COVID-19 Lockdown Effects on Academic Functioning, Mood, and Health Correlates: Data from Dutch Pharmacy Students, PhD Candidates and Postdocs
Abstract
1. Summary
2. Data Description
2.1. Informed Consent
2.2. Demographics
2.3. COVID-19 Test
2.4. Immune Status Questionnaire (ISQ)
2.5. Mood and Being Active
2.6. Quality of Life and Health Correlates
2.7. Smoking
2.8. Alcohol Consumption and Hangovers
2.9. Academic Functioning
2.10. Concluding Questions and Remarks
3. Methods
3.1. Participants, Sample Size and Response Rate
3.2. Data Collection
3.3. Data Handling
4. User Notes
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Cucinotta, D.; Vanelli, M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020, 91, 157–160. [Google Scholar] [CrossRef]
- Mahdy, M.A.A. The impact of COVID-19 pandemic on the academic performance of veterinary medical students. Front. Vet. Sci. 2020, 7, 594261. [Google Scholar] [CrossRef]
- Tasso, A.F.; Hisli Sahin, N.; San Roman, G.J. COVID-19 disruption on college students: Academic and socioemotional impli-cations. Psychol. Trauma 2021, 13, 9–15. [Google Scholar] [CrossRef]
- Wathelet, M.; Duhem, S.; Vaiva, G.; Baubet, T.; Habran, E.; Veerapa, E.; Debien, C.; Molenda, S.; Horn, M.; Grandgenèvre, P.; et al. Factors Associated with mental health disorders among university students in france confined during the COVID-19 pandemic. JAMA Netw. Open 2020, 3, e2025591. [Google Scholar] [CrossRef] [PubMed]
- Bolatov, A.K.; Seisembekov, T.Z.; Askarova, A.Z.; Baikanova, R.K.; Smailova, D.S.; Fabbro, E. Online-Learning due to COVID-19 improved mental health among medical students. Med. Sci. Educ. 2020, 31, 183–192. [Google Scholar] [CrossRef]
- Gallego-Gómez, J.I.; Campillo-Cano, M.; Carrión-Martínez, A.; Balanza, S.; Rodríguez-González-Moro, M.T.; Simonelli-Muñoz, A.J.; Rivera-Caravaca, J.M. The COVID-19 Pandemic and its impact on homebound nursing students. Int. J. Environ. Res. Public Health 2020, 17, 7383. [Google Scholar] [CrossRef]
- Radu, M.-C.; Schnakovszky, C.; Herghelegiu, E.; Ciubotariu, V.-A.; Cristea, I. The Impact of the COVID-19 Pandemic on the Quality of Educational Process: A Student Survey. Int. J. Environ. Res. Public Health 2020, 17, 7770. [Google Scholar] [CrossRef]
- Sundarasen, S.; Chinna, K.; Kamaludin, K.; Nurunnabi, M.; Baloch, G.M.; Khoshaim, H.B.; Hossain, S.F.A.; Sukayt, A. Psy-chological impact of COVID-19 and lockdown among university students in Malaysia: Implications and policy recommenda-tions. Int. J. Environ. Res. Public Health 2020, 17, 6206. [Google Scholar] [CrossRef] [PubMed]
- Rohmani, N.; Andriani, R. Correlation between academic self-efficacy and burnout originating from distance learning among nursing students in Indonesia during the coronavirus disease 2019 pandemic. J. Educ. Eval. Health Prof. 2021, 18, 9. [Google Scholar] [CrossRef]
- Hanafy, S.M.; Jumaa, M.I.; Arafa, M.A. A comparative study of online learning in response to the coronavirus disease 2019 pandemic versus conventional learning. Saudi Med. J. 2021, 42, 324–331. [Google Scholar] [CrossRef] [PubMed]
- Elzainy, A.; El Sadik, A.; Al Abdulmonem, W. Experience of e-learning and online assessment during the COVID-19 pandemic at the College of Medicine, Qassim University. J. Taibah Univ. Med. Sci. 2020, 15, 456–462. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, T.; de La Rubia, M.A.; Hincz, K.P.; Comas-Lopez, M.; Subirats, L.; Fort, S.; Sacha, G.M. Influence of COVID-19 confinement on students’ performance in higher education. PLoS ONE 2020, 15, e0239490. [Google Scholar] [CrossRef]
- Khalil, R.; Mansour, A.E.; Fadda, W.A.; Almisnid, K.; Aldamegh, M.; Al-Nafeesah, A.; Alkhalifah, A.; Al-Wutayd, O. The sudden transition to synchronized online learning during the COVID-19 pandemic in Saudi Arabia: A qualitative study exploring medical students’ perspectives. BMC Med. Educ. 2020, 20, 285. [Google Scholar] [CrossRef] [PubMed]
- Jaap, A.; Dewar, A.; Duncan, C.; Fairhurst, K.; Hope, D.; Kluth, D. Effect of remote online exam delivery on student experience and performance in applied knowledge tests. BMC Med. Educ. 2021, 21, 86. [Google Scholar] [CrossRef] [PubMed]
- Clarke, C.; Mullin, M.; McGrath, D.; Farrelly, N. University Students and Study Habits. Available online: https://www.cambridge.org/core/journals/irish-journal-of-psychological-medicine/article/abs/university-students-and-study-habits/DCBC1A78423A121438137802A0DB3877 (accessed on 14 October 2021).
