Tibial Plateau Leveling Following Tibial Tuberosity Advancement: A Case Series
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Johnson, J.A.; Austin, C.; Breur, G.J. Incidence of canine appendicular musculoskeletal disorders in 16 veterinary teaching hospitals from 1980 through 1989. Vet. Com. Orthop. Traumatol. 1994, 7, 56–69. [Google Scholar] [CrossRef]
- Slocum, B.; Devine., T. Cranial tibial wedge osteotomy: A technique for eliminating cranial tibial thrust in cranial cruciate ligament repair. J. Am. Vet. Med. Assoc. 1984, 184, 564–569. [Google Scholar] [PubMed]
- Slocum, B.; Slocum, T.D. Tibial plateau leveling osteotomy for repair of cranial cruciate ligament rupture in the canine. Vet. Clin. N. Am. Small Anim. Pract. 1993, 23, 777–795. [Google Scholar] [CrossRef]
- Christ, J.P.; Anderson, J.R.; Youk, A.O. Modified cranial closing wedge ostectomy in 25 dogs. Vet. Surg. 2018, 47, 683–691. [Google Scholar] [CrossRef]
- Montavon, P.; Damur, D.; Tepic, S. Advancement of the tibial tuberosity for the treatment of cranial cruciate deficit of the canine stifle. In Proceedings of the 1st World Orthopeadic Veterinary Congress, ESVOT-VOS, Munich, Germany, 5–8 September 2002; p. 152. [Google Scholar]
- Ecthepareborde, S.; Brunel, L.; Bolen, G.; Balligand, M. Preliminary experience of a modified Maquet technique for repair of cranial cruciate ligament rupture in dogs. Vet. Comp. Orthop. Traumatol. 2011, 24, 223–227. [Google Scholar] [CrossRef]
- Samoy, Y.; Verhoeven, G.; Bosmans, T.; Van der Vekens, E.; De Bakker, E.; Verleyen, P.; Van Ryssen, B. TTA Rapid: Description of the Technique and Short Term Clinical Trial Results of the First 50 Cases. Vet. Surg. 2014, 44, 474–484. [Google Scholar] [CrossRef]
- Ness, M.G. The modified Maquet Procedure (MMP) in dogs: Technical development and Initial clinical experience. J. Am. Anim. Hosp. Assoc. 2016, 52, 242–250. [Google Scholar] [CrossRef]
