Successful Treatment of Vertebral Osteosarcoma in a Cat Using Marginal Surgical Excision and Chemotherapy
Abstract
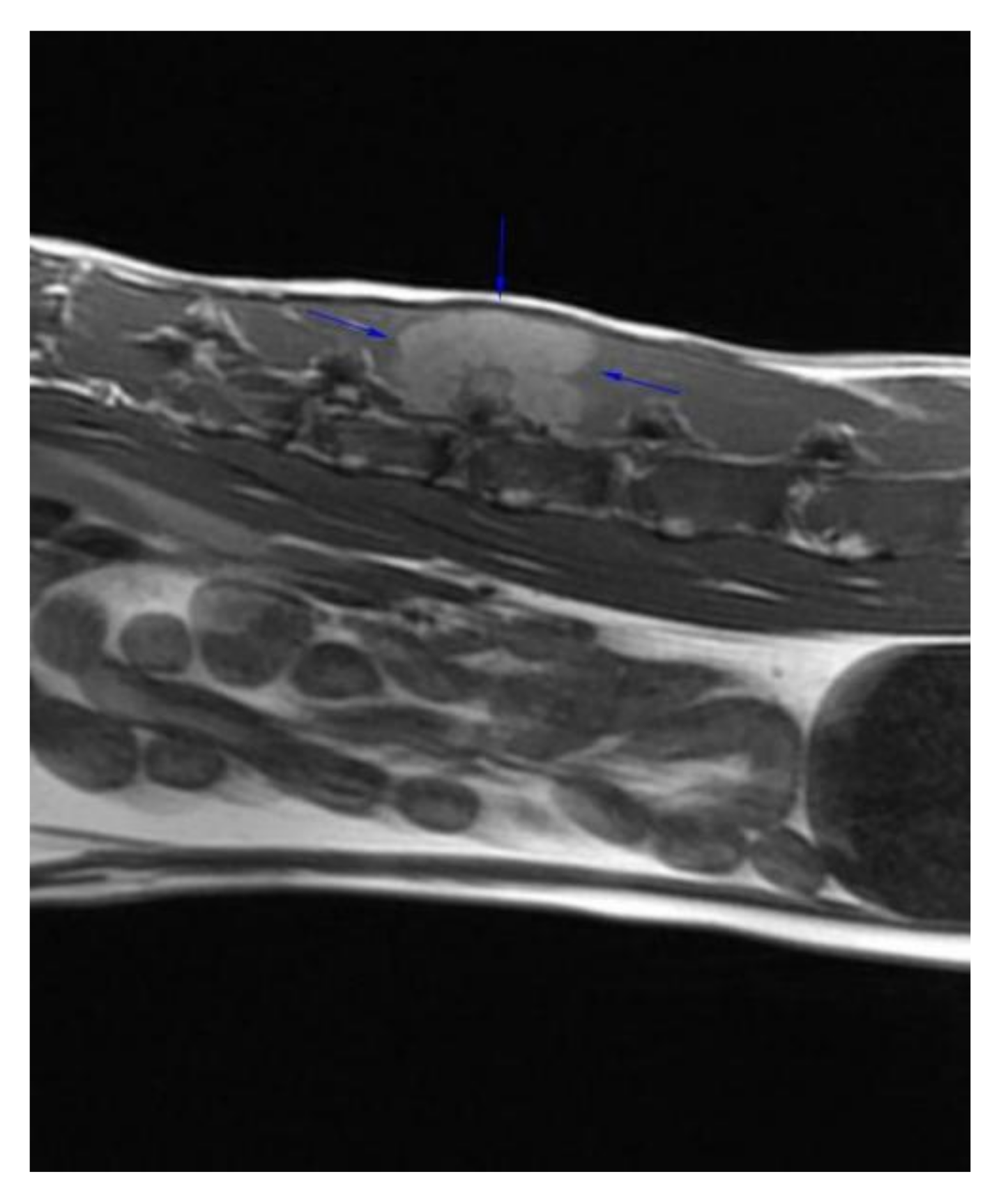
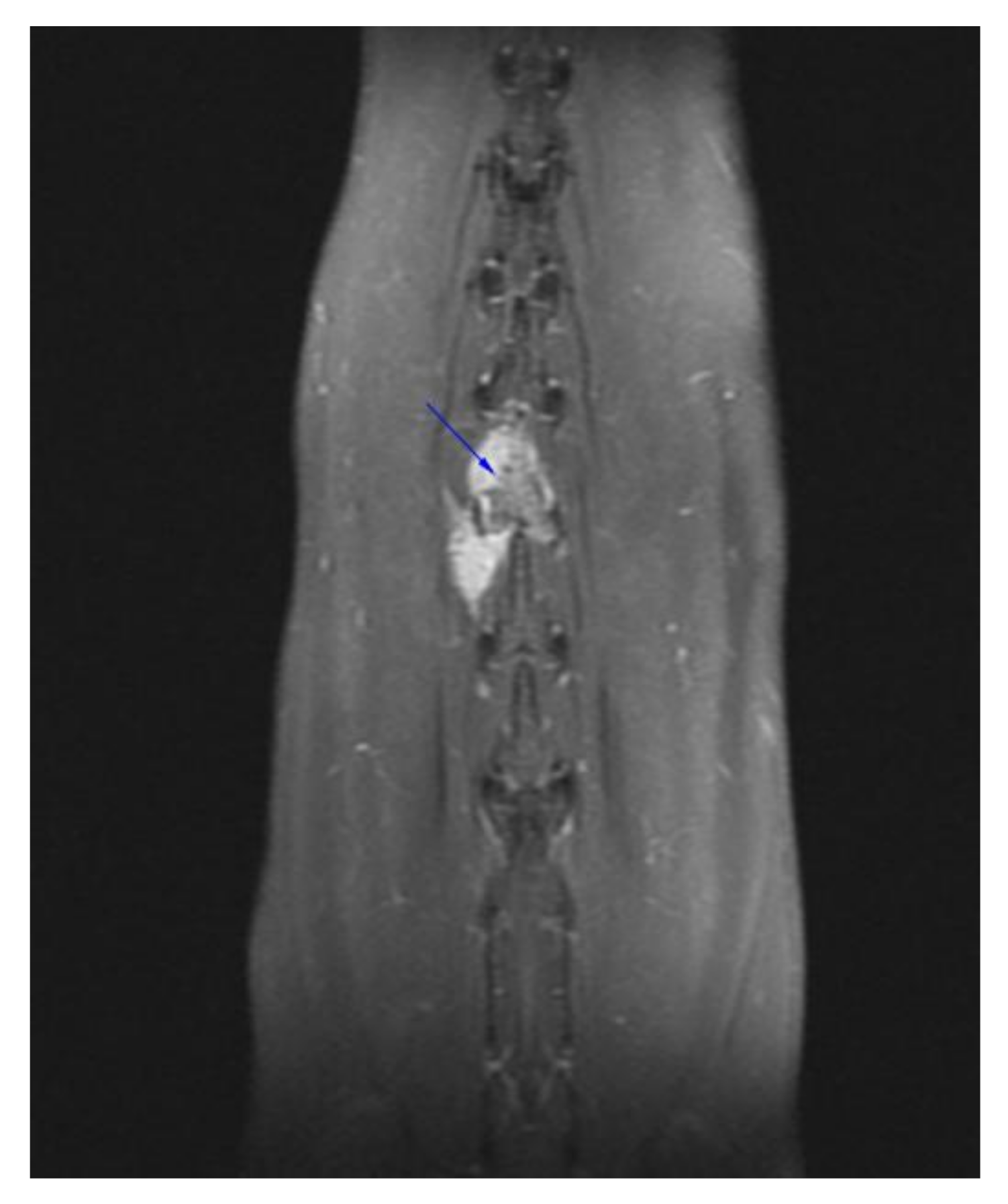
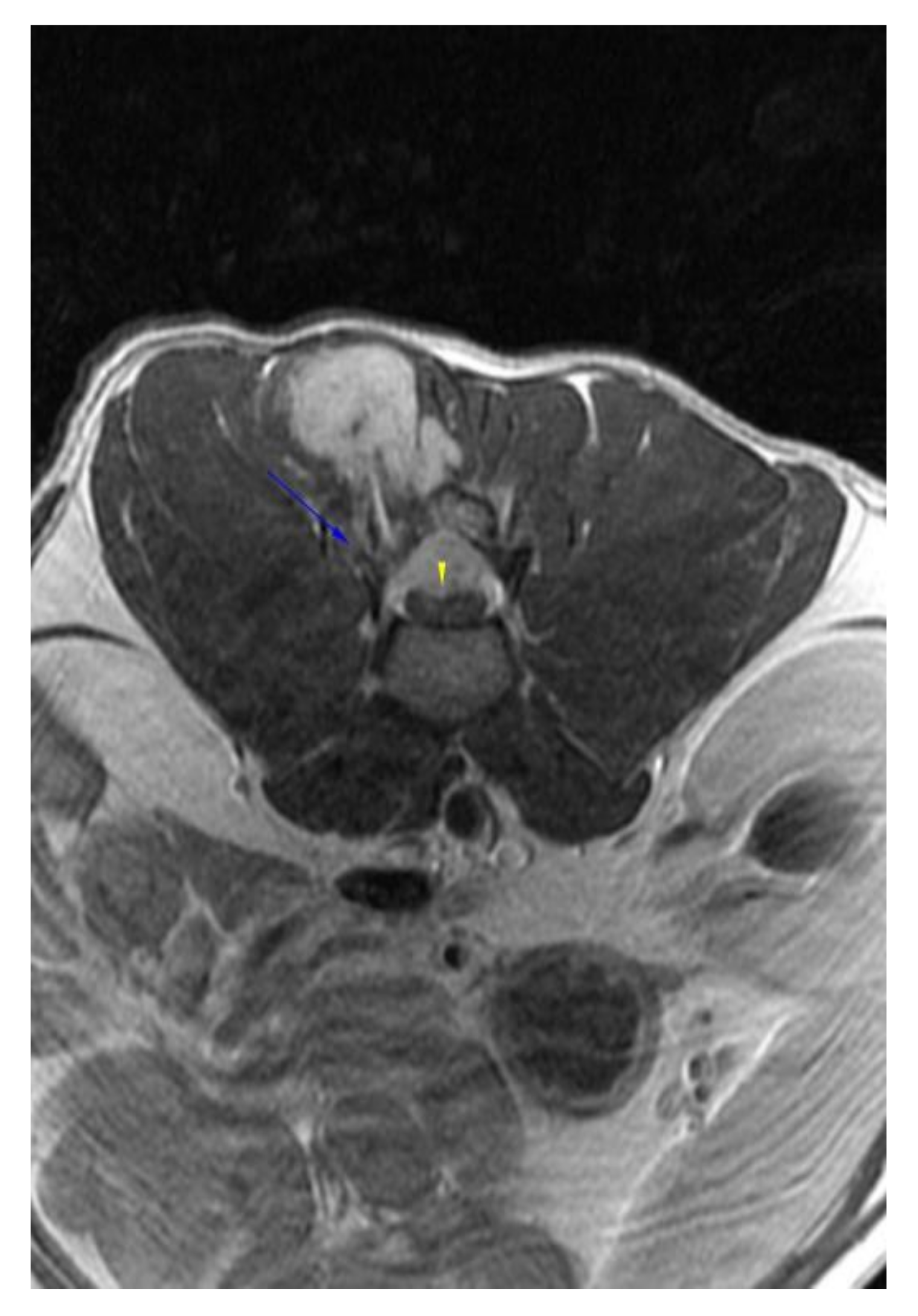
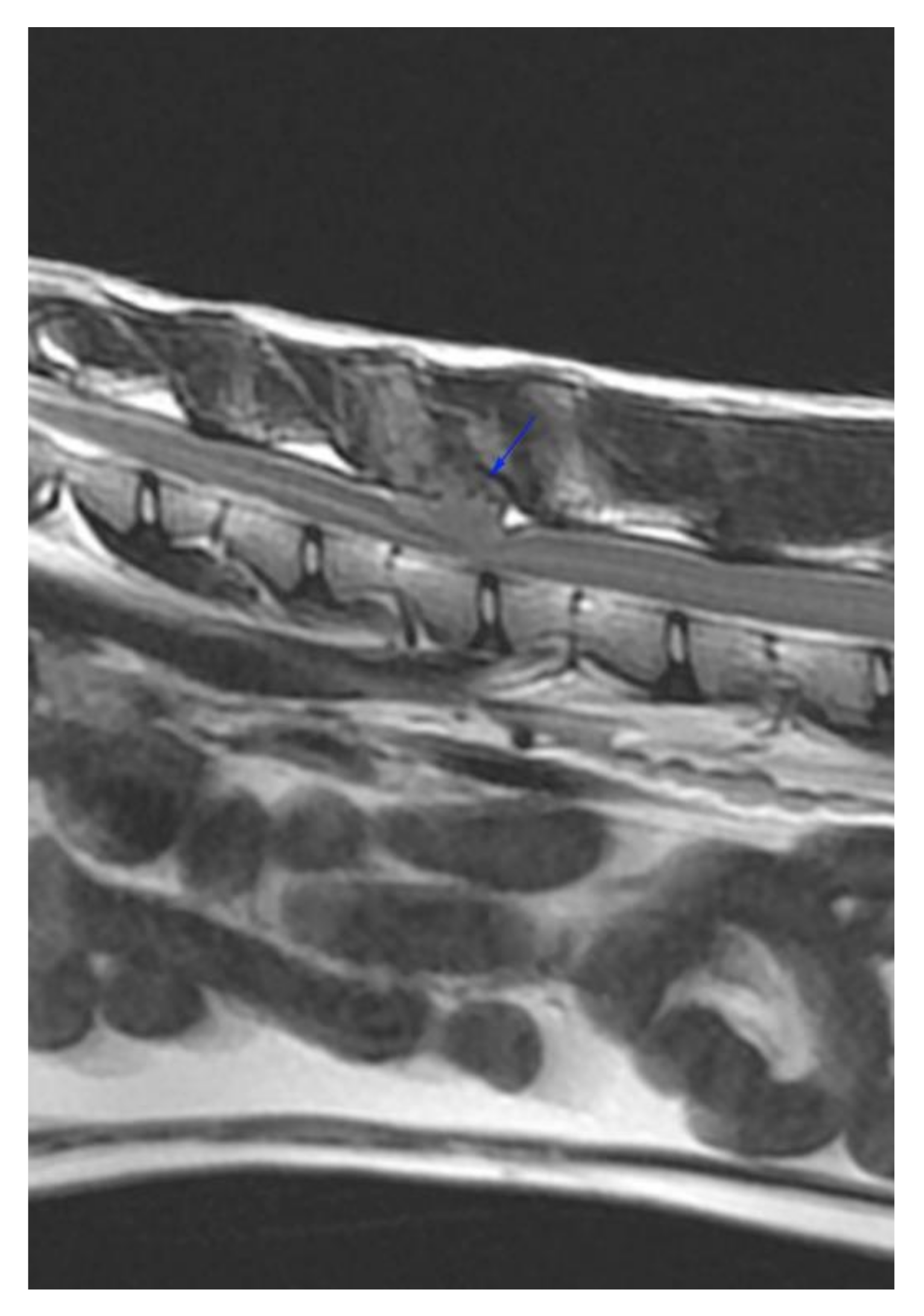
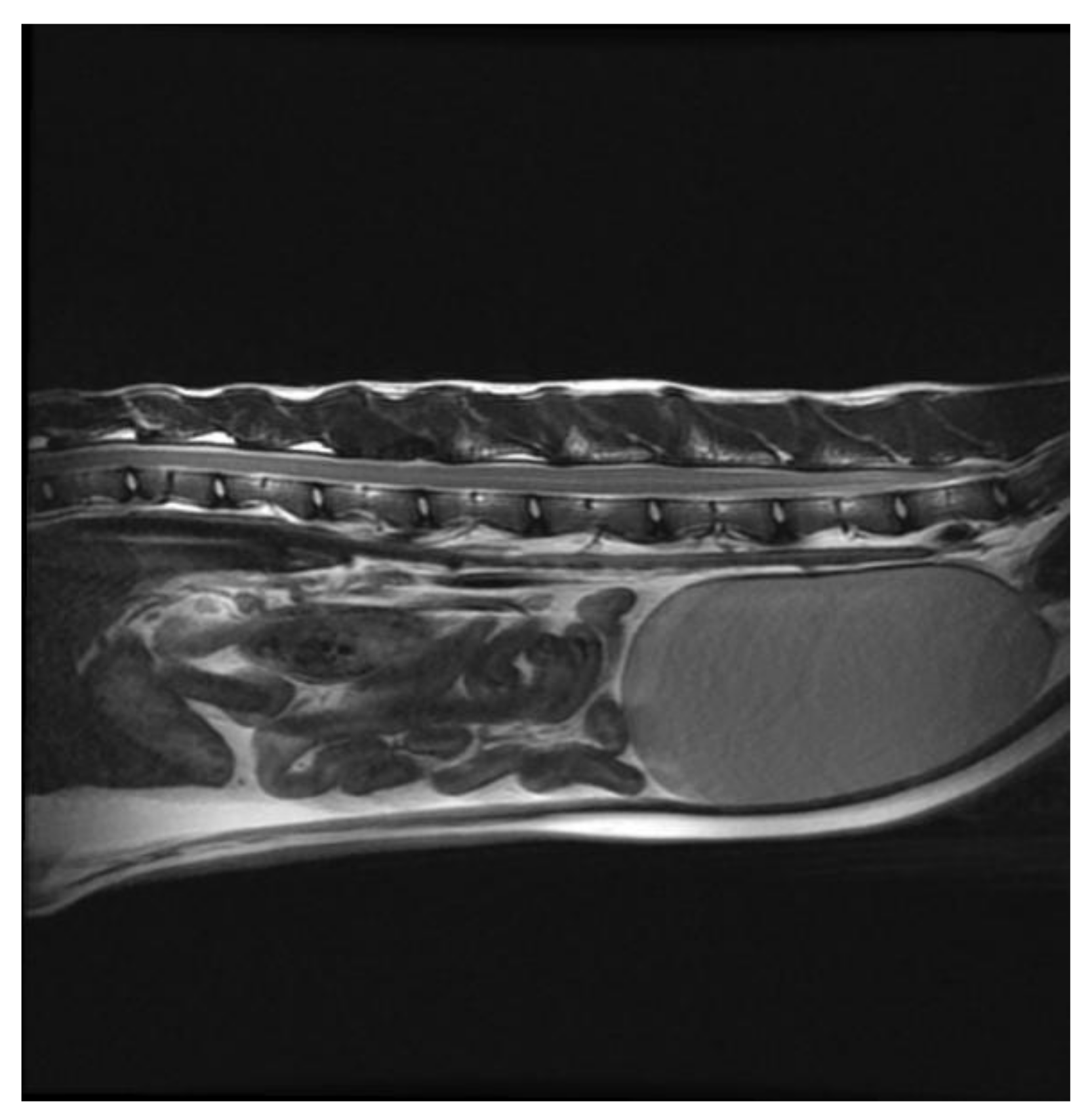
:1. Case Description
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dorn, C.R.; Taylor, D.O.N.; Frye, F.L.; Hibbard, H.H. Survey of Animal Neoplasms in Alameda and Contra Costa Counties, California. i. Methodology and Description of Cases. J. Natl. Cancer Inst. 1968, 40, 295–305. [Google Scholar] [CrossRef]
- Liu, S.-K.; Dorfman, H.D.; Patnaik, A.K. Primary and Secondary Bone Tumours in the Cat. J. Small Anim. Pract. 1974, 15, 141–156. [Google Scholar] [CrossRef] [PubMed]
- Dimopoulou, M.; Kirpensteijn, J.; Moens, H.; Kik, M. Histologic Prognosticators in Feline Osteosarcoma: A Comparison with Phenotypically Similar Canine Osteosarcoma. Vet. Surg. 2008, 37, 466–471. [Google Scholar] [CrossRef] [PubMed]
