A New Orthodontic-Surgical Approach to Mandibular Retrognathia
Abstract
1. Introduction
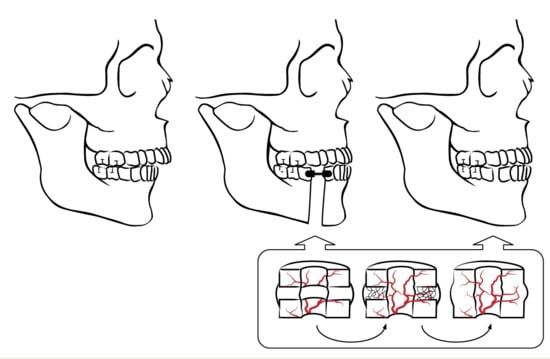
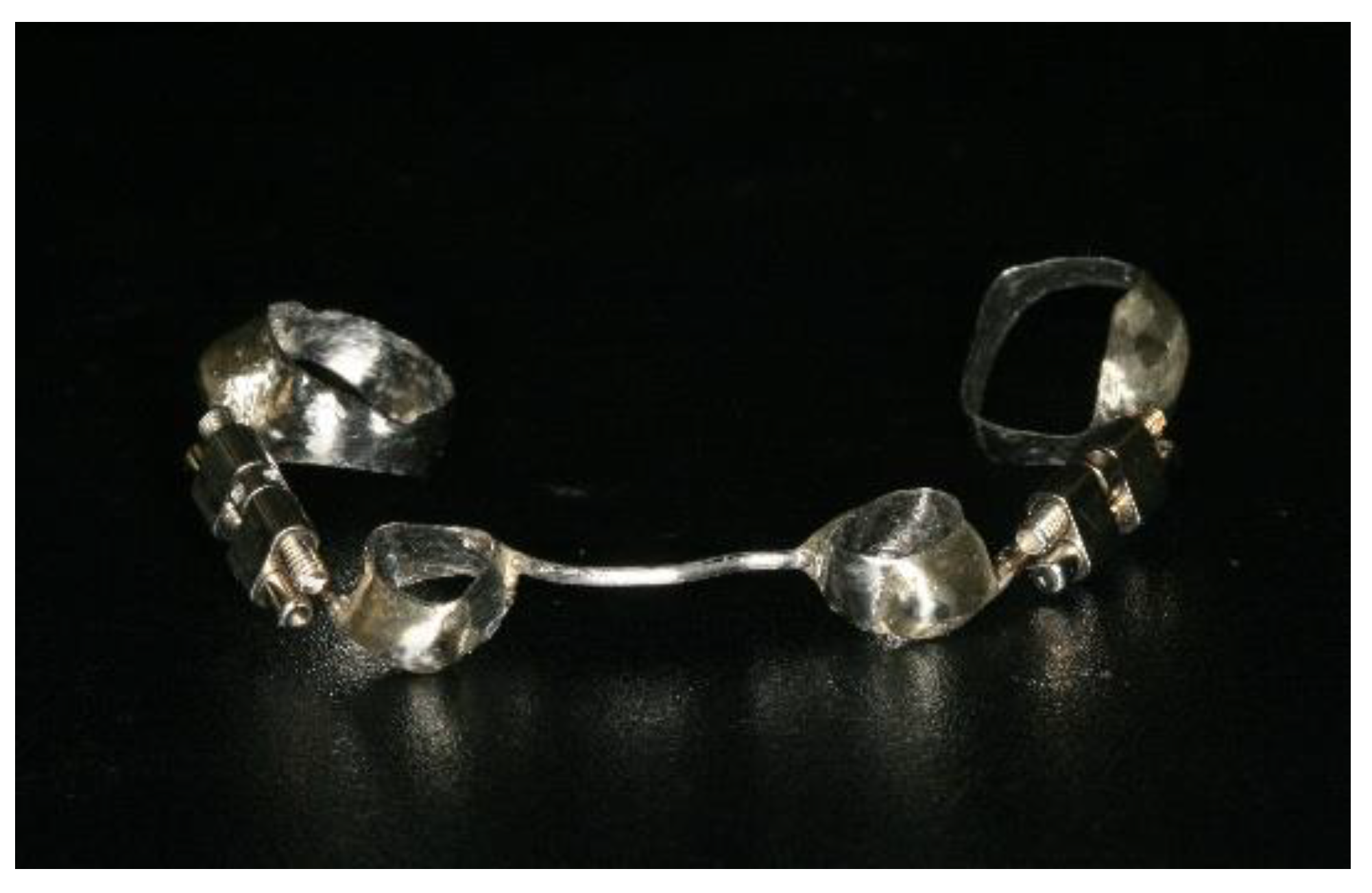
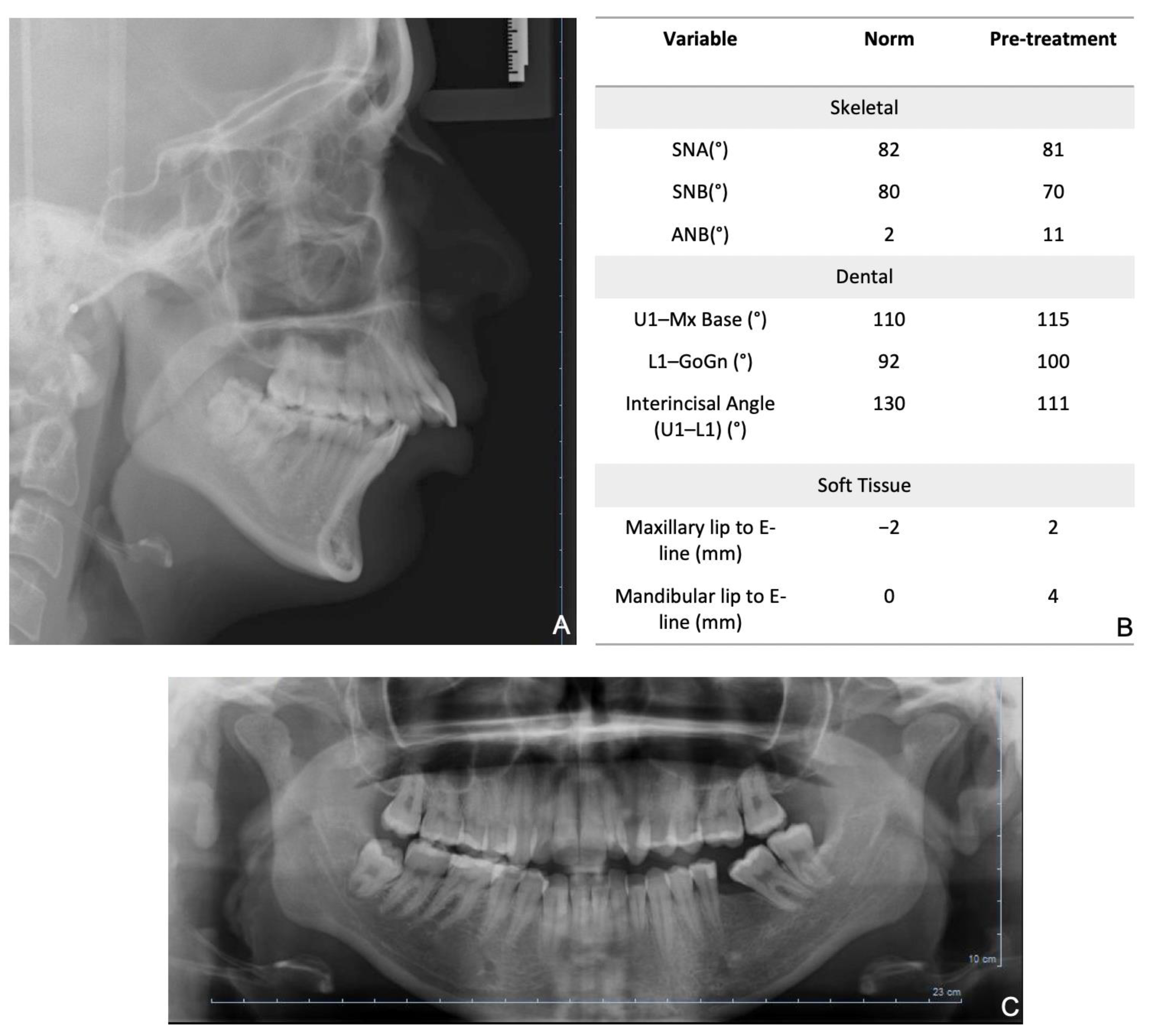
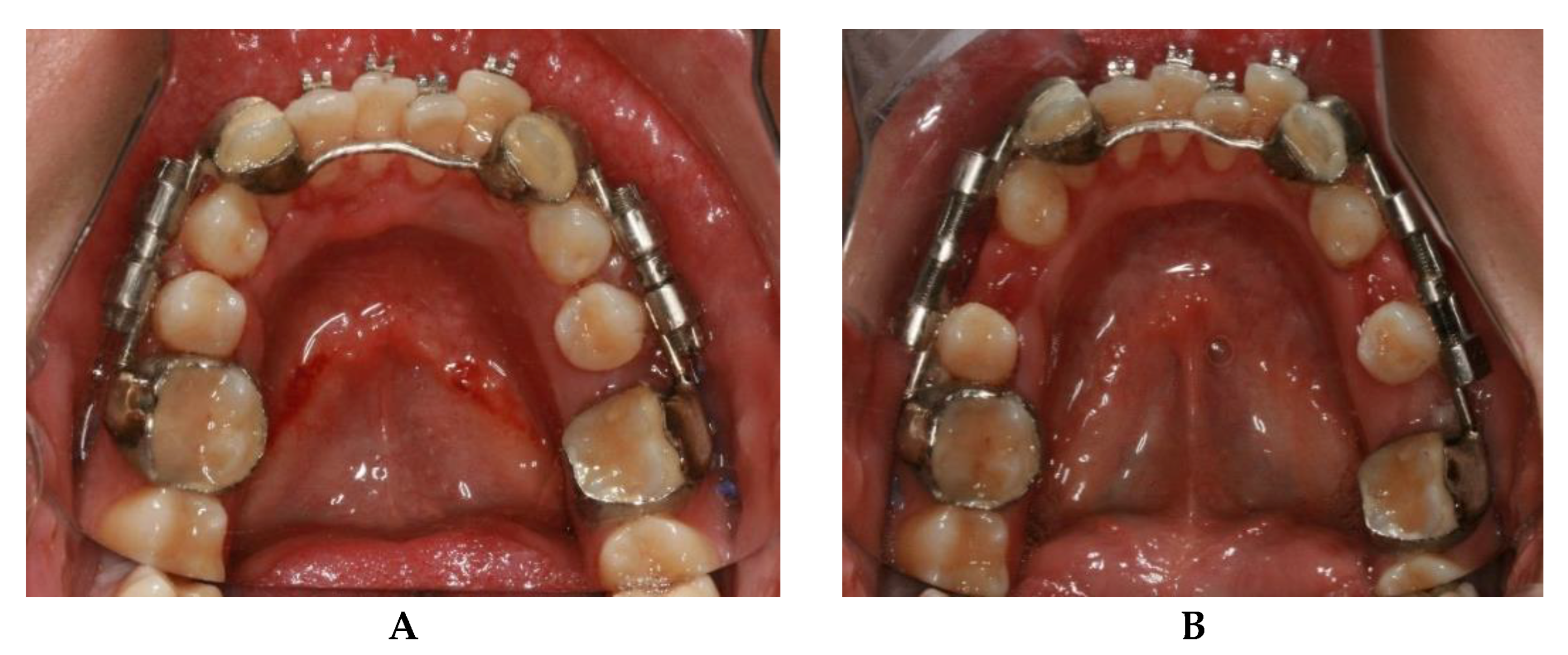
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Al-Moraissi, E.A.; Ellis, E. Bilateral Sagittal Split Ramus Osteotomy Versus Distraction Osteogenesis for Advancement of the Retrognathic Mandible. J. Oral Maxillofac. Surg. 2015, 73, 1564–1574. [Google Scholar] [CrossRef] [PubMed]
- Proffit, W.R.; Jackson, T.H.; Turvey, T.A. Changes in the Pattern of Patients Receiving Surgical-Orthodontic Treatment. Am. J. Orthod. Dentofacial Orthop. 2013, 143, 793–798. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; McGrath, C.; Hägg, U. The Impact of Malocclusion and Its Treatment on Quality of Life: A Literature Review. Int. J. Paediatr. Dent. 2006, 16, 381–387. [Google Scholar] [CrossRef] [PubMed]
- Bernabé, E.; Sheiham, A.; De Oliveira, C.M. Condition-Specific Impacts on Quality of Life Attributed to Malocclusion by Adolescents with Normal Occlusion and Class I, II and III Malocclusion. Angle Orthod. 2008, 78, 977–982. [Google Scholar] [CrossRef] [PubMed]
- Aronson, J.; Shen, X. Experimental Healing of Distraction Osteogenesis Comparing Metaphyseal with Diaphyseal Sites. Clin. Orthop. 1994, 301, 25–30. [Google Scholar] [CrossRef]
- Aronson, J.; Gao, G.G.; Shen, X.C.; McLaren, S.G.; Skinner, R.A.; Badger, T.M.; Lumpkin, C.K. The Effect of Aging on Distraction Osteogenesis in the Rat. J. Orthop. Res. 2001, 19, 421–427. [Google Scholar] [CrossRef]
- Franco, J.E.; Van Sickels, J.E.; Thrash, W.J. Factors Contributing to Relapse in Rigidly Fixed Mandibular Setbacks. J. Oral Maxillofac. Surg. 1989, 47, 451–456. [Google Scholar] [CrossRef]