- Rettallack, L.M.; Daye, R.M. A modified Maquet-tibial tuberosity advancement technique for treatment of canine cranial cruciate ligament disease: Short term outcome and complications. Vet. Surg. 2018, 47, 44–51. [Google Scholar] [CrossRef]
- Beer, P.; Bockstahler, B.; Schnabl-Feichter, E. Tibial plateau levelling osteotomy and tibial tuberosity advancement—A systemic review. Tierärztliche Praxis Ausgabe K: Kleintiere/Heimtiere 2018, 46, 223–225. [Google Scholar] [CrossRef]
- Livet, V.; Baldinger, A.; Viguier, É.; Taroni, M.; Harel, M.; Carozzo, C.; Cachon, T. Comparison of Outcomes Associated with Tibial Plateau Levelling Osteotomy and a Modified Technique for Tibial Tuberosity Advancement for the Treatment of Cranial Cruciate Ligament Disease in Dogs: A Randomized Clinical Study. Vet. Comp. Orthop. Traumatol. 2019, 2, 314–323. [Google Scholar] [CrossRef]
- Moore, E.V.; Weeren, R.; Paek, M. Extended long-term radiographic and functional comparison of tibial plateau leveling osteotomy vs. tibial tuberosity advancement for cranial cruciate ligament rupture in the dog. Vet. Surg. 2020, 49, 146–154. [Google Scholar] [CrossRef] [PubMed]
- Schwede, M.; Rey, J.; Böttcher, P. In vivo fluoroscopic kinematography of cranio-caudal stifle stability after tibial tuberosity advancement (TTA): A retrospective case series of 10 stifles. Open Vet. J. 2018, 8, 295–304. [Google Scholar] [CrossRef] [PubMed]
- Tinga, S.; Kim, S.E.; Banks, S.A. Femorotibial kinematics in dogs treated with tibial plateau levelling osteotomy for cranial cruciate ligament insufficiency: An in vivo fluoroscopic analysis during walk. Vet. Surg. 2019, 49, 187–199. [Google Scholar] [CrossRef] [PubMed]
- Boudrieau, R.J. Tibial plateau levelling osteotomy or tibial tuberosity advancement? Vet. Surg. 2009, 38, 1–22. [Google Scholar] [CrossRef] [PubMed]
