Home Caregivers of Elderly People: Perceptions and Quality of Life
Abstract
1. Introduction
2. Methodology
2.1. Study Design and Sample Selection
2.2. Study Location
2.3. Research Ethics
2.4. Data Collection
2.5. Discourse of the Collective Subject (DCS)
2.6. Health-Related Quality of Life Measured with EQ-5D
2.7. Health State Valuation
2.8. Data Analysis
3. Results
3.1. Sociodemographic Profile and Caregiving Experience
3.2. Emerging Themes from Interviews on Home Care
“It is a routine to see the health center professionals here every week; they rarely miss a visit” (P. 121), or also, “The health center professionals always show up every Thursday” (P. 08).
“It is a relief to have them around; they always offer help when we need it. I remember a time when my father fell and injured his leg; the nurse came here to dress his wounds” (P. 37). Another patient added: “Their presence at home is very important because my mother cannot walk to the health center since she is bedridden” (P. 42).
“They are very polite, always treating us with kindness” (P. 09), or “Sometimes, they seem like part of the family; I can even send a message on WhatsApp, and the nurse is always there to help” (P. 11).
“It’s been a while since I’ve known what it’s like to go out and have fun, I have to stay the whole time taking care of him” (P. 15), “My friends invite me to go out, but with my father bedridden like this, it’s impossible” (P. 13), another participant even stated: “Look, I want to go out, travel, you know? But with my mother like this, it’s just not possible… I’m the only one left to take care of her” (P. 126).
“I can’t sleep more than three hours in a row, I always have to get my mother up to go to the bathroom, and when it’s not that, it’s the medication that I can’t neglect” (P.132), “It’s been a long time since I’ve known what rest is, I even have dark circles under my eyes, but what can I do, right?” (P. 87). Regarding the pain, the patients said: “My arm hurts a lot, but it’s because of his weight, right? I need to bathe him, change him … and he can’t support himself on anything” (P. 75), “…I live on painkillers because of the pain here” (patient pointing to their forearm) (P. 23).
3.3. Analysis of Health-Related Quality of Life
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bloom, D.E.; Luca, D.L. The global demography of aging: Facts, explanations, future. In Handbook of the Economics of Population Aging; North-Holland: Amsterdam, The Netherlands, 2016. [Google Scholar]
- Wool, E.; Shotwell, J.L.; Slaboda, J.; Kozikowski, A.; Smith, K.L.; Abrashkin, K.; Rhodes, K.V.; Norman, G.J.; Pekmezaris, R. A Qualitative Investigation of the Impact of Home-Based Primary Care on Family Caregivers. J. Frailty Aging 2019, 8, 210–214. [Google Scholar] [CrossRef]