- Ueki, K.; Nakagawa, K.; Marukawa, K.; Takazakura, D.; Shimada, M.; Takatsuka, S.; Yamamoto, E. Changes in Condylar Long Axis and Skeletal Stability after Bilateral Sagittal Split Ramus Osteotomy with Poly-l-Lactic Acid or Titanium Plate Fixation. Int. J. Oral Maxillofac. Surg. 2005, 34, 627–634. [Google Scholar] [CrossRef]
- Tucker, M.R. Management of Severe Mandibular Retrognathia in the Adult Patient Using Traditional Orthognathic Surgery. J. Oral Maxillofac. Surg. 2002, 60, 1334–1340. [Google Scholar] [CrossRef]
- Swennen, G.; Schliephake, H.; Dempf, R.; Schierle, H.; Malevez, C. Craniofacial Distraction Osteogenesis: A Review of the Literature. Part 1: Clinical Studies. Int. J. Oral Maxillofac. Surg. 2001, 30, 89–103. [Google Scholar] [CrossRef]
- Diner, P.A.; Kollar, E.M.; Martinez, H.; Vazquez, M.P. Intraoral Distraction for Mandibular Lengthening: A Technical Innovation. J. Craniomaxillofac. Surg. 1996, 24, 92–95. [Google Scholar] [CrossRef]
- Huang, C.-S.; Ko, W.-C.; Lin, W.-Y.; Liou, E.J.-W.; Hong, K.-F.; Chen, Y.-R. Mandibular Lengthening by Distraction Osteogenesis in Children-A One-Year Follow-Up Study. Cleft Palate Craniofac. J. 1999, 36, 269–274. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.R.; Rutrick, R.E.; Burstein, F.D. Distraction Osteogenesis of the Human Craniofacial Skeleton: Initial Experience with a New Distraction System. J. Craniofac. Surg. 1995, 6, 368–374. [Google Scholar] [CrossRef] [PubMed]
- Brevi, B.C.; Toma, L.; Magri, A.S.; Sesenna, E. Use of the Mandibular Distraction Technique to Treat Obstructive Sleep Apnea Syndrome. J. Oral Maxillofac. Surg. 2011, 69, 566–571. [Google Scholar] [CrossRef] [PubMed]
