Endoscopic Retrieval of Esophageal and Gastric Foreign Bodies in Cats and Dogs: A Retrospective Study of 92 Cases
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Collection
2.2. Statistical Analysis
3. Results
3.1. Animals
3.2. Clinical Signs
3.3. FBs (Type, Number, and Localization)
3.3.1. Dogs
3.3.2. Cats
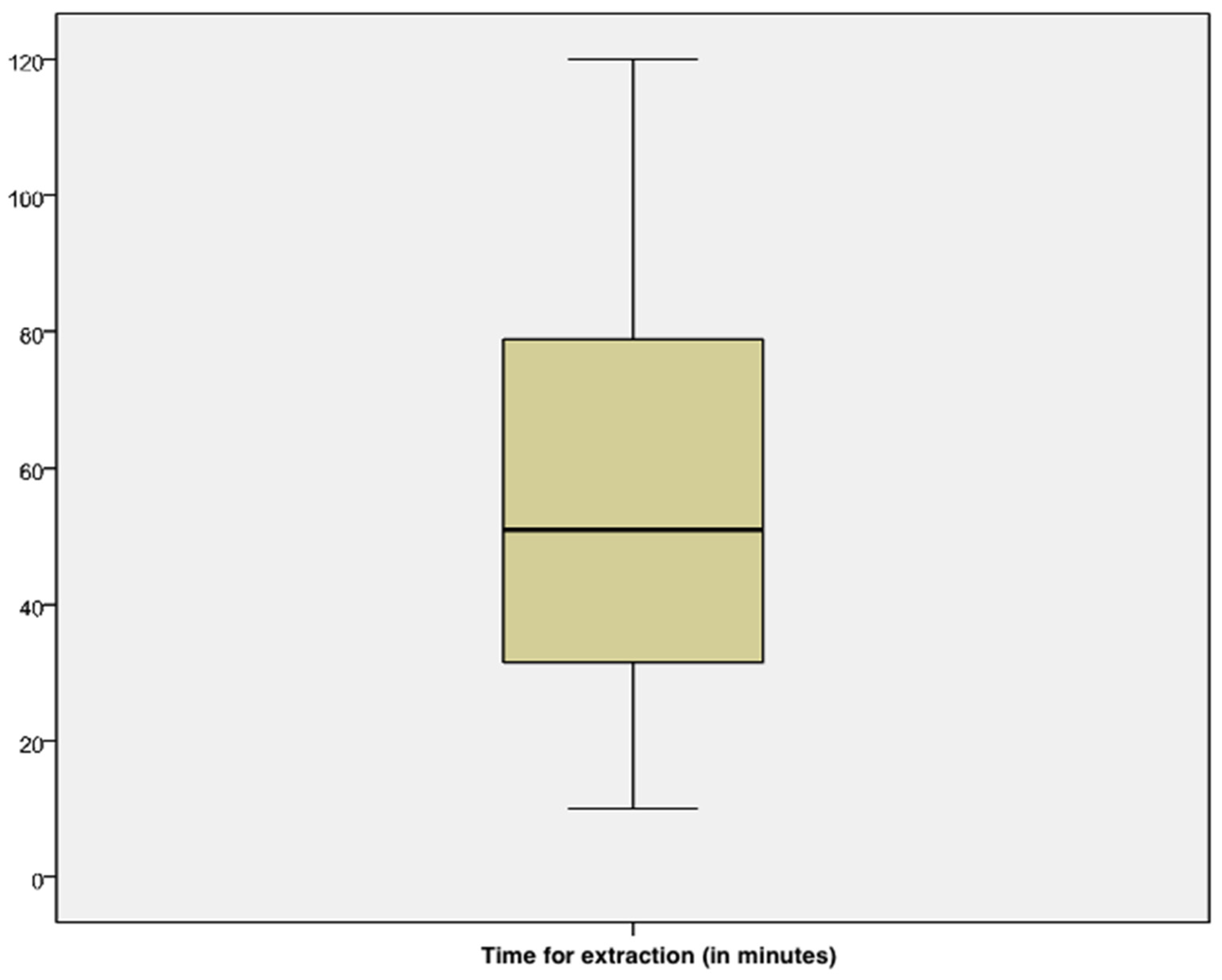
3.4. Endoscopic Removal (Operator’s Experience, Endoscopic Instruments, Timing for the Extraction, and Success Rate)
3.5. Complications
3.6. Univariate Analysis
3.7. Multivariate Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gianella, P.; Pfammatter, N.S.; Burgener, I.A. Oesophageal and gastric endoscopic foreign body removal: Complications and follow-up of 102 dogs. J. Small Anim. Pract. 2009, 50, 649–654. [Google Scholar] [CrossRef]
- Brisson, B.A.; Wainberg, S.H.; Malek, S.; Reabel, S.; Defarges, A.; Sears, W.C. Risk factors and prognostic indicators for surgical outcome of dogs with esophageal foreign body obstructions. J. Am. Vet. Med. Assoc. 2018, 252, 301–308. [Google Scholar] [CrossRef]
- Di Palma, C.; Pasolini, M.P.; Navas, L.; Campanile, A.; Lamagna, F.; Fatone, G.; Micieli, F.; Esposito, C.; Donnarumma, D.; Uccello, V.; et al. Endoscopic and Surgical Removal of Gastrointestinal Foreign Bodies in Dogs: An Analysis of 72 Cases. Animals 2022, 12, 1376. [Google Scholar] [CrossRef] [PubMed]
- Wood, A.N.; Gallagher, A.E. Survey of Instruments and Techniques for Endoscopic Retrieval of Esophageal and Gastric Foreign Bodies in Cats and Dogs. Top. Companion Anim. Med. 2021, 45, 100555. [Google Scholar] [CrossRef] [PubMed]
- Barash, N.R.; Lashnits, E.; Kern, Z.T.; Tolbert, M.K.; Lunn, K.F. Outcomes of esophageal and gastric bone foreign bodies in dogs. J. Vet. Intern. Med. 2022, 36, 500–507. [Google Scholar] [CrossRef] [PubMed]
- Tams, T.R.; Rawlings, C.A. Endoscopic Removal of Gastrointestinal Foreign Bodies. In Small Animal Endoscopy, 3rd ed.; Elsevier: Berkeley, CA, USA, 2010. [Google Scholar]
- Lolli, C.; Marenzoni, M.L.; Strona, P.; Lappo, P.; Etiang, P.; Diverio, S. Infections and risk factors for livestock with species of Anaplasma, Babesia and Brucella under semi-nomadic rearing in Karamoja Region, Uganda. Trop. Anim. Health Prod. 2016, 48, 603–611. [Google Scholar] [CrossRef]
- Jones, S.; Friedenberg, S.G.; Callard, J.; Abernathy, L.; Guillaumin, J. Successful Surgical Correction of a Mesenteric Volvulus with Concurrent Foreign Body Obstruction in Two Puppies. J. Am Anim. Hosp. Assoc. 2017, 53, 297–303. [Google Scholar] [CrossRef]