- Mosquera, I.; Vergara, I.; Larrañaga, I.; Machón, M.; del Río, M.; Calderón, C. Measuring the impact of informal elderly caregiving: A systematic review of tools. Qual. Life Res. 2015, 25, 1059–1092. [Google Scholar] [CrossRef] [PubMed]
- Donnellan, W.J.; Bennett, K.M.; Soulsby, L.K. What are the factors that facilitate or hinder resilience in older spousal dementia carers? A qualitative study. Aging Ment. Health 2014, 19, 932–939. [Google Scholar] [CrossRef]
- Stall, N.; Nowaczynski, M.; Sinha, S.K. Systematic Review of Outcomes from Home-Based Primary Care Programs for Homebound Older Adults. J. Am. Geriatr. Soc. 2014, 62, 2243–2251. [Google Scholar] [CrossRef] [PubMed]
- Shafir, A.; Garrigues, S.K.; Schenker, Y.; Leff, B.; Neil, J.; Ritchie, C. Homebound Patient and Caregiver Perceptions of Quality of Care in Home-Based Primary Care: A Qualitative Study. J. Am. Geriatr. Soc. 2016, 64, 1622–1627. [Google Scholar] [CrossRef]
- Bekdemir, A.; Ilhan, N. Predictors of caregiver burden in caregivers of bedridden patients. J. Nurs. Res. 2019, 27, e24. [Google Scholar] [CrossRef]
- Ohara, Y.; Iwasaki, M.; Motokawa, K.; Hirano, H. Preliminary investigation of family caregiver burden and oral care provided to homebound older patients. Clin. Exp. Dent. Res. 2021, 7, 840–844. [Google Scholar] [CrossRef] [PubMed]
- Schulz, R.; Beach, S.R. Caregiving as a Risk Factor for Mortality. JAMA 1999, 282, 2215–2219. [Google Scholar] [CrossRef]
- Yang, S.-Y.; Fu, S.H.; Hsieh, P.L.; Lin, Y.L.; Chen, M.C.; Lin, P.H. Improving the care stress, life quality, and family functions for family-caregiver in long-term care by home modification. Ind. Health 2022, 60, 485–497. [Google Scholar] [CrossRef]
- Omiya, T.; Kutsumi, M.; Fukui, S. Work, Leisure Time Activities, and Mental Health among Family Caregivers of the Elder People in Japan. Healthcare 2021, 9, 129. [Google Scholar] [CrossRef]
- Mandani, B.; Hosseini, S.A.; Hosseini, M.A.; Noori, A.K.; Ardakani, M.R.K. Perception of family caregivers about barriers of leisure in care of individuals with chronic psychiatric disorders: A qualitative study. Electron. Physician 2018, 10, 6516–6526. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.; Kaur, H. Barrier Free Environment and Universal Design: Approaches to Enhance the Functioning of People at Old Age; Book Age: New Delhi, India, 2015; p. 391. [Google Scholar]
- Rajão, F.L.; Martins, M. Atenção Domiciliar no Brasil: Estudo exploratório sobre a consolidação e uso de serviços no Sistema Único de Saúde. Cien Saude Colet. 2020, 25, 1863–1877. [Google Scholar] [CrossRef]
