Facilitating Development of Problem-Solving Skills in Veterinary Learners with Clinical Examples
Simple Summary
Abstract
1. Introduction
2. Problem and Problem-Solving
2.1. What Is a Problem?
2.2. What Is Problem-Solving
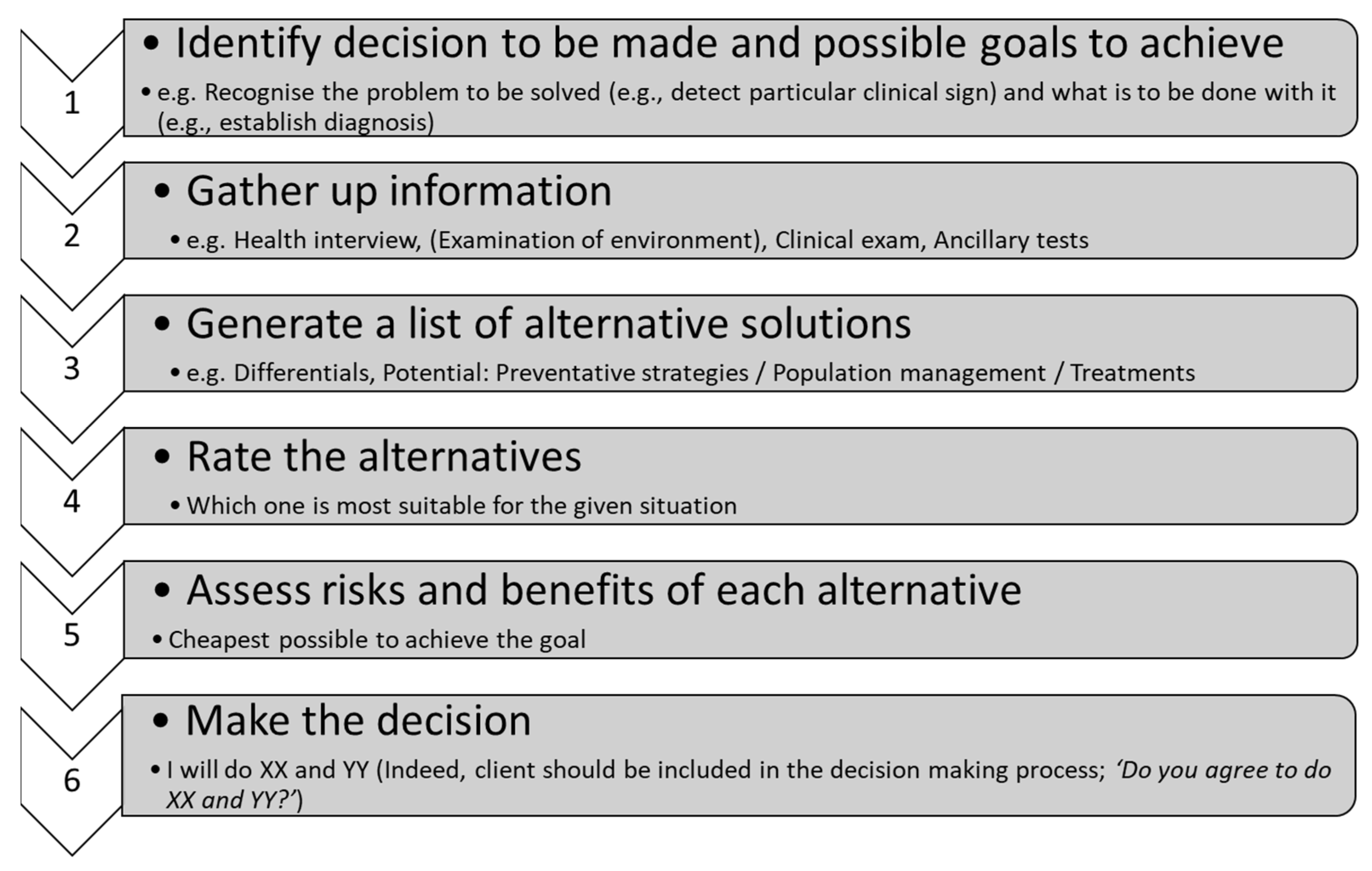
2.3. What Is Decision-Making?
3. Teaching Problem-Solving
3.1. Problem-Solving Techniques
3.2. Specific and Non-Specific Problems
3.3. Role of the Instructor in Teaching Problem-Solving
3.4. Learner Benefits from Learning Problem-Solving Skills
4. Addressing Various Elements of Inadequate Problem-Solving
Poor Problem Detection during Clinical Problem-Solving
- Individual capacity and differences in mental problem-solving skills between people
- Differences in age and gender (variable reports; detected during exams but also in clinical practice) with females and more mature people showing usually better problem-solving skills
- Flows in data gathering, with people having problems in data gathering having poorer problem-solving skills
- Following strict guidelines with little to no adjustments to the particular circumstances/presentations, seeking ‘textbook’ answers and so failing to realize that complaints often do not express themselves clearly such as with poorly expressed signs and syndromes
- Lack of connection of involvement of multiple organ systems/pathophysiology
- Lack of capacity to deal with multiple activities and hypotheses at once (multitasking)
- Lack of lifelong learning/continuing education of veterinary instructors adversely impacting availability of current information and so effective teaching
- Learner inexperience in problem-solving in veterinary medical fields, but may be also generalized poor problem-solving
5. Example Clinical Encounter
- Case encounter occurs early morning
- Holstein-Friesian calf from an embryo transfer recipient cow
- Delivered 10 days ago without assistance
- Had high vigor until last night
- Sudden onset of diarrhea about 6- 8 h before being seen
- Now in sternal recumbency, semi-obtunded
- Examination findings
- ○
- Cardinal signs all at the lower end of ‘normal’
- ○
- Mucous membranes tacky but relatively moist
- ○
- Skin tent 8 s
- ○
- Eyes sunken about 0.5 cm from the orbit
- ○
- Lack of suck reflex
- ○
- No alimentary sounds at the abdomen
5.1. What Should Problem-Solving Address?
- (1)
- Construct the problem list
- What is missing on the learner’s problem list
- (2)
- Create a timeline associated with the problem
- 10 days old
- Can exclude relevant congenital problems
- Was OK up to last night
- Diarrhea detected some 6–8 h before the encounter
- Peracute to acute case
- Laboratory findings may be unreliable
- (3)
- Describe the (anatomical) system involved or the pathophysiological principle applicable to the case
- Alimentary
- Loss of absorptive capacity
- Mechanical damage to the intestinal wall
- Overgrowth of unwanted bacteria and production of D-Lactate
- Cardiovascular
- Dehydration
- Hypokalemia
- Metabolic acidosis
- Neonatal calf diarrhea usually results in a metabolic acidosis, not a metabolic alkalosis
- Toxemia
- May not be high on the list due to the lack of the toxic line on the gums
- Hemolymphatic
- Dehydration and hypovolemic shock
- Sepsis absent or compensated, plus toxemia
- Toxemia likely absent
- Nervous
- Dehydration
- Excess D-Lactate
- Hypoglycemia
- Toxemia
- Respiratory
- Metabolic acidosis
- Urinary
- Lack of perfusion
- (4)
- Propose management for the case
- Immediate
- Treatment should address important derangements
- Dehydration
- Hypoglycemia
- Hypokalemia
- Metabolic acidosis
- ±Toxemia
- Route of administration of the fluid therapy should be considered