- Codivilla, A.; Brand, R.A. The Classic: On the Means of Lengthening, in the Lower Limbs, the Muscles and Tissues Which Are Shortened through Deformity. Clin. Orthop. 2008, 466, 2903–2909. [Google Scholar] [CrossRef]
- Havlik, R.J.; Bartlett, S.P. Mandibular Distraction Lengthening in the Severely Hypoplastic Mandible: A Problematic Case with Tongue Aplasia. J. Craniofac. Surg. 1994, 5, 305–310. [Google Scholar] [CrossRef] [PubMed]
- Akkerman, V. Verlenging van de Onderkaak: Bilaterale Sagittale Splijtingsosteotomie versus Distractieosteogenese. Ned. Tijdschr. Tandheelkd. 2015, 122, 603–608. [Google Scholar] [CrossRef][Green Version]
- Kloukos, D.; Fudalej, P.; Sequeira-Byron, P.; Katsaros, C. Maxillary Distraction Osteogenesis versus Orthognathic Surgery for Cleft Lip and Palate Patients. Cochrane Database Syst. Rev. 2018, 8, CD010403. [Google Scholar] [CrossRef]
- Braumann, B.; Niederhagen, B.; Schmolke, C. Mandibular Distraction Osteogenesis-Preliminary Results of an Animal Study with a Dentally Fixed Distraction Device. J. Orofac. Orthop. Fortschr. Kieferorthopädie 1997, 58, 298–305. [Google Scholar] [CrossRef]
- Guerrero, C.A.; Bell, W.H.; Contasti, G.I.; Rodriguez, A.M. Mandibular Widening by Intraoral Distraction Osteogenesis. Br. J. Oral Maxillofac. Surg. 1997, 35, 383–392. [Google Scholar] [CrossRef]
- Carls, F.R.; Sailer, H.F. Seven Years Clinical Experience with Mandibular Distraction in Children. J. Craniomaxillofac. Surg. 1998, 26, 197–208. [Google Scholar] [CrossRef]
- Chung, M.D.; Rivera, R.D.; Feinberg, S.E.; Sastry, A.M. An Implantable Battery System for a Continuous Automatic Distraction Device for Mandibular Distraction Osteogenesis. J. Med. Devices Trans. ASME 2010, 4, 1–6. [Google Scholar] [CrossRef]
