Effectiveness of Custom-Designed 3D-Printed Drill Guides in the Treatment of Lateral Humeral Condylar Fractures in a French Bulldog Bone Model
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Humeral Model Preparation
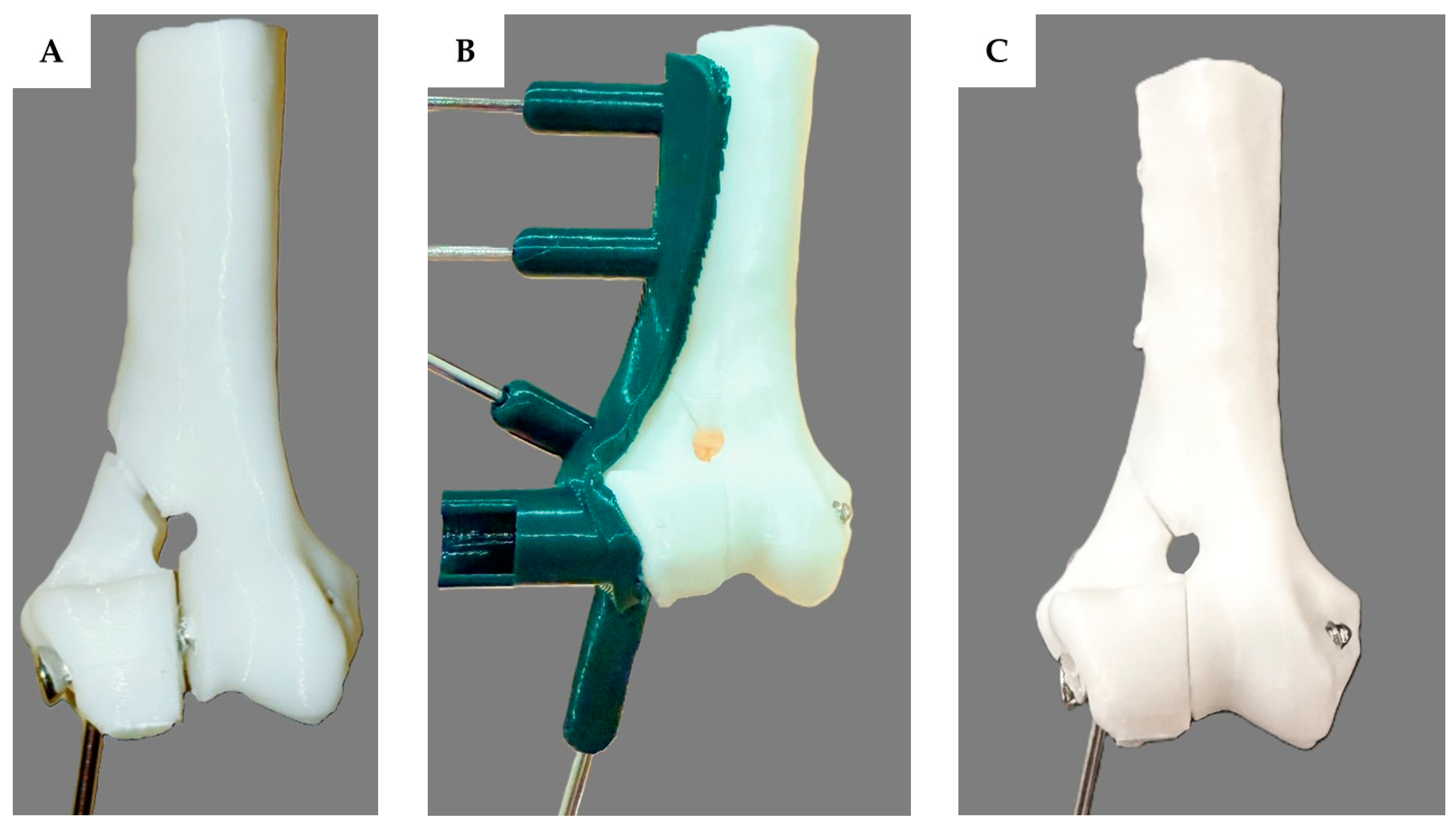
2.2. Three-Dimensional-Printed Patient-Specific Drill Guide Creation
2.3. Implantation Method
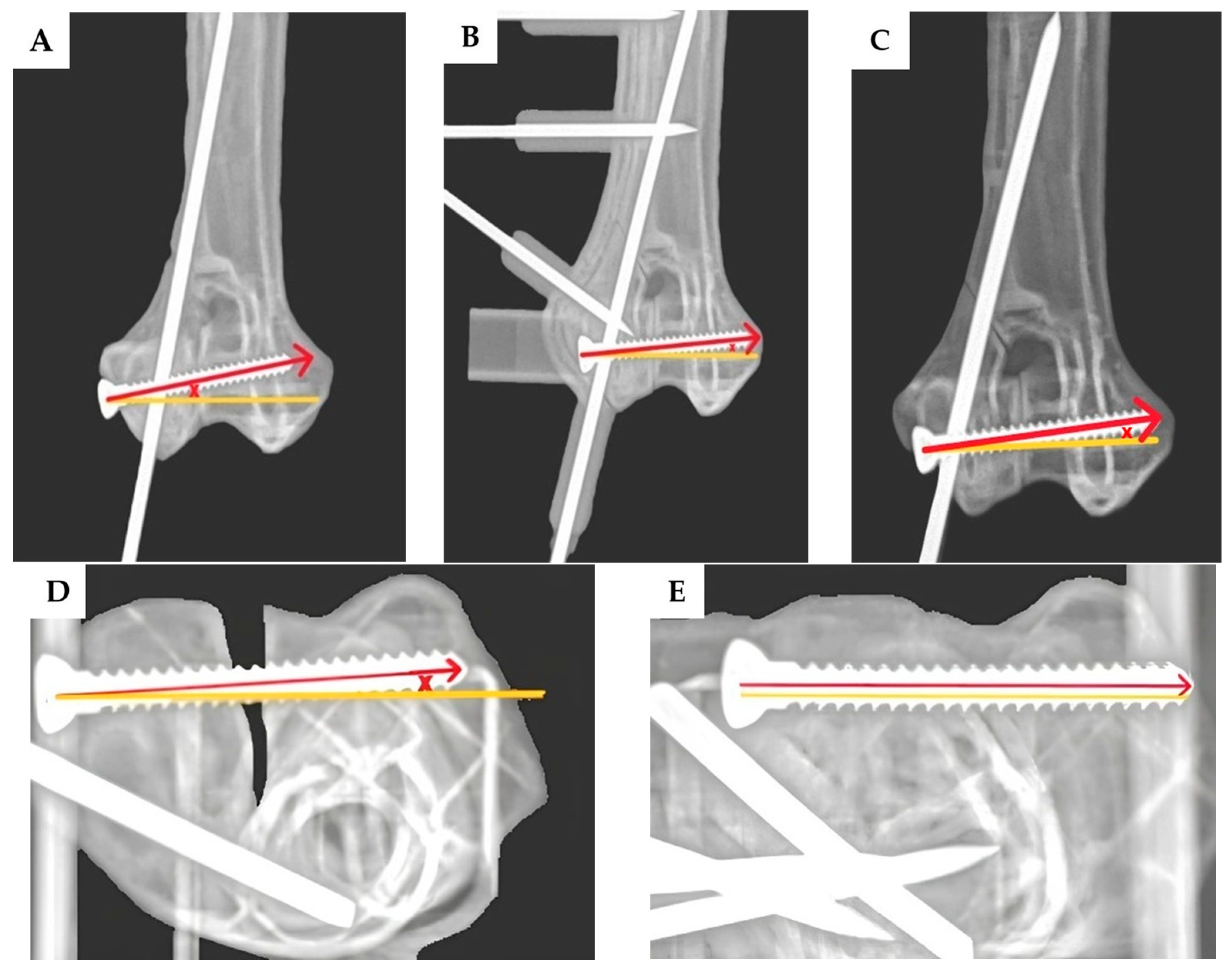
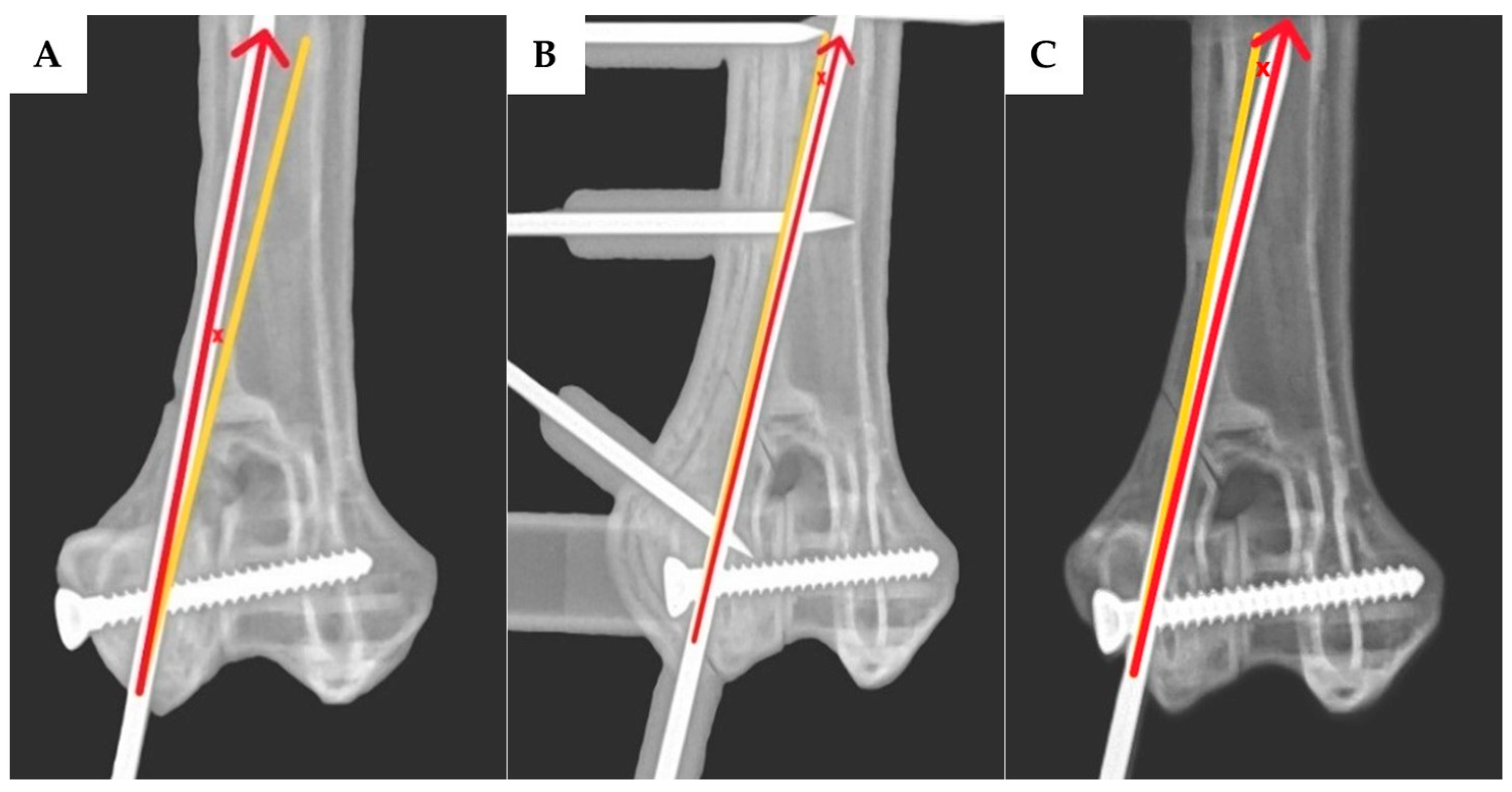
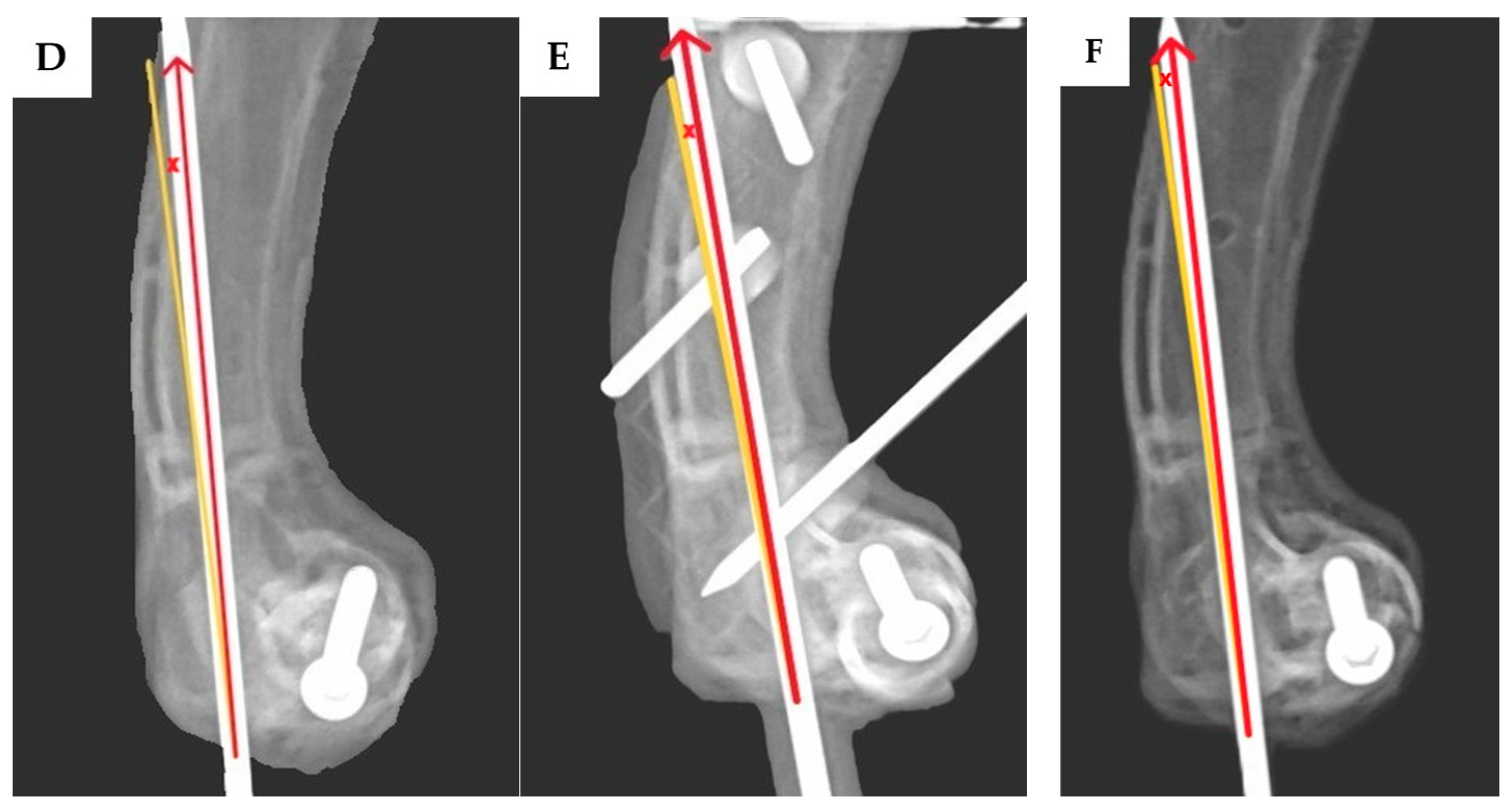
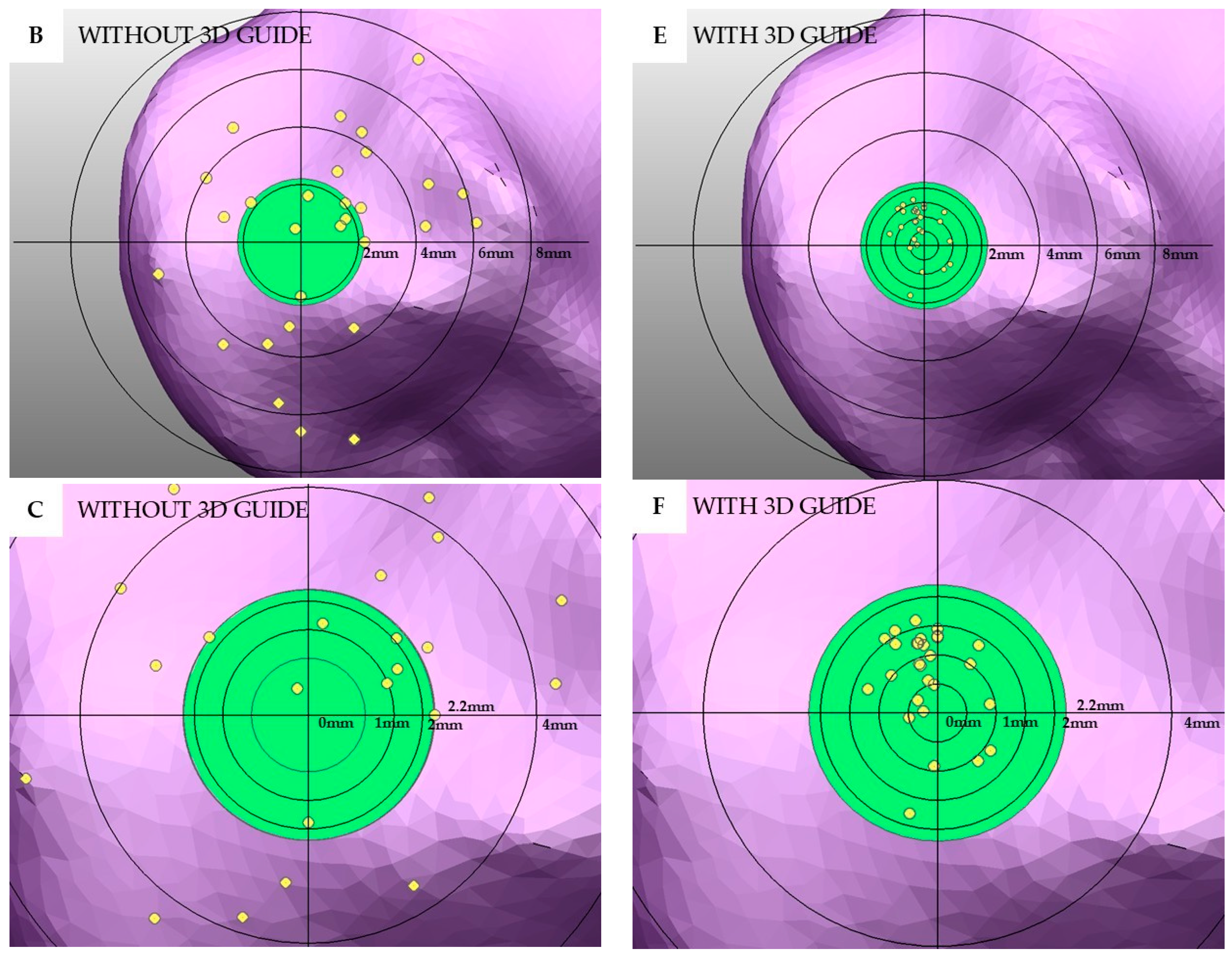
2.4. Assessment of the Transcondylar Screw and Epicondylar Pin Accuracy
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Smith, M.A.J.; Jenkins, G.; Dean, B.L.; O’Neill, T.M.; Macdonald, N.J. Effect of breed as a risk factor for humeral condylar fracture in skeletally immature dogs. J. Small Anim. Pract. 2020, 61, 374–380. [Google Scholar] [CrossRef]
- Rsrvik, A.M. Risk factors for humeral condylar fractures in the dog: A retrospective study. J. Small Anim. Pract. 1993, 34, 277–282. [Google Scholar] [CrossRef]
- Strohmeier, U.W.; Harris, K.P. Humeral intracondylar fissures in French bulldogs. Vet. Rec. 2021, 189, 504. [Google Scholar] [CrossRef] [PubMed]
