Domain Heterogeneity in Radiofrequency Therapies for Pain Relief: A Computational Study with Coupled Models †
Abstract
1. Introduction
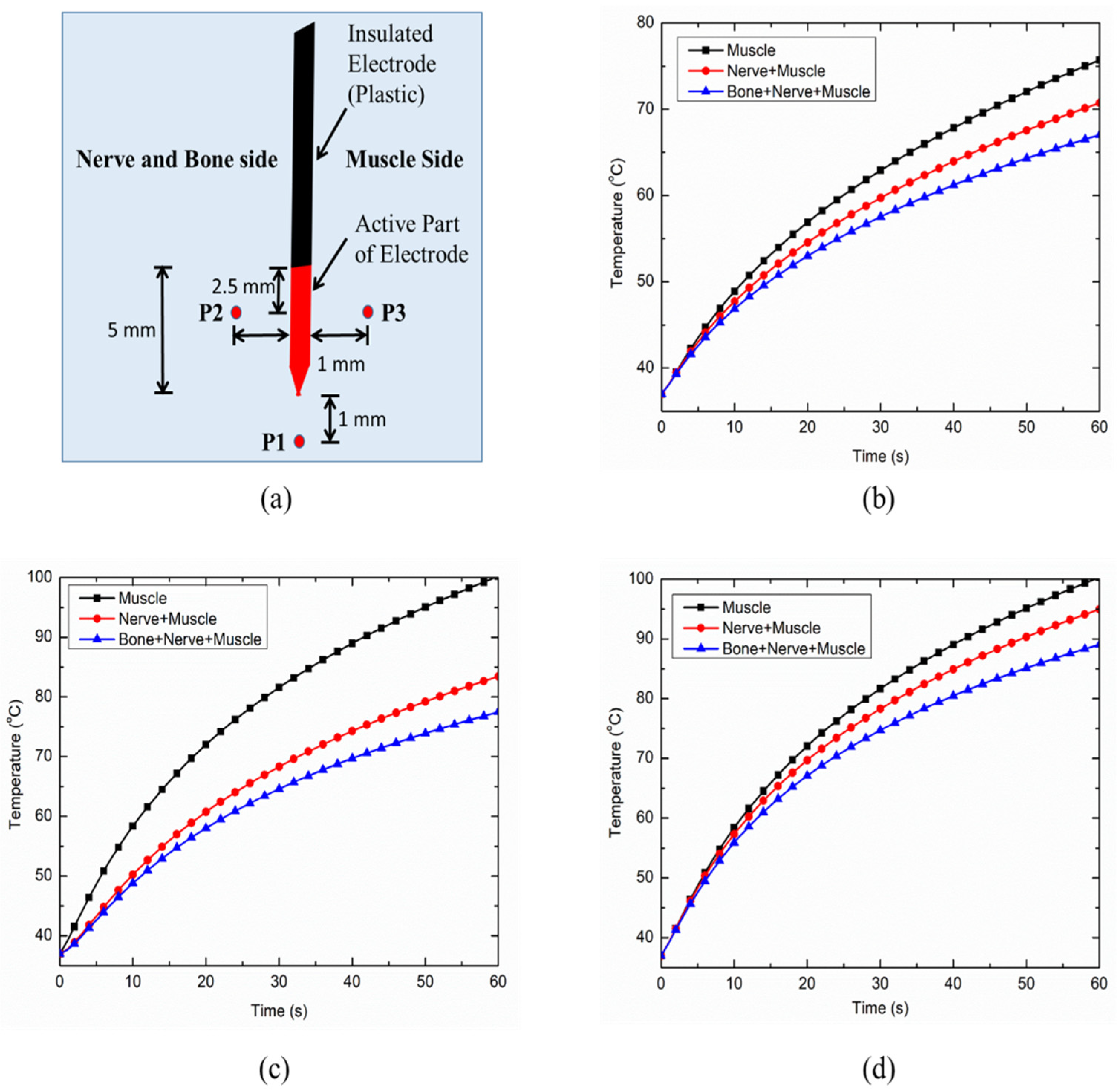
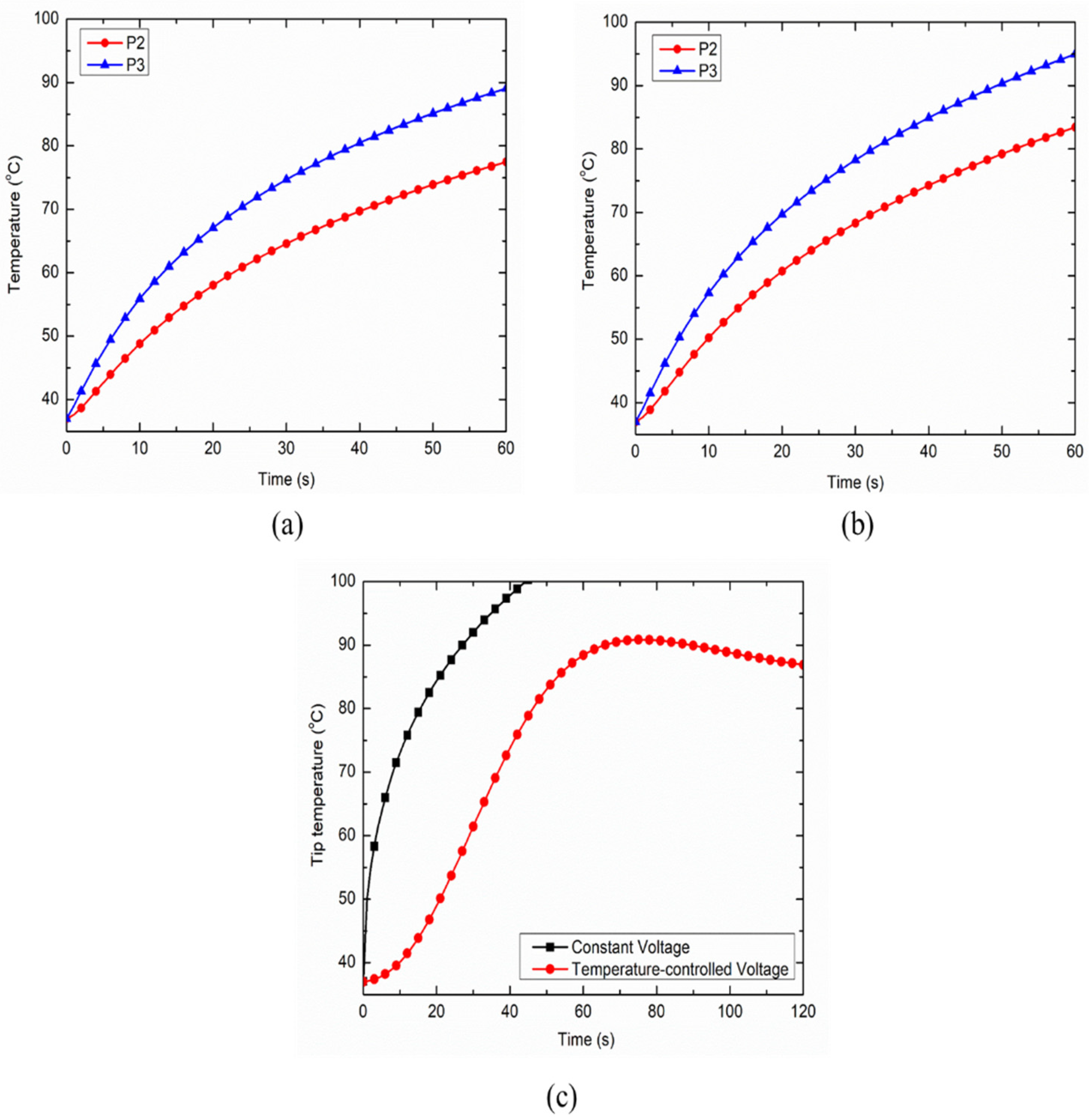
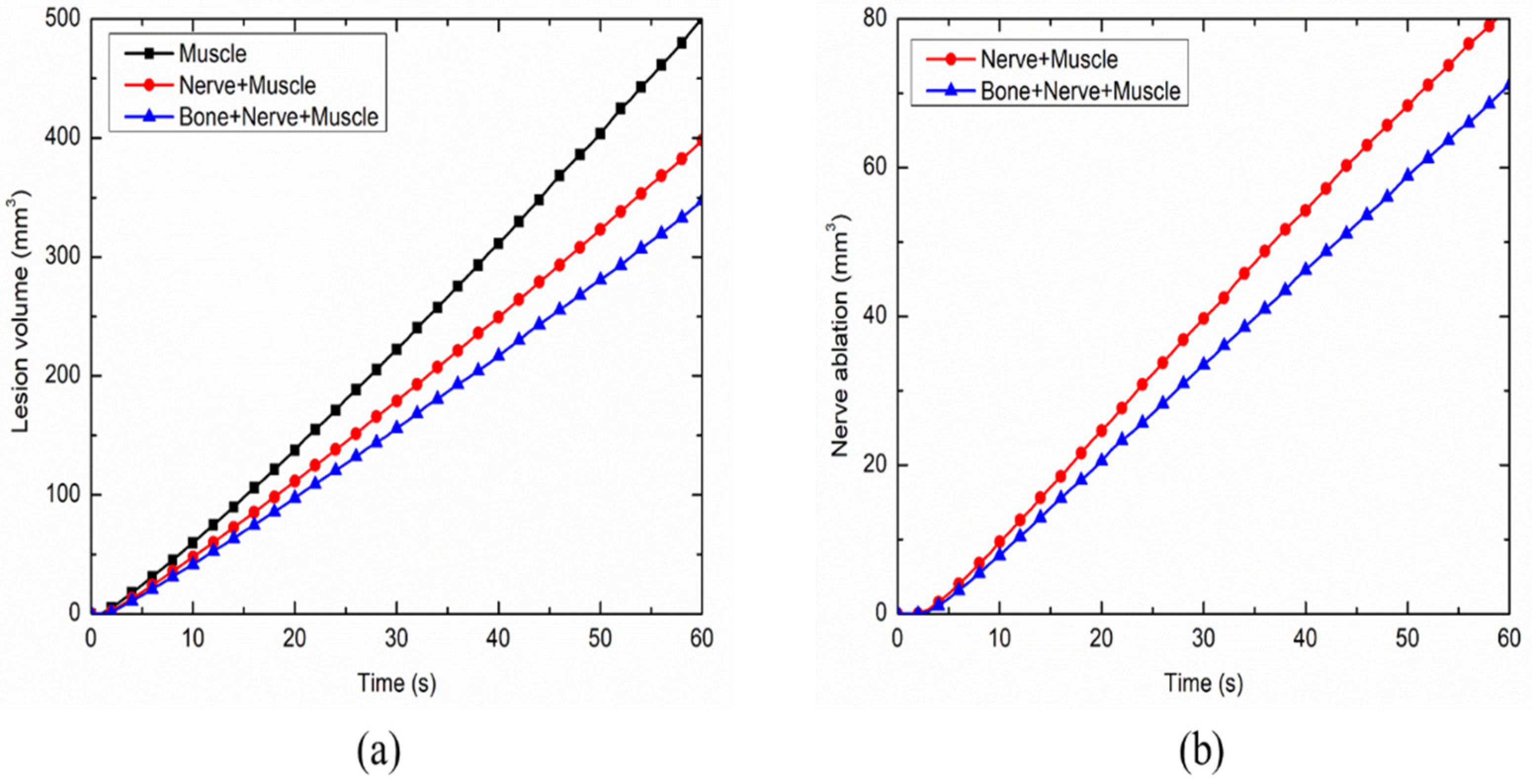
2. Materials and Methods
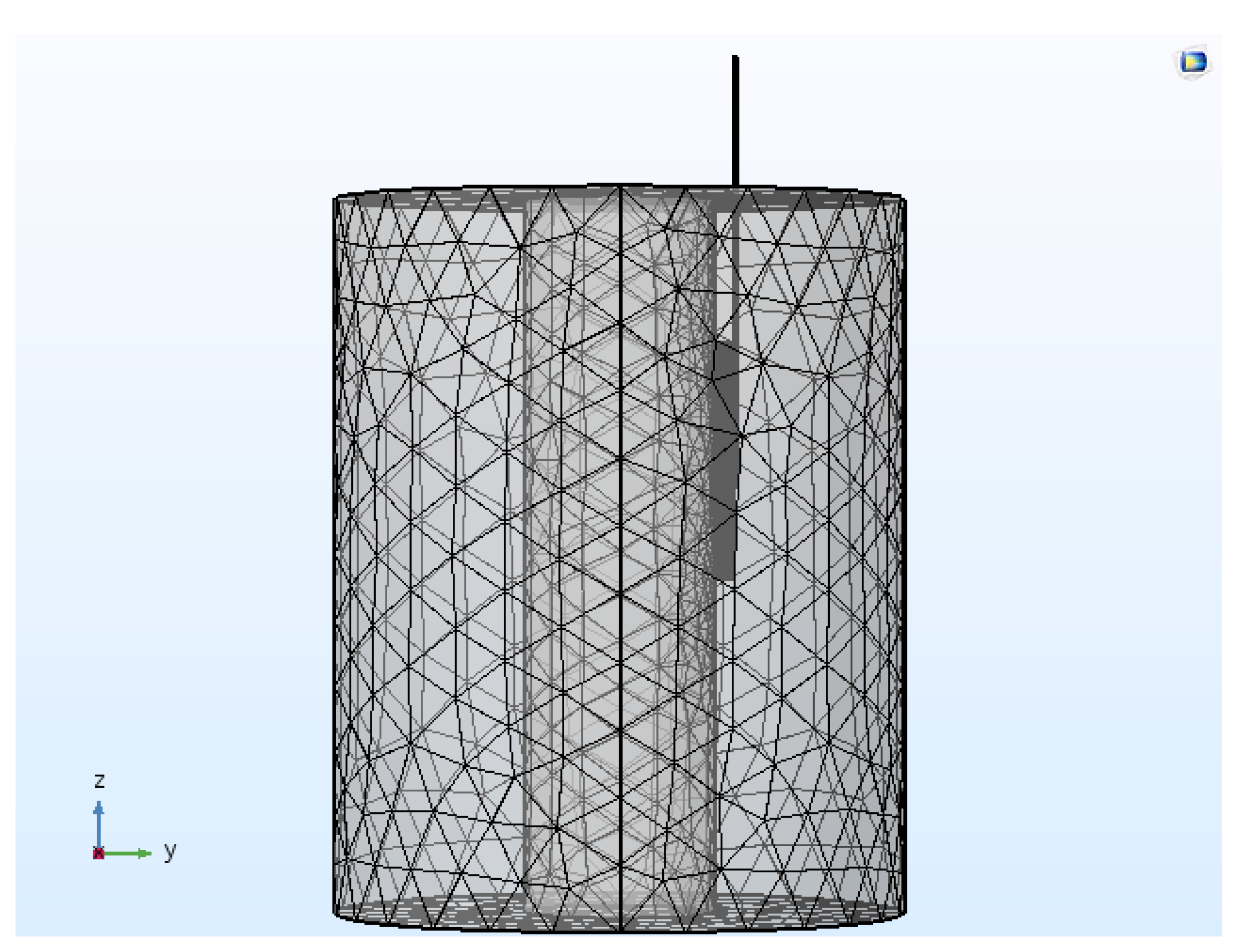
2.1. Computational Domain
2.2. Governing Equations for Coupled Thermo-Electric Model
2.3. Numerical Setup and Modeling Details
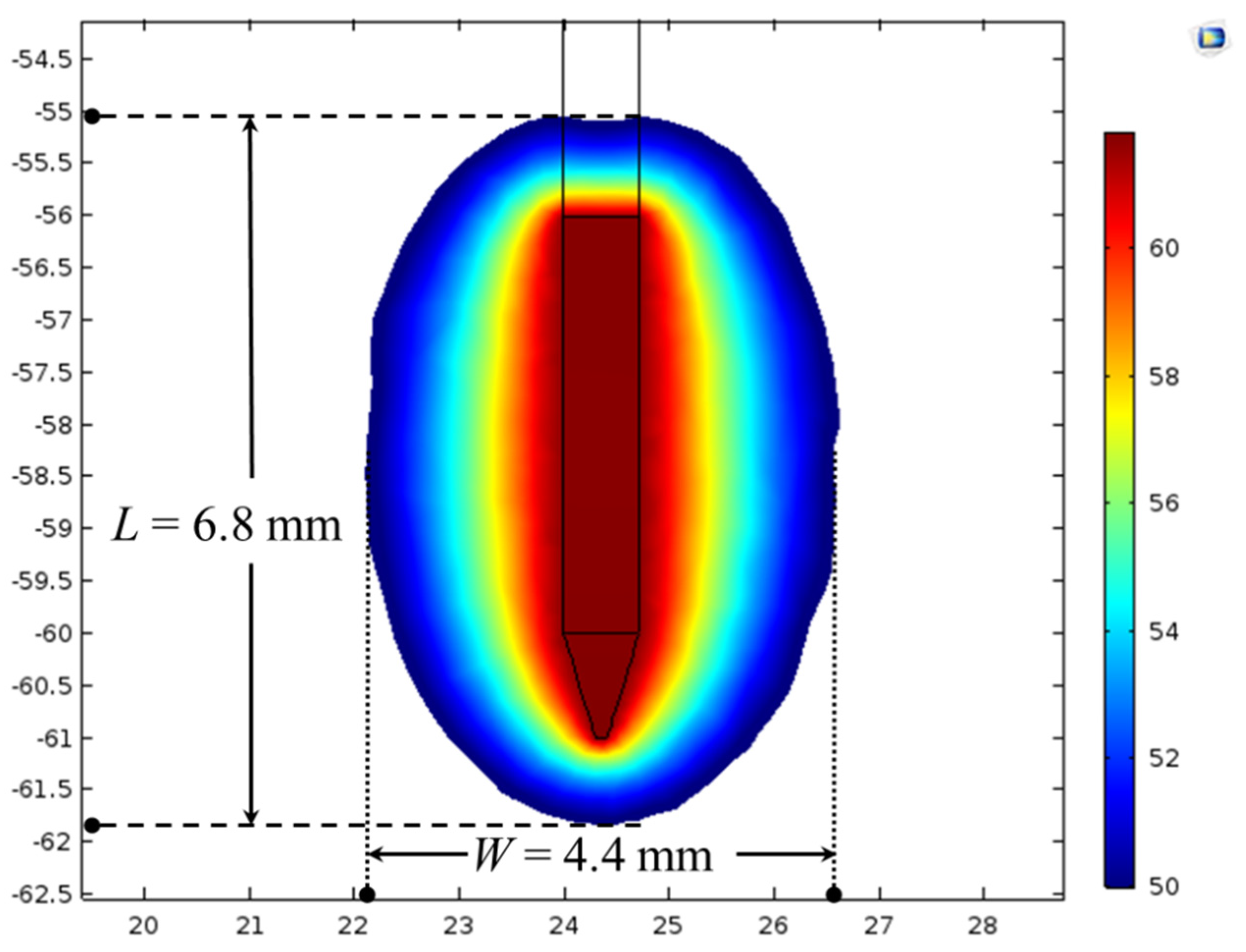
2.4. Model Validation
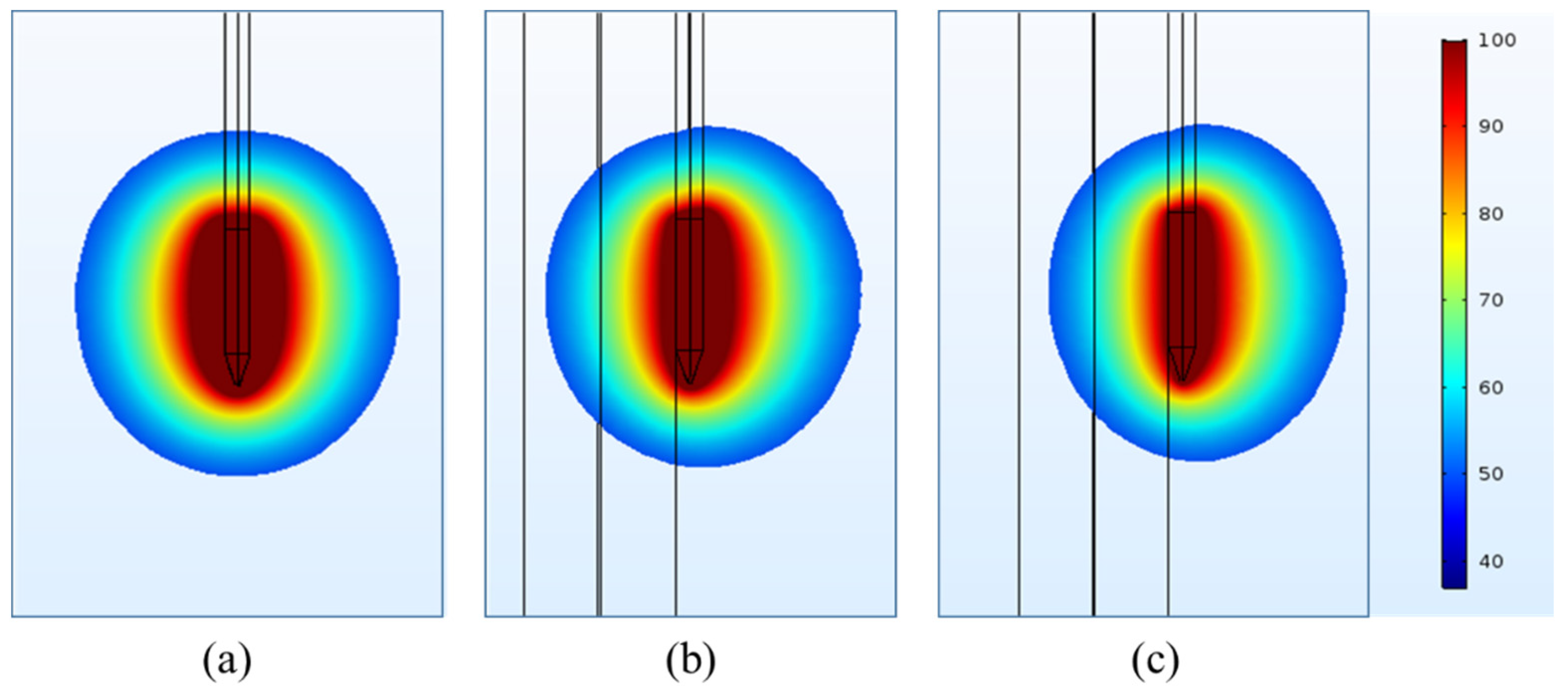
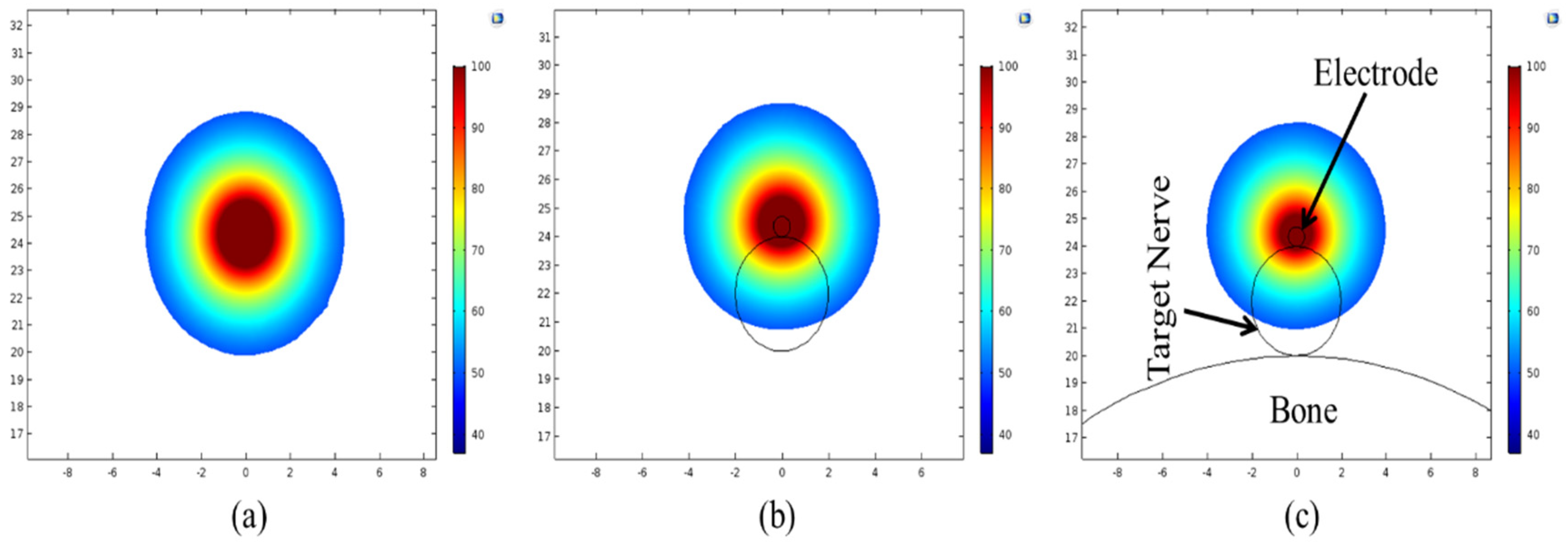
3. Results and Discussion
4. Clinical Applications, Future Outlook and Model Developments
4.1. Heterogeneous Surroundings and Clinical Trials
4.2. Multiscale Models for Biological Tissues
4.3. Coupling Frameworks and Pain Relief Models
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Deer, T.R.; Pope, J.E.; Lamer, T.J.; Provenzano, D. Deer’s Treatment of Pain: An Illustrated Guide for Practitioners; Springer: Berlin/Heidelberg, Germany, 2019. [Google Scholar]
- Altilio, T.; Otis-Green, S.; Hedlund, S.; Fineberg, I.C. Pain management and palliative care. In Handbook of Health Social Work; John Wiley Sons, Inc.: Hoboken, NJ, USA, 2019; pp. 535–568. [Google Scholar]
- Eccleston, C.; Morley, S.; Williams, A.d.C. Psychological approaches to chronic pain management: Evidence and challenges. Br. J. Anaesth. 2013, 111, 59–63. [Google Scholar] [CrossRef]
- Gilron, I.; Carr, D.B.; Desjardins, P.J.; Kehlet, H. Current methods and challenges for acute pain clinical trials. Pain Rep. 2019, 4, e647. [Google Scholar] [CrossRef]
- Hogan, M.-E.; Taddio, A.; Katz, J.; Shah, V.; Krahn, M. Incremental health care costs for chronic pain in Ontario, Canada: A population-based matched cohort study of adolescents and adults using administrative data. Pain 2016, 157, 1626–1633. [Google Scholar] [CrossRef] [PubMed]
- Loh, E.; Reid, J.N.; Alibrahim, F.; Welk, B. Retrospective cohort study of healthcare utilization and opioid use following radiofrequency ablation for chronic axial spine pain in Ontario, Canada. Reg. Anesth. Pain Med. 2019, 44, 398–405. [Google Scholar] [CrossRef]
