Influence of Landing in Neuromuscular Control and Ground Reaction Force with Ankle Instability: A Narrative Review
Abstract
:1. Introduction
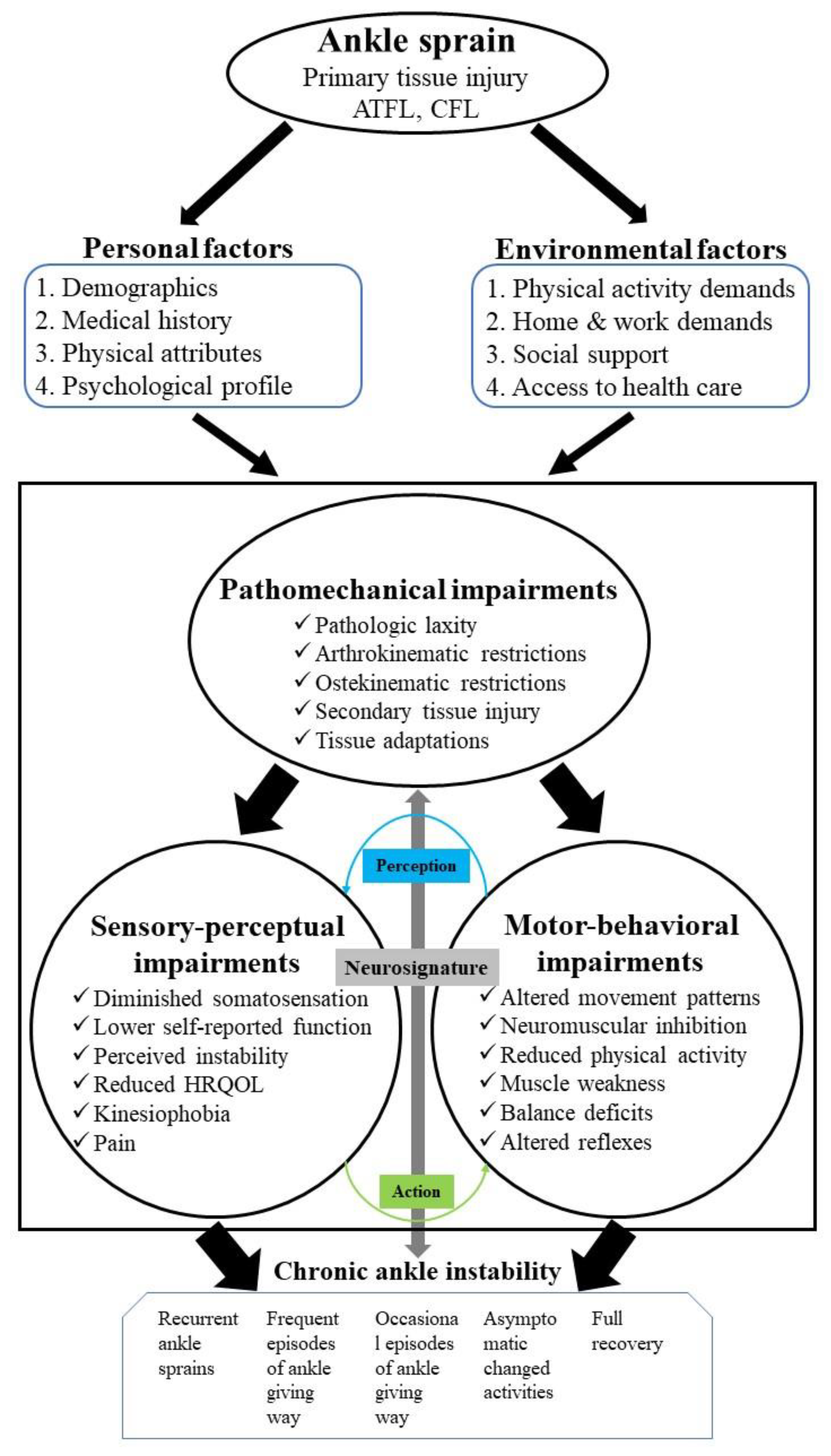
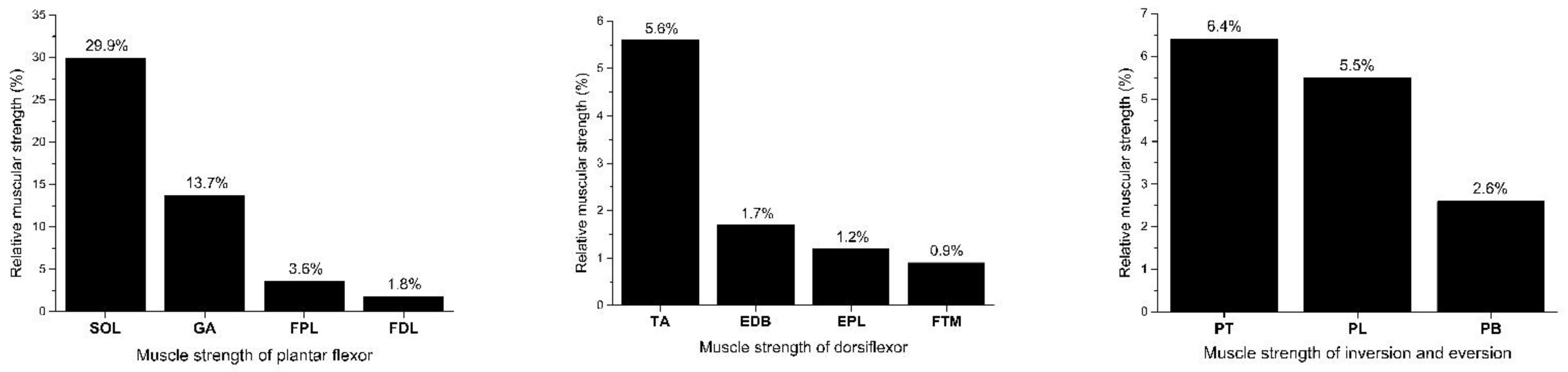
2. The Importance of Neuromuscular Control for Ankle Sprains
3. The Influence of Landing Force on Ankle Instability
4. How CAI Patients Show Postural Control Deficits during Landing Tasks
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hertel, J.; Corbett, R.O. An updated model of chronic ankle instability. J. Athl. Train. 2019, 54, 572–588. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roos, K.G.; Kerr, Z.Y.; Mauntel, T.C.; Djoko, A.; Dompier, T.P.; Wikstrom, E.A. The epidemiology of lateral ligament complex ankle sprains in National Collegiate Athletic Association sports. Am. J. Sports Med. 2017, 45, 201–209. [Google Scholar] [CrossRef]
- Swenson, D.M.; Collins, C.L.; Fields, S.K.; Comstock, R.D. Epidemiology of US high school sports-related ligamentous ankle injuries, 2005/06–2010/11. Clin. J. Sport Med. Off. J. Can. Acad. Sport Med. 2013, 23, 190. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Waterman, B.R.; Owens, B.D.; Davey, S.; Zacchilli, M.A.; Belmont, P.J., Jr. The epidemiology of ankle sprains in the United States. JBJS 2010, 92, 2279–2284. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garrick, J.G.; Requa, R.K. The epidemiology of foot and ankle injuries in sports. Clin. Sports Med. 1988, 7, 29–36. [Google Scholar] [CrossRef]
- Tropp, H.; Odenrick, P.; Gillquist, J. Stabilometry recordings in functional and mechanical instability of the ankle joint. Int. J. Sports Med. 1985, 6, 180–182. [Google Scholar] [CrossRef]
- Yeung, M.S.; Chan, K.M.; So, C.H.; Yuan, W.Y. An epidemiological survey on ankle sprain. Br. J. Sports Med. 1994, 28, 112–116. [Google Scholar] [CrossRef] [Green Version]
- Doherty, C.; Bleakley, C.; Hertel, J.; Caulfield, B.; Ryan, J.; Delahunt, E. Recovery from a first-time lateral ankle sprain and the predictors of chronic ankle instability: A prospective cohort analysis. Am. J. Sports Med. 2016, 44, 995–1003. [Google Scholar] [CrossRef]
- Gribble, P.A.; Bleakley, C.M.; Caulfield, B.M.; Docherty, C.L.; Fourchet, F.; Fong, D.T.-P.; Hertel, J.; Hiller, C.E.; Kaminski, T.W.; McKeon, P.O. Evidence review for the 2016 International Ankle Consortium consensus statement on the prevalence, impact and long-term consequences of lateral ankle sprains. Br. J. Sports Med. 2016, 50, 1496–1505. [Google Scholar] [CrossRef] [Green Version]
- Gribble, P.A.; Delahunt, E.; Bleakley, C.; Caulfield, B.; Docherty, C.; Fourchet, F.; Fong, D.; Hertel, J.; Hiller, C.; Kaminski, T. Selection criteria for patients with chronic ankle instability in controlled research: A position statement of the International Ankle Consortium. J. Orthop. Sports Phys. Ther. 2013, 43, 585–591. [Google Scholar] [CrossRef] [Green Version]
- Boyle, J.; Negus, V. Joint position sense in the recurrently sprained ankle. Aust. J. Physiother. 1998, 44, 159–163. [Google Scholar] [CrossRef] [Green Version]