- Anderson, O.J.; Langley-Hobbs, S.J.; Parsons, K.J. Humeral condylar fractures and fissures in the French bulldog. Vet. Surg. 2023, 52, 134–145. [Google Scholar] [CrossRef]
- Knight, G.C. Internal Fixation of the Fractured Lateral Humeral Condyle. Clin. Commun. 1960, 24, 131–133. [Google Scholar]
- Denny, H.R. Condylar fractures of the humerus in the dog; a review of 133 cases. J. Small Anim. Pract. 1983, 24, 185–197. [Google Scholar] [CrossRef]
- Stambaugh, J.E.; Morshead, D. Kirschner Wire Fixation of Lateral Humeral Condylar Fractures in Small Dogs. Vet. Surg. 1984, 13, 1–5. [Google Scholar]
- Lewis, D.G.; Johnson, M.P. A technique for fixation of intercondylar humeral fractures in immature small dogs. J. Small Anim. Pract. 1981, 22, 293–299. [Google Scholar]
- Guille, A.E.; Lewis, D.D.; Anderson, T.P.; Beaver, D.P.; Carrera-Justiz, S.C.; Thompson, M.S.; Wheeler, J.L. Evaluation of surgical repair of humeral condylar fractures using self-compressing orthofix pins in 23 dogs. Vet. Surg. 2004, 33, 314–322. [Google Scholar] [CrossRef]
- Rochereau, P.; Diop, A.; Maurel, N.; Bernarde, A. Biomechanical comparison of 4.0-mm short-threaded cannulated screws and 4.0-mm short-threaded cancellous screws in a canine humeral condylar fracture model. Vet. Surg. 2012, 41, 712–719. [Google Scholar] [CrossRef]