- Initially, intravenous due to lack of suck reflex and inability to absorb oral fluids
- Continue with oral
- Fluid type
- Treatment plan
- Bolus in 1st hour
- On-going
- On-going care
- On-going fluid therapy
- Re-introduction of milk
- Prevention of further case
- Caused by infectious or non-infectious cause
- All undifferentiated calf diarrhea should be considered infectious until proven otherwise
- If infectious
- Contagious or not
- Zoonotic or not
- Colostrum management
- Housing management
- Zoonotic risk
- Consider immune-compromised people
- (5)
- Identify any unique features associated with the case
- Some of the acid-base (e.g., the excess of D-Lactate) and electrolyte imbalances (e.g., apparent hyperkalemia when the body suffers from absolute hypokalemia) may not be detected by laboratory tests
- Due to the very rapid development, some of the clinical findings may be unreliable (e.g., the real degree of dehydration may not be properly detected with estimation of enophthalmia and/or skin tent)
5.2. Assisting the Learner to Recognise Problems with Example Discussions
6. Conclusions
7. Glossary
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Aranda, L.; Mena-Rodríguez, E.; Rubio, L. Basic Skills in Higher Education: An analysis of attributed importance. Front. Psychol. 2022, 13, 752248. [Google Scholar] [CrossRef]
- Humm, K.R.; May, S.A. Clinical reasoning by veterinary students in the first-opinion setting: Is it encouraged? Is it practiced? J. Vet. Med. Educ. 2018, 45, 156–162. [Google Scholar] [CrossRef] [PubMed]
- The Royal College of Veterinary Surgeons (RCVS). Day One Competences; RCVS: London, UK, 2020; p. 16. [Google Scholar]
- Meyer, C.A.; Hall, H.; Heise, N.; Kaminski, K.; Ivie, K.R.; Clapp, T.R. A systematic approach to teaching case studies and solving novel problems. J. Microbiol. Biol. Educ. 2019, 19, 19-3. [Google Scholar] [CrossRef] [PubMed]
- Murad, M.H.; Coto-Yglesias, F.; Varkey, P.; Prokop, L.J.; Murad, A.L. The effectiveness of self-directed learning in health professions education: A systematic review. Med. Educ. 2010, 44, 1057–1068. [Google Scholar] [CrossRef] [PubMed]
- Klemenc-Ketis, Z.; Kersnik, J. Deficiency areas in decision making in undergraduate medical students. Adv. Med. Educ. Pract. 2014, 5, 223. [Google Scholar] [CrossRef]
- Hunter, S.; Arthur, C. Clinical reasoning of nursing students on clinical placement: Clinical educators’ perceptions. Nurse Educ. Pract. 2016, 18, 73–79. [Google Scholar] [CrossRef]
- Audétat, M.C.; Laurin, S.; Dory, V.; Charlin, B.; Nendaz, M.R. Diagnosis and management of clinical reasoning difficulties: Part I. Clinical reasoning supervision and educational diagnosis. Med. Teach. 2017, 39, 792–796. [Google Scholar] [CrossRef]
- Bowen, J.L. Educational strategies to promote clinical diagnostic reasoning. N. Engl. J. Med. 2006, 355, 2217–2225. [Google Scholar] [CrossRef]
- Lateef, F. Clinical reasoning: The core of medical education and practice. Int. J. Intern. Emerg. Med. 2018, 1, 1015. [Google Scholar]
- Petrovski, K.; McArthur, M. The art and science of consultations in bovine medicine: Use of modified Calgary–Cambridge guides. Maced. Vet. Rev. 2015, 38, 137–147. [Google Scholar] [CrossRef]
- Weitzel, K.W.; Walters, E.A.; Taylor, J. Teaching clinical problem solving: A preceptor’s guide. Am. J. Health-Syst. Pharm. 2012, 69, 1588–1599. [Google Scholar] [CrossRef]
- Hardin, L.E. Problem-solving concepts and theories. J. Vet. Med. Educ. 2003, 30, 226–229. [Google Scholar] [CrossRef]
- Vu, N.V. Describing, teaching, and predicting medical problem-solving: A review. Eval. Health Prof. 1980, 3, 435–460. [Google Scholar] [CrossRef]