- Wachs, L.S.; Nunes, B.P.; Soares, M.U.; Facchini, L.A.; Thumé, E. Prevalência da assistência domiciliar prestada à população idosa brasileira e fatores associados. Cad. Saude Publica 2016, 32, e00048515. [Google Scholar] [CrossRef] [PubMed]
- Lefèvre, F.; Lefèvre, A.M.C.; Teixeira, J.J.V. O Discurso do Sujeito Coletivo: Uma Nova Abordagem Metodológica em Pesquisa Qualitativa; Educs: Caxias do Sul, Brazil, 2000. [Google Scholar]
- Lefèvre, F.; Lefèvre, A.M.C. Pesquisa de Representação Social: Um Enfoque Qualiquantitativo, 2nd ed.; Liber Livro Editora: Brasília, Brazil, 2012. [Google Scholar]
- Genaro, L.E.; Marconato, J.V.; Tagliaferro, E.P.D.S.; Pinotti, F.E.; Valsecki Júnior, A.; Adas Saliba, T.; Rosell, F.L. Home Care for the Elderly: An Integrated Approach to Perception, Quality of Life, and Cognition. Int. J. Environ. Res. Public Health 2024, 21, 539. [Google Scholar] [CrossRef] [PubMed]
- The EuroQol Group. EuroQol—A new facility for the measurement of health-related quality of life. Health Policy 1990, 16, 199–208. [Google Scholar] [CrossRef]
- Devlin, N.J.; Brooks, R. EQ-5D and the EuroQol Group: Past, Present and Future. Appl. Health Econ. Health Policy 2017, 15, 127–137. [Google Scholar] [CrossRef]
- Santos, M.; Cintra, M.A.C.T.; Monteiro, A.L. Brazilian Valuation of EQ-5D-3L Health States: Results from a Saturation Study. Med. Decis. Making 2015, 36, 253–263. [Google Scholar] [CrossRef]
- Cassidy, T.; McLaughlin, M. Psychological distress of female caregivers of significant others with cancer. Cogent Psychol. 2015, 2, 999405. [Google Scholar] [CrossRef]
- Haley, W.E.; LaMonde, L.A.; Han, B.; Narramore, S.; Schonwetter, R. Family Caregiving in Hospice: Effects on Psychological and Health Functioning Among Spousal Caregivers of Hospice Patients with Lung Cancer or Dementia. Hosp. J. 2000, 15, 1–18. [Google Scholar] [CrossRef]
- Williams, A.L.; McCorkle, R. Cancer family caregivers during the palliative, hospice, and bereavement phases: A review of the descriptive psychosocial literature. Palliat. Support. Care 2011, 9, 315–325. [Google Scholar] [CrossRef]
- Barbosa, L.C.; Garbin, C.A.S.; Moimaz, S.A.S.; Saliba, T.A. Cuidadores domiciliares de idosos: Qualidade de vida e práticas no processo de cuidar. Estud. Interdiscipl. Envelhec. 2021, 26, 291–313. [Google Scholar]
- Ascef, B.D.O.; Haddad, J.P.A.; Álvares, J.; Guerra Junior, A.A.; Costa, E.A.; Acurcio, F.D.A.; Silveira, M.R. Qualidade de vida relacionada à saúde dos usuários da atenção primária no Brasil. Rev. Saude Publica 2017, 51, 22s. [Google Scholar] [CrossRef] [PubMed]
- N’Goran, A.A.; Déruaz-Luyet, A.; Haller, D.M.; Zeller, A.; Rosemann, T.; Streit, S.; Herzig, L. Comparing the self-perceived quality of life of multimorbid patients and the general population using the EQ-5D-3L. PLoS ONE 2017, 12, e0188499. [Google Scholar] [CrossRef] [PubMed]
