Spinal Deformities and Advancement in Corrective Orthoses
Abstract
1. Introduction
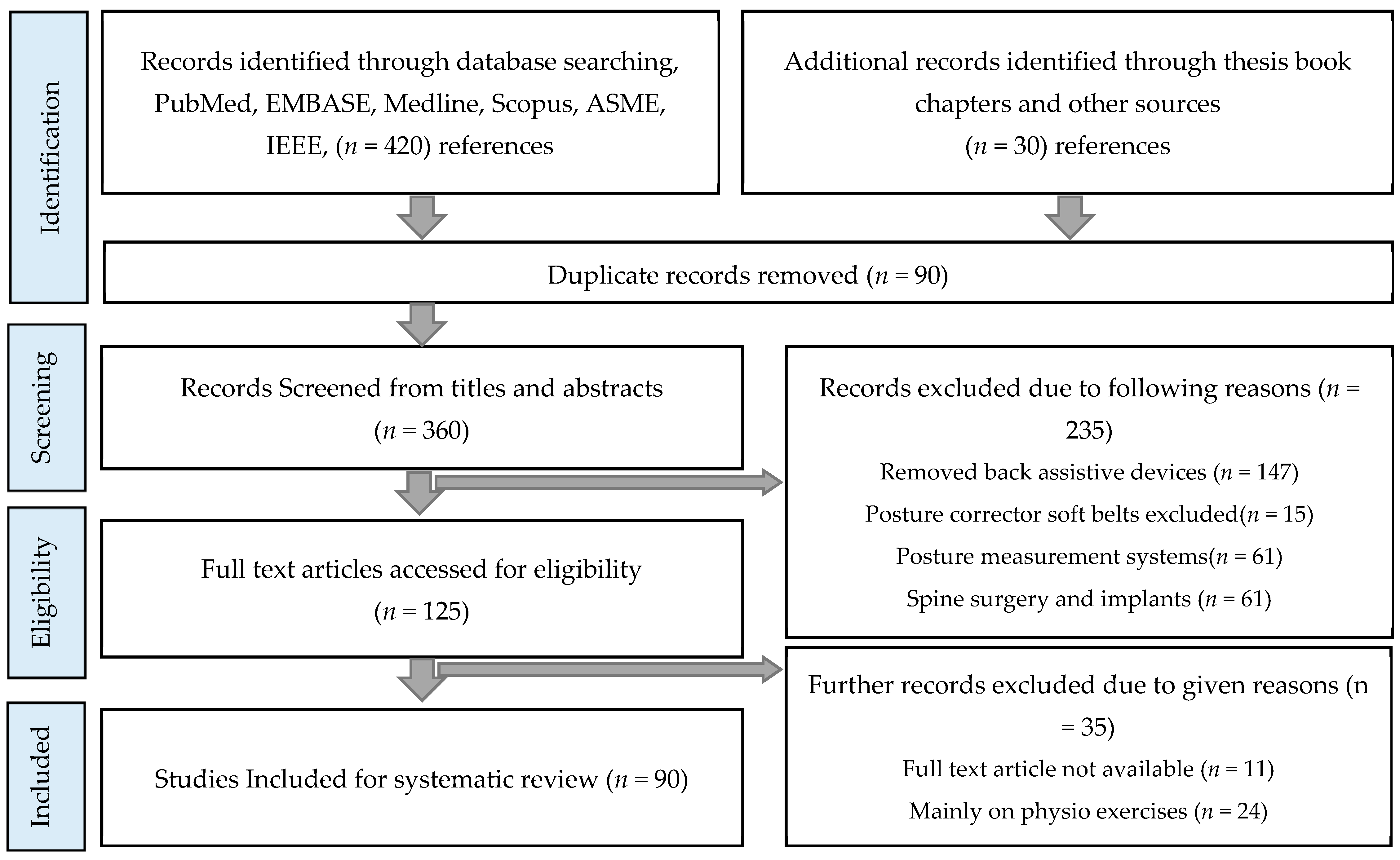
2. Materials and Methods
3. Corrective Orthoses (Braces)
4. Advancement in Spinal Rehabilitation Orthoses
4.1. Mobility and Actuation Technology
4.2. Sensory Designs and Parameter Characterization
4.3. CAD/CAM and Smart Materials
5. Conclusions
- Existing conventional braces and their key aspects, such as construction, materials, rigidity, and correction principle;
- Advancement in brace spinal orthoses technologies in terms of mobility and actuation;
- Use of sensors to track the brace compliance, interface pressure, force distribution, and torso parameter characterization;
- Developments in brace construction technologies, such as CAD/CAM, 3D printing and smart materials.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ogilvie, J. Adolescent idiopathic scoliosis and genetic testing. Curr. Opin. Pediatr. 2010, 22, 67–70. [Google Scholar] [CrossRef]
- Soultanis, K.C.; Payatakes, A.H.; Chouliaras, V.T.; Mandellos, G.C.; Pyrovolou, N.E.; Pliarchopoulou, F.M.; Soucacos, P.N. Rare causes of scoliosis and spine deformity: Experience and particular features. Scoliosis 2007. [Google Scholar] [CrossRef]
- Weinstein, S.L.; Dolan, L.A.; Wright, J.G.; Dobbs, M.B. Effects of bracing in adolescents with idiopathic scoliosis. N. Engl. J. Med. 2013. [Google Scholar] [CrossRef] [PubMed]
- Niu, X.; Yang, C.; Tian, B.; Li, X.; Zheng, S.; Cong, D.; Han, J.; Agrawal, S.K. Investigation of robotic braces of patients with idiopathic scoliosis (IS)—Review of the literature and description of a novel brace. J. Mech. Med. Biol. 2018. [Google Scholar] [CrossRef]
- McAviney, J.; Mee, J.; Fazalbhoy, A.; Du Plessis, J.; Brown, B.T. A systematic literature review of spinal brace/orthosis treatment for adults with scoliosis between 1967 and 2018: Clinical outcomes and harms data. BMC Musculoskelet. Disord. 2020, 21, 87. [Google Scholar] [CrossRef]
- Zaina, F.; De Mauroy, J.C.; Grivas, T.; Hresko, M.T.; Kotwizki, T.; Maruyama, T.; Price, N.; Rigo, M.; Stikeleather, L.; Wynne, J.; et al. Bracing for scoliosis in 2014: State of the art. Eur. J. Phys. Rehabil. Med. 2014, 51, 93–110. [Google Scholar]
- Karavidas, N. Bracing In The Treatment Of Adolescent Idiopathic Scoliosis: Evidence To Date. Adolesc. Health. Med. Ther. 2019. [Google Scholar] [CrossRef]
- Zhang, Y.; Li, X. Treatment of bracing for adolescent idiopathic scoliosis patients: A meta-analysis. Eur. Spine J. 2019, 28, 2012–2019. [Google Scholar] [CrossRef] [PubMed]