- Andrade, N.; Gandhewar, T.; Kalra, R. Development and Evolution of Distraction Devices: Use of Indigenous Appliances for Distraction Osteogenesis-An Overview. Ann. Maxillofac. Surg. 2011, 1, 58. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, J.G.; Gregory, L.S.; Breitbart, A.S.; Grayson, B.H.; Bookstein, F.L. The Le Fort III Advancement OSteotomy in the Child under 7 Years of Age. Plast. Reconstr. Surg. 1990, 86, 647–649. [Google Scholar] [CrossRef]
- Razdolsky, Y.; Pensler, J.M.; Dessner, S. Skeletal Distraction for Mandibular Lengthening with a Completely Intraoral Toothborn Distractor. In Advances in Craniofacial Orthopedics; McNamara, J., Trotman, C., Eds.; Craniofacial Growth Series; Center for Human Growth and Development; University of Michigan: Ann Arbor, MI, USA, 1998; Volume 34, pp. 117–140. [Google Scholar]
- Francisco, V. Distração Osteogénica Mandibular Dento-Ancorada. Ph.D. Thesis, University of Coimbra, Coimbra, Portugal, 2014. [Google Scholar]
- Ilizarov, G. The Tension-Stress Effect on the Genesis and Growth of Tissues. Part I. The Influence of Stability of Fixation and Soft-Tissue Preservation. Clin. Orthop. Relat. Res. 1989, 238, 249–281. [Google Scholar] [CrossRef]
- Molina, F.; Monasterio, F.O. Mandibular Elongation and Remodeling by Distraction: A Farewell to Major Osteotomies. Plast. Reconstr. Surg. 1995, 841–842. [Google Scholar] [CrossRef]
- Labbé, D.; Nicolas, J.; Kaluzinski, E.; Soubeyrand, E.; Sabin, P.; Compère, J.F.; Bénateau, H. Gunshot Wounds: Reconstruction of the Lower Face by Osteogenic Distraction. Plast. Reconstr. Surg. 2005, 116, 1596–1603. [Google Scholar] [CrossRef] [PubMed]