- Cook, J.L.; Tomlinson, J.L.; Reed, A.L. Fluoroscopically Guided Closed Reduction and Internal Fixation of Fractures of the Lateral Portion of the Humeral Condyle: Prospective Clinical Study of the Technique and Results in Ten Dogs. Vet. Surg. 1999, 28, 315–321. [Google Scholar] [CrossRef] [PubMed]
- Kvale, E.; Kalmukov, I.; Grassato, L.; Kalff, S.; Solano, M. Epicondylar plate fixation of humeral condylar fractures in immature French bulldogs: 45 cases (2014–2020). J. Small Anim. Pract. 2022, 63, 532–541. [Google Scholar] [CrossRef]
- Quinn, R.J.; Hoglund, O.V.; Hutchinson, D.J.; Opande, L.; Lim, E.; Birgersson, U.; Granskog, V.; Malkoch, M. Adjunctive fixation of the humeral epicondyle in a lateral condylar fracture model: Ex vivo comparison of pins and plates with a novel composite (AdhFix). Vet. Surg. 2024, 53, 311–319. [Google Scholar] [CrossRef]
- Au Yong, J.A.; Lewis, D.D.; Evans, R.B.; Kim, S.E.; Pozzi, A. Retrospective evaluation of the efficacy of minimally invasive, fluoroscopic-assisted reduction and stabilisation of unicondylar humeral fractures. Aust. Vet. J. 2018, 96, 302–307. [Google Scholar] [CrossRef] [PubMed]