- Foo, C.-C.; Cheung, B.; Chu, K.-M. A comparative study regarding distance learning and the conventional face-to-face approach conducted problem-based learning tutorial during the COVID-19 pandemic. BMC Med. Educ. 2021, 21, 141. [Google Scholar] [CrossRef]
- Biwer, F.; Wiradhany, W.; Oude Egbrink, M.; Hospers, H.; Wasenitz, S.; Jansen, W.; de Bruin, A. Changes and adaptations: How university students self-regulate their online learning during the COVID-19 pandemic. Front. Psychol. 2021, 12, 642593. [Google Scholar] [CrossRef]
- Meeter, M.; Bele, T.; den Hartogh, C.; Bakker, T.; de Vries, R.E.; Plak, S. College students’ motivation and study results after COVID-19 stay-at-home orders. PsyArXiv 2020. [Google Scholar] [CrossRef]
- Stubbe, J.H.; Tiemens, A.; Keizer-Hulsebosch, S.C.; Steemers, S.; van Winden, D.; Buiten, M.; Richardson, A.; van Rijn, R.M. Prevalence of Mental Health Complaints Among Performing Arts Students Is Associated With COVID-19 Preventive Measures. Front. Psychol. 2021, 12, 676587. [Google Scholar] [CrossRef]
- Van Zyl, L.E. Social Study Resources and Social Wellbeing Before and During the Intelligent COVID-19 Lockdown in The Netherlands. Soc. Indic. Res. 2021, 157, 393–415. [Google Scholar] [CrossRef]
- Prowse, R.; Sherratt, F.; Abizaid, A.; Gabrys, R.L.; Hellemans, K.G.C.; Patterson, Z.R.; McQuaid, R.J. Coping with the COVID-19 pandemic: Examining gender differences in stress and mental health among university students. Front. Psychiatry 2021, 12, 650759. [Google Scholar] [CrossRef]
- McQuaid, R.J.; Cox, S.M.; Ogunlana, A.; Jaworska, N. The burden of loneliness: Implications of the social determinants of health during COVID-19. Psychiatry Res. 2021, 296, 113648. [Google Scholar] [CrossRef]
- Pieh, C.; Budimir, S.; Probst, T. The effect of age, gender, income, work, and physical activity on mental health during coro-navirus disease (COVID-19) lockdown in Austria. J. Psychosom. Res. 2020, 136, 110186. [Google Scholar] [CrossRef]
- Barbosa, C.; Cowell, A.J.; Dowd, W.N. Alcohol consumption in response to the COVID-19 pandemic in the United States. J. Addict. Med. 2020. [Google Scholar] [CrossRef]