- Van Sickels, J.E. Distraction Osteogenesis: Advancements in the Last 10 Years. Oral Maxillofac. Surg. Clin. N. Am. 2007, 19, 565–574. [Google Scholar] [CrossRef]
- Cope, J.B.; Samchukov, M.L.; Cherkashin, A.M. Mandibular Distraction Osteogenesis: A Historic Perspective and Future Directions. Am. J. Orthod. Dentofac. Orthop. 1999, 115, 448–460. [Google Scholar] [CrossRef]
- Barbosa, G.L.R.; Pimenta, L.A.; Pretti, H.; Golden, B.A.; Roberts, J.; Drake, A.F. Difference in maxillary sinus volumes of patients with cleft lip and palate. Int. J. Pediatr. Otorhinolaryngol. 2014, 78, 2234–2236. [Google Scholar] [CrossRef]
- Lin, S.J.; Roy, S.; Patel, P.K. Distraction osteogenesis in the pediatric population. Otolaryngol. Head Neck Surg. 2007, 137, 233–238. [Google Scholar] [CrossRef] [PubMed]
- Dessner, S.; Razdolsky, Y.; El-Bialy, T.; Evans, C.A. Mandibular Lengthening Using Preprogrammed Intraoral Tooth-Borne Distraction Devices. J. Oral Maxillofac. Surg. 1999, 57, 1318–1322. [Google Scholar] [CrossRef]
- Conley, R.; Legan, H. Mandibular Symphyseal Distraction Osteogenesis: Diagnosis and Treatment Planning Considerations. Angle Orthod. 2003, 73, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Vale, F.; Travassos, R.; Martins, J.; Figueiredo, J.P.; Marcelino, J.P.; Francisco, I. Radiographic healing patterns after tooth-borne distraction in canine model. J. Clin. Exp. Dent. 2021, 13, e866–e872. [Google Scholar] [CrossRef]
- McCarthy, J.G.; Williams, J.K.; Grayson, B.H.; Crombie, J.S. Controlled multiplanar distraction of the mandible: Device development and clinical application. J. Craniofac. Surg. 1998, 9, 322–329. [Google Scholar] [CrossRef]