- Easter, T.G.; Bilmont, A.; Pink, J.; Oxley, B. Accuracy of three-dimensional printed patient-specific drill guides for treatment of canine humeral intracondylar fissure. Vet. Surg. 2020, 49, 363–372. [Google Scholar] [CrossRef]
- Kim, J.Y.; Kwak, H.H.; Woo, H.M.; Kim, J. Enhancing the Accuracy of Pedicle Screw Placement Using 3D-Printed Screw-Guiding Techniques in the Lumbosacral Region for Small Breed Dogs: A Cadaveric Study. Animals 2024, 15, 14. [Google Scholar] [CrossRef]
- Wong, K.C. 3D-printed patient-specific applications in orthopedics. Orthop. Res. Rev. 2016, 8, 57–66. [Google Scholar] [CrossRef]
- Gauci, M.O. Patient-specific guides in orthopedic surgery. Orthop. Traumatol. Surg. Res. 2022, 108, 103154. [Google Scholar] [CrossRef]
- Nicholas, G.; Vaida, G.; Kevin, T.; Lance, J.W.; Caroline, A.G. A Practical Guide to Image Processing in the Creation of 3D Models for Orthopedics. Tech. Orthop. 2016, 31, 153–163. [Google Scholar] [CrossRef]
- Tobias, K.M.; Johnston, S.A. Fracture of the Humerus. In Veterinary Surgery, Small Animal, 2nd ed.; Tobias, K.M., Johnston, S.A., Eds.; Saunders: Philadelphia, PA, USA, 2018; Volume 1, pp. 820–836. [Google Scholar]