- Hollingworth, R.W.; McLoughlin, C. Developing science students’ metacognitive problem solving skills online. Australas. J. Educ. Technol. 2001, 17, 50–63. [Google Scholar] [CrossRef][Green Version]
- Hargrove, R.A.; Nietfeld, J.L. The impact of metacognitive instruction on creative problem solving. J. Exp. Educ. 2015, 83, 291–318. [Google Scholar] [CrossRef]
- Mechner, F.; Fredrick, T.; Jenkins, T. How can one specify and teach thinking skills? Eur. J. Behav. Anal. 2013, 14, 285–293. [Google Scholar] [CrossRef]
- Berner, E.S.; Bligh, T.; Guerin, R. An indication for a process dimension in medical problem-solving. Med. Educ. 1977, 11, 324–328. [Google Scholar] [CrossRef] [PubMed]
- Jonassen, D. Supporting problem solving in PBL. Interdiscip. J. Probl.-Based Learn. 2011, 5, 95–119. [Google Scholar] [CrossRef]
- Mettes, C.; Pilot, A.; Roossink, H.; Kramers-Pals, H. Teaching and learning problem solving in Science. Part I: A general strategy. J. Chem. Educ. 1980, 57, 882. [Google Scholar] [CrossRef]
- Carson, J. A problem with problem solving: Teaching thinking without teaching knowledge. Math. Educ. 2007, 17, 7–14. [Google Scholar]
- Collins, A. What is the most effective way to teach problem solving? A commentary on productive failure as a method of teaching. Instr. Sci. 2012, 40, 731–735. [Google Scholar] [CrossRef]
- Matinpour, M.; Sedighi, I.; Monajemi, A.; Jafari, F.; Momtaz, H.E.; Seif Rabiei, M.A. Clinical reasoning and improvement in the quality of medical education. Shiraz. E-Med. J. 2014, 15, e18667. [Google Scholar] [CrossRef]
- Woods, D.R. How might I teach problem solving. New Dir. Teach. Learn. 1987, 30, 55–71. [Google Scholar] [CrossRef]
- Papp, K.K.; Huang, G.C.; Clabo, L.M.L.; Delva, D.; Fischer, M.; Konopasek, L.; Schwartzstein, R.M.; Gusic, M. Milestones of critical thinking: A developmental model for medicine and nursing. Acad. Med. 2014, 89, 715–720. [Google Scholar] [CrossRef]
- Modi, J.N.; Anshu; Gupta, P.; Singh, T. Teaching and assessing clinical reasoning skills. Indian Pediatri. 2015, 52, 787–794. [Google Scholar] [CrossRef]
- Gonzalez, L.; Nielsen, A.; Lasater, K. Developing Students’ Clinical Reasoning Skills: A Faculty Guide. J. Nurs. Educ. 2021, 60, 485–493. [Google Scholar] [CrossRef]
- Levett-Jones, T.; Hoffman, K.; Dempsey, J.; Jeong, S.Y.-S.; Noble, D.; Norton, C.A.; Roche, J.; Hickey, N. The ‘five rights’ of clinical reasoning: An educational model to enhance nursing students’ ability to identify and manage clinically ‘at risk’patients. Nurse Educ. Today 2010, 30, 515–520. [Google Scholar] [CrossRef] [PubMed]
- Tanner, C.A. Thinking like a nurse: A research-based model of clinical judgment in nursing. J. Nurs. Educ. 2006, 45, 204–211. [Google Scholar] [PubMed]
- Marshall, J. Assessment of problem-solving ability. Med. Educ. 1977, 11, 329–334. [Google Scholar] [CrossRef]
- Carr, A.N.; Kirkwood, R.N.; Petrovski, K.R. Practical Use of the (Observer)-Reporter–Interpreter-Manager–Expert ((O)RIME) framework in veterinary clinical teaching with clinical examples. Encyclopedia, 2022; submitted. [Google Scholar]
- Linn, A.; Khaw, C.; Kildea, H.; Tonkin, A. Clinical reasoning: A guide to improving teaching and practice. Aust. Fam. Physician 2012, 41, 18–20. [Google Scholar] [PubMed]
- Rencic, J. Twelve tips for teaching expertise in clinical reasoning. Med. Teach. 2011, 33, 887–892. [Google Scholar] [CrossRef] [PubMed]
- Steinert, Y.; Mann, K.V. Faculty Development: Principles and Practices. J. Vet. Med. Educ. 2006, 33, 317–324. [Google Scholar] [CrossRef]
- Carr, A.N.; Kirkwood, R.N.; Petrovski, K.R. Using the five-microskills method in veterinary medicine clinical teaching. Vet. Sci. 2021, 8, 89. [Google Scholar] [CrossRef] [PubMed]
