Identification of Secondary Biomechanical Abnormalities in the Lower Limb Joints after Chronic Transtibial Amputation: A Proof-of-Concept Study Using SPM1D Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Reference and Subjects
2.1.1. Ethics Approval
2.1.2. Patient and Public Involvement
2.2. The Study Processes
2.2.1. Control Group Biomechanics (Collectively)
2.2.2. Patients’ Biomechanics (Individually)
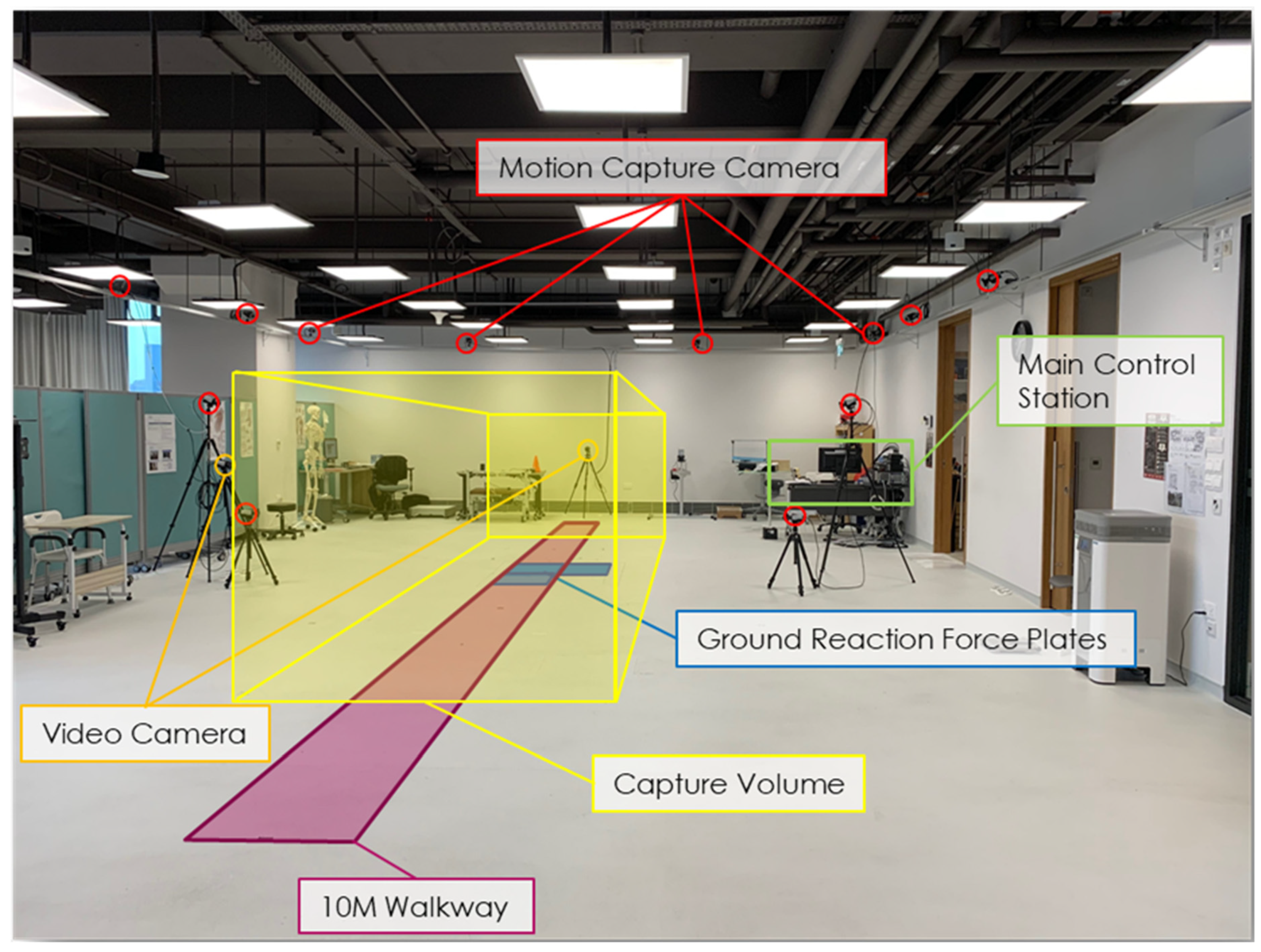
2.3. Data Acquisition
2.4. Data Processing
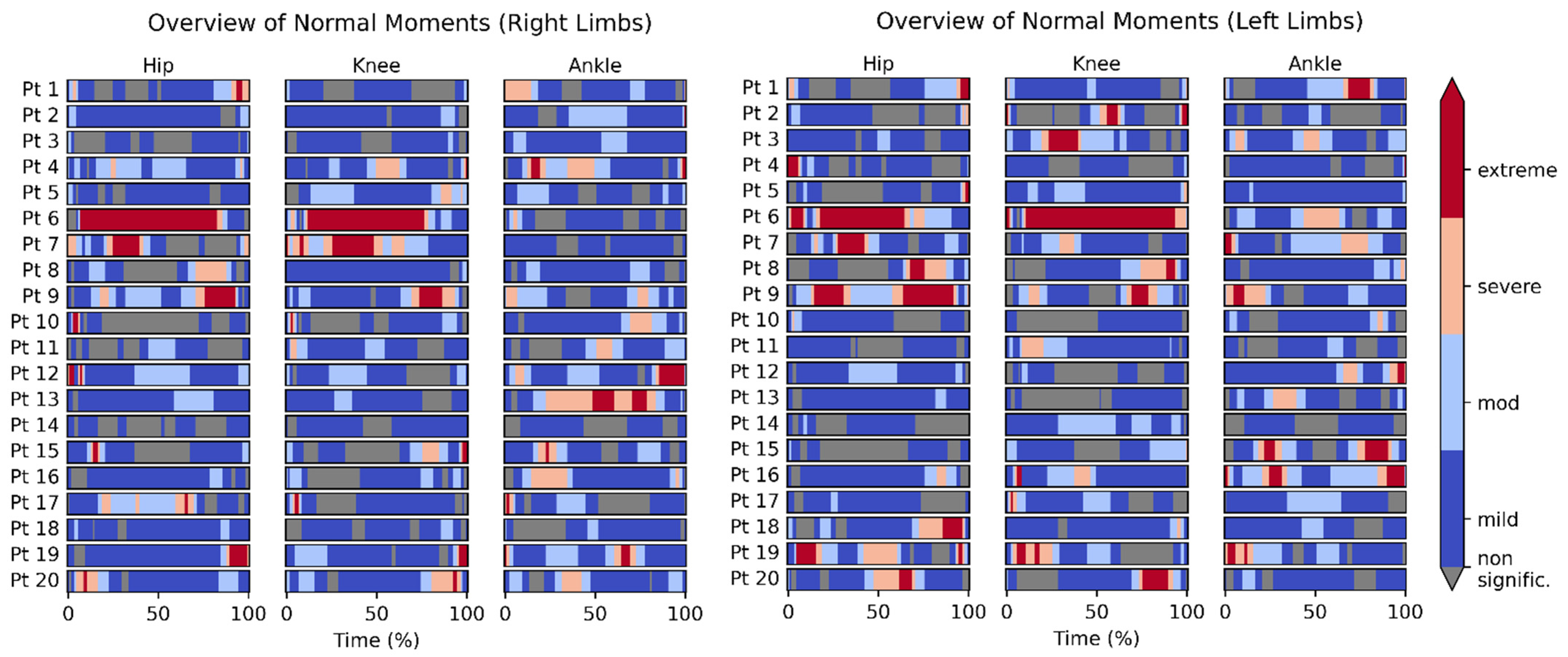
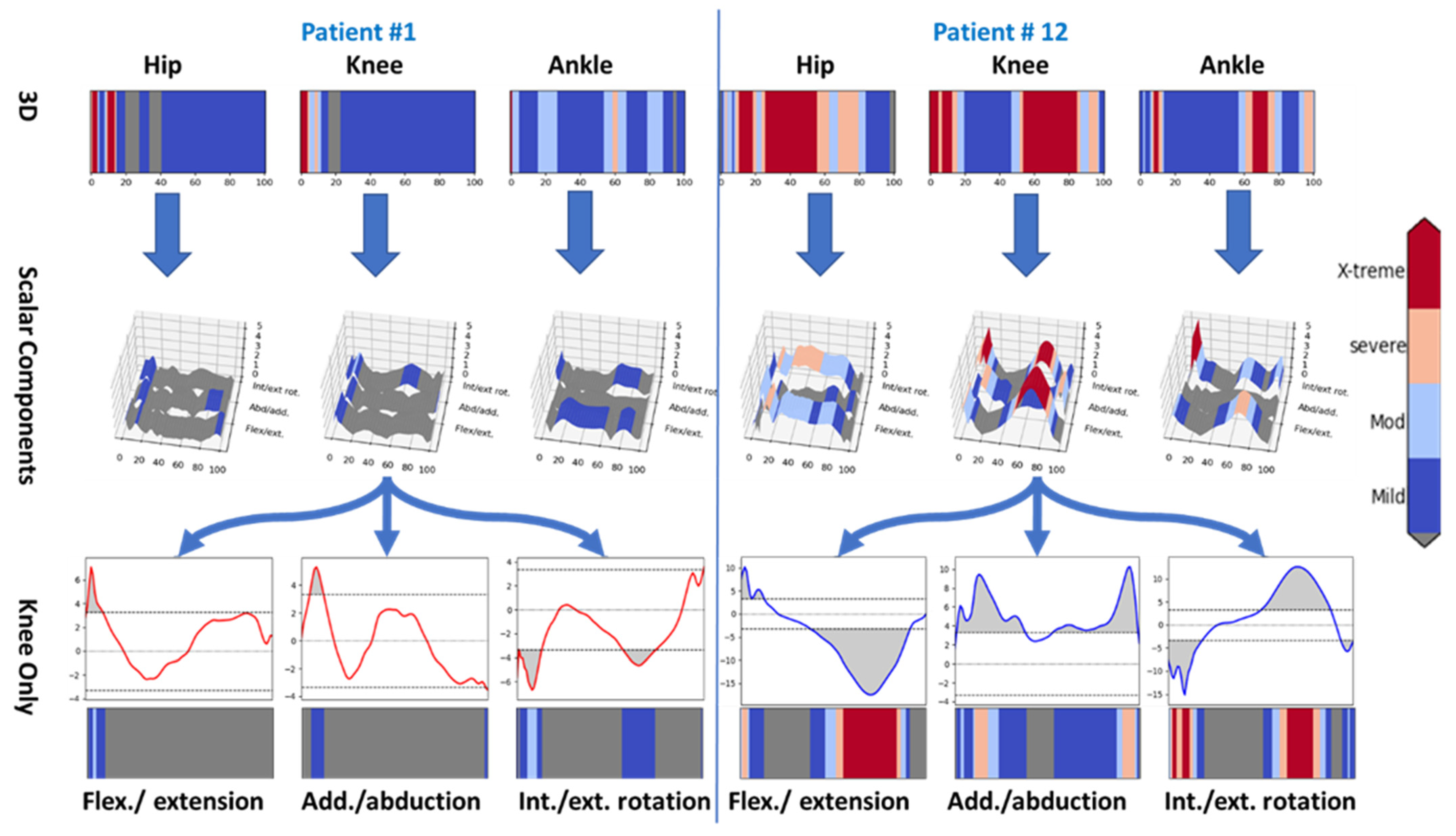
3. Results
4. Discussion
5. Study Limitations
6. Future Work
7. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gaßner, H.; Jensen, D.; Marxreiter, F.; Kletsch, A.; Bohlen, S.; Schubert, R.; Muratori, L.M.; Eskofier, B.; Klucken, J.; Winkler, J.; et al. Gait variability as digital biomarker of disease severity in Huntington’s disease. J. Neurol. 2020, 267, 1594–1601. [Google Scholar] [CrossRef] [Green Version]
