The Impact of a New Arterial Intravascular Pump on Aorta Hemodynamic Surrounding: A Numerical Study
Abstract
1. Introduction
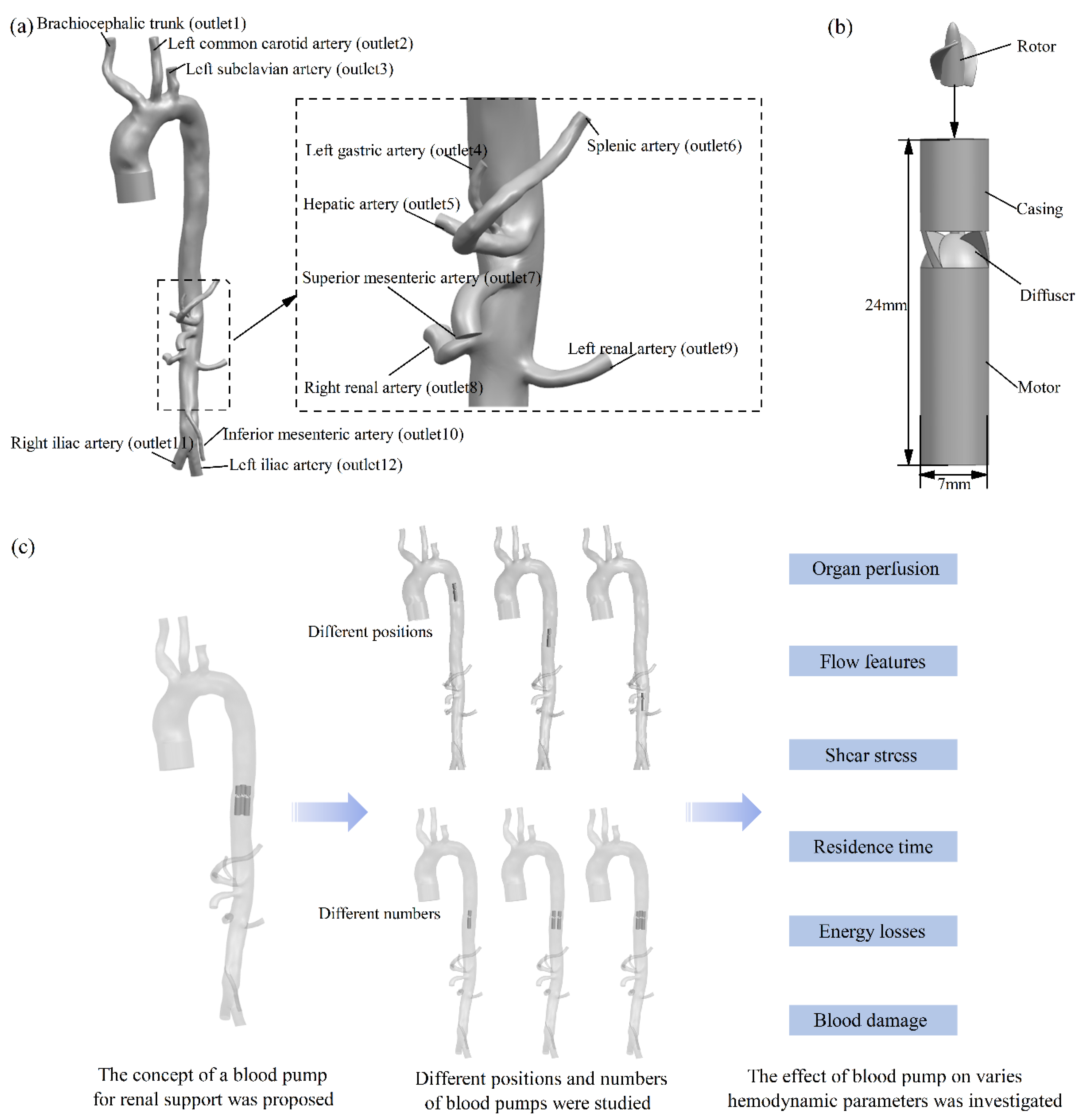
2. Materials and Methods
2.1. Studied Model and Variations
2.2. CFD Methods
2.3. Scalar Shear Stress Predictions
2.4. Residence Time Predictions
2.5. Energy Loss Predictions
2.6. Mesh Details and Sensitivity Analysis
3. Results
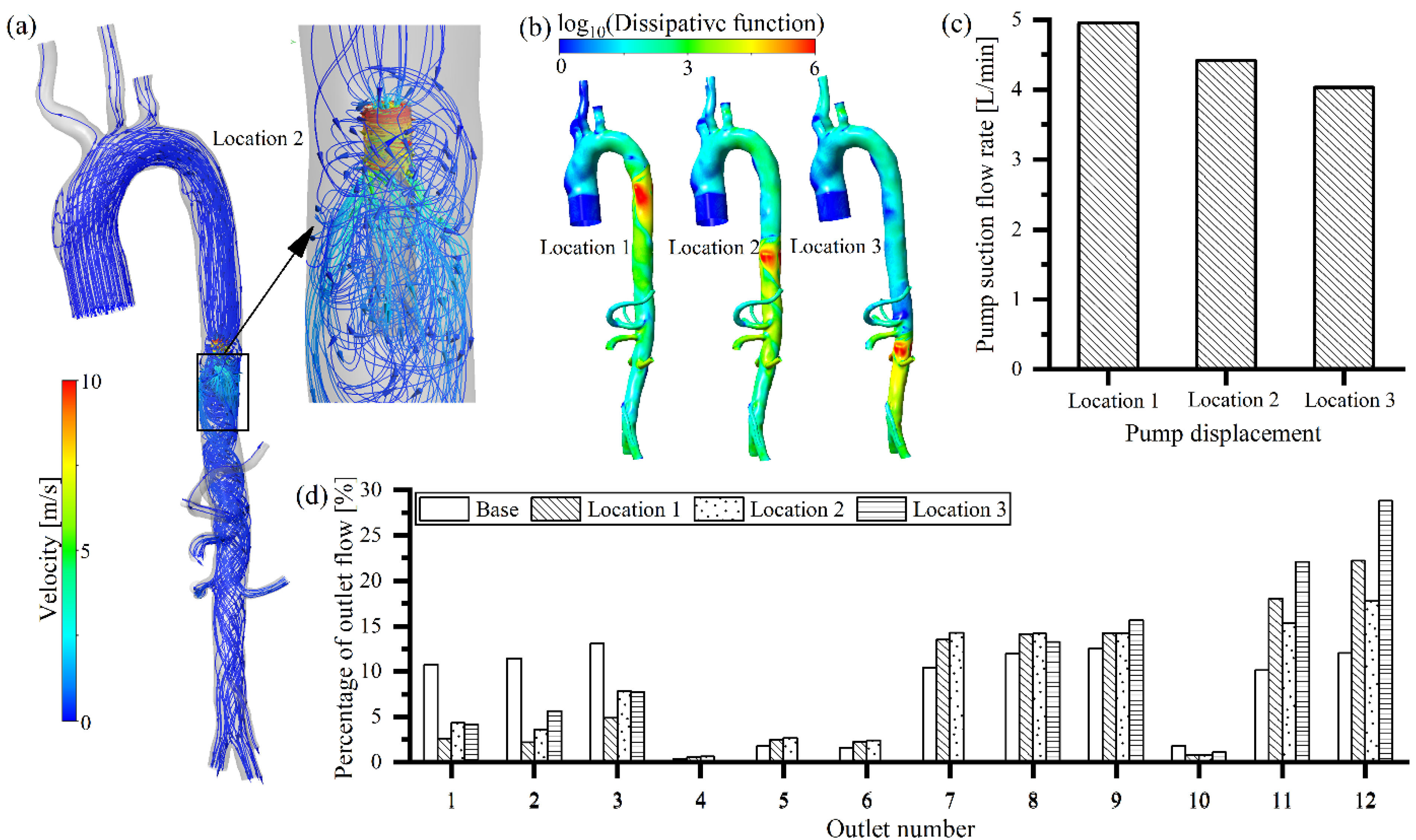
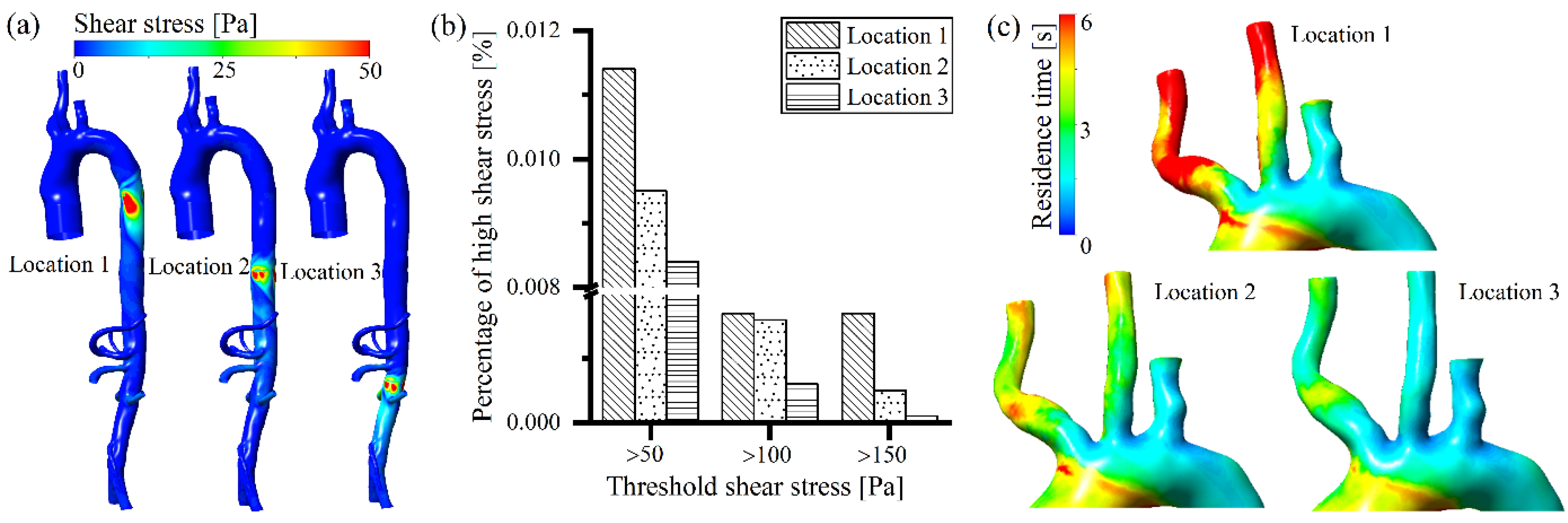
3.1. Effect of Different Positions of the Arterial Intravascular Pump
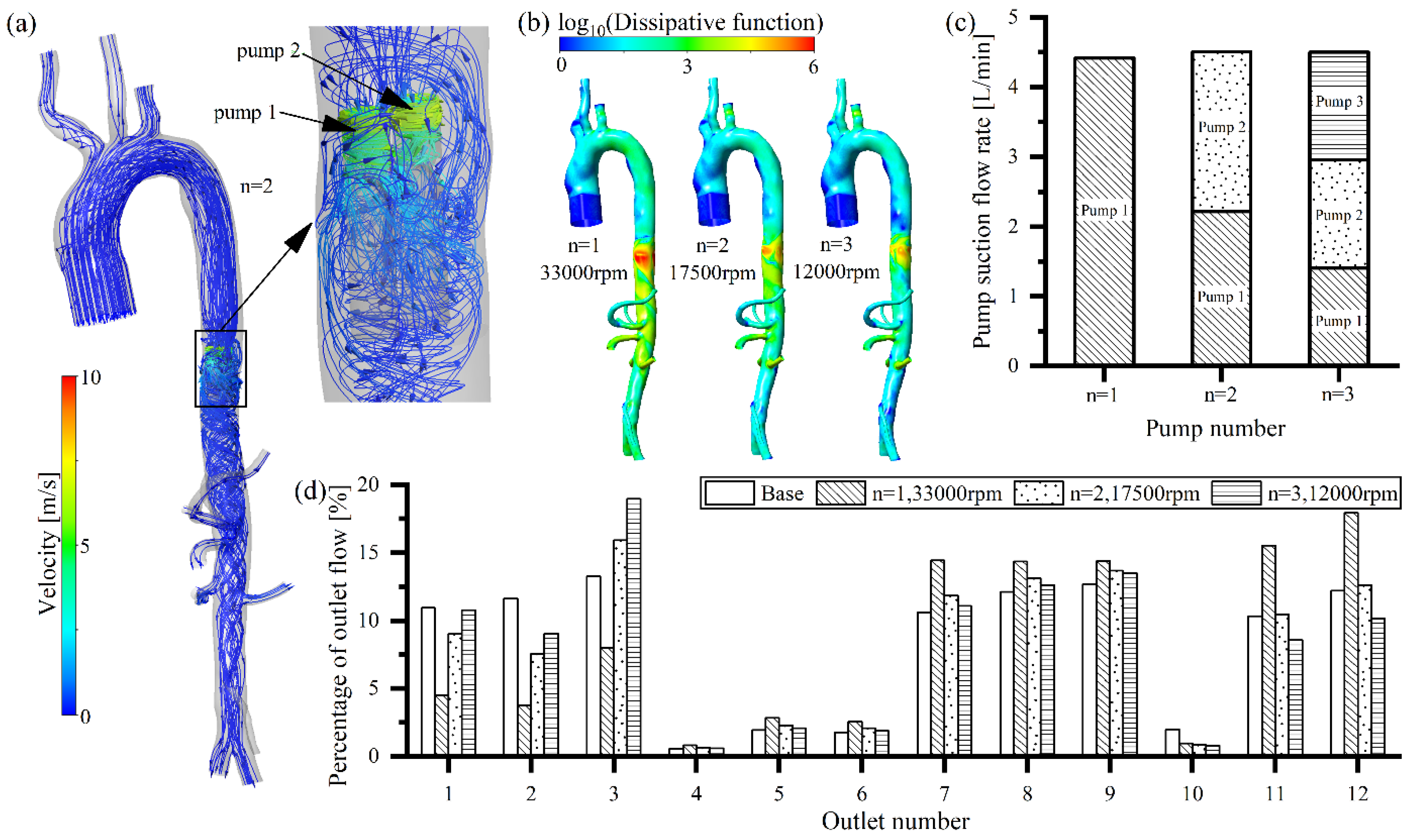
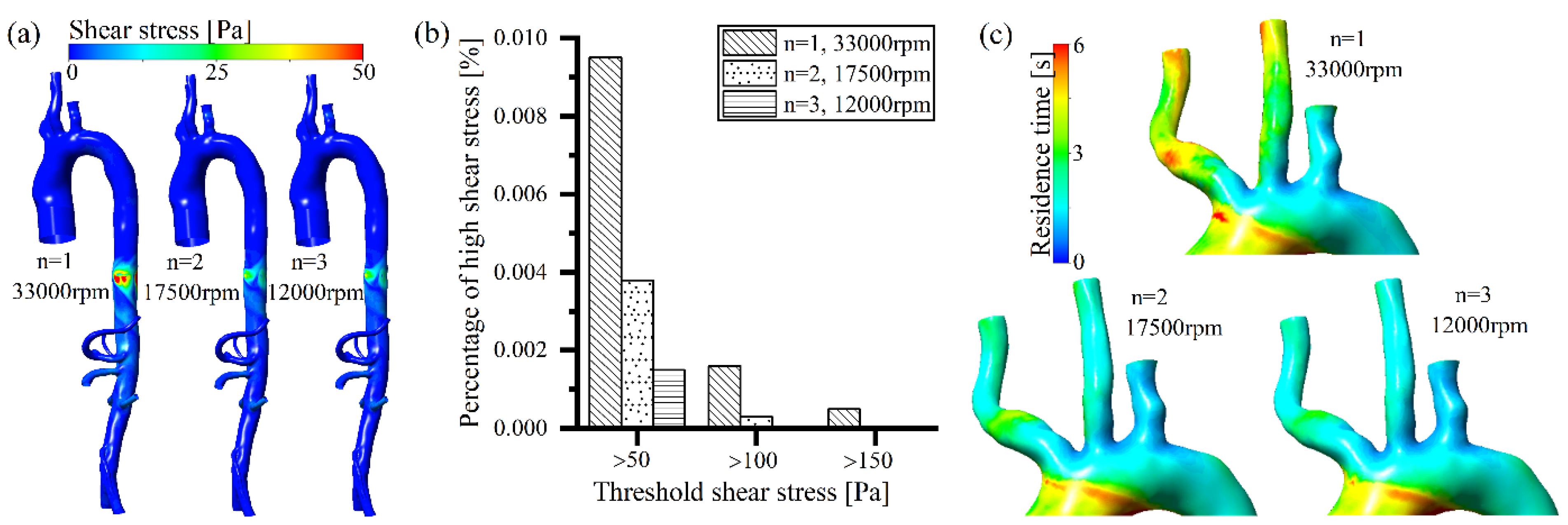
3.2. Effects of Different Numbers of Arterial Intravascular Pumps