- Henningfield, J.E.; Ashworth, J.B.; Gerlach, K.K.; Simone, B.; Schnoll, S.H. The nexus of opioids, pain, and addiction: Challenges and solutions. Prev. Med. 2019, 128, 105852. [Google Scholar] [CrossRef] [PubMed]
- Orhurhu, V.; Urits, I.; Grandhi, R.; Abd-Elsayed, A. Systematic Review of Radiofrequency Ablation for Management of Knee Pain. Curr. Pain Headache Rep. 2019, 23, 55. [Google Scholar] [CrossRef]
- Soloman, M.; Mekhail, M.N.; Mekhail, N. Radiofrequency treatment in chronic pain. Expert Rev. Neurother. 2010, 10, 469–474. [Google Scholar] [CrossRef]
- Abd-Elsayed, A.; Kreuger, L.; Wheeler, S.; Robillard, J.; Seeger, S.; Dulli, D. Radiofrequency ablation of pericranial nerves for treating headache conditions: A promising option for patients. Ochsner J. 2018, 18, 59–62. [Google Scholar] [PubMed]
- Bhatia, A.; Hoydonckx, Y.; Peng, P.; Cohen, S.P. Radiofrequency procedures to relieve chronic hip pain: An evidence-based narrative review. Reg. Anesth. Pain Med. 2018, 43, 72–83. [Google Scholar] [CrossRef] [PubMed]
- Bhatia, A.; Peng, P.; Cohen, S.P. Radiofrequency procedures to relieve chronic knee pain: An evidence-based narrative review. Reg. Anesth. Pain Med. 2016, 41, 501–510. [Google Scholar] [CrossRef]
- Calodney, A.; Rosenthal, R.; Gordon, A.; Wright, R.E. Targeted radiofrequency techniques. In Techniques of Neurolysis; Springer: Berlin/Heidelberg, Germany, 2016; pp. 33–73. [Google Scholar]
- Chua, N.H.; Vissers, K.C.; Sluijter, M.E. Pulsed radiofrequency treatment in interventional pain management: Mechanisms and potential indications—A review. Acta Neurochir. 2011, 153, 763–771. [Google Scholar] [CrossRef] [PubMed]
- Collighan, N.; Richardson, J. Radiofrequency lesioning techniques in the management of chronic pain. Anaesth. Intensive Care Med. 2008, 9, 61–64. [Google Scholar] [CrossRef]
- Jamison, D.E.; Cohen, S.P. Radiofrequency techniques to treat chronic knee pain: A comprehensive review of anatomy, effectiveness, treatment parameters, and patient selection. J. Pain Res. 2018, 11, 1879. [Google Scholar] [CrossRef] [PubMed]
