Clinical Outcomes in Dogs Undergoing Cholecystectomy via a Transverse Incision: A Meta−Analysis of 121 Animals Treated between 2011 and 2021
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Inclusion and Exclusion Criteria
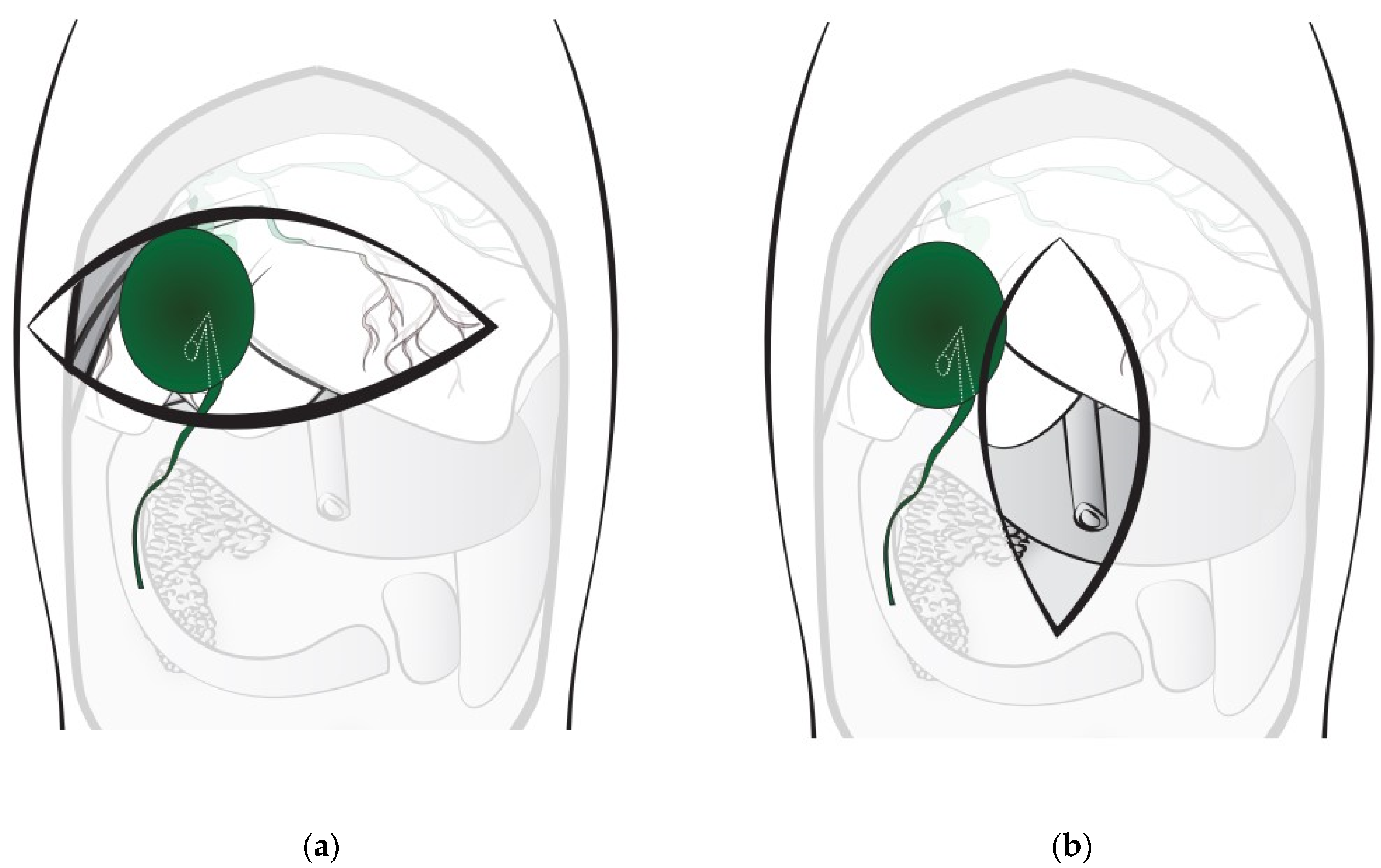
2.2. Surgical Procedures
2.3. Evaluation of Clinical Outcomes Associated with the Transverse Incision Approach
2.4. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Clinical Findings
3.3. Surgical Results
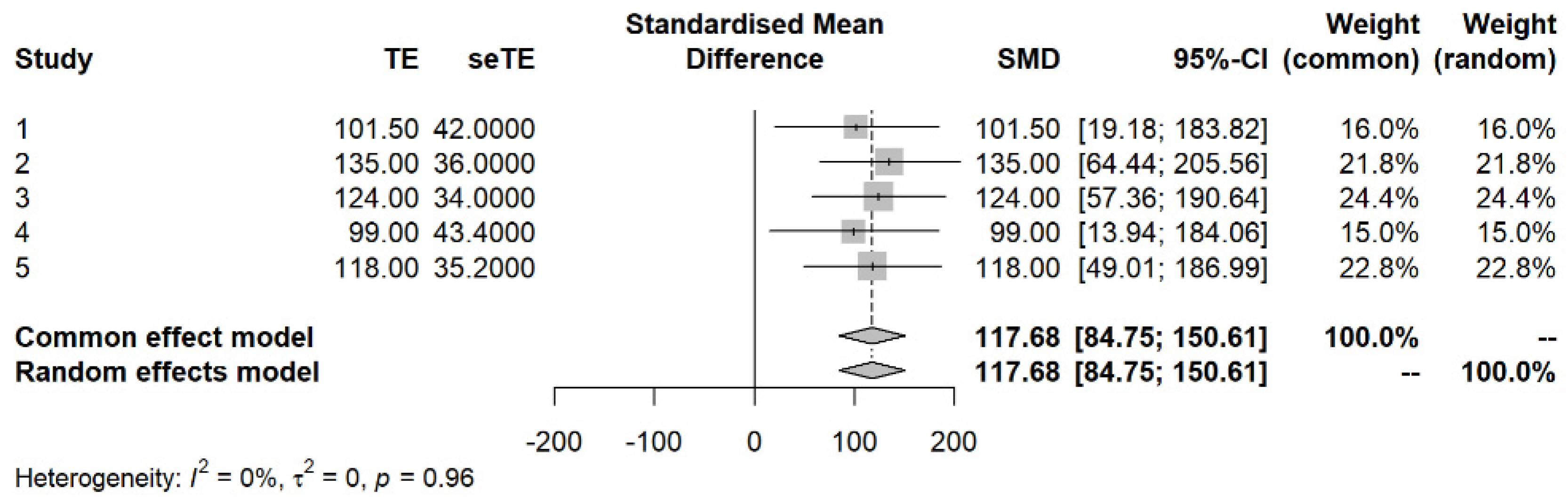
3.4. Meta−Analysis Results
3.5. Microbiology and Histologic Findings
3.6. Complications Related to Surgical Technique and Duration of Hospitalization
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Liu, R.; Liu, Q.; Zhang, X.-P. Prognosis control surgery. Hepatobiliary Surg. Nutr. 2021, 10, 126. [Google Scholar] [CrossRef]
- Epstein, N.E. Timing and prognosis of surgery for spinal epidural abscess: A review. Surg. Neurol. Int. 2015, 6 (Suppl. 19), S475. [Google Scholar] [CrossRef]
- Malek, S.; Sinclair, E.; Hosgood, G.; Moens, N.M.; Baily, T.; Boston, S.E. Clinical findings and prognostic factors for dogs undergoing cholecystectomy for gall bladder mucocele. Vet. Surg. 2013, 42, 418–426. [Google Scholar] [CrossRef]
- Putterman, A.B.; Selmic, L.E.; Kindra, C.; Duffy, D.J.; Risselada, M.; Phillips, H. Influence of normograde versus retrograde catheterization of bile ducts in dogs treated for gallbladder mucocele. Vet. Surg. 2021, 50, 784–793. [Google Scholar] [CrossRef]
- Kutsunai, M.; Kanemoto, H.; Fukushima, K.; Fujino, Y.; Ohno, K.; Tsujimoto, H. The association between gall bladder mucoceles and hyperlipidaemia in dogs: A retrospective case control study. Vet. J. 2014, 199, 76–79. [Google Scholar] [CrossRef]
- Le, V.H.; Smith, D.E.; Johnson, B.L. Conversion of Laparoscopic to Open Cholecystectomy in the Current Era of Laparosccopic Surgery. Am. Surg. 2012, 78, 1392–1395. [Google Scholar] [CrossRef]
- Antoniou, S.A.; Antoniou, G.A.; Koch, O.O.; Pointner, R.; Granderath, F.A. Meta-analysis of laparoscopic vs. open cholecystectomy in elderly patients. World J. Gastroenterol. 2014, 20, 17626. [Google Scholar] [CrossRef] [PubMed]