- Heldmann, E.; Anderson, M.A.; Wagner-Mann, C. Feline Osteosarcoma: 145 Cases (1990–1995). J. Am. Anim. Hosp. Assoc. 2000, 36, 518–521. [Google Scholar] [CrossRef]
- Grimer, R.J.; Cannon, S.R.; Taminiau, A.M.; Bielack, S.; Kempf-Bielack, B.; Windhager, R.; Dominkus, M.; Saeter, G.; Bauer, H.; Meller, I.; et al. Osteosarcoma over the Age of Forty. Eur. J. Cancer 2003, 39, 157–163. [Google Scholar] [CrossRef]
- Tsuchie, H.; Emori, M.; Nagasawa, H.; Miyakoshi, N.; Murahashi, Y.; Shimizu, J.; Mizushima, E.; Yamashita, T.; Shimada, Y. Prognosis of Primary Osteosarcoma in Elderly Patients: A Comparison between Young and Elderly Patients. Med. Princ. Pract. 2019, 28, 425–431. [Google Scholar] [CrossRef] [PubMed]
- Spodnick, G.J.; Berg, J.; Rand, W.M.; Schelling, S.H.; Couto, G.; Harvey, H.J.; Henderson, R.A.; MacEwen, G.; Mauldin, N.; McCaw, D.L. Prognosis for Dogs with Appendicular Osteosarcoma Treated by Amputation Alone: 162 Cases (1978–1988). J. Am. Vet. Med. Assoc. 1992, 200, 995–999. [Google Scholar] [PubMed]