- Hertel, J.; Gay, M.R.; Denegar, C.R. Differences in Postural Control During Single-Leg Stance Among Healthy Individuals With Different Foot Types. J. Athl. Train. 2002, 37, 129–132. [Google Scholar]
- Terada, M.; Pietrosimone, B.G.; Gribble, P.A. Therapeutic interventions for increasing ankle dorsiflexion after ankle sprain: A systematic review. J. Athl. Train. 2013, 48, 696–709. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Theisen, A.; Day, J. Chronic ankle instability leads to lower extremity kinematic changes during landing tasks: A systematic review. Int. J. Exerc. Sci. 2019, 12, 24. [Google Scholar] [PubMed]
- Kim, H.; Palmieri-Smith, R.; Kipp, K. Muscle force contributions to ankle joint contact forces during an unanticipated cutting task in people with chronic ankle instability. J. Biomech. 2021, 124, 110566. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Wang, H.; Simpson, K.J. Chronic Ankle Instability Does Not Influence Tibiofemoral Contact Forces During Drop Landings Using a Musculoskeletal Model. J. Appl. Biomech. 2019, 35, 426–430. [Google Scholar] [CrossRef]
- Stotz, A.; John, C.; Gmachowski, J.; Rahlf, A.L.; Hamacher, D.; Hollander, K.; Zech, A. Effects of elastic ankle support on running ankle kinematics in individuals with chronic ankle instability and healthy controls. Gait Posture 2021, 87, 149–155. [Google Scholar] [CrossRef]
- Olsen, O.-E.; Myklebust, G.; Engebretsen, L.; Bahr, R. Injury mechanisms for anterior cruciate ligament injuries in team handball: A systematic video analysis. Am. J. Sports Med. 2004, 32, 1002–1012. [Google Scholar] [CrossRef]
- Li, Y.; Wang, H.; Simpson, K.J. Chronic Ankle Instability Does Not Influence Tibiofemoral Contact Forces during Drop Landings. Proceedings 2020, 49, 5. [Google Scholar] [CrossRef]
- Söderman, K.; Alfredson, H.; Pietilä, T.; Werner, S. Risk factors for leg injuries in female soccer players: A prospective investigation during one out-door season. Knee Surg. Sports Traumatol. Arthrosc. 2001, 9, 313–321. [Google Scholar] [CrossRef]
- Kramer, L.; Denegar, C.; Buckley, W.E.; Hertel, J. Factors associated with anterior cruciate ligament injury: History in female athletes. J. Sports Med. Phys. Fit. 2007, 47, 446. [Google Scholar]
- Hewett, T.E.; Zazulak, B.T.; Myer, G.D.; Ford, K.R. A review of electromyographic activation levels, timing differences, and increased anterior cruciate ligament injury incidence in female athletes. Br. J. Sports Med. 2005, 39, 347–350. [Google Scholar] [CrossRef] [Green Version]
- Simpson, J.D.; DeBusk, H.; Hill, C.; Knight, A.; Chander, H. The role of military footwear and workload on ground reaction forces during a simulated lateral ankle sprain mechanism. Foot 2018, 34, 53–57. [Google Scholar] [CrossRef]
- Doherty, C.; Delahunt, E.; Caulfield, B.; Hertel, J.; Ryan, J.; Bleakley, C. The incidence and prevalence of ankle sprain injury: A systematic review and meta-analysis of prospective epidemiological studies. Sports Med. 2014, 44, 123–140. [Google Scholar] [CrossRef] [PubMed]