- Bottero, E. Chapter 15 Functional anomalies. In Gastroenterology of the Dog and Cat, 1st ed.; Poletto Editore: Milan, Italy, 2013. [Google Scholar]
- Binvel, M.; Poujol, L.; Peyron, C.; Dunie-Merigot, A.; Bernardin, F. Endoscopic and surgical removal of oesophageal and gastric fishhook foreign bodies in 33 animals. J. Small Anim. Pract. 2018, 59, 45–49. [Google Scholar] [CrossRef]
- Pratt, C.L.; Reineke, E.L.; Drobatz, K.J. Sewing needle foreign body ingestion in dogs and cats: 65 cases (200–2012). J. Am. Vet. Med. Assoc. 2014, 245, 302–308. [Google Scholar] [CrossRef]
- Coleman, A.E.; Merola, V. Clinical signs associated with ingestion of black walnut tree (Juglans nigra), wood, nuts, and hulls in dogs: 93 cases (2001–2012). J. Am. Vet. Med. Assoc. 2016, 248, 195–200. [Google Scholar] [CrossRef]
- Garneau, M.; Mccarthey, R.J. Multiple magnetic gastrointestinal foreign bodies in a dog. J Am. Vet. Med. Assoc. 2015, 246, 537–539. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, J.; Yamashita, M. Esophageal electrochemical burns due to button type lithium batteries in dogs. Vet. Hum. Toxicol. 1998, 40, 193–196. [Google Scholar] [PubMed]
- Fitzgerald, K.T.; Bronstein, A.C. Polyurethane adhesive ingestion. Top. Companion Anim. Med. 2013, 28, 28–31. [Google Scholar] [CrossRef] [PubMed]
- Ryan, W.W.; Greene, R.W. The conservative management of esophageal foreign bodies and their complications: A review of 66 cases in dogs and cats. J. Am. Anim. Hosp. Assoc. 1975, 11, 243–249. [Google Scholar]
- Hayes, G. Gastrointestinal foreign bodies in dogs and cats: A retrospective study of 208 cases. J. Small Anim. Pract. 2009, 50, 576–583. [Google Scholar] [CrossRef]
- Hobday, M.M.; Pachtinger, G.E.; Drobatz, K.J.; Syring, R.S. Linear versus non-linear gastrointestinal foreign bodies in 499 dogs: Clinical presentation, management, and short-term outcome. J. Small Anim. Pract. 2014, 55, 560–565. [Google Scholar] [CrossRef]
- Tello, L.; Perez-Freytes, R. Fluid and Electrolyte Therapy During Vomiting and Diarrhea. Vet. Clin. N. Am. Small Anim. Pract. 2017, 47, 505–519. [Google Scholar] [CrossRef]
- Boag, A.K.; Coe, R.J.; Martinez, T.A.; Hughes, D. Acid-base and electrolyte abnormalities in dogs with gastrointestinal foreign bodies. J. Vet. Intern. Med. 2005, 19, 816–821. [Google Scholar] [CrossRef]