- Leggett, L.E.; Soril, L.J.; Lorenzetti, D.L.; Noseworthy, T.; Steadman, R.; Tiwana, S.; Clement, F. Radiofrequency ablation for chronic low back pain: A systematic review of randomized controlled trials. Pain Res. Manag. 2014, 19, e146–e153. [Google Scholar] [CrossRef] [PubMed]
- Boudier-Revéret, M.; Thu, A.C.; Hsiao, M.Y.; Shyu, S.G.; Chang, M.C. The Effectiveness of Pulsed Radiofrequency on Joint Pain: A Narrative Review. Pain Pract. 2019. [Google Scholar] [CrossRef]
- Deniz, S.; Bakal, O.; Inangil, G. Application of Radiofrequency in Pain Management. In Pain Management; IntechOpen: London, UK, 2016; p. 95. [Google Scholar]
- Mendis, V.; Mottaleb, R.; Sethi, S. Radiofrequency techniques in pain management. Anaesth. Intensive Care Med. 2019, 20, 572–575. [Google Scholar] [CrossRef]
- Berjano, E.J. Theoretical modeling for radiofrequency ablation: State-of-the-art and challenges for the future. Biomed. Eng. Online 2006, 5, 24. [Google Scholar] [CrossRef]
- Chiang, J.; Wang, P.; Brace, C.L. Computational modelling of microwave tumour ablations. Int. J. Hyperth. 2013, 29, 308–317. [Google Scholar] [CrossRef]
- Singh, S.; Melnik, R. Coupled thermo-electro-mechanical models for thermal ablation of biological tissues and heat relaxation time effects. Phys. Med. Biol. 2019, 64, 245008. [Google Scholar] [CrossRef]
- Singh, S.; Repaka, R. Numerical study to establish relationship between coagulation volume and target tip temperature during temperature-controlled radiofrequency ablation. Electromagn. Biol. Med. 2018, 37, 13–22. [Google Scholar] [CrossRef]
- Singh, S.; Repaka, R.; Al-Jumaily, A. Sensitivity analysis of critical parameters affecting the efficacy of microwave ablation using Taguchi method. Int. J. RF Microw. Comput. Aided Eng. 2019, 29, e21581. [Google Scholar] [CrossRef]
- Zhang, B.; Moser, M.A.; Zhang, E.M.; Luo, Y.; Liu, C.; Zhang, W. A review of radiofrequency ablation: Large target tissue necrosis and mathematical modelling. Phys. Med. 2016, 32, 961–971. [Google Scholar] [CrossRef]