- Woods, D.R.; Hrymak, A.N.; Marshall, R.R.; Wood, P.E.; Crowe, C.M.; Hoffman, T.W.; Wright, J.D.; Taylor, P.A.; Woodhouse, K.A.; Bouchard, C.K. Developing problem solving skills: The McMaster problem solving program. J. Eng. Educ. 1997, 86, 75–91. [Google Scholar] [CrossRef]
- Hiss, R.G.; Peirce, J.C. A strategy for developing educational objectives in medicine: Problem-solving skills. J. Med. Educ. 1974, 49, 660–665. [Google Scholar] [CrossRef] [PubMed]
- Chowdhury, R.R.; Kalu, G. Learning to give feedback in medical education. Obstet. Gynaecol. 2004, 6, 243–247. [Google Scholar] [CrossRef]
- Radhakrishnan, N.S.; Singh, H.; Southwick, F.S. Teaching novice clinicians how to reduce diagnostic waste and errors by applying the Toyota Production System. Diagnosis 2019, 6, 179–185. [Google Scholar] [CrossRef]
- Carr, A.N.M.; Kirkwood, R.N.; Petrovski, K.R. Effective Veterinary Clinical Teaching in a Variety of Teaching Settings. Vet. Sci. 2022, 9, 17. [Google Scholar] [CrossRef]
- Kassirer, J.P. Teaching clinical reasoning: Case-based and coached. Acad. Med. 2010, 85, 1118–1124. [Google Scholar] [CrossRef]
- Henry, J.N. Identifying problems in clinical problem solving. Perceptions and interventions with nonproblem-solving clinical behaviors. Phys. Ther. 1985, 65, 1071–1074. [Google Scholar] [CrossRef] [PubMed]
- McKimm, J.; Swanick, T. Clinical Teaching Made Easy a Practical Guide to Teaching and Learning in Clinical Settings; Quay: London, UK, 2010. [Google Scholar]
- Neher, J.O.; Gordon, K.C.; Meyer, B.; Stevens, N. A five-step “microskills” model of clinical teaching. J. Am. Board Fam. Pract./Am. Board Fam. Pract. 1992, 5, 419–424. [Google Scholar]
- Neher, J.O.; Stevens, N.G. The one-minute preceptor: Shaping the teaching conversation. Fam. Med. 2003, 35, 391–393. [Google Scholar]
- Slater, J.A.; Lujan, H.L.; DiCarlo, S.E. Does gender influence learning style preferences of first-year medical students? Adv. Physiol. Educ. 2007, 31, 336–342. [Google Scholar] [CrossRef]
- Ramsbottom-Lucier, M.; Johnson, M.; Elam, C.L. Age and gender differences in students’ preadmission qualifications and medical school performances. Acad. Med. J. Assoc. Am. Med. Coll. 1995, 70, 236–239. [Google Scholar] [CrossRef] [PubMed]
- Kies, S.M.; Williams, B.D.; Freund, G.G. Gender plays no role in student ability to perform on computer-based examinations. BMC Med. Educ. 2006, 6, 57. [Google Scholar] [CrossRef]

| Element Lacking/Parameter | Detection | Strategy to Assist the Learner | Example of Facilitating Discussion |
|---|---|---|---|
| Complex approach to a problem | Reflection ‘Think aloud’ | Purposeful questioning Team work | “Could we consider different ways to solve this problem?” |
| Inefficient data collection | Omission errors (e.g., Procedure/Process incomplete; Sticks to standardized protocol, disregarding clinical presentation) | Modelling of data collection followed by solicitation of new data presentation by the learner Providing more opportunities to practice (e.g., use of simulator/s) Purposeful observation of learners who are skilled in the particular omission | “Can we again go through the process of data collection in this case? I would like you to observe me doing the health interview and clinical exam. I would like you to think of what additional information or clarification would be helpful in this particular case that you may have omitted in your data collection.” |
| Presentation incomplete (e.g., Disregarding data judged as not important, Lack of identification of what is important) | Modelling of data collection followed by solicitation of new data presentation by the learner Providing more opportunities to practice | “Can we again go through the process of data collection in this case? I would like you to observe me doing the health interview and clinical exam. You should pay attention to the items used in obtaining information. Then we can re-discuss your findings.” | |