- Callinan, S.; Smit, K.; Mojica-Perez, Y.; D’Aquino, S.; Moore, D.; Kuntsche, E. Shifts in alcohol consumption during the COVID-19 pandemic: Early indications from Australia. Addiction 2020, 116, 1381–1388. [Google Scholar] [CrossRef]
- Grossman, E.R.; Benjamin-Neelon, S.E.; Sonnenschein, S. Alcohol Consumption during the COVID-19 Pandemic: A Cross-Sectional Survey of US Adults. Int. J. Environ. Res. Public Health 2020, 17, 9189. [Google Scholar] [CrossRef]
- Verster, J.C.; van Herwijnen, J.; Olivier, B.; Kahler, C.W. Validation of the Dutch brief young adult alcohol consequences questionnaire (B-YAACQ). Addict. Behav. 2009, 34, 411–414. [Google Scholar] [CrossRef] [PubMed]
- Hallett, J.; Howat, P.; McManus, A.; Meng, R.; Maycock, B.; Kypri, K. Academic and personal problems among Australian university students who drink at hazardous levels: Web-based survey. Health Promot. J. Aust. 2013, 24, 170–177. [Google Scholar] [CrossRef]
- Van Schrojenstein Lantman, M.; van de Loo, A.; Mackus, M.; Verster, J.C. Development of a definition for the alcohol hangover: Consumer descriptions and expert consensus. Curr. Drug Abus. Rev. 2016, 9, 148–154. [Google Scholar] [CrossRef]
- Verster, J.C.; Scholey, A.; van de Loo, A.J.A.E.; Benson, S.; Stock, A.-K. Updating the definition of the alcohol hangover. J. Clin. Med. 2020, 9, 823. [Google Scholar] [CrossRef] [PubMed]
- Howland, J.; Rohsenow, D.J.; Greece, J.A.; Littlefield, C.A.; Almeida, A.; Heeren, T.; Winter, M.; Bliss, C.A.; Hunt, S.; Hermos, J. The effects of binge drinking on college students’ next-day academic test-taking performance and mood state. Addiction 2010, 105, 655–665. [Google Scholar] [CrossRef] [PubMed]
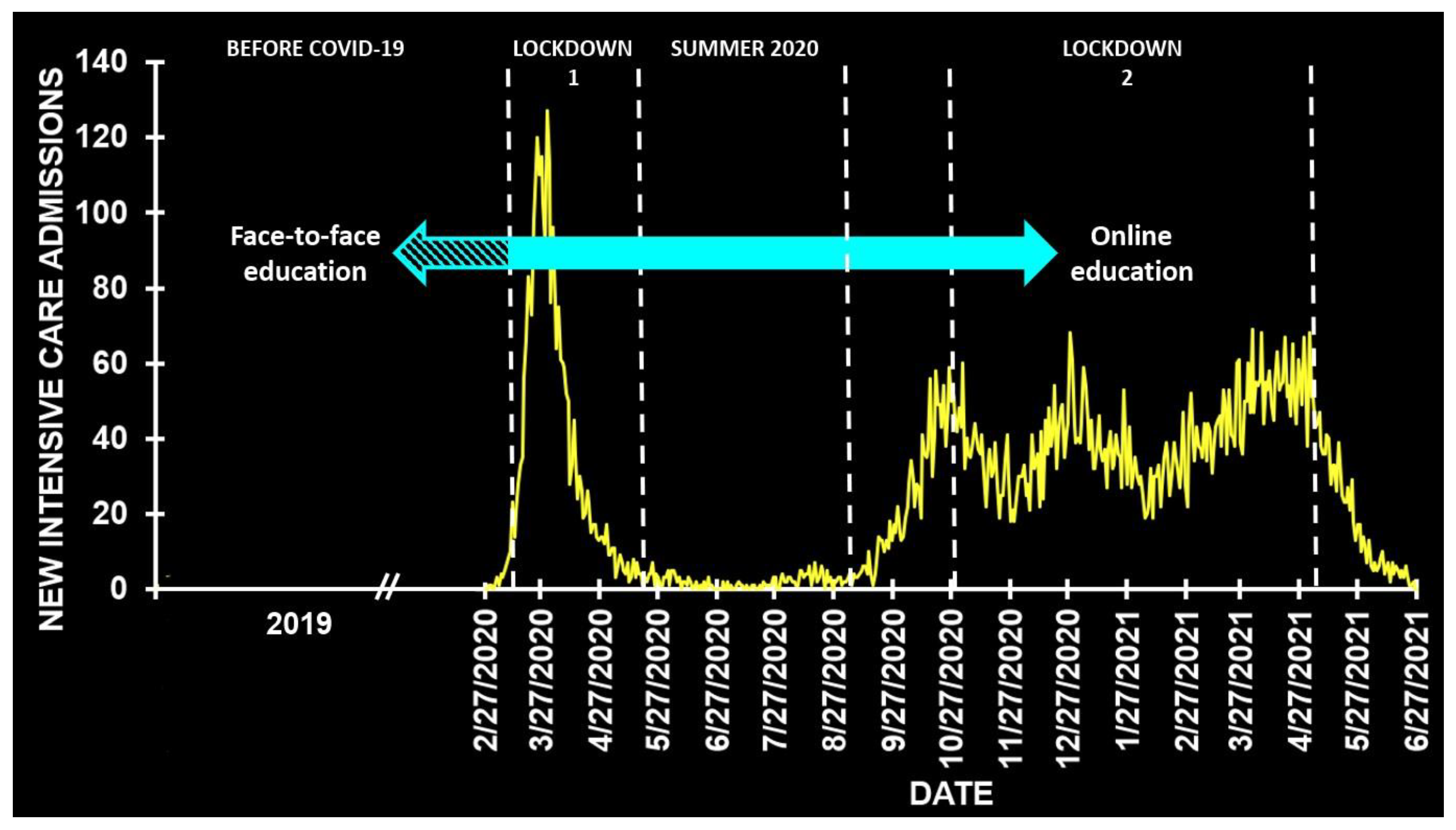
- RIVM. Covid-19 Intensive Care-opnames (IC) in Nederland per ic-Opnamedatum en Meldingsdatum (Volgens NICE Registratie). Available online: https://data.rivm.nl/geonetwork/srv/dut/catalog.search#/metadata/45f911c4-3a62-42f1-b594-524a75db2c94 (accessed on 14 October 2021).