- Jeon, H.G.; Lee, S.Y.; Park, S.E.; Ha, S. Ankle Instability Patients Exhibit Altered Muscle Activation of Lower Extremity and Ground Reaction Force during Landing: A Systematic Review and Meta-Analysis. J. Sports Sci. Med. 2021, 20, 373–390. [Google Scholar] [CrossRef] [PubMed]
- Devita, P.; Skelly, W.A. Effect of landing stiffness on joint kinetics and energetics in the lower extremity. Med. Sci. Sports Exerc. 1992, 24, 108–115. [Google Scholar] [CrossRef] [Green Version]
- Pozzi, F.; Moffat, M.; Gutierrez, G. Neuromuscular control during performance of a dynamic balance task in subjects with and without ankle instability. Int. J. Sports Phys. Ther. 2015, 10, 520. [Google Scholar]
- Denyer, J.R.; Hewitt, N.L.; Mitchell, A.C. Foot structure and muscle reaction time to a simulated ankle sprain. J. Athl. Train. 2013, 48, 326–330. [Google Scholar] [CrossRef] [Green Version]
- Mitchell, A.; Dyson, R.; Hale, T.; Abraham, C. Biomechanics of ankle instability. Part 1: Reaction time to simulated ankle sprain. Med. Sci. Sports Exerc. 2008, 40, 1515–1521. [Google Scholar] [CrossRef]
- Kipp, K.; Palmieri-Smith, R.M. Differences in kinematic control of ankle joint motions in people with chronic ankle instability. Clin. Biomech. 2013, 28, 562–567. [Google Scholar] [CrossRef]
- Nordin, M.; Frankel, V.H. Basic Biomechanics of the Musculoskeletal System; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2001. [Google Scholar]
- Fick, R. Handbuch der Anatomie und Mechanik der Gelenke: T. Spezielle Gelenk-und Muskelmechanik; G. Fischer: Singapore, 1911; Volume 3. [Google Scholar]
- Silver, R.; De La Garza, J.; Rang, M. The myth of muscle balance. A study of relative strengths and excursions of normal muscles about the foot and ankle. J. Bone Jt. Surg. Br. Vol. 1985, 67, 432–437. [Google Scholar] [CrossRef] [PubMed]
- Watkins, J. Structure and Function of the Musculoskeletal System; Human Kinetics: Champaign, IL, USA, 2009. [Google Scholar]
- Brown, C.; Ross, S.; Mynark, R.; Guskiewicz, K. Assessing functional ankle instability with joint position sense, time to stabilization, and electromyography. J. Sport Rehabil. 2004, 13, 122–134. [Google Scholar] [CrossRef]
- Caulfield, B.; Garrett, M. Functional instability of the ankle: Differences in patterns of ankle and knee movement prior to and post landing in a single leg jump. Int. J. Sports Med. 2002, 23, 64–68. [Google Scholar] [CrossRef] [PubMed]
- Delahunt, E.; Monaghan, K.; Caulfield, B. Altered neuromuscular control and ankle joint kinematics during walking in subjects with functional instability of the ankle joint. Am. J. Sports Med. 2006, 34, 1970–1976. [Google Scholar] [CrossRef] [PubMed]
- Ball, N.; Scurr, J. Electromyography normalization methods for high-velocity muscle actions: Review and recommendations. J. Appl. Biomech. 2013, 29, 600–608. [Google Scholar] [CrossRef] [Green Version]