- Kaelin, A.J. Adolescent idiopathic scoliosis: Indications for bracing and conservative treatments. Ann. Transl. Med. 2020. [Google Scholar] [CrossRef]
- Kuroki, H. Brace treatment for adolescent idiopathic scoliosis. J. Clin. Med. 2018, 7, 136. [Google Scholar] [CrossRef]
- Donzelli, S.; Zaina, F.; Martinez, G.; Di Felice, F.; Negrini, A.; Negrini, S. Adolescents with idiopathic scoliosis and their parents have a positive attitude towards the Thermobrace monitor: Results from a survey. Scoliosis Spinal Disord. 2017. [Google Scholar] [CrossRef] [PubMed]
- Chan, A.; Lou, E.; Hill, D. Review of current technologies and methods supplementing brace treatment in adolescent idiopathic scoliosis. J. Child. Orthop. 2013. [Google Scholar] [CrossRef] [PubMed]
- Grivas, T.B.; de Mauroy, J.C.; Wood, G.; Rigo, M.; Hresko, M.T.; Kotwicki, T.; Negrini, S. Brace classification study group (BCSG): Part one-definitions and atlas (Retraction of Vol 11, art no 43, 2016). Scoliosis Spinal Disord. 2016. [Google Scholar] [CrossRef] [PubMed]
- Lonstein, J.E.; Winter, R.B. The Milwaukee brace for the treatment of adolescent idiopathic scoliosis. A review of one thousand and twenty patients. J. Bone Joint Surg. Am. 1994. [Google Scholar] [CrossRef] [PubMed]
- Wiemann, J.M.; Shah, S.A.; Price, C.T. Nighttime bracing versus observation for early adolescent idiopathic scoliosis. J. Pediatr. Orthop. 2014. [Google Scholar] [CrossRef] [PubMed]
- Rigo, M.; Weiss, H.R. The Chêneau concept of bracing–biomechanical aspects. Stud. Health Technol. Inform. 2008, 135, 303–319. [Google Scholar]
- Park, J.H.; Stegall, P.R.; Roye, D.P.; Agrawal, S.K. Robotic Spine Exoskeleton (RoSE): Characterizing the 3-d stiffness of the human torso in the treatment of spine deformity. IEEE Trans. Neural Syst. Rehabil. Eng. 2018. [Google Scholar] [CrossRef]
- Maruyama, T.; Takesita, K.; Kitagawa, T.; Nakao, Y. Milwaukee brace. Physiother. Theory Pract. 2011. [Google Scholar] [CrossRef]
- Noonan, K.J.; Weinstein, S.L.; Jacobson, W.C.; Dolan, L.A. Use of the Milwaukee brace for progressive idiopathic scoliosis. J. Bone Joint Surg. Am. 1996. [Google Scholar] [CrossRef]
- Blount, W.P.; Schmidt, A.C.; Keever, E.D.; Leonard, E.T. The Milwaukee brace in the operative treatment of scoliosis. JBJS 1958, 40, 511–525. [Google Scholar] [CrossRef]
- ORTHOGEA SRL Milwaukee Brace. Available online: https://www.orthogea.com/product-detail/corsetto-milwaukee/ (accessed on 19 November 2020).