- dos Reis, E.; Dourado, V.Z.; Guerra, R.L.F. Qualidade de vida e fatores de riscos à saúde de cuidadoras formais de idosos. Estud. Interdiscip. Envelhec. 2019, 24. [Google Scholar] [CrossRef]
- Schulz, R.; Sherwood, P.R. Physical and mental health effects of family caregiving. J. Soc. Work Educ. 2008, 44, 105–113. [Google Scholar] [CrossRef]
- Carnemolla, P.; Bridge, C. A scoping review of home modification interventions—Mapping the evidence base. Indoor Built Environ. 2020, 29, 299–310. [Google Scholar] [CrossRef]
- Sambasivam, R.; Liu, J.; Vaingankar, J.A.; Ong, H.L.; Tan, M.E.; Fauziana, R.; Picco, L.; Chong, S.A.; Subramaniam, M. The hidden patient: Chronic physical morbidity, psychological distress, and quality of life in caregivers of older adults. Psychogeriatrics 2019, 19, 65–72. [Google Scholar] [CrossRef]
- Shaffer, K.M.; Kim, Y.; Carver, C.S.; Cannady, R.S. Effects of caregiving status and changes in depressive symptoms on development of physical morbidity among long-term cancer caregivers. Health Psychol. 2017, 36, 770. [Google Scholar] [CrossRef]
- Adelman, R.D.; Tmanova, L.L.; Delgado, D.; Dion, S.; Lachs, M.S. Caregiver burden: A clinical review. JAMA 2014, 311, 1052–1060. [Google Scholar] [CrossRef]
- Geng, H.M.; Chuang, D.M.; Yang, F.; Yang, Y.; Liu, W.M.; Liu, L.H.; Tian, H.M. Prevalence and determinants of depression in caregivers of cancer patients: A systematic review and meta-analysis. Medicine 2018, 97, e11863. [Google Scholar] [CrossRef]
- Fletcher, B.A. Symptom experience of family caregivers of patients with cancer. Oncol. Nurs. Forum 2008, 35, E23–E44. [Google Scholar] [CrossRef] [PubMed]
- Washington, K.T.; Oliver, D.P.; Smith, J.B.; McCrae, C.S.; Balchandani, S.M.; Demiris, G. Sleep problems, anxiety, and global self-rated health among hospice family caregivers. Am. J. Hosp. Palliat. Med. 2018, 35, 244–249. [Google Scholar] [CrossRef] [PubMed]
- Oechsle, K.; Ullrich, A.; Marx, G.; Benze, G.; Wowretzko, F.; Zhang, Y.; Dickel, L.M.; Heine, J.; Wendt, K.N.; Nauck, F.; et al. Prevalence and predictors of distress, anxiety, depression, and quality of life in bereaved family caregivers of patients with advanced cancer. Am. J. Hosp. Palliat. Care 2020, 37, 201–213. [Google Scholar] [CrossRef]
- Grand, J.H.; Caspar, S.; Macdonald, S.W. Clinical features and multidisciplinary approaches to dementia care. J. Multidiscip. Healthc. 2011, 4, 125–147. [Google Scholar]
- Vostrý, M.; Lanková, B.; Pešatová, I.; Fleischmann, O.; Jelínková, J. Nonpharmacological Compensation of Aggressive Behavior of Individuals with Moderate Intellectual Disability and Behavioral Disorders—A Case Study. Int. J. Environ. Res. Public Health 2022, 19, 9116. [Google Scholar] [CrossRef]