- Feger, M.A.; Donovan, L.; Hart, J.M.; Hertel, J. Lower Extremity Muscle Activation During Functional Exercises in Patients With and Without Chronic Ankle Instability. PM R J. Inj. Funct. Rehabil. 2014, 6, 602–611. [Google Scholar] [CrossRef] [PubMed]
- Fong, D.T.; Chan, Y.Y.; Mok, K.M.; Yung, P.; Chan, K.M. Understanding acute ankle ligamentous sprain injury in sports. Sports Med. Arthrosc. Rehabil. Ther. Technol. SMARTT 2009, 1, 14. [Google Scholar] [CrossRef] [Green Version]
- Gehring, D.; Wissler, S.; Lohrer, H.; Nauck, T.; Gollhofer, A. Expecting ankle tilts and wearing an ankle brace influence joint control in an imitated ankle sprain mechanism during walking. Gait Posture 2014, 39, 894–898. [Google Scholar] [CrossRef]
- Konradsen, L.; Voigt, M.; Hojsgaard, C. Ankle inversion injuries: The role of the dynamic defense mechanism. Am. J. Sports Med. 1997, 25, 54–58. [Google Scholar] [CrossRef]
- Suda, E.Y.; Amorim, C.F.; Sacco Ide, C. Influence of ankle functional instability on the ankle electromyography during landing after volleyball blocking. J. Electromyogr. Kinesiol. Off. J. Int. Soc. Electrophysiol. Kinesiol. 2009, 19, e84–e93. [Google Scholar] [CrossRef]
- Lin, J.-Z.; Lin, Y.-A.; Lee, H.-J. Are Landing Biomechanics Altered in Elite Athletes with Chronic Ankle Instability. J. Sports Sci. Med. 2019, 18, 653. [Google Scholar] [PubMed]
- Santilli, V.; Frascarelli, M.A.; Paoloni, M.; Frascarelli, F.; Camerota, F.; De Natale, L.; De Santis, F. Peroneus longus muscle activation pattern during gait cycle in athletes affected by functional ankle instability: A surface electromyographic study. Am. J. Sports Med. 2005, 33, 1183–1187. [Google Scholar] [CrossRef] [PubMed]
- Sefton, J.; Hicks-Little, C.; Koceja, D.; Cordova, M. Effect of inversion and ankle bracing on peroneus longus Hoffmann reflex. Scand. J. Med. Sci. Sports 2007, 17, 539–546. [Google Scholar] [CrossRef] [PubMed]
- Delahunt, E.; Monaghan, K.; Caulfield, B. Changes in lower limb kinematics, kinetics, and muscle activity in subjects with functional instability of the ankle joint during a single leg drop jump. J. Orthop. Res. Off. Publ. Orthop. Res. Soc. 2006, 24, 1991–2000. [Google Scholar] [CrossRef]
- Ashton-Miller, J.A.; Ottaviani, R.A.; Hutchinson, C.; Wojtys, E.M. What best protects the inverted weightbearing ankle against further inversion? Evertor muscle strength compares favorably with shoe height, athletic tape, and three orthoses. Am. J. Sports Med. 1996, 24, 800–809. [Google Scholar] [CrossRef] [Green Version]
- Konradsen, L.; Voigt, M. Inversion injury biomechanics in functional ankle instability: A cadaver study of simulated gait. Scand. J. Med. Sci. Sports 2002, 12, 329–336. [Google Scholar] [CrossRef]
- Nashner, L.M. Fixed patterns of rapid postural responses among leg muscles during stance. Exp. Brain Res. 1977, 30, 13–24. [Google Scholar] [CrossRef]