- Verster, J.; Sandalova, E.; Garssen, J.; Bruce, G. The Use of Single-Item Ratings Versus Traditional Multiple-Item Questionnaires to Assess Mood and Health. Eur. J. Investig. Health Psychol. Educ. 2021, 11, 183–198. [Google Scholar] [CrossRef] [PubMed]
- Statistics Netherlands (Centraal Bureau voor de Statistiek, CBS). Wat Is Het Verschil Tussen EenWesterse en Niet-Westerse Allochtoon? Available online: https://www.cbs.nl/nl-nl/faq/specifiek/wat-is-het-verschil-tussen-een-westerse-en-niet-westerse-allochtoon (accessed on 26 June 2021).
- Wilod Versprille, L.J.F.; van de Loo, A.J.A.E.; Mackus, M.; Arnoldy, L.; Sulzer, T.A.L.; Vermeulen, S.A.; Abdulahad, S.; Huls, H.; Baars, T.; Scholey, A.; et al. Development and Validation of the Immune Status Questionnaire (ISQ). Int. J. Environ. Res. Public Health 2019, 16, 4743. [Google Scholar] [CrossRef]
- Kiani, P.; Merlo, A.; Saeed, H.M.; Benson, S.; Bruce, G.; Hoorn, R.; Kraneveld, A.D.; Severeijns, N.R.; Sips, A.S.M.; Scholey, A.; et al. Immune Fitness and the Psychosocial and Health Consequences of the COVID-19 Pandemic Lockdown in The Netherlands: Methodology and Design of the CLOFIT Study. Eur. J. Investig. Health Psychol. Educ. 2021, 11, 199–218. [Google Scholar] [CrossRef]
- Verster, J.C.; Arnoldy, L.; van de Loo, A.J.A.E.; Benson, S.; Scholey, A.; Stock, A.-K. The impact of mood and subjective in-toxication on hangover severity. J. Clin. Med. 2020, 9, 2462. [Google Scholar] [CrossRef] [PubMed]
- Baars, T.; Berge, C.; Garssen, J.; Verster, J.C. Effect of raw milk consumption on perceived health, mood and immune func-tioning among US adults with a poor and normal health: A retrospective questionnaire based study. Complement. Ther. Med. 2019, 47, 102196. [Google Scholar]
- Verster, J.C.; Anogeianaki, A.; Kruisselbrink, D.; Alford, C.; Stock, A.-K. Relationship between alcohol hangover and physical endurance performance: Walking the samaria gorge. J. Clin. Med. 2019, 9, 114. [Google Scholar] [CrossRef] [PubMed]
- Verster, J.; Arnoldy, L.; van de Loo, A.; Kraneveld, A.; Garssen, J.; Scholey, A. The Impact of Having a Holiday or Work in Fiji on Perceived Immune Fitness. Tour. Hosp. 2021, 2, 95–112. [Google Scholar] [CrossRef]
- Van Schrojenstein Lantman, M.; Mackus, M.; Otten, L.; de Kruijff, D.; van de Loo, A.J.; Kraneveld, A.; Garssen, J.; Verster, J.C. Mental resilience, perceived immune functioning, and health. J. Multidiscip. Health 2017, 10, 107–112. [Google Scholar] [CrossRef]
- Verster, J.C.; Tromp, M.D.; Donners, A.A.; Garssen, J. Sleep, eating disorder symptoms, and daytime functioning. Nat. Sci. Sleep 2016, 8, 35–40. [Google Scholar] [CrossRef]
- Abdulahad, S.; Huls, H.; Balikji, S.; van de Loo, A.J.A.E.; Roth, T.; Verster, J.C. Irritable bowel syndrome, immune fitness, and insomnia: Results from an online survey among people reporting sleep complaints. Sleep Vigil. 2019, 3, 121–129. [Google Scholar] [CrossRef]
