Floor-to-Stand Transfers in Older Adults: Insights into Strategies and Lower Extremity Demands
Abstract
1. Introduction
2. Materials and Methods
2.1. Participant Selection and Consent
2.2. Study Procedures
2.2.1. Self-Report Measures
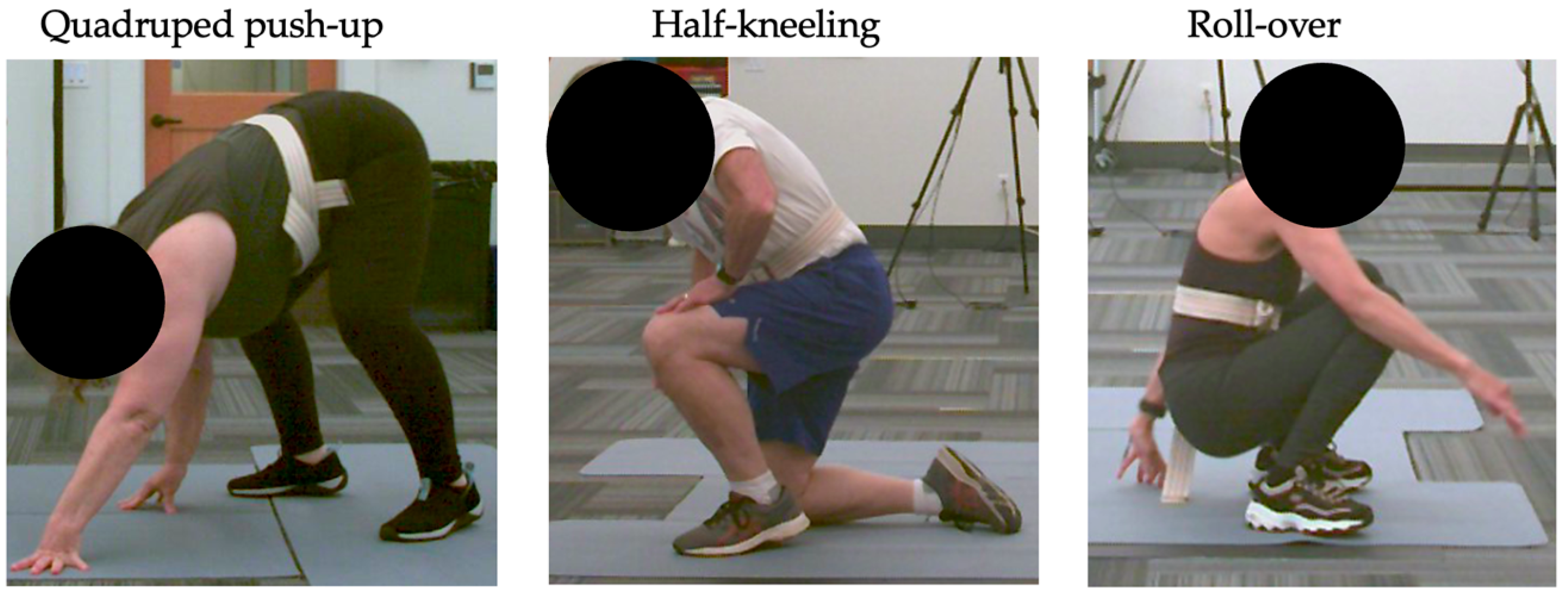
2.2.2. Study Activities
2.2.3. 5XSTS Task
2.2.4. Self-Selected FTS Task
2.2.5. Instructed FTS Task
2.3. Data Analysis
2.4. Statistical Analysis
3. Results
3.1. Participants and Study Activity Performance
3.2. Self-Selected FTS Time Correlations