- Deroy, C.; Corcuff, J.B.; Billen, F.; Hamaide, A. Removal of oesophageal foreign bodies: Comparison between oesophagoscopy and oesophagotomy in 39 dogs. J. Small Anim. Pract. 2015, 56, 613–617. [Google Scholar] [CrossRef]
- Moore, A.H. Removal of oesophageal foreign bodies in dogs: Use of the fluoroscopic method and outcome. J. Small Anim. Pract. 2001, 42, 227–230. [Google Scholar] [CrossRef]
- Bottero, E.; Bertoncello, D.; De Lorenzi, D. A retrospective study about 23 osseus esophageal foreign bodies in the dog and the cat treated endoscopically. Veterinaria 2007, 21, 17–23. [Google Scholar]
- Bekkerman, M.; Sachdev, A.H.; Andrade, J.; Twersky, Y.; Iqbel, S. Endoscopic management of foreign bodies in the gastrointestinal tract: A Review of the literature. Gastroenterol. Res. Pract. 2016, 2016, 5078654. [Google Scholar] [CrossRef] [PubMed]
- Sterman, A.A.; Mankin, K.M.T.; Ham, K.M.; Cook, A.K. Likelihood and outcome of esophageal perforation secondary to esophageal foreign body in dogs. J. Am. Vet. Med. Assoc. 2018, 253, 1053–1056. [Google Scholar] [CrossRef] [PubMed]
- Adamama-Moraitou, K.K.; Rallis, T.S.; Prassinos, N.N.; Galatos, A.D. Benign esophageal stricture in the dog and cat: A retrospective study of 20 cases. Can. J. Vet. Res. 2002, 66, 55–59. [Google Scholar]
- Xu, G.; Chen, Y.C.; Chen, J.; Jia, D.S.; Wu, Z.B.; Li, L. Management of oesophageal foreign bodies in children: A 10-year retrospective analysis from a tertiary care center. BMC Emerg. Med. 2022, 22, 166. [Google Scholar] [CrossRef]


| Breeds | Frequency | Percent |
|---|---|---|
| Mixed-breed dog | 23/86 | 26.7% |
| German Shepherd | 6/86 | 7% |
| Bernese Mountain Dog | 5/86 | 5.8% |
| Dachshund, Cocker Spaniel, Jack Russel Terrier | 4/86 | 4.7% |
| Beagle, Boxer, Golden Retriever, Labrador Retriever, Hound | 3/86 | 3.5% |
| Great Dane, French Bulldog, Bullmastiff, Chihuahua, English Setter, Spitz | 2/86 | 2.3% |
| Poodle, Akita Inu, Border Collie, Corso, Dobermann, Fox Terrier, Husky, Maremma Sheepdog, Belgian Shepherd, Pekingese, Schnauzer, Springer Spaniel, West Highland White Terrier | 1/86 | 1.2% |
| Gastrointestinal Disorders | Frequency | Percent |
|---|---|---|
| Vomiting | 24/92 | 26.1% |
| Anorexia | 3/92 | 3.3% |
| Abdominal pain | 3/92 | 3.3% |
| Inappetence | 2/92 | 2.2% |
| Dysphagia | 2/92 | 2.2% |
| Pica | 1/92 | 1.1% |
| Regurgitation | 1/92 | 1.1% |