- Ewertowska, E.; Mercadal, B.; Muñoz, V.; Ivorra, A.; Trujillo, M.; Berjano, E. Effect of applied voltage, duration and repetition frequency of RF pulses for pain relief on temperature spikes and electrical field: A computer modelling study. Int. J. Hyperth. 2018, 34, 112–121. [Google Scholar] [CrossRef] [PubMed]
- Pérez, J.J.; Pérez-Cajaraville, J.J.; Muñoz, V.; Berjano, E. Computer modeling of electrical and thermal performance during bipolar pulsed radiofrequency for pain relief. Med Phys. 2014, 41, 071708. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Melnik, R. Computational analysis of pulsed radiofrequency ablation in treating chronic pain. In Computational Science–ICCS 2019, Proceedings of the ICCS 2019, Faro, Portugal, 12–14 June 2019; Lecture Notes in Computer, Science; Rodrigues, J.M.F., Cardoso, P.J.S., Monteiro, J., Lam, R., Krzhizhanovskaya, V.V., Lees, M.H., Dongarra, J.J., Sloot, P.M.A., Eds.; Springer: Cham, Switzerland, 2019; Volume 11539, pp. 436–450. [Google Scholar]
- Singh, S.; Melnik, R. Effects of heterogeneous surroundings on the efficacy of continuous radiofrequency for pain relief. Presented at the 2nd International Conference on Bioinformatics and Neurosciences (ICoBN 2019), Vancouver, BC, Canada, 26–28 August 2019; 5p. [Google Scholar]
- Singh, S.; Melnik, R. Radiofrequency ablation for treating chronic pain of bones: Effects of nerve locations. In Bioinformatics and Biomedical Engineering, Proceedings of the IWBBIO 2019, Granada, Spain, 8–10 May 2019; Lecture Notes in Computer Science; Rojas, I., Valenzuela, O., Rojas, F., Ortuño, F., Eds.; Springer: Cham, Switzerland, 2019; Volume 11466, pp. 418–429. [Google Scholar]
- Hasgall, P.; Di Gennaro, F.; Baumgartner, C.; Neufeld, E.; Lloyd, B.; Gosselin, M.; Payne, D.; Klingenböck, A.; Kuster, N. IT’IS Database for Thermal and Electromagnetic Parameters of Biological Tissues, Version 4.0; 15 May 2018. Available online: https://itis.swiss/virtual-population/tissue-properties/database/ (accessed on 4 April 2020).