- Danielsson, A.J.; Hasserius, R.; Ohlin, A.; Nachemson, A.L. A prospective study of brace treatment versus observation alone in adolescent idiopathic scoliosis: A follow-up mean of 16 years after maturity. Spine (Phila. Pa. 1976). 2007. [Google Scholar] [CrossRef] [PubMed]
- Emans, J.B.; Kaelin, A.; Bancel, P.; Hall, J.E.; Miller, M.E. The boston bracing system for idiopathic scoliosis: Follow-up results in 295 patients. Spine (Phila. Pa. 1976). 1986. [Google Scholar] [CrossRef] [PubMed]
- Heary, R.F.; Kumar, S.; Bono, C.M. Bracing for scoliosis. Neurosurgery 2008. [Google Scholar] [CrossRef] [PubMed]
- Corrective orthosis boston brace. Available online: https://commons.wikimedia.org/wiki/File:Bostonbrace.jpg (accessed on 10 July 2020).
- Negrini, S.; Marchini, G. Efficacy of the symmetric, patient-oriented, rigid, three-dimensional, active (SPoRT) concept of bracing for scoliosis: A prospective study of the Sforzesco versus Lyon brace. Eura. Medicophys. 2007, 43, 171–181. [Google Scholar] [PubMed]
- Zaina, F.; Negrini, S.; Fusco, C.; Atanasio, S. How to improve aesthetics in patients with Adolescent Idiopathic Scoliosis (AIS): A SPoRT brace treatment according to SOSORT management criteria. Scoliosis 2009, 4, 18. [Google Scholar] [CrossRef]
- ORTHOGEA SRL Lyon Brace. Available online: https://www.orthogea.com/product-detail/corsetto-lionese/ (accessed on 18 November 2020).
- Hopf, C.; Heine, J. Long-term results of the conservative treatment of scoliosis using the Cheneau brace. Z. Orthop. Ihre Grenzgeb. 1985, 123, 312–322. [Google Scholar] [CrossRef]
- Zaborowska-Sapeta, K.; Kowalski, I.M.; Kotwicki, T.; Protasiewicz-Fałdowska, H.; Kiebzak, W. Effectiveness of Chêneau brace treatment for idiopathic scoliosis: Prospective study in 79 patients followed to skeletal maturity. Scoliosis 2011. [Google Scholar] [CrossRef]
- De Giorgi, S.; Piazzolla, A.; Tafuri, S.; Borracci, C.; Martucci, A.; De Giorgi, G. Chêneau brace for adolescent idiopathic scoliosis: Long-term results. Can it prevent surgery? Eur. Spine J. 2013. [Google Scholar] [CrossRef]
- Wikimedia Commons Cheneau Brace Image. Available online: https://commons.wikimedia.org/wiki/File:Crass_Cheneau_brace.jpg (accessed on 10 July 2020).
- Lee, C.S.; Hwang, C.J.; Kim, D.J.; Kim, J.H.; Kim, Y.T.; Lee, M.Y.; Yoon, S.J.; Lee, D.H. Effectiveness of the Charleston night-time bending brace in the treatment of adolescent idiopathic scoliosis. J. Pediatr. Orthop. 2012. [Google Scholar] [CrossRef]
- Coillard, C.; Leroux, M.A.; Zabjek, K.F.; Rivard, C.H. SpineCor—A non-rigid brace for the treatment of idiopathic scoliosis: Post-treatment results. Eur. Spine J. 2003. [Google Scholar] [CrossRef]
- Gutman, G.; Benoit, M.; Joncas, J.; Beauséjour, M.; Barchi, S.; Labelle, H.; Parent, S.; Mac-Thiong, J.M. The effectiveness of the SpineCor brace for the conservative treatment of adolescent idiopathic scoliosis. Comparison with the Boston brace. Spine J. 2016. [Google Scholar] [CrossRef]
- Weiss, H.R.; Werkmann, M. Retraction: Soft braces in the treatment of Adolescent Idiopathic Scoliosis (AIS)—Review of the literature and description of a new approach. Scoliosis 2013, 8, 7. [Google Scholar] [CrossRef] [PubMed]
- Van Loon, P.J.M.; Kühbauch, B.A.G.; Thunnissen, E. Forced lordosis on the thoracolumbar junction can correct coronal plane deformity in adolescents with double major curve pattern idiopathic scoliosis. Spine (Phila. Pa. 1976). 2008, 33, 797–801. [Google Scholar] [CrossRef]
- Veldhuizen, A.G.; Cheung, J.; Bulthuis, G.J.; Nijenbanning, G. A new orthotic device in the non-operative treatment of idiopathic scoliosis. Med. Eng. Phys. 2002. [Google Scholar] [CrossRef]
- Wong, M.S.; Cheng, J.C.Y.; Lam, T.P.; Ng, B.K.W.; Sin, S.W.; Lee-Shum, S.L.F.; Chow, D.H.K.; Tam, S.Y.P. The effect of rigid versus flexible spinal orthosis on the clinical efficacy and acceptance of the patients with adolescent idiopathic scoliosis. Spine (Phila. Pa. 1976). 2008. [Google Scholar] [CrossRef] [PubMed]
- Weiss, H.R. SpineCor vs. natural history - Explanation of the results obtained using a simple biomechanical model. Stud. Health Technol. Inform. 2008. [Google Scholar] [CrossRef]