| Unspecific Clinical Signs | Frequency | Percent |
| Depression | 4/92 | 4.4% |
| Congestion of the mucosae membranes | 2/92 | 2.2% |
| Weight loss | 2/92 | 2.2% |
| Ataxia | 1/92 | 1.1% |
| Tremors | 1/92 | 1.1% |
| Polyuria and polydipsia | 1/92 | 1.1% |
| Tachycardia | 1/92 | 1.1% |
| Tachypnea | 1/92 | 1.1% |
| Respiratory Disorder | Frequency | Percent |
| Dyspnea | 2/92 | 2.2% |
| Cough | 1/92 | 1.1% |
| Stridor | 1/92 | 1.1% |
| Localization | Frequency | Percent |
|---|---|---|
| Cervical esophagus | 1/86 | 1.2% |
| Thoracic esophagus | 9/86 | 10.5% |
| Stomach (fondus) | 10/86 | 11.6% |
| Stomach (body) | 28/86 | 32.6% |
| Stomach (antrum) | 16/86 | 18.6% |
| Thoracic esophagus + Stomach (body) | 1/86 | 1.2% |
| Stomach (fondus) + Stomach (body) | 14/86 | 16.3% |
| Stomach (fondus) + Stomach (antrum) | 1/86 | 1.2% |
| Stomach (body) + Stomach (antrum) | 2/86 | 2.3% |
| Stomach (antrum) + Duodenum | 2/86 | 2.3% |
| Thoracic esophagus + Stomach (fundus) + Stomach (body) | 1/86 | 1.2% |
| Stomach (fundus) + Stomach (body) + Stomach (antrum) | 1/86 | 1.2% |
| Signalment | Clinical Signs | FBs (Number, Type, and Localization) | Endoscopic Removal | |
|---|---|---|---|---|
| 1. | Domestic Shorthair cat, female neutered, 24 months | Ingestion of FBs was seen by owners | One needle (penetrating FB) in the stomach (body) | Operator’s experience: expert Single endoscopic instrument used (Alligator forceps) Extraction time: 79 min. Successful removal Complications: minor (gastritis) |
| 2. | Domestic Shorthair cat, female neutered, 6 months | Gastrointestinal disorders: abdominal pain | One shoelace (non-penetrating FB) in the stomach (body) | Operator’s experience: expert Single endoscopic instrument used (Grasping forceps) Extraction time: 19 min. Successful removal Complications: minor (gastritis) |
| 3. | Domestic Shorthair cat, female, 12 months | Gastrointestinal disorders: vomiting | One thread (non-penetrating) in the stomach (body) | Operator’s experience: novice Single endoscopic instrument used (Grasping forceps) Extraction time: 26 min. Successful removal Complications: minor (gastritis) |
| 4. | Bengal cat, female, 12 months | Ingestion of FBs was seen by owners | One needle (penetrating) in the stomach (body) | Operator’s experience: middle Single endoscopic instrument used (Alligator forceps) Extraction time: 54 min. Successful removal Complications: minor (gastritis) |
