neese, L.; Jenkins, R.; Rhodes, M.M. A randomized trial of internet-based versus traditional sexual counseling for couples after localized prostate cancer treatment. Cancer 2012, 118, 500–509. [Google Scholar] [CrossRef] [PubMed]
- Nurjannah, I.; Mills, J.; Usher, K.; Park, T. Discharge planning in mental health care: An integrative review of the literature. J. Clin. Nurs. 2014, 23, 1175–1185. [Google Scholar] [CrossRef] [PubMed]
- Sharif, F.; Moshkelgosha, F.; Molazem, Z.; Kalyani, M.N.; Vossughi, M. The effects of discharge plan on stress, anxiety and depression in patients undergoing percutaneous transluminal coronary angioplasty: A randomized controlled trial. Int. J. Community Based Nurs. Midwifery 2014, 2, 60–68. [Google Scholar] [PubMed]
- Andrietta, M.P.; Lopes Moreira, R.S.; Bottura Leite de Barros, A.L. Hospital discharge plan for patients with congestive heart failure. Revista Latino-Americana de Enfermagem 2011, 19, 1445–1452. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Jack, B.W.; Chetty, V.K.; Anthony, D.; Greenwald, J.L.; Sanchez, G.M.; Johnson, A.E.; Martin, S. A reengineered hospital discharge program to decrease rehospitalization: A randomized trial. Ann. Int. Med. 2009, 150, 178–187. [Google Scholar] [CrossRef] [PubMed]
- Rosen, R.C.; Cappelleri, J.C.; Gendrano, N., III. The International Index of Erectile Function (IIEF): A state-of-the-science review. Int. J. Impot. Res. 2002, 14, 226–244. [Google Scholar] [CrossRef] [PubMed]
- Tanagho, E.A.; McAninch, J.W. Smith’s Urology; McGraw Hill Professional: New York, NY, USA, 2008. [Google Scholar]
- Bridgeman, B.; Roberts, S.G. The 4-3-2 Method for Kegel Exercises. Am. J. Men’s Health 2010, 4, 75–76. [Google Scholar] [CrossRef] [PubMed]
- Hodges, P.W.; Stafford, R.E.; Hall, L.; Neumann, P.; Morrison, S.; Frawley, H.; Cameron, A.P. Reconsideration of pelvic floor muscle training to prevent and treat incontinence after radical prostatectomy. Urol. Oncol. 2019. [Google Scholar] [CrossRef] [PubMed]
- Simon, R.M.; Howard, L.; Zapata, D.; Frank, J.; Freedland, S.J.; Vidal, A.C. The association of exercise with both erectile and sexual function in black and white men. J. Sex. Med. 2015, 12, 1202–1210. [Google Scholar] [CrossRef] [PubMed]
- Geraerts, I.; Van Poppel, H.; Devoogdt, N.; De Groef, A.; Fieuws, S.; Van Kampen, M. Pelvic floor muscle training for erectile dysfunction and climacturia 1 year after nerve sparing radical prostatectomy: A randomized controlled trial. Int. J. Impot. Res. 2016, 28, 9–13. [Google Scholar] [CrossRef] [PubMed]
- Brotto, L.A.; Heiman, J.R.; Goff, B.; Greer, B.; Lentz, G.M.; Swisher, E.; Van Blaricom, A. A psychoeducational intervention for sexual dysfunction in women with gynecologic cancer. Arch. Sex. Behav. 2008, 37, 317–329. [Google Scholar] [CrossRef] [PubMed]
- Lassen, B.; Gattinger, H.; Saxer, S. A systematic review of physical impairments following radical prostatectomy: Effect of psychoeducational interventions. J. Adv. Nurs. 2013, 69, 2602–2612. [Google Scholar] [CrossRef] [PubMed]
- Assalian, P. Psychological and interpersonal dimensions of sexual function and dysfunction. Arab J. Urol. 2013, 11, 217–221. [Google Scholar] [CrossRef] [PubMed]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).