- Bassett, G.S.; Bunnell, W.P.; MacEwen, G.D. Treatment of idiopathic scoliosis with the Wilmington brace. Results in patients with a twenty to thirty-nine-degree curve. J. Bone Joint Surg. Am. 1986, 68, 602–605. [Google Scholar] [CrossRef]
- Périé, D.; Aubin, C.E.; Petit, Y.; Beauséjour, M.; Dansereau, J.; Labelle, H. Boston brace correction in idiopathic scoliosis: A biomechanical study. Spine (Phila. Pa. 1976). 2003. [Google Scholar] [CrossRef]
- Rivett, L.A.; Stewart, A.; Potterton, J. The effect of compliance to a Rigo System Cheneau brace and a specific exercise programme on idiopathic scoliosis curvature: A comparative study: SOSORT 2014 award winner. Scoliosis 2014. [Google Scholar] [CrossRef]
- De Mauroy, J.C.; Lecante, C.; Barral, F.; Daureu, D.; Gualerzi, S.; Gagliano, R. The Lyon brace. Disabil. Rehabil. Assist. Technol. 2008. [Google Scholar] [CrossRef]
- de Mauroy, J.C.; Journe, A.; Gagaliano, F.; Lecante, C.; Barral, F.; Pourret, S. The new Lyon ARTbrace versus the historical Lyon brace: A prospective case series of 148 consecutive scoliosis with short time results after 1 year compared with a historical retrospective case series of 100 consecutive scoliosis; SOSORT award 2015 winner. Scoliosis 2015. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Aulisa, A.; Guzzanti, V.; Perisano, C.; Falciglia, F.; Maggi, G.; Aulisa, L. Treatment of lumbar curves in adolescent females affected by idiopathic scoliosis with a progressive action short brace (PASB): Assessment of results according to the SRS committee on bracing and nonoperative management standardization criteria. Scoliosis 2012. [Google Scholar] [CrossRef]
- Gepstein, R.; Leitner, Y.; Zohar, E.; Angel, I.; Shabat, S.; Pekarsky, I.; Friesem, T.; Folman, Y.; Katz, A.; Fredman, B. Effectiveness of the Charleston bending brace in the treatment of single-curve idiopathic scoliosis. J. Pediatr. Orthop. 2002. [Google Scholar] [CrossRef]
- Grivas, T.B.; Bountis, A.; Vrasami, I.; Bardakos, N.V. Brace technology thematic series: The dynamic derotation brace. Scoliosis 2010. [Google Scholar] [CrossRef] [PubMed]
- Spoonamore, M.J.; Dolan, L.A.; Weinstein, S.L. Use of the Rosenberger brace in the treatment of progressive adolescent idiopathic scoliosis. Spine (Phila. Pa. 1976). 2004, 29, 1458–1464. [Google Scholar] [CrossRef]
- Negrini, S.; Marchini, G.; Tessadri, F. Brace technology thematic series—The Sforzesco and Sibilla braces, and the SPoRT (Symmetric, Patient oriented, Rigid, Three-dimensional, active) concept. Scoliosis 2011. [Google Scholar] [CrossRef]
- Colbert, A.P.; Craig, C. Scoliosis management in Duchenne muscular dystrophy: Prospective study of modified Jewett hyperextension brace. Arch. Phys. Med. Rehabil. 1987, 68, 302–304. [Google Scholar]
- Wang, S.V.; Zing, S. Bracing Effects of the Flexpine in Scoliosis Patients. Am. Sci. Res. J. Eng. Technol. Sci. 2017, 34, 261–268. [Google Scholar]
- Coillard, C.; Circo, A.; Rivard, C.H. A new concept for the non-invasive treatment of Adolescent Idiopathic Scoliosis: The Corrective Movement© principle integrated in the SpineCor system. Disabil. Rehabil. Assist. Technol. 2008. [Google Scholar] [CrossRef]
- Morningstar, M. Outcome observations in patients using a scoliosis activity suit: A retrospective chart review after one-year follow-up. J Scoliosis Rehabil 2013, 2013, 1–10. [Google Scholar]
- Richards, B.S.; Bernstein, R.M.; D’Amato, C.R.; Thompson, G.H. Standardization of criteria for adolescent idiopathic scoliosis brace studies: SRS Committee on Bracing and Nonoperative Management. Spine (Phila. Pa. 1976). 2005. [Google Scholar] [CrossRef] [PubMed]
- Negrini, S.; Donzelli, S.; Aulisa, A.G.; Czaprowski, D.; Schreiber, S.; de Mauroy, J.C.; Diers, H.; Grivas, T.B.; Knott, P.; Kotwicki, T. 2016 SOSORT guidelines: Orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis Spinal Disord. 2018, 13, 3. [Google Scholar] [CrossRef] [PubMed]
- Exodynamics ExMS-1. Available online: https://www.exodynamicsmedical.com/ (accessed on 5 May 2020).