| 5. | Domestic Shorthair cat, female, 24 months | Ingestion of FBs was seen by owners | One stuffed toy (non-penetrating) in the stomach (antrum) | Operator’s experience: middle Single endoscopic instrument used (Polypectomy snare) Extraction time: 52 min. Successful removal Complications: minor (gastritis) |
| 6. | Domestic Shorthair cat, female, 48 months | Ingestion of FBs was seen by owners | One thread (non-penetrating) in the stomach (body) | Operator’s experience: middle Single endoscopic instrument used (Alligator forceps) Extraction time: 15 min. Successful removal Complications: minor (gastritis) |
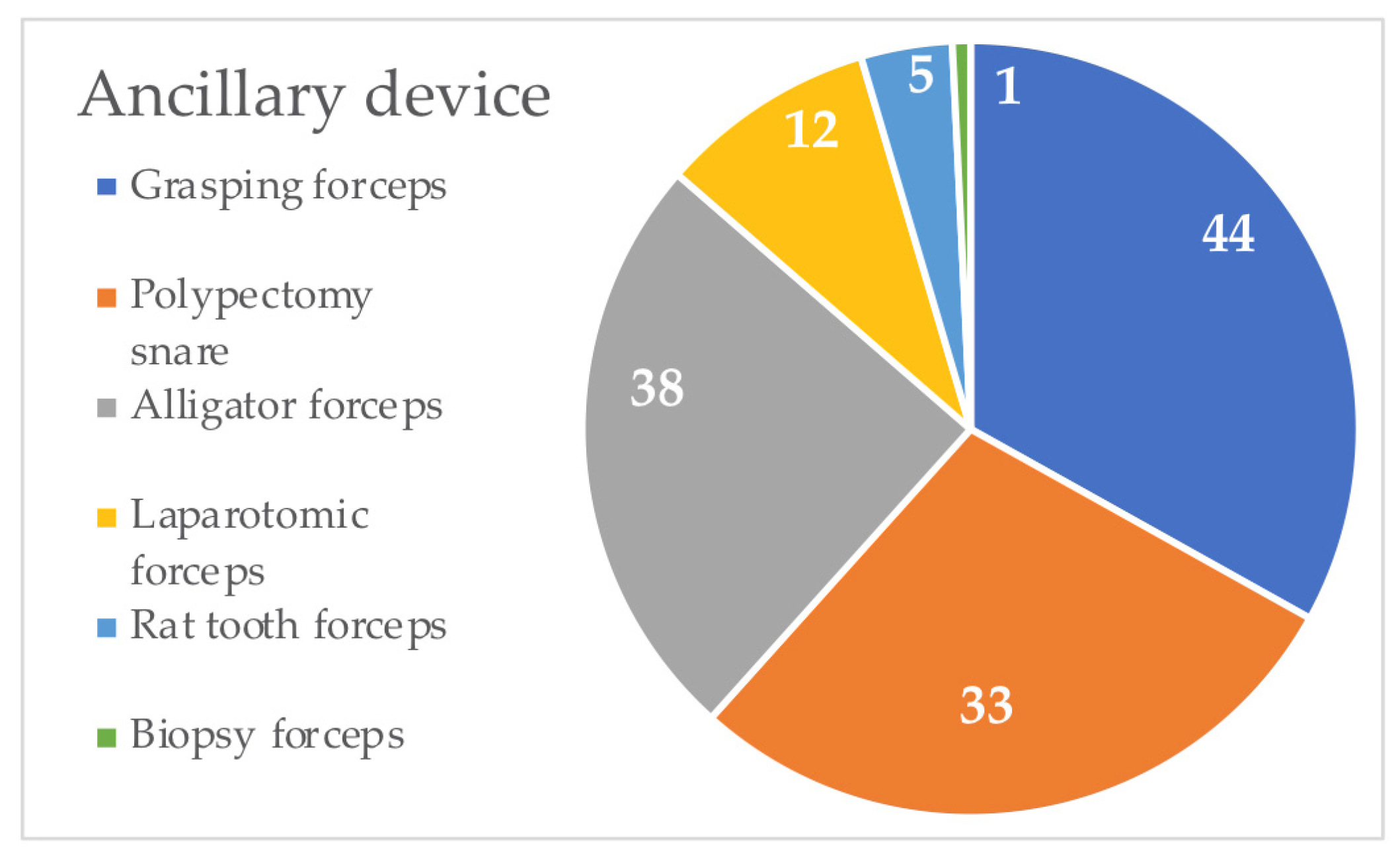
| Ancillary Devices | Frequency |
|---|---|
| Grasping forceps | 44/92 |
| Polypectomy snare | 33/92 |
| Alligator forceps | 38/92 |
| Laparotomic forceps | 12/92 |
| Rat tooth forceps | 5/92 |
| Biopsy forceps | 1/92 |
| Signalment | Clinical Signs | FBs (Type, Number, and Localization) | Endoscopic Removal | |
|---|---|---|---|---|
| 1. | Breed: mixed breed Size: small breed Sex: male Age: 180 months | Ingestion of FBs was seen by owners | Type: aluminum foil for aliments, synthetic casing for aliments FBs number: 2 Localization: thoracic esophagus | Operator’s experience: expert Endoscopic instruments used: rat tooth forceps and laparotomic forceps Extraction time: 88 min. Successful removal Complications: no |
| 2. | Breed: Spitz Size: small breed Sex: female Age: 60 months | Ingestion of FBs was seen by owners | Type: cookie FBs number: 1 Localization: thoracic esophagus | Operator’s experience: expert Endoscopic instruments used: alligator forceps and laparotomic forceps Extraction time: 53 min. Successful removal Complications: no |
| 3. | Breed: Bullmastiff Size: large breed Sex: male Age: 60 months | Unspecific clinical signs: weight loss Gastrointestinal signs: vomiting | Type: rag FBs number: 1 Localization: thoracic esophagus | Operator’s experience: expert Endoscopic instruments used: alligator forceps and laparotomic forceps Extraction time: 48 min. Successful removal Complications: minor (esophagitis) |
| 4. | Breed: West Highland Withe Terrier Size: small breed Sex: male Age: 168 months | Respiratory disorders: dyspnea | Type: apple core FBs number: 1 Localization: thoracic esophagus | Operator’s experience: middle Endoscopic instruments used: alligator forceps and laparotomic forceps Time extraction: 45 min. Successful removal Complications: no |