- Cook, J.L.; Evans, R.; Conzemius, M.G.; Lascelles, B.D.; McIlwraith, C.W.; Pozzi, A.; Clegg, P.; Innes, J.; Schulz, K.; Houlton, J.; et al. Proposed definitions and criteria for reporting time frame, outcome, and complications for clinical orthopedic studies in veterinary medicine. Vet. Surg. 2010, 39, 905–908. [Google Scholar] [CrossRef]
- Gatineau, M.; Dupuis, J.; Planté, J.; Moreau, M. Retrospective study of 476 tibial plateau levelling osteotomy procedures. Rate of subsequent pivot shift, meniscal tear and other complications. Vet. Comp. Orthop. Traumatol. 2011, 24, 333–341. [Google Scholar] [CrossRef]
- Au, K.K.; Gordon-Evans, W.J.; Dunning, D. Comparison of short- and long-term function and radiographic osteoarthrosis in dogs after postoperative physical rehabilitation and tibial plateau leveling osteotomy or lateral fabellar suture stabilization. Vet. Surg. 2010, 39, 173–180. [Google Scholar] [CrossRef]
- Ciliberto, E. Isolated Lateral Meniscal Tear in 4 Boxers; Free Communications ESVOT: Munich, Germany, 2004. [Google Scholar]
- Ridge, P.A. Isolated medial meniscal tear in a Border Collie. Vet. Comp. Orthop. Traumatol. 2006, 19, 110–112. [Google Scholar] [CrossRef]
- Bureau, S. Owner assessment of the outcome of tibial plateau levelling osteotomy without meniscal evaluation for treatment of naturally occurring cranial cruciate ligament rupture: 130 cases (2009 to 2013). J. Small Anim. Pract. 2017, 58, 468–475. [Google Scholar] [CrossRef]
- Tuan, S.; Farrel, M. Tibial tuberosity advancement: What have we learned so far? Companion Anim. 2015, 20, 92–103. [Google Scholar] [CrossRef]
- Bush, M.A.; Bowlt, K.; Gines, J.A.; Owen, M.R. Effect of use of different landmark methods on determining stifle angle and on calculated tibial tuberosity advancement. Vet. Comp. Orthop. Traumatol. 2011, 24, 205–210. [Google Scholar] [CrossRef]
- Tinga, S.; Kim, S.E.; Banks, S.A.; Jones, S.C.; Park, B.H.; Pozzi, A.; Lewis, D.D. Femorotibial kinematics in dogs with cranial cruciate ligament insufficiency: A three-dimensional in-vivo fluoroscopic analysis during walking. BMC Vet. Res. 2018, 14, 85. [Google Scholar] [CrossRef]