3.3. Differences Between Participants Who Performed Various FTS Strategies
3.3.1. Self-Report Measures, Self-Selected FTS Time, and 5XSTS Performance
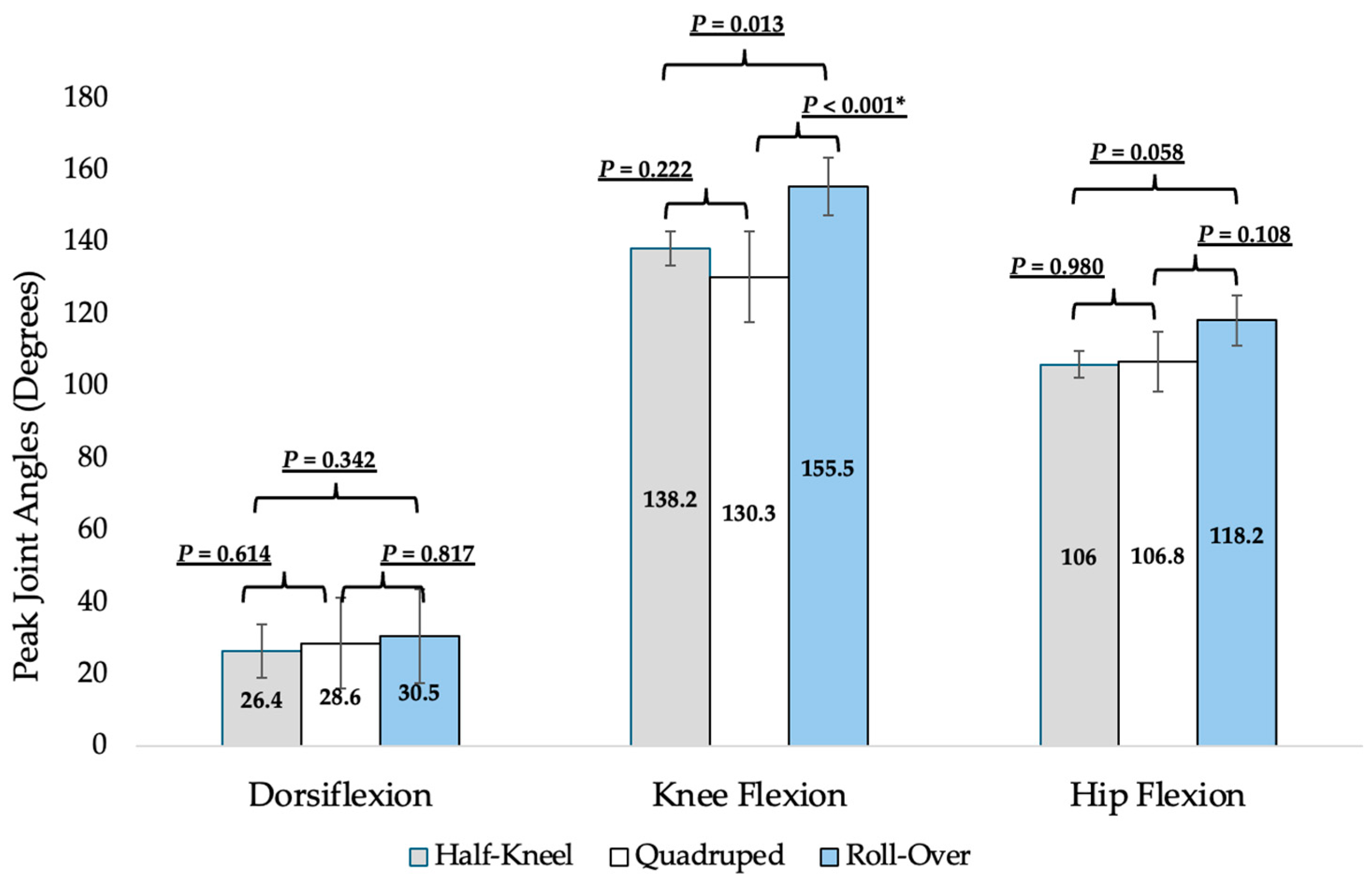
3.3.2. Joint Angles During Self-Selected FTS
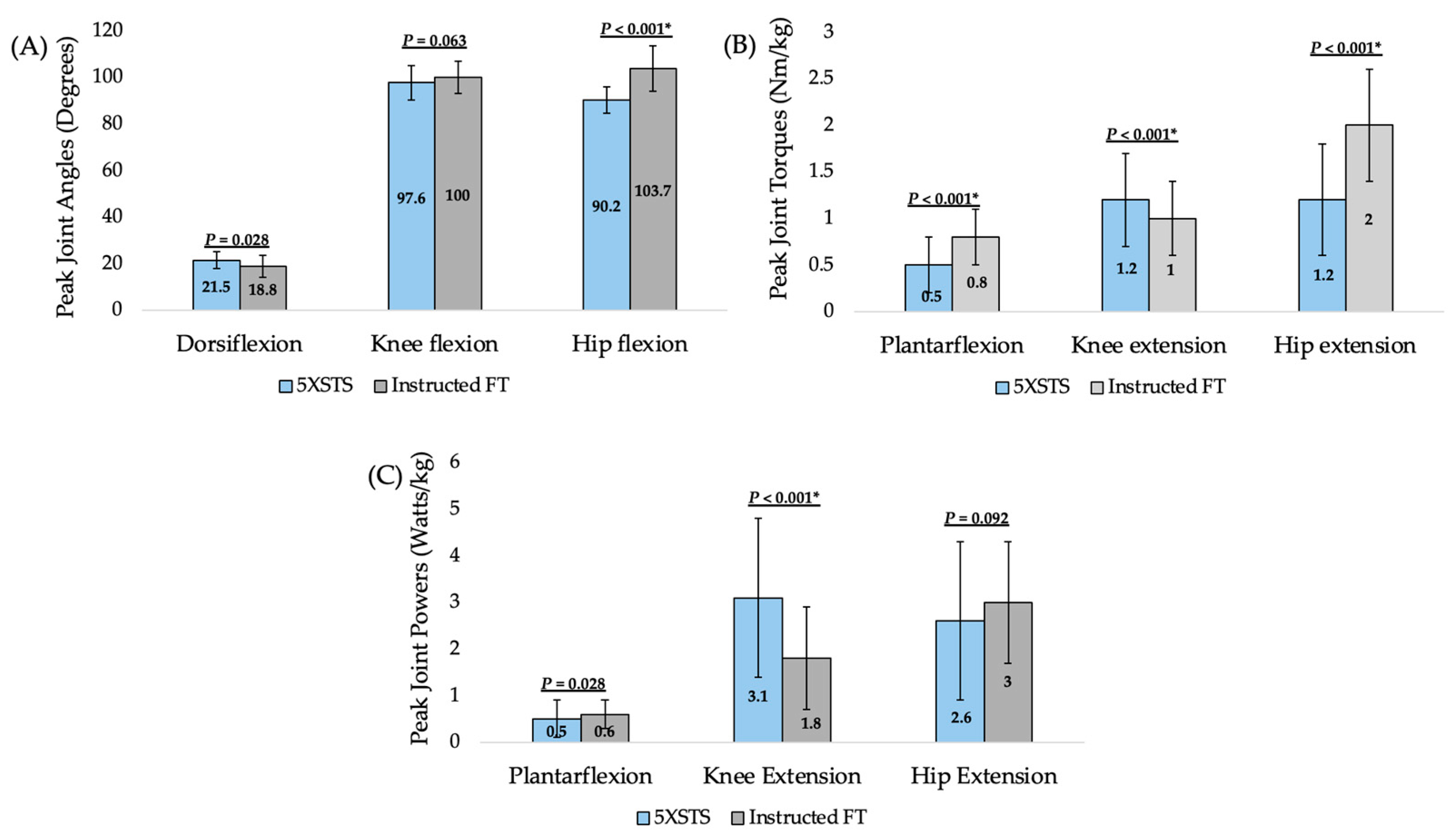
3.4. Lower Extremity Demands Between 5XSTS and Instructed FTS
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| FT | Floor transfer |
| 5XSTS | 5-time sit-to-stand |
| ANOVA | One-way analysis of variance |
| FES-I | Falls Efficacy Scale International |
| FoF | Fear of Falling |
| SE | Self-efficacy |
| PF | Physical function |
| SLUMS | Saint Louis University Mental Status Exam |
| PROMIS | Patient Reported Outcome Measurement Information System |
| RAPA | Rapid Assessment of Physical Activity |
| CAT | Computer Adaptive Testing |
References
- US Census Bureau. Older Americans Month: Data on Aging. Available online: https://www.census.gov/topics/population/older-aging/data.html (accessed on 9 September 2024).