- Dixon, A.; Chen, A.; Rossmeisl, J.H.; Sturges, B.; Vernau, K.; Levine, J.M.; Otamendi, A.; Early, P.; Partnow, A.; Curtis, L.; et al. Surgical Decompression, with or without Adjunctive Therapy, for Palliative Treatment of Primary Vertebral Osteosarcoma in Dogs. Vet. Comp. Oncol. 2019, 17, 472–478. [Google Scholar] [CrossRef]
- Rossmeisl, J.H.; Lanz, O.I.; Waldron, D.R.; Shires, P.K.; Zimmerman, K.L.; Sego, L.H. Surgical Cytoreduction for the Treatment of Non-Lymphoid Vertebral and Spinal Cord Neoplasms in Cats: Retrospective Evaluation of 26 Cases (1990–2005). Vet. Comp. Oncol. 2006, 4, 41–50. [Google Scholar] [CrossRef]
- Dhaliwal, R.S.; Johnson, T.O.; Kitchell, B.E. Primary Extraskeletal Hepatic Osteosarcoma in a Cat. J. Am. Vet. Med. Assoc. 2003, 222, 340–342. [Google Scholar] [CrossRef]
- Spugnini, E.P.; Ruslander, D.; Bartolazzi, A. Extraskeletal Osteosarcoma in a Cat. J. Am. Vet. Med. Assoc. 2001, 219, 60–62. [Google Scholar] [CrossRef]
- Dernell, W.S.; van Vechten, B.J.; Straw, R.C.; LaRue, S.M.; Powers, B.E.; Withrow, S.J. Outcome Following Treatment of Vertebral Tumors in 20 Dogs (1986–1995). J. Am. Anim. Hosp. Assoc. 2000, 36, 245–251. [Google Scholar] [CrossRef]