| Inefficient data reporting | Inability to create appropriate/prioritized list of differential diagnoses | Increased clinical exposure and requirement to present cases at rounds Modelling of data analysis and creating differential diagnosis list Purposeful questioning Providing more opportunities to practice Providing regular feedback ‘Think aloud’ | “Can you summarize what the main findings are in one to two sentences?” or “Can you write down the list of problems for this case?” Learner does. “Now, it will be good to hear a prioritized list of differentials considering rule-ins and rule-outs applicable to this case.” or “Please prioritize the list of problems detected in this case to assist us in creating an appropriate list of differentials.” |
Reporting/Summarizing
| “Let’s discuss further the data gathered. I think you summarized the case you presented as a calf with a fever, swelling of multiple joints, which are tender and, from the health interview you know that this calf had an episode of diarrhea some two weeks ago. In fact, that would be a very good summary. However, you also added a few elements which are very loosely connected to this case. For example, yearlings having diarrhea that seems to be related to parasitic burden. This led you to a conclusion that this calf may be suffering from parasitic gastroenteritis. Parasitic gastroenteritis may be the problem of yearlings which are on pasture. However, this 18-day old calf has been hand-reared. I would like you to think of two completely separate problems. Can we re-discuss your differential again?” or “Please watch me discussing this with the client, particularly how I would put things together.” | ||
| Seek answer in ‘textbook’ presentations only | “Let’s discuss further the data you gathered. Now, it will be good to think of which diagnoses may fit some or a majority of these problems, although they may not be an exact match.” | ||
| Poor problem detection | Difficulty seeing the scope of a problem Lack of recognition of a particular clinical problem Lack of recognition of the effect of the problem on the client | Employ ‘Component opportunity’ Purposeful questioning | “Let’s discuss further the data gathered. You mentioned that in this cow you detected a fever, cough, purulent nasal discharge, abnormal lung sounds on the right cranio-ventral side and that she has calved some 7 days ago. You also mentioned that the client has given her oral calcium about 2 days after calving for suspected milk fever. You connected all detected clinical signs but skipped through the health interview information in your interpretation. I think, it is important to consider the health interview in your problem presentation. Can you think of the main pathophysiological mechanism of hypocalcemia and how that may be related to the current case?” |
| “Do you notice anything else that should be on the list of problems for this particular case?” | |||
| “Can we discuss the parameters you detected and list them separately into ‘normal’ and abnormal? We are all aware that these should be considered together with other findings but for the purpose of this exercise let’s consider them independently. Do you agree?” | |||
| Poor implementation of solutions | Lack of tailoring the solution to the particular circumstances/presentation | Purposeful questioning Modelling of