| 5. | Species: dog Breed: mixed breed Size: small breed Sex: male Age: 120 months | Ingestion of FBs was seen by owners | Type: cartilaginous tissue FBs number: 1 Localization: thoracic esophagus | Operator’s experience: expert Endoscopic instruments used: laparotomic forceps Time extraction: 30 min. Successful removal Complications: no |
| 6. | Species: dog Breed: mixed breed Size: small breed Sex: male Age: 24 months | Gastrointestinal disorders: inappetence, regurgitation | Type: bone FBs number: 1 Localization: thoracic esophagus | Operator’s experience: middle Endoscopic instruments used: laparotomic forceps Time extraction: 56 min. Successful removal Complications: major (perforation, pneumothorax, death) |
| 7. | Species: dog Breed: Dachshund Size: small breed Sex: female Age: 204 months | Ingestion of FBs was seen by owners | Type: bone FBs number: 1 Localization: thoracic esophagus | Operator’s experience: middle Endoscopic instruments used: alligator forceps Time extraction: 29 min. Successful removal Complications: no |
| 8. | Species: dog Breed: mixed breed Size: small breed Sex: male Age: 192 months | Unspecific clinical signs: depression, polyuria, polydipsia Gastrointestinal disorders: anorexia, vomiting | Type: bone FBs number: 1 Localization: thoracic esophagus | Operator’s experience: expert Endoscopic instruments used: grasping forceps, laparotomic forceps Time extraction: 50 min. Successful removal Complications: major (erosion/ulceration, needs to PEG) |
| 9. | Species: Dog Breed: Mixed breed Size: Small breed Sex: Female Age: 180 months | Respiratory disorders: Cough, dyspnea | Type: Bone FBs number: 1 Localization: Thoracic esophagus | Operator’s experience: Middle Endoscopic instruments used: Laparotomic forceps Time extraction: 19 min. Successful removal Complications: Minor (esophagitis) |
| 10 | Species: dog Breed: Jack Russel Terrier Size: small breed Sex: male Age: 60 months | Gastrointestinal disorders: dysphagia | Type: bone FBs number: 1 Localization: thoracic esophagus | Operator’s experience: novice Endoscopic instruments used: polypectomy snare Time extraction: 86 min. Successful removal Complications: major (erosion/ulceration) |
| 11 | Species: dog Breed: Labrador Retriever Size: large breed Sex: male Age: 4 months | Ingestion of FBs was seen by owners | Type: fishhook FBs number: 1 Localization: cervical esophagus | Operator’s experience: middle Endoscopic instruments used: alligator forceps Time extraction: 79 min. Successful removal Complications: minor (esophagitis) |