- National Council on Aging. Nursing Homes Costs. Available online: https://www.ncoa.org/adviser/local-care/nursing-homes-costs/#:~:text=What%20is%20the%20cost%20of,2023%20Cost%20of%20Care%20Survey (accessed on 9 September 2024).
- Genworth Financial. Cost of Care Trends and Insights. Available online: https://www.genworth.com/aging-and-you/finances/cost-of-care/cost-of-care-trends-and-insights (accessed on 9 September 2024).
- Haddad, Y.K.; Miller, G.F.; Kakara, R.; Florence, C.; Bergen, G.; Burns, E.R.; Atherly, A. Healthcare spending for non-fatal falls among older adults, USA. Inj. Prev. 2024, 30, 272–276. [Google Scholar] [CrossRef]
- Ardali, G.; Brody, L.T.; States, R.A.; Godwin, E.M. Reliability and validity of the floor transfer test as a measure of readiness for independent living among older adults. J. Geriatr. Phys. Ther. 2019, 42, 136–147. [Google Scholar] [CrossRef] [PubMed]
- Ardali, G.; States, R.S.; Brody, L.T.; Godwin, E.M. Characteristics of older adults who are unable to perform a floor transfer: Considerations for clinical decision-making. J. Geriatr. Phys. Ther. 2020, 42, 62–70. [Google Scholar] [CrossRef] [PubMed]
- Bergland, A.; Laake, K. Concurrent and predictive validity of “getting up from lying on the floor”. Aging Clin. Exp. Res. 2005, 17, 181–185. [Google Scholar] [CrossRef] [PubMed]
- Murphy, M.A.; Olson, S.L.; Protas, E.J.; Overby, A.R. Screening for falls in community-dwelling elderly. J. Aging Phys. Act. 2003, 11, 66–80. [Google Scholar] [CrossRef][Green Version]
- Tinetti, M.E.; Liu, W.L.; Claus, E.B. Predictors and prognosis of inability to get up after falls among elderly persons. J. Am. Med. Assoc. 1993, 269, 65–70. [Google Scholar] [CrossRef]
- De Brito, L.B.B.; Ricardo, D.R.; de Araujo, D.S.M.S.; Ramos, P.S.; Myers, J.; de Araujo, C.G.S. Ability to sit and rise from the floor as a predictor of all-cause mortality. Euro. J. Prev. Cardiol. 2014, 21, 892–898. [Google Scholar] [CrossRef]
- Taulbee, L.; Trapuzzano, A.; Nguyen, T. Geriatric functional milestones: Promoting movement while aging. GeriNotes 2021, 28, 26–28. [Google Scholar]
- Alexander, N.B.; Ulbrich, J.; Raheja, A.; Channer, D. Rising from the floor in older adults. J. Am. Geriatr. Soc. 1997, 45, 564–569. [Google Scholar] [CrossRef]
- Ardali, G.; States, R.S.; Brody, L.T.; Godwin, E.M. The relationship between performance of sit-to-stand from a chair and getting down and up from the floor in community-dwelling older adults. Physiother. Theory Pract. 2022, 38, 818–829. [Google Scholar] [CrossRef]