| “Let’s discuss further the management you propose. You mentioned that this dairy enterprise has been under new management for a few months and there has been a rise in cases of left displaced abomasum. Can you think of management solutions for this enterprise that are a priority to prevent future cases from occurring rather than continue with surgical interventions ?” |
| Lack of suitable solutions (e.g., learner lacks understanding of what is the goal of the intervention) | “Can we go through the solution you are proposing? This farm has an individual cow with respiratory disease and you have recommended treatment with ceftiofur, a third-generation cephalosporin antimicrobial. I think it is important to consider responsible antimicrobial use in your treatment recommendation. Can you think of another antimicrobial that may be more suitable for an individual case and how that may be related to good antimicrobial stewardship?” | ||
| Proposed solution offensive | “I think we should discuss how you delivered your recommendations to the client? You mentioned that his management was poor and all his problems were due to this. It is important to consider how that made the client feel. We are aware that there are some management areas that need to be improved. However, the delivery of the message must be carefully crafted. It is important to praise the client for what they are currently doing well but also make suggestions on how to improve the current practices. Can you think of a way of doing this?” | ||
| Seeks ‘textbook’ solutions only | “Let’s discuss further the solutions you propose. It is good to think of tailoring solutions for this particular enterprise, even if they are not an exact match to each individual problem occurring on the farm.” | ||
| Poor evaluation of the outcome | Lack of holistic approach to the expected outcome |
| Item | Potential Causes/Importance | Example Assisting Discussion |
|---|---|---|
| Clinical problems that should be detected | ||
| Cardinal signs ‘normal’ | No sepsis, but may have toxemia | |
| Enophthalmos 0.5 cm | Used to estimate dehydration | “It would be useful to think of pathophysiologic mechanisms that may lead to enophthalmos.” |
| Lack of alimentary motility | Used to estimate D-lactate acidemia and hypokalemia | “Can you think of few factors that may result in decreased motility of the alimentary system (ileus) in this calf?” |
| Lack of suck reflex | Used to estimate D-lactate acidemia and hypokalemia | “Can you think of few factors that may result in loss of the suck reflex in this calf?” |
| Semi-obtunded |
| “If we know that lab results for some metabolites and electrolytes may not be reliable, we have to think about what may be the effects of some of these metabolites or electrolytes on the calf’s demeanor and on the parasympathetic system.” “Can you also think of what may be happening with the gut microbiota and what may be the effect of the changes if they occur?” |
| Severe peracute diarrhea | Rapidly developing | After discussion on enophthalmos and skin tent: “We have discussed the significance of the enophthalmos and the prolonged skin tent. Think of the speed of development of these signs and how they may be affected by the peracute development of diarrhea in this calf?” |
| Skin tent 8 sec | Used to estimate dehydration | “It would be good to think of the pathophysiologic mechanisms that may lead to prolonged skin tent.” |
| Sternal recumbency |
| “Can you think of a few factors that may result in sternal recumbency in this calf?” |
| Laboratory findings that need to be considered | ||
| Hypokalemia | ||
| Metabolic acidosis |
| “We know that typically, diarrhea leads to alkalemia due to loss of electrolytes in feces. Indeed, this is true for mature cattle as well. However, this may not be the situation in neonates. Can you think of what electrolytes may be lost with the diarrhea in this calf? Then, please think of the outcome on the acid-base status and the expected electrolyte balance?” |