- Verster, J.C.; van de Loo, A.J.; Benson, S.; Scholey, A.; Stock, A.-K. The Assessment of overall hangover severity. J. Clin. Med. 2020, 9, 786. [Google Scholar] [CrossRef] [PubMed]
- Couper, M.P.; Miller, P.V. Web Survey Methods: Introduction. Public Opin. Q. 2008, 72, 831–835. [Google Scholar] [CrossRef]
- Shaz, B.H.; Demmons, D.G.; Crittenden, C.P.; Carnevale, C.V.; Lee, M.; Burnett, M.; Easley, K.; Hillyer, C.D. Motivators and barriers to blood donation in African American college students. Transfus. Apher. Sci. 2009, 41, 191–197. [Google Scholar] [CrossRef][Green Version]
- Head, A.J.; Eisenberg, M.B. How today’s college students use Wikipedia for course-related research. First Monday 2010, 15. [Google Scholar] [CrossRef]
- Gutter, M.S.; Copur, Z. Financial behaviors and financial well-being of college students: Evidence from a national survey. J. Fam. Econ. Issues 2011, 32, 699–714. [Google Scholar] [CrossRef]
- Warrener, C.D.; Tasso, A. An empirical examination of the relationship between dating abuse and entitlement within a college population. Partn. Abus. 2017, 8, 377–394. [Google Scholar] [CrossRef]
| Question | Variable | Number of Items | Completers |
|---|---|---|---|
| 1 | Education level | 1 | 341 |
| 2 | Age | 1 | 341 |
| 3 | Sex | 1 | 341 |
| 4 | Ethnicity | 1 | 339 |
| 5 | Living situation | 1 | 341 |
| 6 | Tested for COVID-19 | 1 | 331 |
| 7 | ISQ | 9 | 331 |
| 8 | Mood and being active | 8 | 261 |
| 9 | QoL, health correlates | 3 | 254 |
| 10 | Smoking | 2 | 254 (17) |
| 11 | Alcohol consumption | 4 | 254 (162) |
| 12 | Academic functioning | 10 | 250 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hendriksen, P.A.; Merlo, A.; Bijlsma, E.Y.; Engels, F.; Garssen, J.; Bruce, G.; Verster, J.C. COVID-19 Lockdown Effects on Academic Functioning, Mood, and Health Correlates: Data from Dutch Pharmacy Students, PhD Candidates and Postdocs. Data 2021, 6, 120. https://doi.org/10.3390/data6110120
Hendriksen PA, Merlo A, Bijlsma EY, Engels F, Garssen J, Bruce G, Verster JC. COVID-19 Lockdown Effects on Academic Functioning, Mood, and Health Correlates: Data from Dutch Pharmacy Students, PhD Candidates and Postdocs. Data. 2021; 6(11):120. https://doi.org/10.3390/data6110120
Chicago/Turabian StyleHendriksen, Pauline A., Agnese Merlo, Elisabeth Y. Bijlsma, Ferdi Engels, Johan Garssen, Gillian Bruce, and Joris C. Verster. 2021. "COVID-19 Lockdown Effects on Academic Functioning, Mood, and Health Correlates: Data from Dutch Pharmacy Students, PhD Candidates and Postdocs" Data 6, no. 11: 120. https://doi.org/10.3390/data6110120
APA StyleHendriksen, P. A., Merlo, A., Bijlsma, E. Y., Engels, F., Garssen, J., Bruce, G., & Verster, J. C. (2021). COVID-19 Lockdown Effects on Academic Functioning, Mood, and Health Correlates: Data from Dutch Pharmacy Students, PhD Candidates and Postdocs. Data, 6(11), 120. https://doi.org/10.3390/data6110120