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lin, L.; Chen, Y.; Han, D.; Yang, A.; Wang, A.Y.; Qi, W. Cardiorenal Syndrome in COVID-19 Patients: A Systematic Review. Front. Cardiovasc. Med. 2022, 9, 915533. [Google Scholar] [CrossRef] [PubMed]
- Kolben, Y.; Kessler, A.; Puris, G.; Nachman, D.; Alvarez, P.; Briasoulis, A.; Asleh, R. Management of heart failure with reduced ejection fraction: Challenges in patients with atrial fibrillation, renal disease and in the elderly. Rev. Cardiovasc. Med. 2022, 23, 16. [Google Scholar] [CrossRef] [PubMed]
- Go, A.S.; Mozaffarian, D.; Roger, V.L.; Benjamin, E.J.; Berry, J.D.; Borden, W.B.; Bravata, D.M.; Dai, S.; Ford, E.S.; Fox, C.S.; et al. Heart disease and stroke statistics—2013 update: A report from the American Heart Association. Circulation 2013, 127, e6–e245. [Google Scholar] [CrossRef] [PubMed]
- Polonsky, T.S.; Bakris, G.L. Heart Failure and Changes in Kidney Function: Focus on Understanding, Not Reacting. Heart Fail. Clin. 2019, 15, 455–461. [Google Scholar] [CrossRef] [PubMed]
- Verbrugge, F.H.; Guazzi, M.; Testani, J.M.; Borlaug, B.A. Altered Hemodynamics and End-Organ Damage in Heart Failure: Impact on the Lung and Kidney. Circulation 2020, 142, 998–1012. [Google Scholar] [CrossRef]
- Hou, F.F.; Yang, X. Advances in the Management of Acute Cardiorenal Syndrome in China: Biomarkers for Predicting Development and Outcomes. Kidney Dis. 2017, 2, 145–150. [Google Scholar] [CrossRef]