| Unreliable laboratory findings |
| “It is important to realize that due to a few pathophysiological derangements, blood electrolytes and acid-base balance testing may not be reliable in neonatal calves. Can you think what electrolytes may not be represented correctly in the biochemistry panel in this calf and why?” “Can you think of what may be happening with the gut microbiota and what may be the effect of the changes, if they occur?” Learner should answer that there is overgrowth of gram-negative bacteria and production of D-Lactate. “Now, can you think of what form of lactate is normally produced in the body of mammals that is a subject of the laboratory analysis?” Learner should answer L-Lactate. “Now, after we established these differences, could you think of reasons why D-Lactate concentrations not been reported with the biochemical tests?” “Some electrolytes in diarrhea shift from intracellular to extracellular. Can you give an example?” Learner should answer potassium,“Can you now think what would be the result of this shift of potassium on the serum biochemical test results?” |
| Additional considerations in the management of this case | ||
| 10-day old calf | Age-related etiology | “Can you think of the common causative agents associated with calf diarrhea?” Learner lists a few. “Now, can you think of the age at which these causative agents usually cause diarrhea in calves?” |
| Dairy | Not on dam | “Let’s think of the usual management of neonatal dairy calves. Can you think on the feature that differs from beef calves?” |
| Embryo-transfer product | Expensive | “Let’s think about the cost-benefit of treatment of this calf. Can you think what parameters should be accounted for before making the final decision?” |
| Prevention of further cases | Animal welfare Client frustration Economics Loss of genetics | “Can you tell me what you think should be done in future to prevent recurrence of this problem? What factors should be considered when making decisions on the prevention strategies? Can you explain why prevention is important for the client?” |
| Role of management | Colostrum management Environment Hygiene Stress | “Could you explain what management factors may contribute to the occurrence of diarrhea in this calf on this enterprise?” |
| Zoonotic potential | Public health | “We already mentioned the common pathogens associated with calf diarrhea. Can you think of what risks there are for people involved in management of this and other calves on the enterprise and discuss what specific factors need to be considered?” |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carr, A.N.; Kirkwood, R.N.; Petrovski, K.R. Facilitating Development of Problem-Solving Skills in Veterinary Learners with Clinical Examples. Vet. Sci. 2022, 9, 510. https://doi.org/10.3390/vetsci9100510
Carr AN, Kirkwood RN, Petrovski KR. Facilitating Development of Problem-Solving Skills in Veterinary Learners with Clinical Examples. Veterinary Sciences. 2022; 9(10):510. https://doi.org/10.3390/vetsci9100510
Chicago/Turabian StyleCarr, Amanda (Mandi) Nichole, Roy Neville Kirkwood, and Kiro Risto Petrovski. 2022. "Facilitating Development of Problem-Solving Skills in Veterinary Learners with Clinical Examples" Veterinary Sciences 9, no. 10: 510. https://doi.org/10.3390/vetsci9100510
APA StyleCarr, A. N., Kirkwood, R. N., & Petrovski, K. R. (2022). Facilitating Development of Problem-Solving Skills in Veterinary Learners with Clinical Examples. Veterinary Sciences, 9(10), 510. https://doi.org/10.3390/vetsci9100510