- Singh, S.; Repaka, R. Temperature-controlled radiofrequency ablation of different tissues using two-compartment models. Int. J. Hyperth. 2017, 33, 122–134. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Repaka, R. Effect of different breast density compositions on thermal damage of breast tumor during radiofrequency ablation. Appl. Therm. Eng. 2017, 125, 443–451. [Google Scholar] [CrossRef]
- Singh, S.; Repaka, R. Parametric sensitivity analysis of critical factors affecting the thermal damage during RFA of breast tumor. Int. J. Therm. Sci. 2018, 124, 366–374. [Google Scholar] [CrossRef]
- Singh, S.; Bhowmik, A.; Repaka, R. Thermal analysis of induced damage to the healthy cell during RFA of breast tumor. J. Therm. Boil. 2016, 58, 80–90. [Google Scholar] [CrossRef]
- Singh, S.; Repaka, R. Numerical investigation of convective cooling in minimizing skin burns during radiofrequency ablation of breast tumor. Sādhanā 2018, 43, 90. [Google Scholar] [CrossRef]
- Singh, S.; Repaka, R. Thermal characterization using fourier and non-fourier conduction during radiofrequency ablation of breast tumor. Multiph. Sci. Technol. 2018, 30, 207–219. [Google Scholar] [CrossRef]
- COMSOL Multiphysics v. 5.2; COMSOL AB: Stockholm, Sweden, 2016; Available online: www.comsol.com (accessed on 4 April 2020).
- Besler, E.; Curtis Wang, Y.; Chan, T.C.; Sahakian, A.V. Real-time monitoring radiofrequency ablation using tree-based ensemble learning models. Int. J. Hyperth. 2019, 36, 427–436. [Google Scholar] [CrossRef] [PubMed]
- Besler, E.; Wang, Y.C.; Chan, T.; Sahakian, A.V. Classifying Small Volumes of Tissue for Real-Time Monitoring Radiofrequency Ablation. In Proceedings of the Conference on Artificial Intelligence in Medicine in Europe, Poznan, Poland, 26–29 June 2019; pp. 205–215. [Google Scholar]
- Buchlak, Q.D.; Esmaili, N.; Leveque, J.-C.; Farrokhi, F.; Bennett, C.; Piccardi, M.; Sethi, R.K. Machine learning applications to clinical decision support in neurosurgery: An artificial intelligence augmented systematic review. Neurosurg. Rev. 2019, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Farrokhi, F.; Buchlak, Q.D.; Sikora, M.; Esmaili, N.; Marsans, M.; McLeod, P.; Mark, J.; Cox, E.; Bennett, C.; Carlson, J. Investigating risk factors and predicting complications in deep brain stimulation surgery with machine learning algorithms. World Neurosurg. 2020, 134, e325–e338. [Google Scholar] [CrossRef] [PubMed]
- Foreman, B. Neurocritical Care: Bench to Bedside (Eds. Claude Hemphill, Michael James) Integrating and Using Big Data in Neurocritical Care. Neurotherapeutics 2020, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Cosman, E.R., Jr.; Cosman, E.R., Sr. Electric and thermal field effects in tissue around radiofrequency electrodes. Pain Med. 2005, 6, 405–424. [Google Scholar] [CrossRef]
- Shealy, C.N. Percutaneous radiofrequency denervation of spinal facets: Treatment for chronic back pain and sciatica. J. Neurosurg. 1975, 43, 448–451. [Google Scholar] [CrossRef]
- Ajrawat, P.; Radomski, L.; Bhatia, A.; Peng, P.; Nath, N.; Gandhi, R. Radiofrequency Procedures for the Treatment of Symptomatic Knee Osteoarthritis: A Systematic Review. Pain Med. 2020, 21, 333–348. [Google Scholar] [CrossRef]
- Boesch, J.M.; Campoy, L.; Southard, T.; Dewey, C.; Erb, H.N.; Gleed, R.D.; Martin-Flores, M.; Sakai, D.M.; Sutton, J.; Williamson, B. Histological, electrophysiological and clinical effects of thermal radiofrequency therapy of the saphenous nerve and pulsed radiofrequency therapy of the sciatic nerve in dogs. Vet. Anaesth. Analg. 2019, 46, 689–698. [Google Scholar] [CrossRef]
- Filippiadis, D.; Charalampopoulos, G.; Mazioti, A.; Alexopoulou, E.; Vrachliotis, T.; Brountzos, E.; Kelekis, N.; Kelekis, A. Interventional radiology techniques for pain reduction and mobility improvement in patients with knee osteoarthritis. Diagn. Interv. Imaging 2019, 100, 391–400. [Google Scholar] [CrossRef]
- Filippiadis, D.; Velonakis, G.; Mazioti, A.; Konstantos, C.; Brountzos, E.; Kelekis, N.; Kelekis, A. Intra-articular application of pulsed radiofrequency combined with viscosupplementation for improvement of knee osteoarthritis symptoms: A single centre prospective study. Int. J. Hyperth. 2018, 34, 1265–1269. [Google Scholar] [CrossRef]
- Ho, K.W.D.; Przkora, R.; Kumar, S. Sphenopalatine ganglion: Block, radiofrequency ablation and neurostimulation-a systematic review. J. Headache Pain 2017, 18, 118. [Google Scholar] [CrossRef]
- Kwak, S.; Jeong, D.; Choo, Y.J.; Chang, M.C. Management of neuropathic pain induced by cubital tunnel syndrome using pulsed radiofrequency: Two case reports. Medicine 2019, 98, e15599. [Google Scholar] [CrossRef] [PubMed]
- Schneider, B.J.; Doan, L.; Maes, M.K.; Martinez, K.R.; Gonzalez Cota, A.; Bogduk, N. Systematic Review of the Effectiveness of Lumbar Medial Branch Thermal Radiofrequency Neurotomy, Stratified for Diagnostic Methods and Procedural Technique. Pain Med. 2020. [Google Scholar] [CrossRef] [PubMed]
- Sluijter, M.E.; Teixeira, A.; Serra, V.; Balogh, S.; Schianchi, P. Intra-articular application of pulsed radiofrequency for arthrogenic pain—Report of six cases. Pain Pract. 2008, 8, 57–61. [Google Scholar] [CrossRef] [PubMed]
- Xie, K.; Liu, S.; Huang, B.; Yao, M. Effects of Supraorbital Foramen Variations on the Treatment Efficacy of Radiofrequency Therapy for V1 Trigeminal Neuralgia: A Retrospective Study. Pain Res. Manag. 2020, 2020, 8142489. [Google Scholar] [CrossRef]
- Cohen, B.R.; Soriano, E.T. Pulsed Radiofrequency Neuromodulation in Interventional Pain Management—A Growing Technology. J. Radiol. Nurs. 2018, 37, 181–187. [Google Scholar] [CrossRef]
- Hata, J.; Perret-Karimi, D.; DeSilva, C.; Leung, D.; Betesh, N.; Luo, Z.D.; Dawodu, S.; Sinavsky, K.; Stokes, O.J.; English, S. Pulsed radiofrequency current in the treatment of pain. Crit. Rev.™ Phys. Rehabil. Med. 2011, 23. [Google Scholar] [CrossRef]
- Vallejo, R.; Benyamin, R.M.; Aliaga, L. Radiofrequency vs. pulse radiofrequency: The end of the controversy. Tech. Reg. Anesth. Pain Manag. 2010, 14, 128–132. [Google Scholar] [CrossRef]
- Vatansever, D.; Tekin, I.; Tuglu, I.; Erbuyun, K.; Ok, G. A comparison of the neuroablative effects of conventional and pulsed radiofrequency techniques. Clin. J. Pain 2008, 24, 717–724. [Google Scholar] [CrossRef] [PubMed]