- de Araújo Reis, L.; de Souza Rocha, T.; Duarte, S.F.P. Quedas: Risco e fatores associados em idosos institucionalizados. Rev. Baiana Enferm. 2014, 28. [Google Scholar]
- Cott, C.A.; Tierney, M.C. Acceptable and unacceptable risk: Balancing everyday risk by family members of older cognitively impaired adults who live alone. Health Risk Soc. 2013, 15, 402–415. [Google Scholar] [CrossRef]
- Car, L.T.; El-Khatib, M.; Perneczky, R.; Papachristou, N.; Atun, R.; Rudan, I.; Car, J.; Vincent, C.; Majeed, A. Prioritizing problems in and solutions to homecare safety of people with dementia: Supporting carers, streamlining care. BMC Geriatr. 2017, 17, 26. [Google Scholar]
- Häikiö, K.; Sagbakken, M.; Rugkåsa, J. Dementia and patient safety in the community: A qualitative study of family carers’ protective practices and implications for services. BMC Health Serv. Res. 2019, 19, 635. [Google Scholar] [CrossRef]
- Hung, L.; Hudson, A.; Gregorio, M.; Jackson, L.; Mann, J.; Horne, N.; Berndt, A.; Wallsworth, C.; Wong, L.; Phinney, A. Creating Dementia-Friendly Communities for Social Inclusion: A Scoping Review. Gerontol. Geriatr. Med. 2021, 7, 23337214211013596. [Google Scholar] [CrossRef]
- Seng, B.K.; Luo, N.; Ng, W.Y.; Lim, J.; Chionh, H.L.; Goh, J.; Yap, P. Validity and reliability of the Zarit Burden Interview in assessing caregiving burden. Ann. Acad. Med. Singap. 2010, 39, 758–763. [Google Scholar] [CrossRef] [PubMed]
- Carod-Artal, F.J.; Mesquita, H.M.; Ziomkowski, S.; Martinez-Martin, P. Burden and health-related quality of life among caregivers of Brazilian Parkinson’s disease patients. Park. Relat. Disord. 2013, 19, 943–948. [Google Scholar] [CrossRef] [PubMed]
| Variables | n | % | |
|---|---|---|---|
| Gender | |||
| Masculine | 11 | 7.97 | |
| Feminine | 127 | 92.03 | |
| Age range (years) | |||
| 18–25 years | 6 | 4.35 | |
| 26–30 years | 15 | 10.87 | |
| 31–35 years | 22 | 15.94 | |
| 40–50 years | 27 | 19.57 | |
| >50 years | 68 | 49.28 | |
| Ethnicity/color | |||
| White | 78 | 56.52 | |
| Black | 39 | 28.26 | |
| Brown | 21 | 15.22 | |
| Relationship with the patient | |||
| None | 35 | 25.36 | |
| Spouse | 17 | 12.32 | |
| Children | 62 | 44.93 | |
| Grandchildren | 13 | 9.42 | |
| Mother/Father | 11 | 7.97 | |
| Working time as a caregiver | |||
| 1–12 months | 14 | 10.14 | |
| 13–24 months | 38 | 27.54 | |
| 25–36 months | 22 | 15.94 | |
| 37–48 months | 16 | 11.59 | |
| >50 months | 48 | 34.78 |
| Theme | Definition |
|---|---|
| Frequency and regularity of home visits | Reports on the consistent and weekly presence of healthcare professionals at the home, indicating a continuous pattern of care. |