- Hu, W.; He, W.; Liu, W.; Fang, X.; Wu, Y.; Yu, F.; Hao, W. Risk Factors and Prognosis of Cardiorenal Syndrome Type 1 in Elderly Chinese Patients: A Retrospective Observational Cohort Study. Kidney Blood Press. Res. 2016, 41, 672–679. [Google Scholar] [CrossRef]
- Hadjiphilippou, S.; Kon, S.P. Cardiorenal syndrome: Review of our current understanding. J. R. Soc. Med. 2016, 109, 12–17. [Google Scholar] [CrossRef]
- Chávez-Iñiguez, J.S.; Sánchez-Villaseca, S.J.; García-Macías, L.A. Cardiorenal syndrome: Classification, pathophysiology, diagnosis and management. Literature review. Arch. Cardiol. Mex. 2022, 92, 253–263. [Google Scholar] [CrossRef]
- Damman, K.; Testani, J.M. The kidney in heart failure: An update. Eur. Heart J. 2015, 36, 1437–1444. [Google Scholar] [CrossRef] [PubMed]
- Hsu, P.L.; Cheng, S.J.; Saumarez, R.C.; Dawes, W.N.; McMahon, R.A. An extended computational model of the circulatory system for designing ventricular assist devices. ASAIO J. 2008, 54, 594–599. [Google Scholar] [CrossRef] [PubMed]
- Vora, A.N.; Schuyler Jones, W.; DeVore, A.D.; Ebner, A.; Clifton, W.; Patel, M.R. First-in-human experience with Aortix intraaortic pump. Catheter. Cardiovasc. Interv. 2019, 93, 428–433. [Google Scholar] [CrossRef] [PubMed]
- Annamalai, S.K.; Esposito, M.L.; Reyelt, L.A.; Natov, P.; Jorde, L.E.; Karas, R.H.; Kapur, N.K. Abdominal Positioning of the Next-Generation Intra-Aortic Fluid Entrainment Pump (Aortix) Improves Cardiac Output in a Swine Model of Heart Failure. Circ. Heart Fail. 2018, 11, e005115. [Google Scholar] [CrossRef] [PubMed]
- Shabari, F.R.; George, J.; Cuchiara, M.P.; Langsner, R.J.; Heuring, J.J.; Cohn, W.E.; Hertzog, B.A.; Delgado, R. Improved hemodynamics with a novel miniaturized intra-aortic axial flow pump in a porcine model of acute left ventricular dysfunction. ASAIO J. 2013, 59, 240–245. [Google Scholar] [CrossRef]
- Yuan, L.; Yifeng, X.; Hongyu, W.; Anqiang, S.; Xiaoyan, D.; Zengsheng, C.; Yubo, F. A new way to evaluate thrombotic risk in failure heart and ventricular assist devices. Med. Nov. Technol. Devices 2022, 16, 100135. [Google Scholar]
- Inc, Puzzle Medical. Available online: https://www.puzzlemed.com/ (accessed on 2 September 2022).