- Bohannon, R.W.; Lusardi, M.M. Getting up from the floor: Determinants and techniques among healthy older adults. Physiother. Theory Pract. 2009, 20, 233–242. [Google Scholar] [CrossRef]
- Fleming, J. Inability to get up after falling, subsequent time on floor, and summoning help: Prospective cohort study in people over 90. BMJ 2008, 337, a2227. [Google Scholar] [CrossRef] [PubMed]
- Simpson, J.M.; Salkin, S. Are elderly people at risk of falling taught how to get up again? Age Ageing 1993, 22, 294–296. [Google Scholar] [CrossRef]
- Swancutt, D.R.; Hope, S.V.; Kent, B.P.; Robinson, M.; Goodwin, V.A. Knowledge, skills and attitudes of older people and staff about getting up from the floor following a fall: A qualitative investigation. BMC Geriatr. 2020, 20, 385. [Google Scholar] [CrossRef]
- Delbaere, K.; Close, J.; Mikolaizak, A.; Sachdev, P.; Brodaty, H.; Lord, S. The falls efficacy scale international (FES-I). A comprehensive longitudinal validation study. Age Ageing 2010, 39, 210–216. [Google Scholar] [CrossRef]
- Dewan, N.; MacDermid, J.C. Fall Efficacy Scale-International (FES-I). J. Physiother. 2014, 60, 60. [Google Scholar] [CrossRef]
- Hauer, K.; Yardley, L.; Beyer, N.; Kempen, G.; Dias, N.; Campbell, M.; Becker, C.; Todd, C. Validation of the Falls Efficacy Scale and Falls Efficacy Scale International in geriatric patients with and without cognitive impairment: Results of self-report and interview-based questionnaires. Gerontology 2010, 56, 190–199. [Google Scholar] [CrossRef]
- Hauer, K.A.; Kempen, G.M.; Schwenk, M.; Yardley, L.; Beyer, N.; Todd, C.; Oster, P.; Zijlstra, G.R. Validity and sensitivity to change of the falls efficacy scale international to assess fear of falling in older adults with and without cognitive impairment. Gerontology 2011, 57, 462–472. [Google Scholar] [CrossRef]
- Tinetti, M.E.; Richman, D.; Powell, L. Falls efficacy as a measure of fear of falling. J. Gerontol. 1990, 45, 239–243. [Google Scholar] [CrossRef] [PubMed]
- Yardley, L.; Beyer, N.; Hauer, K.; Kempen, G.; Piot-Ziegler, C.; Todd, C. Development and initial validation of the Falls Efficacy Scale-International (FES-I). Age Ageing 2005, 34, 614–619. [Google Scholar] [CrossRef] [PubMed]
- Samant, P.; Mohan, V.; Shyam, A.; Sancheti, P. Study of Relationship Between Fear of Falling & Ability to Sit On and Rise From the Floor in Elderly Population. Int. J. Physiother. Res. 2019, 7, 3181–3183. [Google Scholar] [CrossRef]
- Computer Adaptive Tests. HealthMeasures. Updated 31 July 2024. Available online: https://www.healthmeasures.net/index.php?option=com_content&view=category&layout=blog&id=164&Itemid=1133 (accessed on 30 October 2024).