- Igor, G.; Ryu, J.H.; Nedelchev, S. Twisted String Actuation Systems: Applications, Modelling, and Control; Elsevier Science: Amsterdam, The Netherlands, 2021; ISBN 9780128141953. [Google Scholar]
- Gaponov, I.; Popov, D.; Lee, S.J.; Ryu, J.H. Auxilio: A portable cable-driven exosuit for upper extremity assistance. Int. J. Control. Autom. Syst. 2017. [Google Scholar] [CrossRef]
- Seong, H.S.; Kim, D.H.; Gaponov, I.; Ryu, J.H. Development of a Twisted String Actuator-based Exoskeleton for Hip Joint Assistance in Lifting Tasks. In Proceedings of the IEEE International Conference on Robotics and Automation, Paris, France, 15 September 2020. [Google Scholar]
- Medical, G. Green Sun Medical Brace. Available online: http://www.greensunmedical.com/ (accessed on 8 December 2020).
- Myontec No Title. Available online: https://www.myontec.com/ (accessed on 18 August 2020).
- Redaelli, D.F.; Colombo, G.; Fraschini, P.; Biffi, E.; Reni, G. Current and future manufacturing of chest orthoses, considering the case of osteogenesis imperfecta. In Proceedings of the ASME Design Engineering Technical Conference, Quebec, QC, Canada, 26–29 August 2018. [Google Scholar]
- Donzelli, S.; Zaina, F.; Negrini, S. In defense of adolescents: They really do use braces for the hours prescribed, if good help is provided. Results from a prospective everyday clinic cohort using thermobrace. Scoliosis 2012. [Google Scholar] [CrossRef] [PubMed]
- Lou, E.; Hill, D.L.; Raso, J.V. A wireless sensor network system to determine biomechanics of spinal braces during daily living. Med. Biol. Eng. Comput. 2010. [Google Scholar] [CrossRef]
- Lou, E.; Venkateswaran, S.; Hill, D.L.; Raso, J.V.; Donauer, A. An intelligent active brace system for the treatment of scoliosis. IEEE Trans. Instrum. Meas. 2004. [Google Scholar] [CrossRef]
- Lou, E.; Benfield, D.; Raso, J.; Hill, D.; Durdle, N. Intelligent brace system for the treatment of scoliosis. Stud. Health Technol. Inform. 2002. [Google Scholar] [CrossRef]
- Chalmers, E.; Lou, E.; Hill, D.; Zhao, V.H.; Wong, M.S. Development of a pressure control system for brace treatment of scoliosis. IEEE Trans. Neural Syst. Rehabil. Eng. 2012. [Google Scholar] [CrossRef]
- Murray, R.C.; Ophaswongse, C.; Park, J.H.; Agrawal, S.K. Characterizing Torso Stiffness in Female Adolescents with and without Scoliosis. IEEE Robot. Autom. Lett. 2020. [Google Scholar] [CrossRef]
- Santamaria, V.; Luna, T.; Khan, M.; Agrawal, S. The robotic Trunk-Support-Trainer (TruST) to measure and increase postural workspace during sitting in people with spinal cord injury. Spinal Cord Ser. Cases 2020. [Google Scholar] [CrossRef]
- Khan, M.I.; Santamaria, V.; Kang, J.; Bradley, B.M.; Dutkowsky, J.P.; Gordon, A.M.; Agrawal, S.K. Enhancing Seated Stability Using Trunk Support Trainer (TruST). IEEE Robot. Autom. Lett. 2017. [Google Scholar] [CrossRef]
- Santamaria, V.; Khan, M.; Luna, T.; Kang, J.; Dutkowsky, J.; Gordon, A.; Agrawal, S. Promoting Functional and Independent Sitting in Children with Cerebral Palsy Using the Robotic Trunk Support Trainer. IEEE Trans. Neural Syst. Rehabil. Eng. 2020. [Google Scholar] [CrossRef]
- Ophaswongse, C.; Murray, R.C.; Santamaria, V.; Wang, Q.; Agrawal, S.K. Human Evaluation of Wheelchair Robot for Active Postural Support (WRAPS). Robotica 2019. [Google Scholar] [CrossRef]
- Ophaswongse, C.; Agrawal, S.K. Optimal design of a novel 3-DOF orientational parallel mechanism for pelvic assistance on a wheelchair: An approach based on kinematic geometry and screw theory. IEEE Robot. Autom. Lett. 2020. [Google Scholar] [CrossRef]
- Bratic, D.; Noel, A. Vertebral decompression device. U.S. Patent 15/567,651, 29 March 2018. [Google Scholar]
- Grazioso, S.; Selvaggio, M.; Di Gironimo, G. Design and development of a novel body scanning system for healthcare applications. Int. J. Interact. Des. Manuf. 2018. [Google Scholar] [CrossRef]
- Grazioso, S.; Selvaggio, M.; Caporaso, T.; Di Gironimo, G. A Digital Photogrammetric Method to Enhance the Fabrication of Custom-Made Spinal Orthoses. J. Prosthetics Orthot. 2019. [Google Scholar] [CrossRef]
- Guy, A.; Labelle, H.; Barchi, S.; Audet-Duchesne, E.; Cobetto, N.; Parent, S.; Raison, M.; Aubin, C.-É. Braces Designed Using CAD/CAM Combined or Not with Finite Element Modeling Lead to Effective Treatment and Quality of Life after Two Years. Spine (Phila. Pa. 1976). 2020. [Google Scholar] [CrossRef] [PubMed]