- Shultz, S.J.; Perrin, D.H.; Adams, J.M.; Arnold, B.L.; Gansneder, B.M.; Granata, K.P. Assessment of neuromuscular response characteristics at the knee following a functional perturbation. J. Electromyogr. Kinesiol. 2000, 10, 159–170. [Google Scholar] [CrossRef]
- Mokhtarzadeh, H.; Yeow, C.H.; Goh, J.C.H.; Oetomo, D.; Malekipour, F.; Lee, P.V.-S. Contributions of the soleus and gastrocnemius muscles to the anterior cruciate ligament loading during single-leg landing. J. Biomech. 2013, 46, 1913–1920. [Google Scholar] [CrossRef]
- Brown, C.; Padua, D.; Marshall, S.W.; Guskiewicz, K. Individuals with mechanical ankle instability exhibit different motion patterns than those with functional ankle instability and ankle sprain copers. Clin. Biomech. 2008, 23, 822–831. [Google Scholar] [CrossRef]
- De Ridder, R.; Willems, T.; Vanrenterghem, J.; Robinson, M.A.; Palmans, T.; Roosen, P. Multi-segment foot landing kinematics in subjects with chronic ankle instability. Clin. Biomech. 2015, 30, 585–592. [Google Scholar] [CrossRef] [PubMed]
- Doherty, C.; Bleakley, C.; Hertel, J.; Caulfield, B.; Ryan, J.; Delahunt, E. Single-leg drop landing movement strategies 6 months following first-time acute lateral ankle sprain injury. Scand. J. Med. Sci. Sports 2015, 25, 806–817. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, M.; Youm, C.; Son, M.; Kim, J.; Kim, Y. Effects of chronic ankle instability and induced mediolateral muscular fatigue of the ankle on competitive taekwondo athletes. J. Phys. Ther. Sci. 2017, 29, 1329–1335. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, X.; Aeles, J.; Vanwanseele, B. Comparison of foot muscle morphology and foot kinematics between recreational runners with normal feet and with asymptomatic over-pronated feet. Gait Posture 2017, 54, 290–294. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.-Z.; Tai, W.-H.; Chiu, L.-Y.; Lin, Y.-A.; Lee, H.-J. The effect of divided attention with bounce drop jump on dynamic postural stability. Int. J. Sports Med. 2020, 41, 776–782. [Google Scholar] [PubMed]
- Caulfield, B.; Garrett, M. Changes in ground reaction force during jump landing in subjects with functional instability of the ankle joint. Clin. Biomech. 2004, 19, 617–621. [Google Scholar] [CrossRef]
- Bigouette, J.; Simon, J.; Liu, K.; Docherty, C.L. Altered vertical ground reaction forces in participants with chronic ankle instability while running. J. Athl. Train. 2016, 51, 682–687. [Google Scholar] [CrossRef] [Green Version]
- Boden, B.P.; Dean, G.S.; Feagin, J.A.; Garrett, W.E. Mechanisms of anterior cruciate ligament injury. Orthopedics 2000, 23, 573–578. [Google Scholar] [CrossRef]
- Bates, N.A.; Ford, K.R.; Myer, G.D.; Hewett, T.E. Kinetic and kinematic differences between first and second landings of a drop vertical jump task: Implications for injury risk assessments. Clin. Biomech. 2013, 28, 459–466. [Google Scholar] [CrossRef] [Green Version]
- Attenborough, A.S.; Hiller, C.E.; Smith, R.M.; Stuelcken, M.; Greene, A.; Sinclair, P.J. Chronic ankle instability in sporting populations. Sports Med. 2014, 44, 1545–1556. [Google Scholar] [CrossRef]