- Velanovich, V. Laparoscopic vs open surgery. Surg. Endosc. 2000, 14, 16–21. [Google Scholar] [CrossRef] [PubMed]
- Mayhew, P.D.; Mehler, S.J.; Radhakrishnan, A. Laparoscopic cholecystectomy for management of uncomplicated gall bladder mucocele in six dogs. Vet. Surg. 2008, 37, 625–630. [Google Scholar] [CrossRef] [PubMed]
- Simon, A.; Monnet, E. Laparoscopic cholecystectomy with single port access system in 15 dogs. Vet. Surg. 2020, 49 (Suppl. 1), O156–O162. [Google Scholar] [CrossRef] [PubMed]
- Scott, J.; Singh, A.; Mayhew, P.D.; Brad Case, J.; Runge, J.J.; Gatineau, M.; Kilkenny, J. Perioperative complications and outcome of laparoscopic cholecystectomy in 20 dogs. Vet. Surg. 2016, 45, O49–O59. [Google Scholar] [CrossRef]
- Brown, S.R.; Goodfellow, P.B. Transverse verses midline incisions for abdominal surgery. Cochrane Database Syst. Rev. 2005, 2005, CD005199. [Google Scholar] [CrossRef]
- Halm, J.A.; Lip, H.; Schmitz, P.I.; Jeekel, J. Incisional hernia after upper abdominal surgery: A randomised controlled trial of midline versus transverse incision. Hernia 2009, 13, 275–280. [Google Scholar] [CrossRef]
- Inaba, T.; Okinaga, K.; Fukushima, R.; Iinuma, H.; Ogihara, T.; Ogawa, F.; Iwasaki, K.; Tanaka, M.; Yamada, H. Prospective randomized study of two laparotomy incisions for gastrectomy: Midline incision versus transverse incision. Gastric Cancer 2004, 7, 167–171. [Google Scholar] [CrossRef]
- Arunkumar, S.; Dilipkumar, D.; Shivaprakash, B.V.; Bhagvantappa. Comparison of right flank and ventral midline approach for ovariohysterectomy in dogs. J. Entomol. Zool. Stud. 2017, 5, 2411–2416. [Google Scholar]
- Mehler, S.J.; Bennett, R.A. Canine extrahepatic biliary tract disease and surgery. Compend. Contin. Educ. Pract. Vet. 2006, 28, 302. [Google Scholar]
- Burns, B.R.; Hofmeister, E.H.; Brainard, B.M. Anesthetic complications in dogs undergoing hepatic surgery: Cholecystectomy versus non-cholecystectomy. Vet. Anaesth. Analg. 2014, 41, 186–190. [Google Scholar] [CrossRef] [PubMed]