- Bardet, J.F. Fractures of the Humerus in Dogs and Cats A Retrospective Study of 130 Cases. Vet. Surg. 1983, 12, 73–77. [Google Scholar] [CrossRef]
- Cheng, C. Humeral fractures. Essent. Emerg. Trauma 2012, 22, 454–464. [Google Scholar]
- Nortje, J.; Bruce, W.J.; Worth, A.J. Surgical repair of humeral condylar fractures in New Zealand working farm dogs—Long-term outcome and owner satisfaction. N. Z. Vet. J. 2015, 63, 110–116. [Google Scholar] [CrossRef]
- Villamil, C.S.; Phillips, A.S.J.; Pegram, C.L.; O’Neill, D.G.; Meeson, R.L. Impact of breed on canine humeral condylar fracture configuration, surgical management, and outcome. Vet. Surg. 2020, 49, 639–647. [Google Scholar] [CrossRef]
- Little, D.J.M.; Young, D.J.D.; Ferris, K.K.; Berry, C.M. Incomplete Ossification of the Humeral Condyle in Spaniels. Vet. Surg. 1994, 23, 475–487. [Google Scholar] [CrossRef]
- Morgan, O.D.; Reetz, J.A.; Brown, D.C.; Tucker, S.M.; Mayhew, P.D. Complication rate, outcome, and risk factors associated with surgical repair of fractures of the lateral aspect of the humeral condyle in dogs. Vet. Comp. Orthop. Traumatol. 2008, 21, 400–405. [Google Scholar] [CrossRef] [PubMed]