- Louw, Q.; Grimmer, K. Biomechanical factors associated with the risk of knee injury when landing from a jump. S. Afr. J. Sports Med. 2006, 18, 18–23. [Google Scholar] [CrossRef] [Green Version]
- McNair, P.J.; Prapavessis, H. Normative data of vertical ground reaction forces during landing from a jump. J. Sci. Med. Sport 1999, 2, 86–88. [Google Scholar] [CrossRef]
- Williams III, D.S.; Davis, I.M.; Scholz, J.P.; Hamill, J.; Buchanan, T.S. High-arched runners exhibit increased leg stiffness compared to low-arched runners. Gait Posture 2004, 19, 263–269. [Google Scholar] [CrossRef]
- Song, K.; Wikstrom, E.A. Plausible mechanisms of and techniques to assess ankle joint degeneration following lateral ankle sprains: A narrative review. Physician Sportsmed. 2019, 47, 275–283. [Google Scholar] [CrossRef] [PubMed]
- Valderrabano, V.; Horisberger, M.; Russell, I.; Dougall, H.; Hintermann, B. Etiology of ankle osteoarthritis. Clin. Orthop. Relat. Res. 2009, 467, 1800–1806. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gribble, P.A.; Robinson, R.H. Alterations in knee kinematics and dynamic stability associated with chronic ankle instability. J. Athl. Train. 2009, 44, 350. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dai, B.; Cook, R.F.; Meyer, E.A.; Sciascia, Y.; Hinshaw, T.J.; Wang, C.; Zhu, Q. The effect of a secondary cognitive task on landing mechanics and jump performance. Sports Biomech. Int. Soc. Biomech. Sports 2018, 17, 192–205. [Google Scholar] [CrossRef]
- Krosshaug, T.; Nakamae, A.; Boden, B.P.; Engebretsen, L.; Smith, G.; Slauterbeck, J.R.; Hewett, T.E.; Bahr, R. Mechanisms of anterior cruciate ligament injury in basketball: Video analysis of 39 cases. Am. J. Sports Med. 2007, 35, 359–367. [Google Scholar] [CrossRef]
- Wikstrom, E.A.; Naik, S.; Lodha, N.; Cauraugh, J.H. Bilateral balance impairments after lateral ankle trauma: A systematic review and meta-analysis. Gait Posture 2010, 31, 407–414. [Google Scholar] [CrossRef]
- Munn, J.; Sullivan, S.J.; Schneiders, A.G. Evidence of sensorimotor deficits in functional ankle instability: A systematic review with meta-analysis. J. Sci. Med. Sport 2010, 13, 2–12. [Google Scholar] [CrossRef]
- Arnold, B.L.; De La Motte, S.; Linens, S.; Ross, S.E. Ankle instability is associated with balance impairments: A meta-analysis. Med. Sci. Sports Exerc. 2009, 41, 1048–1062. [Google Scholar] [CrossRef] [Green Version]
- McKeon, P.O.; Hertel, J. Systematic review of postural control and lateral ankle instability, part I: Can deficits be detected with instrumented testing? J. Athl. Train. 2008, 43, 293–304. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wright, C.J.; Arnold, B.L.; Ross, S.E. Altered kinematics and time to stabilization during drop-jump landings in individuals with or without functional ankle instability. J. Athl. Train. 2016, 51, 5–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ross, S.E.; Guskiewicz, K.M. Examination of static and dynamic postural stability in individuals with functionally stable and unstable ankles. Clin. J. Sport Med. 2004, 14, 332–338. [Google Scholar] [CrossRef] [PubMed]