- Kanai, H.; Hagiwara, K.; Nukaya, A.; Kondo, M.; Aso, T. Short-term outcome of laparoscopic cholecystectomy for benign gall bladder diseases in 76 dogs. J. Vet. Med. Sci. 2018, 80, 1747–1753. [Google Scholar] [CrossRef] [PubMed]
- Hattersley, R.; Downing, F.; Gibson, S.; Demetriou, J.; Elmenhorst, K.; Kulendra, N.; Mielke, B.; Woods, S. Impact of intra-operative hypotension on mortality rates and post-operative complications in dogs undergoing cholecystectomy. J. Small Anim. Pract. 2020, 61, 624–629. [Google Scholar] [CrossRef]
- Asakawa, M.; Fukuzawa, M.; Asakawa, M.G.; Flanders, J.A. Preoperative serum C-reactive protein concentration can be used to detect gallbladder rupture in dogs with gallbladder mucocele. Am. J. Vet. Res. 2021, 83, 23–32. [Google Scholar] [CrossRef]
- Woolson, R.F. Wilcoxon signed-rank test. In Wiley Encyclopedia of Clinical Trials; John Wiley and Sons: New York, NY, USA, 2007; pp. 1–3. [Google Scholar] [CrossRef]
- Chastant-Maillard, S.; Guillemot, C.; Feugier, A.; Mariani, C.; Grellet, A.; Mila, H. Reproductive performance and pre-weaning mortality: Preliminary analysis of 27,221 purebred female dogs and 204,537 puppies in France. Reprod. Domest. Anim. 2017, 52 (Suppl. 2), 158–162. [Google Scholar] [CrossRef] [PubMed]
- Jaffey, J.; Graham, A.; VanEerde, E.; Hostnik, E.; Alvarez, W.; Arango, J.; Jacobs, C.; DeClue, A. Gallbladder mucocele: Variables associated with outcome and the utility of ultrasonography to identify gallbladder rupture in 219 dogs (2007–2016). J. Vet. Intern. Med. 2018, 32, 195–200. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.; Choe, C.; Yoo, J.G.; Oh, S.I.; Jung, Y.; Cho, A.; Kim, S.; Do, Y.J. Major medical causes by breed and life stage for dogs presented at veterinary clinics in the Republic of Korea: A survey of electronic medical records. PeerJ 2018, 6, e5161. [Google Scholar] [CrossRef]
- Friesen, S.L.; Upchurch, D.A.; Hollenbeck, D.L.; Roush, J.K. Clinical findings for dogs undergoing elective and nonelective cholecystectomies for gall bladder mucoceles. J. Small Anim. Pr. 2021, 62, 547–553. [Google Scholar] [CrossRef] [PubMed]
- Lu, X.; Yang, Q.; Zhu, L.; Liu, L.; Tang, H.; Deng, J.; Lu, X. Correlation analysis of sacrococcygeal pressure and operation time in patients undergoing general anesthesia in the supine position. J. Int. Med. Res. 2021, 49, 300060520984595. [Google Scholar] [CrossRef]