- Weiss, H.R.; Seibel, S.; Moramarco, M.; Kleban, A. Bracing scoliosis: The evolution to CAD/CAM for improved in-brace corrections. Hard Tissue 2013, 2, 43. [Google Scholar] [CrossRef][Green Version]
- Mauroy, J.C.D.; Lecante, C.; Barral, F.; Pourret, S. Prospective study and new concepts based on scoliosis detorsion of the first 225 early in-brace radiological results with the new Lyon brace: ARTbrace. Scoliosis 2014. [Google Scholar] [CrossRef][Green Version]
- Cobetto, N.; Aubin, C.E.; Parent, S.; Clin, J.; Barchi, S.; Turgeon, I.; Labelle, H. Effectiveness of braces designed using computer-aided design and manufacturing (CAD/CAM) and finite element simulation compared to CAD/CAM only for the conservative treatment of adolescent idiopathic scoliosis: A prospective randomized controlled trial. Eur. Spine J. 2016. [Google Scholar] [CrossRef]
- Cobetto, N.; Aubin, C.É.; Parent, S.; Barchi, S.; Turgeon, I.; Labelle, H. 3D correction of AIS in braces designed using CAD/CAM and FEM: A randomized controlled trial. Scoliosis Spinal Disord. 2017. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Tanaka, H. Feasibility study applying a parametric model as the design generator for 3D–printed orthosis for fracture immobilization. 3D Print. Med. 2018. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Tanaka, H. Rapid customization system for 3D-printed splint using programmable modeling technique—A practical approach. 3D Print. Med. 2018. [Google Scholar] [CrossRef] [PubMed]
- Patterson, A.E.; Pereira, T.R.; Allison, J.T.; Messimer, S.L. IZOD impact properties of full-density fused deposition modeling polymer materials with respect to raster angle and print orientation. Proc. Inst. Mech. Eng. Part C J. Mech. Eng. Sci. 2019. [Google Scholar] [CrossRef]
- Lanzotti, A.; Martorelli, M.; Maietta, S.; Gerbino, S.; Penta, F.; Gloria, A. A comparison between mechanical properties of specimens 3D printed with virgin and recycled PLA. In Proceedings of the Procedia CIRP, Napels, Italy, 18–20 July 2019. [Google Scholar]
- Chan, W.Y.; Yip, J.; Yick, K.L.; Ng, S.P.; Lu, L.; Cheung, K.M.C.; Kwan, K.Y.H.; Cheung, J.P.Y.; Yeung, K.W.K.; Tse, C.Y. Mechanical and Clinical Evaluation of a Shape Memory Alloy and Conventional Struts in a Flexible Scoliotic Brace. Ann. Biomed. Eng. 2018. [Google Scholar] [CrossRef] [PubMed]
- Narang, Y.S.; Vlassak, J.J.; Howe, R.D. Mechanically Versatile Soft Machines through Laminar Jamming. Adv. Funct. Mater. 2018. [Google Scholar] [CrossRef]
- Wang, T.; Zhang, J.; Li, Y.; Hong, J.; Wang, M.Y. Electrostatic Layer Jamming Variable Stiffness for Soft Robotics. IEEE/ASME Trans. 2019. [Google Scholar] [CrossRef]
- Choi, W.H.; Kim, S.; Lee, D.; Shin, D. Soft, Multi-DoF, Variable Stiffness Mechanism Using Layer Jamming for Wearable Robots. IEEE Robot. Autom. Lett. 2019. [Google Scholar] [CrossRef]


| Device/Origin | Rigidity | Construction | Principle of Correction/Remarks |
|---|---|---|---|
| Milwaukee brace, United States 1945 [14,18] | Rigid | Polyethylene, aluminum, and steel | Symmetrical design with a posterior opening. Previously used for post-operative immobilization of neuromuscular scoliosis. Not used anymore to treat scoliosis, but still used for Scheuermann’s kyphosis and high thoracic curves. |
| Wilmington brace, United States 1969 [41] | Rigid | Polyethylene, custom-made/handmade | Thoracic-lumbar-sacral orthosis (TLSO) with underarm symmetrical design and anterior opening. Initially designed to treat curves between 25° and 39° with apices at or inferior to T7. |
| Boston brace, United States 1972 [23,42] | Rigid | Polyethylene, prefabricated envelope/models | Symmetrical design with posterior opening. Developed for the lumbar curve, extended to treat thoracolumbar and thoracic curves. Reduced cost and fabrication time compared to Milwaukee. TLI (thoracolumbar lordotic intervention) by Loon et al. [37] to ensure forced lordosis at thoracolumbar spine. Applied when Cobb angle is over 25° |
| Chêneau and derivatives, France/Germany1960 [31,43] | Rigid | Polyethylene, custom-made/CAD-CAM, handmade | The principle of correction of Chêneau brace is a combination of sagittal balance, regional de-rotation, physiological profile, and three-point pressure bending system. A three-dimensional (3D) Rigo System Chêneau brace (RSCB) and Chêneau light brace were developed as an extension of the J Chêneau brace in 1990 and 2005, respectively. |