- Wikstrom, E.A.; Tillman, M.D.; Chmielewski, T.L.; Cauraugh, J.H.; Borsa, P.A. Dynamic Postural Stability Deficits in Subjects with Self-Reported Ankle Instability. Med. Sci. Sports Exerc. 2007, 39, 397. [Google Scholar] [CrossRef]
- McKinley, P.; Pedotti, A. Motor strategies in landing from a jump: The role of skill in task execution. Exp. Brain Res. 1992, 90, 427–440. [Google Scholar] [CrossRef]
- Pai, Y.-C.; Patton, J. Center of mass velocity-position predictions for balance control. J. Biomech. 1997, 30, 347–354. [Google Scholar] [CrossRef]
- Park, W.; Singh, D.P.; Huston, R.L.; Song, S. A quantitative method for representing balance strategies of goal-directed human motions. Comput. Biol. Med. 2008, 38, 1094–1102. [Google Scholar] [CrossRef]
- Wikstrom, E.A.; Tillman, M.D.; Schenker, S.M.; Borsa, P.A. Jump-landing direction influences dynamic postural stability scores. J. Sci. Med. Sport 2008, 11, 106–111. [Google Scholar] [CrossRef]
- Lord, S.R.; CLARK, R.D.; Webster, I. Visual acuity and contrast sensitivity in relation to falls in an elderly population. Age Ageing 1991, 20, 175–181. [Google Scholar] [CrossRef]
- Schmidt, R.A.; Lee, T.D.; Winstein, C.; Wulf, G.; Zelaznik, H.N. Motor Control and Learning: A Behavioral Emphasis; Human kinetics: Champaign, IL, USA, 2018. [Google Scholar]
- Wikstrom, E.A.; Tillman, M.D.; Chmielewski, T.L.; Borsa, P.A. Measurement and evaluation of dynamic joint stability of the knee and ankle after injury. Sports Med. 2006, 36, 393–410. [Google Scholar] [CrossRef] [PubMed]
| System | Content |
|---|---|
| Sensory system | Vision, vestibular sense, proprioception, touch, vibration sense |
| Motor system | Muscle strength, neuromuscular control |
| Central nervous system | Integration of sensory and motor factor |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, J.-Z.; Lin, Y.-A.; Tai, W.-H.; Chen, C.-Y. Influence of Landing in Neuromuscular Control and Ground Reaction Force with Ankle Instability: A Narrative Review. Bioengineering 2022, 9, 68. https://doi.org/10.3390/bioengineering9020068
Lin J-Z, Lin Y-A, Tai W-H, Chen C-Y. Influence of Landing in Neuromuscular Control and Ground Reaction Force with Ankle Instability: A Narrative Review. Bioengineering. 2022; 9(2):68. https://doi.org/10.3390/bioengineering9020068
Chicago/Turabian StyleLin, Jian-Zhi, Yu-An Lin, Wei-Hsun Tai, and Chung-Yu Chen. 2022. "Influence of Landing in Neuromuscular Control and Ground Reaction Force with Ankle Instability: A Narrative Review" Bioengineering 9, no. 2: 68. https://doi.org/10.3390/bioengineering9020068
APA StyleLin, J.-Z., Lin, Y.-A., Tai, W.-H., & Chen, C.-Y. (2022). Influence of Landing in Neuromuscular Control and Ground Reaction Force with Ankle Instability: A Narrative Review. Bioengineering, 9(2), 68. https://doi.org/10.3390/bioengineering9020068