| 12. | Species: dog Breed: mixed breed Size: small breed Sex: male Age: 6 months | Gastrointestinal disorders: dysphagia, vomiting | Type: wood FBs number: 1 Localization: thoracic esophagus | Operator’s experience: middle Endoscopic instruments used: polypectomy snare and grasping forceps Time extraction: 89 min. Successful removal Complications: minor (esophagitis) |
| Variable | p Value ≤ 0.05 | OR > 1 | 95% IC |
|---|---|---|---|
| Good time | 0.035 | 7.234 | 0.884–59.220 |
| Variable | p Value ≤ 0.05 | OR < 1 | 95% IC |
| Medium breed | 0.048 | 0.843 | 0.762–0.933 |
| Polypectomy snare | 0.001 | 0.094 | 0.019–0.466 |
| Grasping forceps | 0.016 | 0.169 | 0.034–0.832 |
| Multiple forceps | 0.002 | 0.111 | 0.022–0.551 |
| Excellent time | 0.048 | 0.843 | 0.762–0.933 |
| Not acceptable time | 0.000 | 0.067 | 0.012–0.363 |
| Variable | p Value ≤ 0.2 | OR > 1 | 95% IC |
| Expert operator | 0.148 | 3.094 | 0.628–15.247 |
| Variable | p Value ≤ 0.2 | OR < 1 | 95% IC |
| Large breed | 0.169 | 0.417 | 0.117–1.489 |
| Adult | 0.151 | 0.393 | 0.106–1.450 |
| Thoracic esophagus | 0.193 | 0.864 | 0.793–0.942 |
| Middle operator | 0.175 | 0.413 | 0.112–1.525 |
| Laparotomic forceps | 0.171 | 0.863 | 0.790–0.941 |
| Acceptable time | 0.064 | 0.311 | 0.086–1.122 |
| Variable | p Value ≤ 0.05 | OR > 1 | 95% IC |
|---|---|---|---|
| Puppy | 0.002 | 8.375 | 1.889–37.136 |
| Expert operator | 0.005 | 4.083 | 1.490–11.188 |
| Successful removal | 0.048 | 1.373 | 1.202–1.568 |
| Variable | p Value ≤ 0.05 | OR < 1 | 95% IC |
| Adult | 0.024 | 0.294 | 0.098–0.885 |
| Unspecific clinical signs | 0.048 | 0.728 | 0.638–0.832 |
| Polypectomy snare | 0.047 | 0.314 | 0.096–1.026 |
| Variable | p Value ≤ 0.2 | OR > 1 | 95% IC |
| Species | 0.121 | 3.526 | 0.658–18.910 |
| Small breed | 0.116 | 2.160 | 0.818–5.705 |
| Older | 0.161 | 2.250 | 0.711–7.124 |
| Variable | p Value ≤ 0.2 | OR < 1 | 95% IC |
| Large breed | 0.141 | 0.441 | 0.146–1.333 |
| Middle operator | 0.168 | 0.494 | 0.180–1.360 |
| Novice operator | 0.068 | 0.175 | 0.022–1.406 |
| Rat tooth forceps | 0.197 | 0.747 | 0.661–0.844 |
| Multiple forceps | 0.071 | 0.370 | 0.123–1.115 |
| Variable | p Value ≤ 0.05 | OR < 1 | 95% IC |
|---|---|---|---|
| Adult | 0.038 | 0.405 | 0.171–0.961 |