- Daley, B.J.; Cecil, W.; Clarke, P.C.; Cofer, J.B.; Guillamondegui, O.D. How slow is too slow? Correlation of operative time to complications: An analysis from the Tennessee Surgical Quality Collaborative. J. Am. Coll. Surg. 2015, 220, 550–558. [Google Scholar] [CrossRef]
- Zou, X.; Patterson, T.A.; Divine, R.L.; Sadovova, N.; Zhang, X.; Hanig, J.P.; Paule, M.G.; Slikker, W., Jr.; Wang, C. Prolonged exposure to ketamine increases neurodegeneration in the developing monkey brain. Int. J. Dev. Neurosci. 2009, 27, 727–731. [Google Scholar] [CrossRef] [PubMed]
- Cheng, H.; Clymer, J.W.; Chen, B.P.-H.; Sadeghirad, B.; Ferko, N.C.; Cameron, C.G.; Hinoul, P. Prolonged operative duration is associated with complications: A systematic review and meta-analysis. J. Surg. Res. 2018, 229, 134–144. [Google Scholar] [CrossRef]
- Maaløe, N.; Aabakke, A.J.; Secher, N.J. Midline versus transverse incision for cesarean delivery in low-income countries. Int. J. Gynaecol. Obstet. 2014, 125, 1–2. [Google Scholar] [CrossRef]
- Mathai, M.; Hofmeyr, G.J.; Mathai, N.E. Abdominal surgical incisions for caesarean section. Cochrane Database Syst. Rev. 2013, 31, CD004453. [Google Scholar] [CrossRef]
- Saha, S.P.; Bhattarcharjee, N.; Das Mahanta, S.; Naskar, A.; Bhattacharyya, S.K. A randomized comparative study on modified Joel-Cohen incision versus Pfannenstiel incision for cesarean section. J. Turk. Ger. Gynecol. Assoc. 2013, 14, 28–34. [Google Scholar] [CrossRef] [PubMed]
- Costa, G.L.; Di Pietro, S.; Interlandi, C.; Leonardi, F.; Macrì, D.; Ferrantelli, V.; Macrì, F. Effect on physiological parameters and anaesthetic dose requirement of isoflurane when tramadol given as a continuous rate infusion vs a single intravenous bolus injection during ovariohysterectomy in dogs. PLoS ONE 2023, 18, e0281602. [Google Scholar] [CrossRef] [PubMed]
- Piegols, H.J.; Hayes, G.M.; Lin, S.; Singh, A.; Langlois, D.K.; Duffy, D.J. Association between biliary tree manipulation and outcome in dogs undergoing cholecystectomy for gallbladder mucocele: A multi-institutional retrospective study. Vet. Surg. 2021, 50, 767–774. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Data (n = 121) |