- Gruber-Baldini, A.L.; Velozo, C.; Romero, S.; Shulman, L.M. Validation of the PROMIS® measures of self-efficacy for managing chronic conditions. Qual. Life Res. 2017, 26, 1915–1924. [Google Scholar] [CrossRef] [PubMed]
- Houck, J.; Kang, D.; Cuddeford, T. Do clinical criteria based on PROMIS outcomes identify acceptable symptoms and function for patients with musculoskeletal problems. Musculoskelet. Sci. Pract. 2021, 55, 102423. [Google Scholar] [CrossRef]
- Cook, K.F.; Jensen, S.E.; Schalet, B.D.; Beaumont, J.L.; Amtmann, D.; Czajkowski, S.; Dewalt, D.A.; Fries, J.F.; Pilkonis, P.A.; Reeve, B.B.; et al. PROMIS measures of pain, fatigue, negative affect, physical function, and social function demonstrated clinical validity across a range of chronic conditions. J. Clin. Epidemiol. 2016, 73, 89–102. [Google Scholar] [CrossRef] [PubMed]
- Deyo, R.A.; Katrina Ramsey Buckley, D.I.; Michaels, L.; Kobus, A.; Eckstrom, E.; Forro, V.; Morris, C. Performance of a patient reported outcomes measurement information system (PROMIS) short form in older adults with chronic musculoskeletal pain. Pain Med. 2016, 17, 314–324. [Google Scholar] [CrossRef]
- Bohannon, R.W. Measurement of sit-to-stand among older adults. Top. Geriatr. Rehabil. 2012, 28, 11–16. [Google Scholar] [CrossRef]
- Bohannon, R.W. Reference values for the five-repetition sit-to-stand test: A descriptive meta-analysis of data from elders. Percept. Mot. Ski. 2006, 103, 215–222. [Google Scholar] [CrossRef]
- Schaubert, K.L.; Bohannon, R.W. Reliability and validity of three strength measures obtained from community-dwelling elderly persons. J. Strength. Cond. Res. 2005, 19, 717–720. [Google Scholar] [CrossRef]
- Hofmeyer, M.R.; Neil, B.; Alexander, N.B.; Nyquist, L.V.; Medell, J.L.; Koreishi, A. Floor-rise strategy training in older adults. J. Am. Geriatr. Soc. 2002, 50, 1702–1706. [Google Scholar] [CrossRef]
- Klima, D.W.; Anderson, C.; Samrah, D.; Patel, D.; Chui, K.; Newton, R. Standing up from the floor in community-dwelling older adults. J. Aging Phys. Act. 2016, 24, 207–213. [Google Scholar] [CrossRef]
- Schwickert, L.; Oberle, C.; Becker, C.; Lindemann, U.; Klenk, J.; Schwenk, M.; Bourke, A.; Zijlstra, W. Model development to study strategies of younger and older adults getting up from the floor. Aging Clin. Exp. Res. 2016, 27, 277–287. [Google Scholar] [CrossRef] [PubMed]
- Tariq, S.H.; Tumosa, N.; Chibnall, J.T.; Perry, H.M., III; Morley, J.E. The Saint Louis University Mental Status (SLUMS) Examination for detecting mild cognitive impairment and dementia is more sensitive than the Mini Mental Status Examination (MMSE)—A pilot study. Am. J. Geriatr. Psych. 2006, 14, 900–910. [Google Scholar] [CrossRef]
- American Thoracic Society. ATS statement: Guidelines for the six-minute walk test. Am. J. Respir. Crit. Care Med. 2002, 166, 11–117. [Google Scholar] [CrossRef]
- Liguori, G.; Feito, Y.; Fountaine, C.; Roy, B. ACSM’s Guidelines for Exercise Testing and Prescription, 11th ed.; Wolters Kluwer: Philadelphia, PA, USA, 2022. [Google Scholar]
- Topolski, T.D.; LoGerfo, J.; Patrick, D.L.; Williams, B.; Patrick, M.A.J.M.B. The rapid assessment of physical activity (RAPA) among older adults. Prev. Chronic Dis. Public Health Res. Pract. Policy 2006, 3, A118. [Google Scholar]
- University of Washington Research Health Promotion Research Center. How Physically Active Are You? An Assessment of Level and Intensity of Physical Activity. Available online: http://depts.washington.edu/hprc/rapa (accessed on 1 November 2023).
- Intro to PROMIS. HealthMeasures. Updated 16 May 2024. Available online: https://www.healthmeasures.net/explore-measurement-systems/promis/intro-to-promis (accessed on 30 October 2024).
- General Self-Efficacy and Self-Efficacy for Managing Chronic Conditions. HealthMeasures. Updated 25 October 2017. Available online: https://www.healthmeasures.net/images/PROMIS/manuals/PROMIS_Self_Efficacy_Managing_Chronic_Conditions_Scoring_Manual.pdf (accessed on 30 October 2024).