- Dennler, R.; Kipfer, N.M.; Tepic, S.; Hassing, M.; Montavon, P.M. Inclination of the patellar ligament in relation to flexion angle in stifle joint of dogs without degenerative joint disease. Am. J. Vet. Res. 2006, 67, 1849–1854. [Google Scholar] [CrossRef]
- Millet, M.; Bismuth, C.; Labrunie, A.; Marin, B.; Filleur, A.; Pillard, P.; Sonet, J.; Cachon, T.; Etchepareborde, S. Measurement of the patellar tendon-tibial plateau angle and tuberosity advancement in dogs with cranial cruciate ligament rupture. Reliability of the common tangent and tibial plateau methods of measurement. Vet. Comp. Orthop. Traumatol. 2013, 26, 469–478. [Google Scholar] [CrossRef] [PubMed]
- Etchepareborde, S.; Mills, J.; Busoni, V.; Brunel, L.; Balligand, M. Theoretical discrepancy between cage size and efficient tibial tuberosity advancement in dogs treated for cranial cruciate ligament rupture. Vet. Comp. Orthop. Traumatol. 2011, 24, 27–31. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kapler, M.W.; Marcellin-Little, D.J.; Roe, S.C. Planned wedge size compared to achieved advancement in dogs undergoing the modified Maquet procedure. Vet. Comp. Orthop. Traumatol. 2015, 28, 379–384. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Meeson, R.L.; Corah, L.; Conroy, M.C.; Calvo, I. Relationship between tibial conformation cage size and advancement achieved in TTA procedure. Vet. Res. 2018, 14, 104. [Google Scholar] [CrossRef]
- Drygas, K.A.; Pozzi, A.; Goring, R.L.; Horodyski, M.; Lewis, D.D. Effect of tibial plateau levelling osteotomy on patellar tendon angle: A radiographic cadaveric study. Vet. Surg. 2010, 39, 418–424. [Google Scholar] [CrossRef]
- Sumner, J.P.; Markel, M.D.; Mui, P. Caudal cruciate ligament damage in dogs with cranial cruciate ligament rupture. Vet. Surg. 2010, 39, 936–941. [Google Scholar] [CrossRef]