- Hanley, B.; Tucker, C.B. Gait variability and symmetry remain consistent during high-intensity 10,000 m treadmill running. J. Biomech. 2018, 79, 129–134. [Google Scholar] [CrossRef] [Green Version]
- Gao, Z.; Mei, Q.; Xiang, L.; Baker, J.S.; Fernandez, J.; Gu, Y. Effects of limb dominance on the symmetrical distribution of plantar loading during walking and running. Proc. Inst. Mech. Eng. Part P J. Sports Eng. Technol. 2022, 236, 17–23. [Google Scholar] [CrossRef]
- Zhang, B.; Lu, Q. A Current Review of Foot Disorder and Plantar Pressure Alternation in the Elderly. Phys. Act. Health 2020, 4, 95–106. [Google Scholar] [CrossRef]
- Pataky, T.C. One-dimensional statistical parametric mapping in Python. Comput. Methods Biomech. Biomed. Eng. 2012, 15, 295–301. [Google Scholar] [CrossRef]
- Pataky, T.C. Generalized n-dimensional biomechanical field analysis using statistical parametric mapping. J. Biomech. 2010, 43, 1976–1982. [Google Scholar] [CrossRef]
- Pataky, T.C.; Robinson, M.A.; Vanrenterghem, J. Vector field statistical analysis of kinematic and force trajectories. J. Biomech. 2013, 46, 2394–2401. [Google Scholar] [CrossRef] [Green Version]
- Robinson, M.A.; Vanrenterghem, J.; Pataky, T.C. Statistical Parametric Mapping (SPM) for alpha-based statistical analyses of multi-muscle EMG time-series. J. Electromyogr. Kinesiol. 2015, 25, 14–19. [Google Scholar] [CrossRef]
- Mavroforou, A.; Koutsias, S.; Fafoulakis, F.; Balogiannis, I.; Stamatiou, G.; Giannoukas, A.D. The evolution of lower limb amputation through the ages. Historical note. Int. Angiol. 2007, 26, 385–389. [Google Scholar]
- Nerlich, A.G.; Zink, A.; Szeimies, U.; Hagedorn, H.G. Ancient Egyptian prosthesis of the big toe. Lancet 2000, 356, 2176–2179. [Google Scholar] [CrossRef]
- Varma, P.; Stineman, M.G.; Dillingham, T.R. Epidemiology of limb loss. Phys. Med. Rehabil. Clin. N. Am. 2014, 25, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Riandini, T.; Pang, D.; Toh, M.; Tan, C.S.; Choong, A.; Lo, Z.J.; Chandrasekar, S.; Tai, E.S.; Tan, K.B.; Venkataraman, K. National Rates of Lower Extremity Amputation in People with and without Diabetes in a Multi-Ethnic Asian Population: A Ten Year Study in Singapore. Eur. J. Vasc. Endovasc. Surg. 2022, 63, 147–155. [Google Scholar] [CrossRef] [PubMed]
- Yong, G.K. Speech by Minister for Health, Mr Gan Kim Yong, at the Moh Committee of Supply Debate. 13 April 2016. Available online: https://www.moh.gov.sg/news-highlights/details/speech-by-minister-for-health-mr-gan-kim-yong-at-the-moh-committee-of-supply-debate-2016 (accessed on 28 October 2021).