- Physical Function. HealthMeasures. Updated 20 June 2020. Available online: https://www.healthmeasures.net/images/PROMIS/manuals/PROMIS_Physical_Function_Scoring_Manual.pdf (accessed on 30 October 2024).
- Cella, D.; Riley, W.; Stone, A.; Rothrock, N.; Reeve, B.; Yount, S.; Amtmann, D.; Bode, R.; Buysse, D.; Choi, S.; et al. The patient-reported outcomes measurement information system (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. J. Clin. Epidemiol. 2010, 63, 1179–1194. [Google Scholar] [CrossRef]
- Schalet, B.D.; Hays, R.D.; Jensen, S.E.; Beaumont, J.L.; Fries, J.F.; Cella, D. Validity of PROMIS physical function measured in diverse clinical samples. J. Clin. Epidemiol. 2016, 73, 112–118. [Google Scholar] [CrossRef]
- Broderick, J.E.; Schneider, S.; Junghaenel, D.U.; Schwartz, J.E.; Stone, A.A. Validity and reliability of patient-reported outcomes measurement information system instruments in osteoarthritis. Arthritis Care Res. 2013, 65, 1625–1633. [Google Scholar] [CrossRef]
- Cronin, N.J. Using deep neural networks for kinematic analysis: Challenges and opportunities. J. Biomech. 2021, 123, 110460. [Google Scholar] [CrossRef]
- Mathis, A.; Mamidanna, P.; Cury, K.M.; Abe, T.; Murthy, V.N.; Mathis, M.W.; Bethge, M. DeepLabCut: Markerless pose estimation of user-defined body parts with deep learning. Nat. Neurosci. 2018, 21, 1281. [Google Scholar] [CrossRef] [PubMed]
- Walker, J.; Thomas, A.; David, E.; Lunn, D.E.; Nicholson, G.; Tucker, C.B. Concurrent validity of Theia3D markerless motion capture for detecting sagittal kinematic differences between gait speeds. J. Sports Sci. 2025, 43, 1560–1571. [Google Scholar] [CrossRef]
- Kanko, R.M.; Laende, E.K.; Strutzenberger, G.; Brown, M.; Selbie, W.S.; DePaul, V.; Scott, S.H.; Deluzio, K. Assessment of spatiotemporal gait parameters using a deep learning algorithm-based markerless motion capture system. J. Biomech. 2021, 122, 110414. [Google Scholar] [CrossRef]
- Song, K.; Hullfish, T.J.; Silva, R.S.; Silbernagel, K.G.; Baxter, J.R. Markerless motion capture estimates of lower extremities and kinetics are comparable to marker-based across 8 movements. J. Biomech. 2023, 157, 111751. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.; Wei, L.; Huang, X.; Tu, L.; Xu, Y.; Li, X.; Hu, Z. Comparison of lower limb kinematic and kinetic estimation during athlete jumping between markerless and marker-based motion capture systems. Sci. Rep. 2025, 15, 18552. [Google Scholar] [CrossRef] [PubMed]
- Kanko, R.M.; Laende, E.; Selbie, W.S.; Deluzio, K.J. Inter-session repeatability of markerless motion capture gait kinetics. J. Biomech. 2021, 121, 110422. [Google Scholar] [CrossRef] [PubMed]
- Kanko, R.M.; Laende, E.K.; Davis, E.M.; Selbie, W.S.; Deluzio, K.J. Concurrent assessment of gait kinematics using marker-based and markerless motion capture. J. Biomech. 2021, 127, 110665. [Google Scholar] [CrossRef]
| Characteristics | Mean (SD) |
|---|---|
| Age (years) | 69.1 (8.8) |