- Shirazi-Adl, A.; Maesfar, W. Effect of tibial tubercle elevation on biomechanics of the entire knee joint under muscle loads. Clin. Biomech. 2007, 22, 344–351. [Google Scholar] [CrossRef]
- Brown, N.P.; Bertocci, G.E.; Marcellin-Little, D.J. Canine stifle joint biomechanics associated with tibial plateau leveling osteotomy predicted by use of a computer model. Am. J. Vet. Res. 2014, 75, 626–632. [Google Scholar] [CrossRef] [PubMed]
- De Sandre-Robinson, D.M.; Tano, C.A.; Fiore, K.L.; Prytherch, B. Radiographic evaluation and comparison of the patellar ligament following tibial plateau leveling osteotomy and tibial tuberosity advancement in dogs: 106 cases (2009–2012). J. Am. Vet. Med. Assoc. 2017, 250, 68–74. [Google Scholar] [CrossRef]
- Stauffer, K.D.; Tuttle, T.A.; Elkins, A.D.; Wehrenberg, A.P.; Character, B.J. Complications associated with 696 tibial plateau leveling osteotomies (2001–2003). J. Am. Anim. Hosp. Assoc. 2006, 42, 44–50. [Google Scholar] [CrossRef] [PubMed]
- Mattern, K.L.; Berry, C.R.; Peck, J.N.; De Hann, J.J. Radiographic and ultrasonographic evaluation of patellar ligament following tibial plateau leveling osteotomy. Vet. Radiol. Ultrasound 2006, 47, 185–191. [Google Scholar] [CrossRef]
- Tepic, S.; Damur, D.; Montavon, P.V. Biomechanics of the stifle joint. In Proceedings of the 1st World Orthopaedic Veterinary Congress, ESVOT-VOS, Munich, Germany, 5–8 September 2002; pp. 189–190. [Google Scholar]
| Case | Breed | Age | Sex | Weight | Previous Surgery | Deterioration/Onset of Lameness | Hindlimb Lameness |
|---|---|---|---|---|---|---|---|
| 1 | Golden retriever | 60 months | M | 40.0 | 3 months | Lame since index surgery and deterioration in the last 4 weeks | 2/5 right |
| 2 | Mongrel | 84 months | F | 26.3 | 36 months | Lame since index surgery and deterioration in the last 6 months | 3/5 left |
| 3 | Springer Spaniel | 72 months | M | 19.4 | 8 months | Lame since index surgery | 2/5 right |