- Amma, R.; Hisano, G.; Murata, H.; Major, M.J.; Takemura, H.; Hobara, H. Inter-limb weight transfer strategy during walking after unilateral transfemoral amputation. Sci. Rep. 2021, 11, 4793. [Google Scholar] [CrossRef] [PubMed]
- Norvell, D.C.; Czerniecki, J.M.; Reiber, G.E.; Maynard, C.; Pecoraro, J.A.; Weiss, N.S. The prevalence of knee pain and symptomatic knee osteoarthritis among veteran traumatic amputees and nonamputees. Arch. Phys. Med. Rehabil. 2005, 86, 487–493. [Google Scholar] [CrossRef]
- Agrawal, V.; Gailey, R.; Gaunaurd, I.; Gailey, R., 3rd; O’Toole, C. Weight distribution symmetry during the sit-to-stand movement of unilateral transtibial amputees. Ergonomics 2011, 54, 656–664. [Google Scholar] [CrossRef]
- Ozyurek, S.; Demirbuken, I.; Angin, S. Altered movement strategies in sit-to-stand task in persons with transtibial amputation. Prosthet. Orthot. Int. 2014, 38, 303–309. [Google Scholar] [CrossRef]
- Kolasinski, S.L.; Neogi, T.; Hochberg, M.C.; Oatis, C.; Guyatt, G.; Block, J.; Callahan, L.; Copenhaver, C.; Dodge, C.; Felson, D.; et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the Hand, Hip, and Knee. Arthr. Care Res. 2020, 72, 149–162. [Google Scholar] [CrossRef]
- Taylor, B.C.; Poka, A. Osteomyoplastic Transtibial Amputation: The Ertl Technique. J. Am. Acad. Orthop. Surg. 2016, 24, 259–265. [Google Scholar] [CrossRef]
- Ferris, A.E.; Christiansen, C.L.; Heise, G.D.; Hahn, D.; Smith, J.D. Ertl and Non-Ertl amputees exhibit functional biomechanical differences during the sit-to-stand task. Clin. Biomech. 2017, 44, 1–6. [Google Scholar] [CrossRef]
- Melzer, I.; Yekutiel, M.; Sukenik, S. Comparative study of osteoarthritis of the contralateral knee joint of male amputees who do and do not play volleyball. J. Rheumatol. 2001, 28, 169–172. [Google Scholar]
- Ferris, A.E. Biomechanical Assessment of Ertl and Burgess Transtibial Amputation Techniques; University of Northern Colorado: Greeley, CO, USA, 2016. [Google Scholar]
- Pröbsting, E.; Kannenberg, A.; Blumentritt, S. Back pain and osteoarthritis as secondary disabilities of lower limb amputation. Can. Prosthet. Orthot. J. 2018, 1. [Google Scholar] [CrossRef]
- Ebrahimzadeh, M.H.; Hariri, S. Long-term outcomes of unilateral transtibial amputations. Mil. Med. 2009, 174, 593–597. [Google Scholar] [CrossRef] [Green Version]
- Liang, P.; Kwong, W.H.; Sidarta, A.; Yap, C.K.; Tan, W.K.; Lim, L.S.; Chan, P.Y.; Kuah, C.W.K.; Wee, S.K.; Chua, K.; et al. An Asian-centric human movement database capturing activities of daily living. Sci. Data 2020, 7, 290. [Google Scholar] [CrossRef]
- Orendurff, M.S.; Raschke, S.U.; Winder, L.; Moe, D.; Boone, D.A.; Kobayashi, T. Functional level assessment of individuals with transtibial limb loss: Evaluation in the clinical setting versus objective community ambulatory activity. J. Rehabil. Assist. Technol. Eng. 2016, 3, 2055668316636316. [Google Scholar] [CrossRef]
- Alhossary, A.A.; Pataky, T.; Ang, W.T.; Chua, K.S.G.; Donnelly, C.J. MovementRx: Versatile clinical movement analysis using Statistical Parametric Mapping. Res. Sq. 2021. preprint. [Google Scholar] [CrossRef]
- Cappozzo, A.; Catani, F.; Croce, U.D.; Leardini, A. Position and orientation in space of bones during movement: Anatomical frame definition and determination. Clin. Biomech. 1995, 10, 171–178. [Google Scholar] [CrossRef]
- Cappozzo, A.; Catani, F.; Leardini, A.; Benedetti, M.G.; Croce, U.D. Position and orientation in space of bones during movement: Experimental artefacts. Clin. Biomech. 1996, 11, 90–100. [Google Scholar] [CrossRef]