- Shilo, D.; Emodi, O.; Aizenbud, D.; Rachmiel, A. Controlling the vector of distraction osteogenesis in the management of obstructive sleep apnea. Ann. Maxillofac. Surg. 2016, 6, 214–218. [Google Scholar] [CrossRef]
- Suffern, R.; Miskry, S.; Osher, J. Contemporary 3D planning for distraction osteogenesis creating predictable outcomes. Adv. Oral Maxillofac. Surg. 2021, 3, 100098. [Google Scholar] [CrossRef]
- Silveira, A.; Moura, P.M.; Harshbarger, R.J. Orthodontic Considerations for Maxillary Distraction Osteogenesis in Growing Patients with Cleft Lip and Palate Using Internal Distractors. Semin. Plast. Surg. 2014, 28, 207–212. [Google Scholar] [CrossRef]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vale, F.; Queiroga, J.; Pereira, F.; Ribeiro, M.; Marques, F.; Travassos, R.; Nunes, C.; Paula, A.B.; Francisco, I. A New Orthodontic-Surgical Approach to Mandibular Retrognathia. Bioengineering 2021, 8, 180. https://doi.org/10.3390/bioengineering8110180
Vale F, Queiroga J, Pereira F, Ribeiro M, Marques F, Travassos R, Nunes C, Paula AB, Francisco I. A New Orthodontic-Surgical Approach to Mandibular Retrognathia. Bioengineering. 2021; 8(11):180. https://doi.org/10.3390/bioengineering8110180
Chicago/Turabian StyleVale, Francisco, Joana Queiroga, Flávia Pereira, Madalena Ribeiro, Filipa Marques, Raquel Travassos, Catarina Nunes, Anabela Baptista Paula, and Inês Francisco. 2021. "A New Orthodontic-Surgical Approach to Mandibular Retrognathia" Bioengineering 8, no. 11: 180. https://doi.org/10.3390/bioengineering8110180
APA StyleVale, F., Queiroga, J., Pereira, F., Ribeiro, M., Marques, F., Travassos, R., Nunes, C., Paula, A. B., & Francisco, I. (2021). A New Orthodontic-Surgical Approach to Mandibular Retrognathia. Bioengineering, 8(11), 180. https://doi.org/10.3390/bioengineering8110180