- Walter, C.U.; Dernell, W.S.; LaRue, S.M.; Lana, S.E.; Lafferty, M.H.; LaDue, T.A.; Withrow, S.J. Curative-Intent Radiation Therapy as a Treatment Modality for Appendicular and Axial Osteosarcoma: A Preliminary Retrospective Evaluation of 14 Dogs with the Disease. Vet. Comp. Oncol. 2005, 3, 1–7. [Google Scholar] [CrossRef]
- Hahn, K.A.; Endicott, M.M.; King, G.K.; Harris-King, F.D. Evaluation of Radiotherapy Alone or in Combination with Doxorubicin Chemotherapy for the Treatment of Cats with Incompletely Excised Soft Tissue Sarcomas: 71 Cases (1989–1999). J. Am. Vet. Med. Assoc. 2007, 231, 742–745. [Google Scholar] [CrossRef]
- Poirier, V.J.; Thamm, D.H.; Kurzman, I.D.; Jeglum, K.A.; Chun, R.; Obradovich, J.E.; O’Brien, M.; Fred, R.M.; Phillips, B.S.; Vail, D.M. Liposome-Encapsulated Doxorubicin (Doxil) and Doxorubicin in the Treatment of Vaccine-Associated Sarcoma in Cats. J. Vet. Intern. Med. 2002, 16, 726–731. [Google Scholar] [CrossRef]