- Moores, A.P.; Tivers, M.S.; Grierson, J. Clinical assessment of a shaft screw for stabilization of the humeral condyle in dogs. Vet. Comp. Orthop. Traumatol. 2014, 27, 179–185. [Google Scholar] [CrossRef] [PubMed]
- Perry, K.L.; Bruce, M.; Woods, S.; Davies, C.; Heaps, L.A.; Arthurs, G.I. Effect of fixation method on postoperative complication rates after surgical stabilization of lateral humeral condylar fractures in dogs. Vet. Surg. 2015, 44, 246–255. [Google Scholar] [CrossRef]
- Roelofs, L.J.M.; Assink, N.; Kraeima, J.; Ten Duis, K.; Doornberg, J.N.; de Vries, J.P.M.; Meesters, A.M.L.; FFA, I.J. Clinical Application of 3D-Assisted Surgery Techniques in Treatment of Intra-Articular Distal Radius Fractures: A Systematic Review in 718 Patients. J. Clin. Med. 2024, 13, 7296. [Google Scholar] [CrossRef]
- Punyaratabandhu, T.; Liacouras, P.C.; Pairojboriboon, S. Using 3D models in orthopedic oncology: Presenting personalized advantages in surgical planning and intraoperative outcomes. 3D Print. Med. 2018, 4, 12. [Google Scholar] [CrossRef]
- Ejnisman, L.; Gobbato, B.; de Franca Camargo, A.F.; Zancul, E. Three-Dimensional Printing in Orthopedics: From the Basics to Surgical Applications. Curr. Rev. Musculoskelet. Med. 2021, 14, 1–8. [Google Scholar] [CrossRef]