- Gooneie, A.; Schuschnigg, S.; Holzer, C. A review of multiscale computational methods in polymeric materials. Polymers 2017, 9, 16. [Google Scholar] [CrossRef]
- Badu, S.; Prabhakar, S.; Melnik, R.; Singh, S. Atomistic to continuum model for studying mechanical properties of RNA nanotubes. Comput. Methods Biomech. Biomed. Eng. 2020, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Antoniouk, A.V.; Melnik, R. Mathematics and Life Sciences; De Gruyter: Berlin, Germany, 2013. [Google Scholar]
- Melnik, R.V.; Roberts, A.H. Computational models for multi-scale coupled dynamic problems. Future Gener. Comput. Syst. 2004, 20, 453–464. [Google Scholar] [CrossRef]
- Melnik, R.V.; Wei, X.; Moreno–Hagelsieb, G. Nonlinear dynamics of cell cycles with stochastic mathematical models. J. Biol. Syst. 2009, 17, 425–460. [Google Scholar] [CrossRef]
- Ortiz-Catalan, M. The stochastic entanglement and phantom motor execution hypotheses: A theoretical framework for the origin and treatment of phantom limb pain. Front. Neurol. 2018, 9, 748. [Google Scholar] [CrossRef]
- Stroe, M.; Crolet, J.; Racila, M. Mechanotransduction in cortical bone and the role of piezoelectricity: A numerical approach. Comput. Methods Biomech. Biomed. Eng. 2013, 16, 119–129. [Google Scholar] [CrossRef]
- Jacob, J.; More, N.; Kalia, K.; Kapusetti, G. Piezoelectric smart biomaterials for bone and cartilage tissue engineering. Inflamm. Regen. 2018, 38, 2. [Google Scholar] [CrossRef]
- Melnik, R.V. Generalised solutions, discrete models and energy estimates for a 2D problem of coupled field theory. Appl. Math. Comput. 2000, 107, 27–55. [Google Scholar] [CrossRef]
- Mahapatra, D.R.; Melnik, R. Modelling and analysis of collagen piezoelectricity in human cornea. Dyn. Contin. Discret. Impulsive Syst. Ser. A Math. Anal. 2006, 13, 377–384. [Google Scholar]
- Melnik, R. Convergence of the operator-difference scheme to generalized solutions of a coupled field theory problem. J. Differ. Equ. Appl. 1998, 4, 185–212. [Google Scholar] [CrossRef]
- Melnik, R.; Mahapatra, R. Coupled effects in quantum dot nanostructures with nonlinear strain and bridging modelling scales. Comput. Struct. 2007, 85, 698–711. [Google Scholar] [CrossRef][Green Version]
- Melnik, R.; Melnik, K. A note on the class of weakly coupled problems of non-stationary piezoelectricity. Commun. Numer. Methods Eng. 1998, 14, 839–847. [Google Scholar] [CrossRef]
- Melnik, R.; Melnik, K. Modelling dynamics of piezoelectric solids in the two-dimensional case. Appl. Math. Model. 2000, 24, 147–163. [Google Scholar] [CrossRef]
- Melnik, R.V. Numerical analysis of dynamic characteristics of coupled piezoelectric systems in acoustic media. Math. Comput. Simul. 2003, 61, 497–507. [Google Scholar] [CrossRef]
- Melnik, R.V.N. The stability condition and energy estimate for nonstationary problems of coupled electroelasticity. Math. Mech. Solids 1997, 2, 153–180. [Google Scholar] [CrossRef]
- Patil, S.R.; Melnik, R.V. Coupled electromechanical effects in II–VI group finite length semiconductor nanowires. J. Phys. D Appl. Phys. 2009, 42, 145113. [Google Scholar] [CrossRef][Green Version]
- Prabhakar, S.; Melnik, R.V.; Neittaanmäki, P.; Tiihonen, T. Coupled electromechanical effects in wurtzite quantum dots with wetting layers in gate controlled electric fields: The multiband case. Phys. E Low Dimens. Syst. Nanostruct. 2012, 46, 97–104. [Google Scholar] [CrossRef]
- Singh, S.; Melnik, R. Thermal ablation of biological tissues in disease treatment: A review of computational models and future directions. Electromagn. Biol. Med. 2020. [Google Scholar] [CrossRef]
- Melnik, R.; Strunin, D.; Roberts, A. Nonlinear analysis of rubber-based polymeric materials with thermal relaxation models. Numer. Heat Transf. Part A Appl. 2005, 47, 549–569. [Google Scholar] [CrossRef]
- Strunin, D.; Melnik, R.; Roberts, A. Numerical modelling of thermoelastic processes using nonlinear theories with thermal relaxation time. ANZIAM J. 2000, 42, 1356–1378. [Google Scholar] [CrossRef][Green Version]
- Strunin, D.; Melnik, R.; Roberts, A. Coupled thermomechanical waves in hyperbolic thermoelasticity. J. Therm. Stresses 2001, 24, 121–140. [Google Scholar]
- Andreozzi, A.; Brunese, L.; Iasiello, M.; Tucci, C.; Vanoli, G.P. Modeling heat transfer in tumors: A review of thermal therapies. Ann. Biomed. Eng. 2019, 47, 676–693. [Google Scholar] [CrossRef] [PubMed]
- Melnik, R.; Roberts, A.; Thomas, K. Coupled thermomechanical dynamics of phase transitions in shape memory alloys and related hysteresis phenomena. Mech. Res. Commun. 2001, 28, 637–651. [Google Scholar] [CrossRef]
- Melnik, R.V. Discrete models of coupled dynamic thermoelasticity for stress–temperature formulations. Appl. Math. Comput. 2001, 122, 107–132. [Google Scholar] [CrossRef]
- Wang, L.-X.; Melnik, R.V. Differential-algebraic approach to coupled problems of dynamic thermoelasticity. Appl. Math. Mech. 2006, 27, 1185–1196. [Google Scholar] [CrossRef]
- Wang, L.X.; Melnik, R.V. Thermo-mechanical wave propagations in shape memory alloy rod with phase transformations. Mech. Adv. Mater. Struct. 2007, 14, 665–676. [Google Scholar] [CrossRef]
- Wang, L.X.; Melnik, R.V. Finite volume analysis of nonlinear thermo-mechanical dynamics of shape memory alloys. Heat Mass Transf. 2007, 43, 535–546. [Google Scholar] [CrossRef][Green Version]
- Dhote, R.; Melnik, R.; Zu, J. Dynamic thermo-mechanical coupling and size effects in finite shape memory alloy nanostructures. Comput. Mater. Sci. 2012, 63, 105–117. [Google Scholar] [CrossRef]
- Dhote, R.; Fabrizio, M.; Melnik, R.; Zu, J. Hysteresis phenomena in shape memory alloys by non-isothermal Ginzburg–Landau models. Commun. Nonlinear Sci. Numer. Simul. 2013, 18, 2549–2561. [Google Scholar] [CrossRef]
- Dhote, R.; Melnik, R.; Zu, J. Dynamic multi-axial behavior of shape memory alloy nanowires with coupled thermo-mechanical phase-field models. Meccanica 2014, 49, 1561–1575. [Google Scholar] [CrossRef]
- Dhote, R.; Gomez, H.; Melnik, R.; Zu, J. 3D coupled thermo-mechanical phase-field modeling of shape memory alloy dynamics via isogeometric analysis. Comput. Struct. 2015, 154, 48–58. [Google Scholar] [CrossRef]
- Dhote, R.P.; Gomez, H.; Melnik, R.N.; Zu, J. Shape memory alloy nanostructures with coupled dynamic thermo-mechanical effects. Comput. Phys. Commun. 2015, 192, 48–53. [Google Scholar] [CrossRef]