- Barber, L.G.; Sørenmo, K.U.; Cronin, K.L.; Shofer, F.S. Combined Doxorubicin and Cyclophosphamide Chemotherapy for Nonresectable Feline Fibrosarcoma. J. Am. Anim. Hosp. Assoc. 2000, 36, 416–421. [Google Scholar] [CrossRef]
- Troedson, K.; Hossann, M.; Hirschberger, J.; Ratzlaff, C.; Baer, S.; Meyer-Lindenberg, A.; Winger, K.; Wess, G.; Doerfelt, R.; Schweiger, M.; et al. Neoadjuvant Therapy of Locally Advanced Feline Injection Site Sarcoma with Thermosensitive Doxorubicin-Containing Phosphatidyldiglycerol Liposomes or Free Doxorubicin in Combination with Regional Hyperthermia. In Proceedings of the 28. Jahrestagung der FG “Innere Medizin und Klinische Labordiagnostik” der DVG (InnLab)—Teil 1: Vorträge, Online, 28–29 January 2020; Volume 48. [Google Scholar]
- Bray, J.; Polton, G. Neoadjuvant and Adjuvant Chemotherapy Combined with Anatomical Resection of Feline Injection-Site Sarcoma: Results in 21 Cats. Vet. Comp. Oncol. 2016, 14, 147–160. [Google Scholar] [CrossRef]
- Frezoulis, P.; Harper, A. The Role of Toceranib Phosphate in Dogs with Non-Mast Cell Neoplasia: A Systematic Review. Vet. Comp. Oncol. 2022, 20, 362–371. [Google Scholar] [CrossRef]