| Stomach (body) | 0.007 | 0.290 | 0.116–0.728 |
| Polypectomy snare | 0.047 | 0.413 | 0.172–0.995 |
| Variable | p Value ≤ 0.2 | OR > 1 | 95% IC |
| Older | 0.080 | 3.152 | 0.829–11.981 |
| Stomach (antrum) | 0.063 | 2.769 | 0.923–8.313 |
| GI clinical signs | 0.112 | 2.101 | 0.835–5.285 |
| Laparotomic forceps | 0.102 | 3.511 | 0.722–17.080 |
| Variable | p Value ≤ 0.2 | OR < 1 | 95% IC |
| Large breed | 0.123 | 0.505 | 0.211–1.210 |
| Penetrating FBs | 0.053 | 0.430 | 0.181–1.020 |
| Cervical esophagus | 0.199 | 0.374 | 0.286–0.487 |
| Grasping forceps | 0.067 | 0.451 | 0.191–1.064 |
| Outcome = Failure to Remove | |||
|---|---|---|---|
| Variable | p Value | OR | 95% IC |
| Polypectomy snare | 0.002 | 14.286 | 2.644–77.176 |
| Grasping forceps | 0.014 | 8.514 | 1.545–46.917 |
| Outcome = time excellent for extraction | |||
| Successful removal | 0.004 | 22.400 | 2.718–184.574 |
| Outcome = time excellent/good for extraction | |||
| Adult | 0.003 | 0.179 | 0.058–0.551 |
| Penetrating FBs | 0.010 | 0.241 | 0.081–0.713 |
| GI clinical signs | 0.033 | 3.517 | 1.107–11.171 |
| Polypectomy snare | 0.032 | 0.314 | 0.109–0.906 |
| Grasping forceps | 0.003 | 0.173 | 0.056–0.543 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maggi, G.; Tessadori, M.; Marenzoni, M.L.; Porciello, F.; Caivano, D.; Marchesi, M.C. Endoscopic Retrieval of Esophageal and Gastric Foreign Bodies in Cats and Dogs: A Retrospective Study of 92 Cases. Vet. Sci. 2023, 10, 560. https://doi.org/10.3390/vetsci10090560
Maggi G, Tessadori M, Marenzoni ML, Porciello F, Caivano D, Marchesi MC. Endoscopic Retrieval of Esophageal and Gastric Foreign Bodies in Cats and Dogs: A Retrospective Study of 92 Cases. Veterinary Sciences. 2023; 10(9):560. https://doi.org/10.3390/vetsci10090560
Chicago/Turabian StyleMaggi, Giulia, Mattia Tessadori, Maria Luisa Marenzoni, Francesco Porciello, Domenico Caivano, and Maria Chiara Marchesi. 2023. "Endoscopic Retrieval of Esophageal and Gastric Foreign Bodies in Cats and Dogs: A Retrospective Study of 92 Cases" Veterinary Sciences 10, no. 9: 560. https://doi.org/10.3390/vetsci10090560
APA StyleMaggi, G., Tessadori, M., Marenzoni, M. L., Porciello, F., Caivano, D., & Marchesi, M. C. (2023). Endoscopic Retrieval of Esophageal and Gastric Foreign Bodies in Cats and Dogs: A Retrospective Study of 92 Cases. Veterinary Sciences, 10(9), 560. https://doi.org/10.3390/vetsci10090560