- Dhote, R.; Gomez, H.; Melnik, R.; Zu, J. Effect of aspect ratio and boundary conditions in modeling shape memory alloy nanostructures with 3D coupled dynamic phase-field theories. Math. Probl. Eng. 2016, 2016, 3647470. [Google Scholar] [CrossRef]
- Andreozzi, A.; Iasiello, M.; Netti, P.A. A thermoporoelastic model for fluid transport in tumour tissues. J. R. Soc. Interface 2019, 16, 20190030. [Google Scholar] [CrossRef] [PubMed]
- Karaki, W.; Lopez, C.A.; Borca-Tasciuc, D.-A.; De, S. A continuum thermomechanical model of in vivo electrosurgical heating of hydrated soft biological tissues. Int. J. Heat Mass Transf. 2018, 127, 961–974. [Google Scholar] [CrossRef] [PubMed]
- Matus, P.; Melnik, R.V.; Wang, L.; Rybak, I. Applications of fully conservative schemes in nonlinear thermoelasticity: Modelling shape memory materials. Math. Comput. Simul. 2004, 65, 489–509. [Google Scholar] [CrossRef]
- Melnik, R.V.; Roberts, A. Modelling nonlinear dynamics of shape-memory-alloys with approximate models of coupled thermoelasticity. ZAMM J. Appl. Math. Mech 2003, 83, 93–104. [Google Scholar] [CrossRef]
- Dhote, R.; Fabrizio, M.; Melnik, R.; Zu, J. A three-dimensional non-isothermal Ginzburg–Landau phase-field model for shape memory alloys. Model. Simul. Mater. Sci. Eng. 2014, 22, 085011. [Google Scholar] [CrossRef]
- Dhote, R.; Gomez, H.; Melnik, R.; Zu, J. Isogeometric analysis of a dynamic thermo-mechanical phase-field model applied to shape memory alloys. Comput. Mech. 2014, 53, 1235–1250. [Google Scholar] [CrossRef]
- Melnik, R.V. Computational analysis of coupled physical fields in piezothermoelastic media. Comput. Phys. Commun. 2001, 142, 231–237. [Google Scholar] [CrossRef]
- Melnik, R. Modelling coupled dynamics: Piezoelectric elements under changing temperature conditions. Int. Commun. Heat Mass Transf. 2003, 30, 83–92. [Google Scholar] [CrossRef]
- Patil, S.R.; Melnik, R. Thermopiezoelectric effects on optoelectronic properties of CdTe/ZnTe quantum wires. Phys. Status Solidi A 2009, 206, 960–964. [Google Scholar] [CrossRef]
- Prabhakar, S.; Melnik, R.V.; Neittaanmäki, P.; Tiihonen, T. Coupled magneto-thermo-electromechanical effects and electronic properties of quantum dots. J. Comput. Theor. Nanosci. 2013, 10, 534–547. [Google Scholar] [CrossRef]
- Wang, D.; Du, H.; Wang, L.; Melnik, R. A phase field approach for the fully coupled thermo-electro-mechanical dynamics of nanoscale ferroelectric actuators. Smart Mater. Struct. 2018, 27, 055012. [Google Scholar] [CrossRef]
- Melnik, R.; Uhlherr, A.; Hodgkin, J.; De Hoog, F. Distance geometry algorithms in molecular modelling of polymer and composite systems. Comput. Math. Appl. 2003, 45, 515–534. [Google Scholar] [CrossRef][Green Version]
- Petras, A.; Leoni, M.; Guerra, J.M.; Jansson, J.; Gerardo-Giorda, L. A computational model of open-irrigated radiofrequency catheter ablation accounting for mechanical properties of the cardiac tissue. Int. J. Numer. Methods Biomed. Eng. 2019, 35, e3232. [Google Scholar] [CrossRef] [PubMed]
- Woeppel, K.; Yang, Q.; Cui, X.T. Recent advances in neural electrode–tissue interfaces. Curr. Opin. Biomed. Eng. 2017, 4, 21–31. [Google Scholar] [CrossRef]
- Won, S.M.; Song, E.; Zhao, J.; Li, J.; Rivnay, J.; Rogers, J.A. Recent advances in materials, devices, and systems for neural interfaces. Adv. Mater. 2018, 30, 1800534. [Google Scholar] [CrossRef]
- Yan, S.; Gu, K.; Wu, X.; Wang, W. Computer simulation study on the effect of electrode–tissue contact force on thermal lesion size in cardiac radiofrequency ablation. Int. J. Hyperth. 2020, 37, 37–48. [Google Scholar] [CrossRef]
- Melnik, R.V. Computationally efficient algorithms for modelling thermal degradation and spiking phenomena in polymeric materials. Comput. Chem. Eng. 2003, 27, 1473–1484. [Google Scholar] [CrossRef]
- Melnik, R. Mathematical and Computer Modelling of Coupled Reaction Kinetics and Heat Transfer in Processing Polymeric Materials. Model. Simul. Mater. Sci. Eng. 2002, 10, 341–358. [Google Scholar] [CrossRef][Green Version]
- Gupta, R.; Noraziah, A.; Gupta, A.; Fauzi, A.A.C. Challenges in Predicting Wood Plastic Composites (WPCs). Adv. Sci. Lett. 2017, 23, 11035–11039. [Google Scholar] [CrossRef]
- Audigier, C.; Mansi, T.; Delingette, H.; Rapaka, S.; Passerini, T.; Mihalef, V.; Jolly, M.-P.; Pop, R.; Diana, M.; Soler, L. Comprehensive preclinical evaluation of a multi-physics model of liver tumor radiofrequency ablation. Int. J. Comput. Assist. Radiol. Surg. 2017, 12, 1543–1559. [Google Scholar] [CrossRef] [PubMed]
- Chaichanyut, M.; Tungjitkusolmun, S. Microwave ablation using four-tine antenna: Effects of blood flow velocity, vessel location, and total displacement on porous hepatic cancer tissue. Comput. Math. Methods Med. 2016, 2016, 4846738. [Google Scholar] [CrossRef] [PubMed]
- Paul, A.; Paul, A. Thermomechanical analysis of a triple layered skin structure in presence of nanoparticle embedding multi-level blood vessels. Int. J. Heat Mass Transf. 2020, 148, 119076. [Google Scholar] [CrossRef]
- Salimpour, M.R.; Shirani, E. Heat transfer analysis of skin during thermal therapy using thermal wave equation. J. Therm. Biol. 2017, 64, 7–18. [Google Scholar]
- Shao, Y.; Arjun, B.; Leo, H.; Chua, K. A computational theoretical model for radiofrequency ablation of tumor with complex vascularization. Comput. Biol. Med. 2017, 89, 282–292. [Google Scholar] [CrossRef]
- Keangin, P.; Rattanadecho, P. A numerical investigation of microwave ablation on porous liver tissue. Adv. Mech. Eng. 2018, 10. [Google Scholar] [CrossRef]
- Nield, D.A.; Bejan, A. Heat transfer through a porous medium. In Convection in Porous Media; Springer: Berlin/Heidelberg, Germany, 2013; pp. 31–46. [Google Scholar]
- Schutt, D.J.; Haemmerich, D. Effects of variation in perfusion rates and of perfusion models in computational models of radio frequency tumor ablation. Med. Phys. 2008, 35, 3462–3470. [Google Scholar] [CrossRef]
- Yang, X.-D.; Melnik, R.V. Effect of internal viscosity on Brownian dynamics of DNA molecules in shear flow. Comput. Boil. Chem. 2007, 31, 110–114. [Google Scholar] [CrossRef][Green Version]
- Yang, X.-D.; Melnik, R.V. Accounting for the effect of internal viscosity in dumbbell models for polymeric fluids and relaxation of DNA. Discret. Contin. Dyn. Syst. 2007, 1052–1060. Available online: scholars.wlu.ca/cgi/viewcontent.cgi?article=1031context=math_faculty (accessed on 4 April 2020).