| Lyon brace, France 1947 [44,45] | Very rigid | Polymeta-crylate and radiolucent duralumin | The correction principle is the three-point pressure system with rotation angular breathing (RAB). Three regional, two-dimensional (2D) individual moldings. A 3D asymmetrical rigid torsion brace (ART), which is a Lyon brace derivative. Correction principle is global detorsion. Moldings: 3D helicoidal correction with coupled movements. Material: 4 m polycarbonate, rigid. The sagittal plane is fixed in a physiological posture to improve a flat back if necessary. In the middle, under the breast, the clamping of the two hemi-shells realizes the “tube mayonnaise” effect with passive axial lengthening and geometric detorsion. The polycarbonate–skin interface is a soft contact type with a mechanical detorsion of a cylinder. |
| PASB, Italy 1976 [46] | Rigid | Polyethylene, custom/handmade | Progressive action short brace (PASB) is a TLSO for the correction of thoraco-lumbar, thoraco-lumbar-sacral, and idiopathic lumber curves. |
| Charleston brace, United States 1979 [33,47] | Rigid | Polyethylene | Correction principle: Heuter–Volkmann principle TLSO, asymmetrical, anterior opening.Bending brace, side bending posture, single lumbar, thoracic, or thoracolumbar curves. Aggressive design for correction. |
| Providence brace, United States 1992 [6] | Rigid | Polyethylene, custom-made/CAD-CAM, handmade | Surpasses the Charleston night brace due to less aggressive design. Asymmetric anterior opening. TLSO type, and curve correction by de-rotational and lateral forces as opposed to side bending posture, as seen in the Charleston brace. Very successful in treating flexible, single lumbar and thoracolumbar curves; however, it can be quite effective with thoracic and double curves. |
| Dynamic Derotating Brace, Greece 1982 [48] | Rigid | Polypropylene and aluminum, custom made/CAD-CAM, handmade | Developed as a modification of the Boston brace in 1982, in Greece. It opens posteriorly, with a TLSO-type underarm brace with aluminum blades set to produce anti-rotating and de-rotating effects on the trunk and thorax of scoliosis patients.It is recommended for extremely high thoracic curves when the apex vertebra is T5 or above. |
| Rosenberger brace, United States 1983 [49] | Rigid | Polyethylene | Correction principle: three-point pressure system.Asymmetrical, anterior opening, TLSO, reduces the curves with a translator and de-rotational loads. The limitation is its retrospective design. |
| 3D Sibilla brace [50] | Low rigidity | − | Proposed for mild curve progression for a Cobb angle <30° that cannot be treated by SEAS * exercises. The brace is recommended to wear for 18 to 20 h daily, up to Risser stage 3. |
| Sforzesco brace, Italy [50] | Very rigid | Copolyester radiolucent duralumin, custom-made/CAD-CAM, handmade | 3D active, symmetrical, incorporating the features of Milwaukee, Lyon, Sibilla, Risser cast, and Chêneau braces. Used for severe adolescent scoliosis (Cobb 45°–50°) when surgery is not a possible option or patients do not want it to be operated on. It is also a full-time brace and is recommended to be worn over 18 h a day. |
| SpoRT Brace [26,50] | Rigid | Polycarbonate, aluminum | The SPoRT bracing (three-dimensional elongation pushing in a down–up direction) is different from the other corrective systems: symmetric design, three-point, traction, and postural and movement-based. |
| Jewett hyperextensionbrace, [51] | Rigid | Metallic, prefabricated | Used to treat hyperkyphosis. It cannot handle rotational deformities of scoliosis. Stable framework construction restricts lateral flexion and hyperextension of the vertebral column, and provides stabilization in the sagittal plane. |
| Flexpine brace, South Korea [52] | Semi-rigid | 3D-printed, elastic tissue, foldable plastic body | Lightweight, 4 mm-thick brace. 3D-printed brace made from foldable plastic. Allows mobility and enhances exercise’s potential to treat scoliosis. |
| SpineCor dynamic brace, Canada 1993 [34,53] | Elastic | Elastic tissue, Prefabricated envelope/models | Dynamic bracing solution for idiopathic scoliosis and round back (hyperkyphosis) deformity. SpineCor treatment is suitable for children from the age of five with idiopathic scoliosis and certain syndrome-related scoliosis curves from 20°–50°. (Treatment is recommended for as low as 15° for children with a higher risk of progression.) |