- Li, Y.; Yu, J.; Wang, H.; Xi, Y.; Deng, X.; Chen, Z.; Fan, Y. Investigation of the influence of blade configuration on the hemodynamic performance and blood damage of the centrifugal blood pump. Artif. Organs 2022, 46, 1817–1832. [Google Scholar] [CrossRef]
- Chen, Z.; Jena, S.K.; Giridharan, G.A.; Koenig, S.C.; Slaughter, M.S.; Griffith, B.P.; Wu, Z.J. Flow features and device-induced blood trauma in CF-VADs under a pulsatile blood flow condition: A CFD comparative study. Int. J. Numer. Methods Biomed. Eng. 2018, 34, e2924. [Google Scholar] [CrossRef]
- Semenzin, C.S.; Simpson, B.; Gregory, S.D.; Tansley, G. Validated Guidelines for Simulating Centrifugal Blood Pumps. Cardiovasc. Eng. Technol. 2021, 12, 273–285. [Google Scholar] [CrossRef]
- Day, S.W.; McDaniel, J.C.; Wood, H.G.; Allaire, P.E.; Song, X.; Lemire, P.P.; Miles, S.D. A prototype HeartQuest ventricular assist device for particle image velocimetry measurements. Artif. Organs 2002, 26, 1002–1005. [Google Scholar] [CrossRef]
- Wu, P.; Huo, J.; Dai, W.; Wu, W.T.; Yin, C.; Li, S. On the Optimization of a Centrifugal Maglev Blood Pump Through Design Variations. Front. Physiol. 2021, 12, 699891. [Google Scholar] [CrossRef]
- Wu, P.; Xiang, W.; Yin, C.; Li, S. The Design and Evaluation of a Portable Extracorporeal Centrifugal Blood Pump. Front. Physiol. 2021, 12, 766867. [Google Scholar] [CrossRef] [PubMed]
- Vercaemst, L.; Vandezande, E.; Janssens, P.; Yvan, T.; Peter, D.; Meyns, B. Impella-A Miniaturized Cardiac Support System in an Era of Minimal Invasive Cardiac Surgery. J. Am. Soc. Extra-Corpor. Technol. 2002, 34, 92–100. [Google Scholar]
- Taskin, M.E.; Fraser, K.H.; Zhang, T.; Wu, C.; Griffith, B.P.; Wu, Z.J. Evaluation of Eulerian and Lagrangian models for hemolysis estimation. ASAIO J. 2012, 58, 363–372. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Wang, H.; Xi, Y.; Sun, A.; Deng, X.; Chen, Z.; Fan, Y. Impact of volute design features on hemodynamic performance and hemocompatibility of centrifugal blood pumps used in ECMO. Artif. Organs 2022. [Google Scholar] [CrossRef] [PubMed]
- Rayz, V.L.; Boussel, L.; Ge, L.; Leach, J.R.; Martin, A.J.; Lawton, M.T.; McCulloch, C.; Saloner, D. Flow residence time and regions of intraluminal thrombus deposition in intracranial aneurysms. Ann. Biomed. Eng. 2010, 38, 3058–3069. [Google Scholar] [CrossRef]
- Delgado-Montero, A.; Martinez-Legazpi, P.; Desco, M.M.; Rodríguez-Pérez, D.; Díaz-Otero, F.; Rossini, L.; Pérez Del Villar, C.; Rodríguez-González, E.; Chazo, C.; Benito, Y.; et al. Blood Stasis Imaging Predicts Cerebral Microembolism during Acute Myocardial Infarction. J. Am. Soc. Echocardiogr. 2020, 33, 389–398. [Google Scholar] [CrossRef]
- Menichini, C.; Xu, X.Y. Mathematical modeling of thrombus formation in idealized models of aortic dissection: Initial findings and potential applications. J. Math. Biol. 2016, 73, 1205–1226. [Google Scholar] [CrossRef]
- Manchester, E.L.; Pirola, S.; Salmasi, M.Y.; O’Regan, D.P.; Athanasiou, T.; Xu, X.Y. Analysis of Turbulence Effects in a Patient-Specific Aorta with Aortic Valve Stenosis. Cardiovasc. Eng. Technol. 2021, 12, 438–453. [Google Scholar] [CrossRef]
- Zhang, J.X.; Yang, Z.H.; Fung, P.C.W. Dissipation function of the first-order phase transformation in solids via internal-friction measurements. Phys. Rev. B Condens. Matter 1995, 52, 268–277. [Google Scholar] [CrossRef]