- Trebacz, P.; Frymus, J.; Barteczko, A.; Pawlik, M.; Kurkowska, A.; Czopowicz, M. A 3D Printed Anatomically Pre-Contoured Plate for the Treatment of Y-T Humeral Condylar Fractures: A Feline Cadaveric Study. Animals 2024, 14, 537. [Google Scholar] [CrossRef] [PubMed]
- Si, J.; Zhang, C.; Tian, M.; Jiang, T.; Zhang, L.; Yu, H.; Shi, J.; Wang, X. Intraoral Condylectomy with 3D-Printed Cutting Guide versus with Surgical Navigation: An Accuracy and Effectiveness Comparison. J. Clin. Med. 2023, 12, 3816. [Google Scholar] [CrossRef] [PubMed]
- Barnes, D.M.; Morris, A.P.; Anderson, A.A. Defining a safe corridor for transcondylar screw insertion across the canine humeral condyle: A comparison of medial and lateral surgical approaches. Vet. Surg. 2014, 43, 1020–1031. [Google Scholar] [CrossRef] [PubMed]
- Altwal, J.; Wilson, C.H.; Griffon, D.J. Applications of 3-dimensional printing in small-animal surgery: A review of current practices. Vet. Surg. 2022, 51, 34–51. [Google Scholar] [CrossRef]
- Marturello, D.M.; James, J.C.; Perry, K.L.; Dejardin, L.M. Accuracy of anatomic 3-dimensionally printed canine humeral models. Vet. Surg. 2023, 52, 116–126. [Google Scholar] [CrossRef]




Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Srikusalanukul, J.; Chantarapanich, N.; Thitiyanaporn, C. Effectiveness of Custom-Designed 3D-Printed Drill Guides in the Treatment of Lateral Humeral Condylar Fractures in a French Bulldog Bone Model. Vet. Sci. 2025, 12, 888. https://doi.org/10.3390/vetsci12090888
Srikusalanukul J, Chantarapanich N, Thitiyanaporn C. Effectiveness of Custom-Designed 3D-Printed Drill Guides in the Treatment of Lateral Humeral Condylar Fractures in a French Bulldog Bone Model. Veterinary Sciences. 2025; 12(9):888. https://doi.org/10.3390/vetsci12090888
Chicago/Turabian StyleSrikusalanukul, Jirawat, Nattapon Chantarapanich, and Chaiyakorn Thitiyanaporn. 2025. "Effectiveness of Custom-Designed 3D-Printed Drill Guides in the Treatment of Lateral Humeral Condylar Fractures in a French Bulldog Bone Model" Veterinary Sciences 12, no. 9: 888. https://doi.org/10.3390/vetsci12090888
APA StyleSrikusalanukul, J., Chantarapanich, N., & Thitiyanaporn, C. (2025). Effectiveness of Custom-Designed 3D-Printed Drill Guides in the Treatment of Lateral Humeral Condylar Fractures in a French Bulldog Bone Model. Veterinary Sciences, 12(9), 888. https://doi.org/10.3390/vetsci12090888