- Yang, X.-D.; Melnik, R.V. Effect of internal viscosity of polymeric fluids under strong extensional flows. Chin. J. Polym. Sci. 2009, 27, 189–193. [Google Scholar] [CrossRef]
- Kamath, H.; Willatzen, M.; Melnik, R.V. Vibration of piezoelectric elements surrounded by fluid media. Ultrasonics 2006, 44, 64–72. [Google Scholar] [CrossRef] [PubMed]
- Liang, F.; Yang, X.; Zhang, W.; Qian, Y.; Melnik, R. Parametric Vibration Analysis of Pipes Conveying Fluid by Nonlinear Normal Modes and a Numerical Iterative Approach. Adv. Appl. Math. Mech. 2019, 11, 38–52. [Google Scholar] [CrossRef]
- Alber, M.; Tepole, A.B.; Cannon, W.R.; De, S.; Dura-Bernal, S.; Garikipati, K.; Karniadakis, G.; Lytton, W.W.; Perdikaris, P.; Petzold, L. Integrating machine learning and multiscale modeling—Perspectives, challenges, and opportunities in the biological, biomedical, and behavioral sciences. NPJ Digit. Med. 2019, 2, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Peng, G.C.; Alber, M.; Tepole, A.B.; Cannon, W.R.; De, S.; Dura-Bernal, S.; Garikipati, K.; Karniadakis, G.; Lytton, W.W.; Perdikaris, P. Multiscale Modeling Meets Machine Learning: What Can We Learn? Arch. Comput. Methods Eng. 2020, 1–21. [Google Scholar] [CrossRef]
- Negro, R.; Rucco, M.; Creanza, A.; Mormile, A.; Limone, P.P.; Garberoglio, R.; Spiezia, S.; Monti, S.; Cugini, C.; El Dalati, G. Machine Learning Prediction of Radiofrequency Thermal Ablation Efficacy: A New Option to Optimize Thyroid Nodule Selection. Eur. Thyroid J. 2019, 1–8. [Google Scholar] [CrossRef]
- Hajimolahoseini, H.; Hashemi, J.; Gazor, S.; Redfearn, D. Inflection point analysis: A machine learning approach for extraction of IEGM active intervals during atrial fibrillation. Artif. Intell. Med. 2018, 85, 7–15. [Google Scholar] [CrossRef]
- Lötsch, J.; Ultsch, A. Machine learning in pain research. Pain 2018, 159, 623. [Google Scholar] [CrossRef]
- Wang, Y.C.; Chan, T.C.-H.; Sahakian, A.V. Real-time estimation of lesion depth and control of radiofrequency ablation within ex vivo animal tissues using a neural network. Int. J. Hyperth. 2018, 34, 1104–1113. [Google Scholar] [CrossRef]
- Besler, E.; Wang, Y.C.; Sahakian, A.V. Early and Late Fusion Machine Learning on Multi-Frequency Electrical Impedance Data to Improve Radiofrequency Ablation Monitoring. IEEE J. Biomed. Health Inform. 2019. [Google Scholar] [CrossRef]
- Li, K.; Vakharia, V.N.; Sparks, R.; França, L.G.; Granados, A.; McEvoy, A.W.; Miserocchi, A.; Wang, M.; Ourselin, S.; Duncan, J.S. Optimizing trajectories for cranial laser interstitial thermal therapy using computer-assisted planning: A machine learning approach. Neurotherapeutics 2019, 16, 182–191. [Google Scholar] [CrossRef] [PubMed]
- Yildiz, F.; Özdemir, A.T. Prediction of laser-induced thermal damage with artificial neural networks. Laser Phys. 2019, 29, 075205. [Google Scholar] [CrossRef]
- Zhang, J.; Chauhan, S. Neural network methodology for real-time modelling of bio-heat transfer during thermo-therapeutic applications. Artif. Intell. Med. 2019, 101, 101728. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Zhong, Y.; Gu, C. Neural network modelling of soft tissue deformation for surgical simulation. Artif. Intell. Med. 2019, 97, 61–70. [Google Scholar] [CrossRef]
- Melnik, R.V. Coupling control and human factors in mathematical models of complex systems. Eng. Appl. Artif. Intell. 2009, 22, 351–362. [Google Scholar] [CrossRef]
- Melnik, R.V. Markov chain network training and conservation law approximations: Linking microscopic and macroscopic models for evolution. Appl. Math. Comput. 2008, 199, 315–333. [Google Scholar] [CrossRef]
- Moayedi, M.; Davis, K.D. Theories of pain: From specificity to gate control. J. Neurophysiol. 2013, 109, 5–12. [Google Scholar] [CrossRef]
- Argüello, E.J.; Silva, R.J.; Huerta, M.K.; Avila, R.S. Computational modeling of peripheral pain: A commentary. Biomed. Eng. Online 2015, 14, 56. [Google Scholar] [CrossRef]
- Kucyi, A.; Davis, K.D. The dynamic pain connectome. Trends Neurosci. 2015, 38, 86–95. [Google Scholar] [CrossRef]
- Seth, B.; de Gray, L. Genesis of chronic pain. Anaesth. Intensive Care Med. 2016, 17, 431–435. [Google Scholar] [CrossRef]
- Tiemann, L.; Hohn, V.D.; Dinh, S.T.; May, E.S.; Nickel, M.M.; Gross, J.; Ploner, M. Distinct patterns of brain activity mediate perceptual and motor and autonomic responses to noxious stimuli. Nat. Commun. 2018, 9, 1–12. [Google Scholar] [CrossRef]
- Li, Y.; Yue, J.; Yang, C. Unraveling the role of Mg++ in osteoarthritis. Life Sci. 2016, 147, 24–29. [Google Scholar] [CrossRef] [PubMed]
- Srebro, D.; Vuckovic, S.; Milovanovic, A.; Kosutic, J.; Savic Vujovic, K.; Prostran, M. Magnesium in pain research: State of the art. Curr. Med. Chem. 2017, 24, 424–434. [Google Scholar]
- Mercadal, B.; Vicente, R.; Ivorra, A. Pulsed Radiofrequency for Chronic Pain: An Electroporation Mediated Calcium Signaling Process? Biophys. J. 2018, 114, 287a. [Google Scholar] [CrossRef]
- Li, Z.; Peng, Y.; Pang, X.; Tang, B. Potential Therapeutic Effects of Mg/HCOOH Metal Organic Framework on Relieving Osteoarthritis. ChemMedChem 2019, 15, 13–16. [Google Scholar] [CrossRef] [PubMed]
- Kosik-Bogacka, D.I.; Lanocha-Arendarczyk, N.; Kot, K.; Zietek, P.; Karaczun, M.; Prokopowicz, A.; Kupnicka, P.; Ciosek, Z. Calcium, magnesium, zinc and lead concentrations in the structures forming knee joint in patients with osteoarthritis. J. Trace Elem. Med. Biol. 2018, 50, 409–414. [Google Scholar] [CrossRef]

| Material (Tissue/Electrode) | Electrical Conductivity σ [S/m] | Specific Heat Capacity c [J/(kg·K)] | Thermal Conductivity k [W/(m·K)] | Density ρ [kg/m3] | Blood Perfusion ωb [s−1] |
|---|---|---|---|---|---|
| Muscle | 0.446 | 3421 | 0.49 | 1090 | 6.35 × 10−4 |
| Bone | 0.0222 | 1313 | 0.32 | 1908 | 4.67 × 10−4 |
| Nerve | 0.111 | 3613 | 0.49 | 1075 | 3.38 × 10−3 |
| Plastic | 10−5 | 1045 | 0.026 | 70 | – |
| Electrode | 7.4 × 106 | 480 | 15 | 8000 | – |
| Blood | – | 3617 | – | 1050 | – |
| Applied Voltage(V) | Electrical Conductivity σ [S/m] | Ambient Temperature [°C] | Numerically Predicted ΔT from the Previous Study [45] [°C] | Experimentally Measured ΔT from the Previous Study [45] [°C] | ΔT Computed from the Present Study [°C] |
|---|---|---|---|---|---|
| 7 | 0.38 | 26 | 6.8 | 7 | 6.75 |
| 13 | 0.44 | 26 | 27.7 | 26 | 26.83 |
| 16 | 0.47 | 26 | 44.8 | 41 | 43.39 |
| 16 | 0.47 | 34 | 44.8 | 48 | 43.40 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Singh, S.; Melnik, R. Domain Heterogeneity in Radiofrequency Therapies for Pain Relief: A Computational Study with Coupled Models. Bioengineering 2020, 7, 35. https://doi.org/10.3390/bioengineering7020035
Singh S, Melnik R. Domain Heterogeneity in Radiofrequency Therapies for Pain Relief: A Computational Study with Coupled Models. Bioengineering. 2020; 7(2):35. https://doi.org/10.3390/bioengineering7020035
Chicago/Turabian StyleSingh, Sundeep, and Roderick Melnik. 2020. "Domain Heterogeneity in Radiofrequency Therapies for Pain Relief: A Computational Study with Coupled Models" Bioengineering 7, no. 2: 35. https://doi.org/10.3390/bioengineering7020035
APA StyleSingh, S., & Melnik, R. (2020). Domain Heterogeneity in Radiofrequency Therapies for Pain Relief: A Computational Study with Coupled Models. Bioengineering, 7(2), 35. https://doi.org/10.3390/bioengineering7020035