- London, C.; Mathie, T.; Stingle, N.; Clifford, C.; Haney, S.; Klein, M.K.; Beaver, L.; Vickery, K.; Vail, D.M.; Hershey, B.; et al. Preliminary Evidence for Biologic Activity of Toceranib Phosphate (Palladia®) in Solid Tumours. Vet. Comp. Oncol. 2012, 10, 194–205. [Google Scholar] [CrossRef] [Green Version]
- Al-Dissi, A.N.; Haines, D.M.; Singh, B.; Kidney, B.A. Immunohistochemical Expression of Vascular Endothelial Growth Factor and Vascular Endothelial Growth Factor Receptor in Canine Cutaneous Fibrosarcomas. J. Comp. Pathol. 2009, 141, 229–236. [Google Scholar] [CrossRef]
- Holtermann, N.; Kiupel, M.; Hirschberger, J. The Tyrosine Kinase Inhibitor Toceranib in Feline Injection Site Sarcoma: Efficacy and Side Effects. Vet. Comp. Oncol. 2017, 15, 632–640. [Google Scholar] [CrossRef] [PubMed]
- Ohba, T.; Cates, J.M.; Cole, H.A.; Slosky, D.A.; Haro, H.; Ichikawa, J.; Ando, T.; Schwartz, H.S.; Schoenecker, J.G. Pleiotropic effects of bisphosphonates on osteosarcoma. Bone 2014, 63, 110–120. [Google Scholar] [CrossRef] [PubMed]