| Importance of home care for treatment continuity | Caregivers’ perception of the positive impact of home visits on maintaining the patient’s health and addressing emergencies. |
| Emotional bond with healthcare professionals | Descriptions of the politeness, empathy, and emotional closeness of professionals with caregivers and patients, often compared to family members. |
| Feeling of loneliness and social isolation | Expressions of emotional distress due to a lack of social life, restricted freedom, and the burden of exclusive dedication to caregiving. |
| Physical and emotional overload | Reports of physical and psychological exhaustion related to the caregiving routine, sleep disruptions, muscular pain, and lack of adequate rest. |
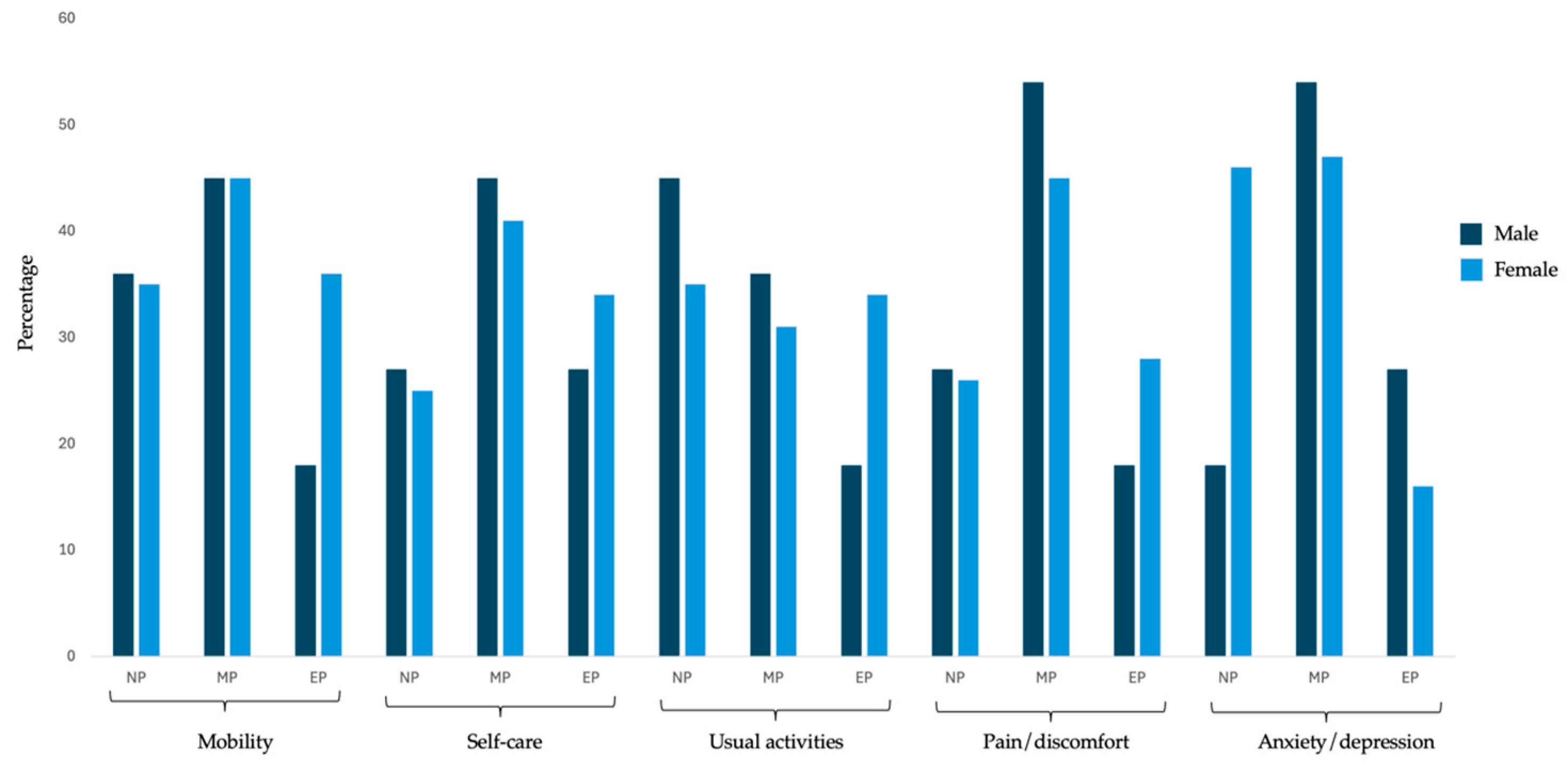
| EQ-5D Dimension | Gender | |||
|---|---|---|---|---|
| Male n (%) | Female n (%) | p | ||
| Mobility | No problem | 4 (36.36%) | 38 (34.86%) | 0.66 |
| Moderate problems | 5 (45.45%) | 49 (45.41%) | 0.72 | |
| Extreme problems | 2 (18.18%) | 40 (36.73%) | 0.03 * | |
| Self-care | No problem | 3 (27.27%) | 32 (25.20%) | 0.52 |
| Moderate problems | 5 (45.45%) | 52 (40.95%) | 0.08 | |
| Extreme problems | 3 (27.27%) | 43 (33.86%) | 0.05 | |
| Usual activities | No problem | 5 (45.45%) | 45 (35.43%) | 0.05 |
| Moderate problems | 4 (36.36%) | 39 (30.71%) | 0.06 | |
| Extreme problems | 2 (18.18%) | 43 (33.86%) | <0.001 * | |
| Pain/discomfort | No problem | 3 (27.27%) | 33 (25.98%) | 0.05 |
| Moderate problems | 6 (54.55%) | 58 (45.67%) | 0.04 * | |
| Extreme problems | 2 (18.18%) | 36 (28.35%) | 0.02 * | |
| Anxiety/depression | No problem | 2 (18.18%) | 46 (36.22%) | 0.02 * |
| Moderate problems | 6 (54.55%) | 60 (47.24%) | 0.06 | |
| Extreme problems | 3 (27.27%) | 21 (16.54%) | 0.03 * | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Genaro, L.E.; Marconato, J.V.; Valsecki Júnior, A.; Adas Saliba, T.; Rosell, F.L. Home Caregivers of Elderly People: Perceptions and Quality of Life. Geriatrics 2025, 10, 61. https://doi.org/10.3390/geriatrics10030061
Genaro LE, Marconato JV, Valsecki Júnior A, Adas Saliba T, Rosell FL. Home Caregivers of Elderly People: Perceptions and Quality of Life. Geriatrics. 2025; 10(3):61. https://doi.org/10.3390/geriatrics10030061
Chicago/Turabian StyleGenaro, Luís Eduardo, José Victor Marconato, Aylton Valsecki Júnior, Tânia Adas Saliba, and Fernanda Lopez Rosell. 2025. "Home Caregivers of Elderly People: Perceptions and Quality of Life" Geriatrics 10, no. 3: 61. https://doi.org/10.3390/geriatrics10030061
APA StyleGenaro, L. E., Marconato, J. V., Valsecki Júnior, A., Adas Saliba, T., & Rosell, F. L. (2025). Home Caregivers of Elderly People: Perceptions and Quality of Life. Geriatrics, 10(3), 61. https://doi.org/10.3390/geriatrics10030061