|---|---|
| Age, median (range) | |
| Sex | |
| Castrated males | 57 |
| Intact males | 6 |
| Spayed females | 47 |
| Intact females | 11 |
| Weight, median (range) | |
| <10 kg | 112 |
| 10 to <25 kg | 9 |
| ≥25 kg | 0 |
| Breeds | |
| Maltese | 25 |
| Shih Tzu | 19 |
| Poodle | 19 |
| Miniature Schnauzer | 14 |
| Yorkshire Terrier | 9 |
| Pomeranian | 6 |
| American Cocker Spaniel | 7 |
| Mixed | 5 |
| Miniature Pinscher | 4 |
| English Cocker Spaniel | 3 |
| Chihuahua | 3 |
| Dachshund | 1 |
| Siberian Husky | 1 |
| Pekinese | 1 |
| Japanese Chin | 1 |
| Bichon Frise | 1 |
| Belgian Malinois | 1 |
| Beagle | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chae, H.-K.; Jeong, J.-Y.; Lee, S.-Y.; Hwang, H.-M.; Shin, K.-I.; Park, J.-H.; Ji, S.-Y.; Hong, Y.-J. Clinical Outcomes in Dogs Undergoing Cholecystectomy via a Transverse Incision: A Meta−Analysis of 121 Animals Treated between 2011 and 2021. Vet. Sci. 2023, 10, 395. https://doi.org/10.3390/vetsci10060395
Chae H-K, Jeong J-Y, Lee S-Y, Hwang H-M, Shin K-I, Park J-H, Ji S-Y, Hong Y-J. Clinical Outcomes in Dogs Undergoing Cholecystectomy via a Transverse Incision: A Meta−Analysis of 121 Animals Treated between 2011 and 2021. Veterinary Sciences. 2023; 10(6):395. https://doi.org/10.3390/vetsci10060395
Chicago/Turabian StyleChae, Hyung-Kyu, Ju-Yeon Jeong, Se-Yoon Lee, Hyun-Min Hwang, Kyoung-In Shin, Jung-Hoon Park, Seo-Yeoun Ji, and Yeon-Jung Hong. 2023. "Clinical Outcomes in Dogs Undergoing Cholecystectomy via a Transverse Incision: A Meta−Analysis of 121 Animals Treated between 2011 and 2021" Veterinary Sciences 10, no. 6: 395. https://doi.org/10.3390/vetsci10060395
APA StyleChae, H.-K., Jeong, J.-Y., Lee, S.-Y., Hwang, H.-M., Shin, K.-I., Park, J.-H., Ji, S.-Y., & Hong, Y.-J. (2023). Clinical Outcomes in Dogs Undergoing Cholecystectomy via a Transverse Incision: A Meta−Analysis of 121 Animals Treated between 2011 and 2021. Veterinary Sciences, 10(6), 395. https://doi.org/10.3390/vetsci10060395