- Bell, A.L.; Brand, R.A.; Pedersen, D.R. Prediction of hip joint centre location from external landmarks. Hum. Mov. Sci. 1989, 8, 3–16. [Google Scholar] [CrossRef]
- Bell, A.L.; Pedersen, D.R.; Brand, R.A. A comparison of the accuracy of several hip center location prediction methods. J. Biomech. 1990, 23, 617–621. [Google Scholar] [CrossRef]
- Wu, G.; Siegler, S.; Allard, P.; Kirtley, C.; Leardini, A.; Rosenbaum, D.; Whittle, M.; D’Lima, D.D.; Cristofolini, L.; Witte, H.; et al. ISB recommendation on definitions of joint coordinate system of various joints for the reporting of human joint motion—Part I: Ankle, hip, and spine. J. Biomech. 2002, 35, 543–548. [Google Scholar] [CrossRef]
- Teichtahl, A.J.; Wluka, A.E.; Morris, M.E.; Davis, S.R.; Cicuttini, F.M. The associations between the dominant and nondominant peak external knee adductor moments during gait in healthy subjects: Evidence for symmetry. Arch. Phys. Med. Rehabil. 2009, 90, 320–324. [Google Scholar] [CrossRef]
- Allet, L.; IJzerman, H.; Meijer, K.; Willems, P.; Savelberg, H. The influence of stride-length on plantar foot-pressures and joint moments. Gait Posture 2011, 34, 300–306. [Google Scholar] [CrossRef] [Green Version]
- Monaco, V.; Rinaldi, L.A.; Macri, G.; Micera, S. During walking elders increase efforts at proximal joints and keep low kinetics at the ankle. Clin. Biomech. 2009, 24, 493–498. [Google Scholar] [CrossRef]
- Farrokhi, S.; Mazzone, B.; Yoder, A.; Grant, K.; Wyatt, M. A Narrative Review of the Prevalence and Risk Factors Associated With Development of Knee Osteoarthritis After Traumatic Unilateral Lower Limb Amputation. Mil. Med. 2016, 181, 38–44. [Google Scholar] [CrossRef] [Green Version]
- Lemaire, E.D.; Fisher, F.R. Osteoarthritis and elderly amputee gait. Arch. Phys. Med. Rehabil. 1994, 75, 1094–1099. [Google Scholar] [CrossRef]
- Orekhov, G.; Robinson, A.M.; Hazelwood, S.J.; Klisch, S.M. Knee joint biomechanics in transtibial amputees in gait, cycling, and elliptical training. PLoS ONE 2019, 14, e0226060. [Google Scholar] [CrossRef] [Green Version]



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alhossary, A.; Ang, W.T.; Chua, K.S.G.; Tay, M.R.J.; Ong, P.L.; Murakami, T.; Quake, T.; Binedell, T.; Wee, S.K.; Phua, M.W.; et al. Identification of Secondary Biomechanical Abnormalities in the Lower Limb Joints after Chronic Transtibial Amputation: A Proof-of-Concept Study Using SPM1D Analysis. Bioengineering 2022, 9, 293. https://doi.org/10.3390/bioengineering9070293
Alhossary A, Ang WT, Chua KSG, Tay MRJ, Ong PL, Murakami T, Quake T, Binedell T, Wee SK, Phua MW, et al. Identification of Secondary Biomechanical Abnormalities in the Lower Limb Joints after Chronic Transtibial Amputation: A Proof-of-Concept Study Using SPM1D Analysis. Bioengineering. 2022; 9(7):293. https://doi.org/10.3390/bioengineering9070293
Chicago/Turabian StyleAlhossary, Amr, Wei Tech Ang, Karen Sui Geok Chua, Matthew Rong Jie Tay, Poo Lee Ong, Tsurayuki Murakami, Tabitha Quake, Trevor Binedell, Seng Kwee Wee, Min Wee Phua, and et al. 2022. "Identification of Secondary Biomechanical Abnormalities in the Lower Limb Joints after Chronic Transtibial Amputation: A Proof-of-Concept Study Using SPM1D Analysis" Bioengineering 9, no. 7: 293. https://doi.org/10.3390/bioengineering9070293
APA StyleAlhossary, A., Ang, W. T., Chua, K. S. G., Tay, M. R. J., Ong, P. L., Murakami, T., Quake, T., Binedell, T., Wee, S. K., Phua, M. W., Wei, Y. J., & Donnelly, C. J. (2022). Identification of Secondary Biomechanical Abnormalities in the Lower Limb Joints after Chronic Transtibial Amputation: A Proof-of-Concept Study Using SPM1D Analysis. Bioengineering, 9(7), 293. https://doi.org/10.3390/bioengineering9070293