| 4 | Labrador Retriever | 88 months | M | 31.5 | 3 months | Lame since index surgery | 2/5 right |
| 5 | West Highland White Terrier | 92 months | F | 10.85 | 3 months | Lame since index surgery and deterioration in the last 6 weeks | 5/5 right |
| 6 | Labrador Retriever | 72 months | M | 31.3 | 36 months | Lame since index surgery and deterioration in the last 6 months | 3/5 right |
| 7 | Mongrel | 120 months | F | 20.5 | 36 months | Lame since index surgery and deterioration in the last week | 5/5 right |
| Case | TTAT | Preop SFA | Preop PLATP | Preop TPA | TPLT | Stifle Inspection | Postop SFA | Postop PTATP | Postop TPA |
|---|---|---|---|---|---|---|---|---|---|
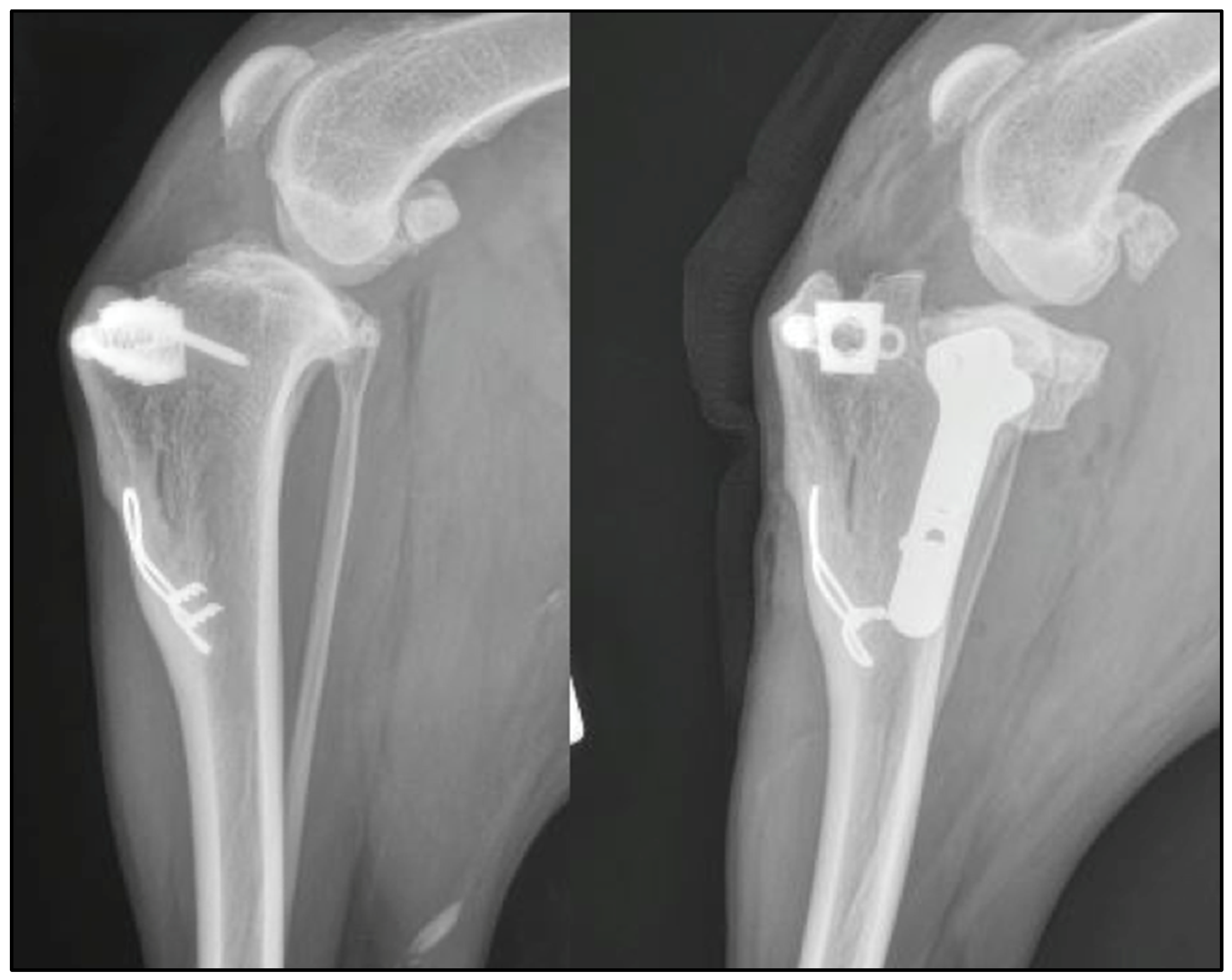
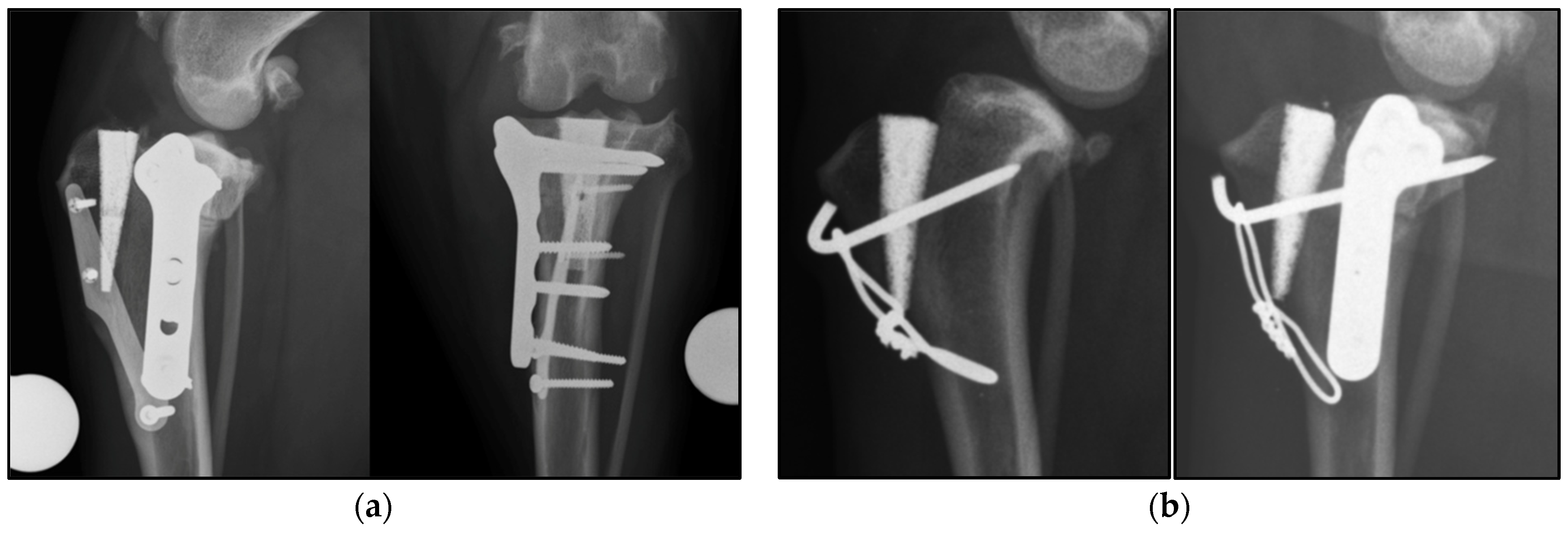
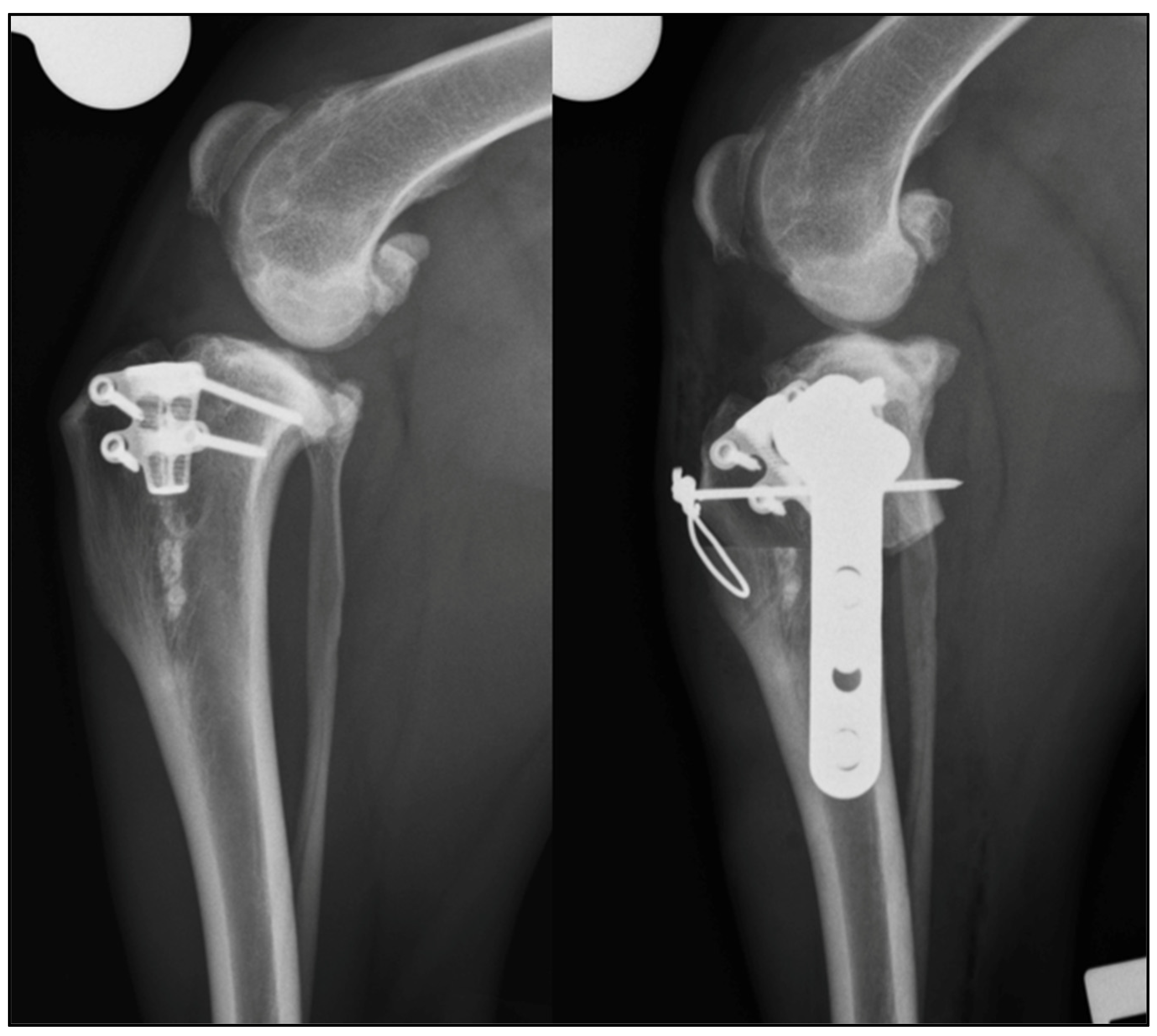
| 1 | Modified Maquet tibial tuberosity advancement | 104° | 94 ° | 28° | TPLO | Complete CCL rupture, intact menisci | 109° | 77° | 9° |
| 2 | TTA rapid | 112° | 96° | 32° | Modified CCWO (mCCWO) | Complete CCL rupture and medial meniscal tear (caudal horn) | 129° | 87° | 0° |
| 3 | Modified Maquet Procedure (MMP) | 104° | 90° | 24° | TPLO | Partial CCL rupture and intact menisci | 105° | 74° | 4° |
| 4 | MMP | 108° | 96° | 26° | TPLO and tension band | N/A | 106° | 86° | 9° |
| 5 | MMP | 137° | 102° | 34° | TPLO and tension band | N/A | 117 ° | 79° | 4° |
| 6 | MMP with 2 staples | 111° | 95° | 27° | TPLO | N/A | 115° | 79° | 8° |
| 7 | Modified Maquet Technique (MMT) | 108° | 83° | 22° | TPLO | Complete CCL rupture and medial meniscal tear (cranial horn) | 127° | 70° | 1° |
| Case | Short-Term Follow Up | Subjective Lameness Score | Clinical Findings | Radiographic Findings | Long Term Follow Up | LOAD Score |
|---|---|---|---|---|---|---|
| 1 | 8 weeks | 0 | Mild muscle atrophy, mild reduction of range of motion (ROM), negative TCT | Good healing of the bone, tibial tuberosity fracture healed and moderate stifle effusion | 61 months | 9/52 |