| SpinealiteTM brace [36,37] | Elastic | Elastic tissue, prefabricated envelope/models | SpinealiteTM is used to treat lumbar lordosis. It uses a single band for the back compression force, which is quite helpful for the correction of flexion in the sagittal plane. |
| Triac brace, Netherlands [38,39] | Low rigidity | Soft plastic and metallic connections, prefabricated envelope/models | The flexible Triac brace was designed to improve cosmetic appearance and comfort. It was developed for primary curve correction in idiopathic scoliosis (IS). Planes of action are frontal and sagittal. Not recommended for the treatment of thoracic or double curves. |
| ScoliSmart, USA [54] | Soft suit | Prefabricated/fabric, elastic | ScoliSmart utilizes the energy of a human’s natural movement to generate new muscle memory. This new muscle memory decreases and stabilizes asymmetrical muscle firing, thus reducing the risk of curve progression and helping the spine unravel naturally, so it is never forced. |
| Device | Actuation | Structure | Application | Remarks |
|---|---|---|---|---|
| Greensun medical brace, United States [61] | Passive (elastic and metallic connections, prefabricated and adjusted for each patient) | Semi-rigid | Treat idiopathic scoliosis | It is a low-rigidity brace, consisting of semi-rigid segments encircling the torso, which are joined by the elastic elements. These elastic elements give required immobilization by engendering stabilizing forces while allowing the relative motion of semi-rigid segments. Real-time monitoring of the correction progress to adjust the brace. |
| Inflatable intelligent active brace [66] | Active (pneumatic bladder) | Rigid | Treat idiopathic Scoliosis | Use the air bladder to control interface pressure by inflating the bladder. The control system is comprised of a microcontroller, a force feedback component, and a force transducer. |
| Japet (Atlas) [75] | Active (four electric actuators) | Rigid | Pain relief, recover mobility | Extends the spine to release the pain. The adaptable system maintains complete freedom of movement without restricting muscular activity. |
| ExMs-1 by Exo-dynamics [57] | Active (four electric actuators) | Rigid | Pain relief, assistance while bending | Extends the spine and offers automatic, customizable back support without sacrificing mobility. This device is not intended to diagnose, treat, cure, or prevent any disease. |
| RoSE dynamic brace [17,69] | Active (electric, series elastic actuators) | Rigid (parallel Stewart platforms) | Treat idiopathic scoliosis, torso stiffness characterization | Three-point bending (push, movement, and elongation are other actuation mechanisms) and plane of action (3D, frontal, frontal horizontal, sagittal, and brace map classification). |
| TruST [70,71,72] | Active (electric, servo motors) | Rigid (pulley cable system) | Trunk support trainer | TruST is a cable pulley system; it uses four motors mounted on a stationary platform to apply forces through an adjustable but rigid belt on the trunk. TruST assists patients who have lost postural stability of the torso. |
| WRAPS [73,74] | Active series electric actuators | Rigid | Torso postural Support | WRAPS is a parallel robotic device consisting of two rings over the chest and hips connected by 2RPS-2UPS architecture. WRAPS can modulate forces/displacements applied to the torso in four degrees of freedom. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ali, A.; Fontanari, V.; Fontana, M.; Schmölz, W. Spinal Deformities and Advancement in Corrective Orthoses. Bioengineering 2021, 8, 2. https://doi.org/10.3390/bioengineering8010002
Ali A, Fontanari V, Fontana M, Schmölz W. Spinal Deformities and Advancement in Corrective Orthoses. Bioengineering. 2021; 8(1):2. https://doi.org/10.3390/bioengineering8010002
Chicago/Turabian StyleAli, Athar, Vigilio Fontanari, Marco Fontana, and Werner Schmölz. 2021. "Spinal Deformities and Advancement in Corrective Orthoses" Bioengineering 8, no. 1: 2. https://doi.org/10.3390/bioengineering8010002
APA StyleAli, A., Fontanari, V., Fontana, M., & Schmölz, W. (2021). Spinal Deformities and Advancement in Corrective Orthoses. Bioengineering, 8(1), 2. https://doi.org/10.3390/bioengineering8010002