| Mass (kg) | 74.4 (15.3) |
| Height (cm) | 168.4 (11.4) |
| BMI (kg/m2) | 25.7 (4.22) |
| SLUMS Score | 27.1 (0.1) |
| FES-I Score | 18.1 (2.0) |
| PROMIS SE T-score | 54.2 (4.9) |
| PROMIS PF T-score | 53.7 (6.5) |
| RAPA 1 score: Aerobic | 6.2 (0.8) |
| RAPA 2 score: Strength and Flexibility | 2.2 (1.1) |
| 5XSTS time (seconds) | 9.6 (1.7) |
| Self-selected FTS time (seconds) | 4.7 (2.1) |
| Self-Report and 5XSTS Performance Measures | Correlation to FT Time |
|---|---|
| Age (years) | r = 0.52, p = 0.002 * |
| PROMIS SE (T-score) | r = −0.27, p = 0.125 |
| PROMIS PF (T-score) | r = −0.33, p = 0.060 |
| FES-I Score | r = 0.19, p = 0.271 |
| 5XSTS time (seconds) | r = 0.56, p < 0.001 * |
| 5XSTS ankle plantar flexion torque (Nm/kg) | r = −0.08, p = 0.676 |
| 5XSTS ankle plantar flexion power (W/kg) | r = −0.30, p = 0.098 |
| 5XSTS knee extension torque (Nm/kg) | r = −0.27, p = 0.139 |
| 5XSTS knee extension power (W/kg) | r = −0.46, p = 0.009 |
| 5XSTS hip extension torque (Nm/kg) | r = −0.30, p = 0.095 |
| 5XSTS hip extension power (W/kg) | r = −0.35, p = 0.050 |
| Half-Kneel | Quadruped | Roll-Over | |
|---|---|---|---|
| Self-Report Measures | |||
| PROMIS Self-Efficacy in Daily Activities (T-score) | 56.02 (5.40) | 51.84 (3.90) | 53.20 (2.82) |
| PROMIS Physical Function (T-score) | 53.62 (7.32) | 51.38 (5.37) | 57.98 (4.29) |
| FES-I score | 17.47 (1.33) | 19.36 (2.50) | 17.33 (1.37) |
| Physical Measures | |||
| FTS time (seconds) | 4.04 (1.35) | 6.26 (2.13) | 3.68 (2.70) |
| 5XSTS time (seconds) | 9.29 (1.48) | 10.36 (1.44) | 9.36 (2.46) |
| 5XSTS peak ankle plantar flexion torque (Nm/kg) | 0.52 (0.32) | 0.49 (0.18) | 0.49 (0.30) |
| 5XSTS peak ankle plantar flexion power (W/kg) | 0.50 (0.31) | 0.45 (0.29) | 0.74 (0.67) |
| 5XSTS peak knee extension torque (Nm/kg) | 1.31 (0.52) | 1.10 (0.33) | 1.26 (0.55) |
| 5XSTS peak knee extension power (W/kg) | 3.47 (2.04) | 2.42 (0.81) | 3.12 (1.24) |
| 5XSTS peak hip extension torque (Nm/kg) | 1.17 (0.66) | 1.13 (0.52) | 1.20 (0.64) |
| 5XSTS peak hip extension power (W/kg) | 2.61 (1.69) | 2.38 (1.50) | 2.72 (1.63) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stutzenberger, L.; Whited, T. Floor-to-Stand Transfers in Older Adults: Insights into Strategies and Lower Extremity Demands. Geriatrics 2025, 10, 119. https://doi.org/10.3390/geriatrics10050119
Stutzenberger L, Whited T. Floor-to-Stand Transfers in Older Adults: Insights into Strategies and Lower Extremity Demands. Geriatrics. 2025; 10(5):119. https://doi.org/10.3390/geriatrics10050119
Chicago/Turabian StyleStutzenberger, Lyndsay, and Tyler Whited. 2025. "Floor-to-Stand Transfers in Older Adults: Insights into Strategies and Lower Extremity Demands" Geriatrics 10, no. 5: 119. https://doi.org/10.3390/geriatrics10050119
APA StyleStutzenberger, L., & Whited, T. (2025). Floor-to-Stand Transfers in Older Adults: Insights into Strategies and Lower Extremity Demands. Geriatrics, 10(5), 119. https://doi.org/10.3390/geriatrics10050119