| 2 | 8 weeks | 1 | Very mild muscle atrophy, mild reduction of ROM, negative TCT | N/A | 17 months | 20/52 |
| 3 | 8 weeks | 1 | Mild muscle atrophy, mild reduction of the ROM, negative TCT | Almost complete bone healing, absence of implant associated complication, patellar ligament thickening | 42 months | 2/52 |
| 4 | 12 weeks | 1 | Moderate muscle atrophy, mild reduction of ROM, negative TCT | Good healing of the bone, healing of the tibial tuberosity fracture, mild stifle effusion | 83 months | 3/52 |
| 5 | 8 weeks | 1 | Mild muscle atrophy, normal ROM, negative TCT | Almost complete healing of the bone and no signs of stifle effusion | 8 months | 4/32 |
| 6 | 12 weeks | 0 | No muscle atrophy, mild reduction in ROM, negative TCT | Complete healing of the bone and mild stifle effusion | 17 months | 2/52 |
| 7 | 20 weeks | 0 | No muscle atrophy, negative TCT | N/A | N/A (dog died of kidney disease) | N/A |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Serrani, D.; Picavet, P.P.; Marti, J.; Bouvy, B.; Balligand, M.; Witte, P.G. Tibial Plateau Leveling Following Tibial Tuberosity Advancement: A Case Series. Vet. Sci. 2022, 9, 16. https://doi.org/10.3390/vetsci9010016
Serrani D, Picavet PP, Marti J, Bouvy B, Balligand M, Witte PG. Tibial Plateau Leveling Following Tibial Tuberosity Advancement: A Case Series. Veterinary Sciences. 2022; 9(1):16. https://doi.org/10.3390/vetsci9010016
Chicago/Turabian StyleSerrani, Daniele, Pierre Paul Picavet, Juan Marti, Bernard Bouvy, Marc Balligand, and Philip George Witte. 2022. "Tibial Plateau Leveling Following Tibial Tuberosity Advancement: A Case Series" Veterinary Sciences 9, no. 1: 16. https://doi.org/10.3390/vetsci9010016
APA StyleSerrani, D., Picavet, P. P., Marti, J., Bouvy, B., Balligand, M., & Witte, P. G. (2022). Tibial Plateau Leveling Following Tibial Tuberosity Advancement: A Case Series. Veterinary Sciences, 9(1), 16. https://doi.org/10.3390/vetsci9010016