- Fraser, K.H.; Taskin, M.E.; Griffith, B.P.; Wu, Z.J. The use of computational fluid dynamics in the development of ventricular assist devices. Med. Eng. Phys. 2011, 33, 263–280. [Google Scholar] [CrossRef]
- Fraser, K.H.; Zhang, T.; Taskin, M.E.; Griffith, B.P.; Wu, Z.J. A quantitative comparison of mechanical blood damage parameters in rotary ventricular assist devices: Shear stress, exposure time and hemolysis index. J. Biomech. Eng. 2012, 134, 081002. [Google Scholar] [CrossRef] [PubMed]
- Wiegmann, L.; Boes, S.; de Zelicourt, D.; Thamsen, B.; Schmid Daners, M.; Meboldt, M.; Kurtcuoglu, V. Blood Pump Design Variations and Their Influence on Hydraulic Performance and Indicators of Hemocompatibility. Ann. Biomed. Eng. 2018, 46, 417–428. [Google Scholar] [CrossRef] [PubMed]
- Lv, J.; Li, Y.; Shi, S.; Liu, S.; Xu, X.; Wu, H.; Zhang, B.; Song, Q. Frontier and Hotspot Evolution in Cardiorenal Syndrome: A Bibliometric Analysis From 2003 to 2022. Curr. Probl. Cardiol. 2022. [Google Scholar] [CrossRef] [PubMed]
- Kosiorek, A.; Biegus, J.; Rozentryt, P.; Hurkacz, M.; Zymliński, R. Cardiorenal syndrome: Decongestion in heart failure across wide spectrum of kidney pathophysiology. Adv. Clin. Exp. Med. 2022, 31, 445–455. [Google Scholar] [CrossRef] [PubMed]
- Nezami, F.R.; Khodaee, F.; Edelman, E.R.; Keller, S.P. A Computational Fluid Dynamics Study of the Extracorporeal Membrane Oxygenation-Failing Heart Circulation. ASAIO J. 2021, 67, 276–283. [Google Scholar] [CrossRef]

| Outlet Number | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Static Pressure (mmHg) | 101 | 100 | 102 | 103 | 103 | 103 | 103 | 102 | 99 | 103 | 104 | 104 |
| Rotating Speed (rpm) | Flow Rate (L/min) |
|---|---|
| 10,000 | 0.0–1.4 |
| 17,000 | 0.5–2.6 |
| 20,000 | 0.5–3.1 |
| 22,000 | 0.9–3.4 |
| 24,000 | 1.4–3.7 |
| 26,000 | 1.8–4.0 |
| 28,000 | 2.6–4.4 |
| 30,000 | 3.4–4.7 |
| 33,000 | 4.2–5.3 |
| Energy Losses | Variable | r2 |
|---|---|---|
| Mean dissipation | Shear stress above 50 Pa | 0.96 |
| Shear stress above 150 Pa | 0.72 | |
| Shear stress above 100 Pa | 0.68 | |
| Shear stress above 50 Pa | 0.78 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, Y.; Xi, Y.; Wang, H.; Sun, A.; Deng, X.; Chen, Z.; Fan, Y. The Impact of a New Arterial Intravascular Pump on Aorta Hemodynamic Surrounding: A Numerical Study. Bioengineering 2022, 9, 547. https://doi.org/10.3390/bioengineering9100547
Li Y, Xi Y, Wang H, Sun A, Deng X, Chen Z, Fan Y. The Impact of a New Arterial Intravascular Pump on Aorta Hemodynamic Surrounding: A Numerical Study. Bioengineering. 2022; 9(10):547. https://doi.org/10.3390/bioengineering9100547
Chicago/Turabian StyleLi, Yuan, Yifeng Xi, Hongyu Wang, Anqiang Sun, Xiaoyan Deng, Zengsheng Chen, and Yubo Fan. 2022. "The Impact of a New Arterial Intravascular Pump on Aorta Hemodynamic Surrounding: A Numerical Study" Bioengineering 9, no. 10: 547. https://doi.org/10.3390/bioengineering9100547
APA StyleLi, Y., Xi, Y., Wang, H., Sun, A., Deng, X., Chen, Z., & Fan, Y. (2022). The Impact of a New Arterial Intravascular Pump on Aorta Hemodynamic Surrounding: A Numerical Study. Bioengineering, 9(10), 547. https://doi.org/10.3390/bioengineering9100547