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Giuliano, A.; De Busscher, V.; Lu, D.D.A.; Ng, K.W.L.; Beatty, J.A. Successful Treatment of Vertebral Osteosarcoma in a Cat Using Marginal Surgical Excision and Chemotherapy. Vet. Sci. 2022, 9, 315. https://doi.org/10.3390/vetsci9070315
Giuliano A, De Busscher V, Lu DDA, Ng KWL, Beatty JA. Successful Treatment of Vertebral Osteosarcoma in a Cat Using Marginal Surgical Excision and Chemotherapy. Veterinary Sciences. 2022; 9(7):315. https://doi.org/10.3390/vetsci9070315
Chicago/Turabian StyleGiuliano, Antonio, Virginie De Busscher, Diane D. A. Lu, Karen W. L. Ng, and Julia A. Beatty. 2022. "Successful Treatment of Vertebral Osteosarcoma in a Cat Using Marginal Surgical Excision and Chemotherapy" Veterinary Sciences 9, no. 7: 315. https://doi.org/10.3390/vetsci9070315
APA StyleGiuliano, A., De Busscher, V., Lu, D. D. A., Ng, K. W. L., & Beatty, J. A. (2022). Successful Treatment of Vertebral Osteosarcoma in a Cat Using Marginal Surgical Excision and Chemotherapy. Veterinary Sciences, 9(7), 315. https://doi.org/10.3390/vetsci9070315






