A Comprehensive Digital Workflow for Enhancing Dental Restorations in Severe Structural Wear
Abstract
1. Introduction
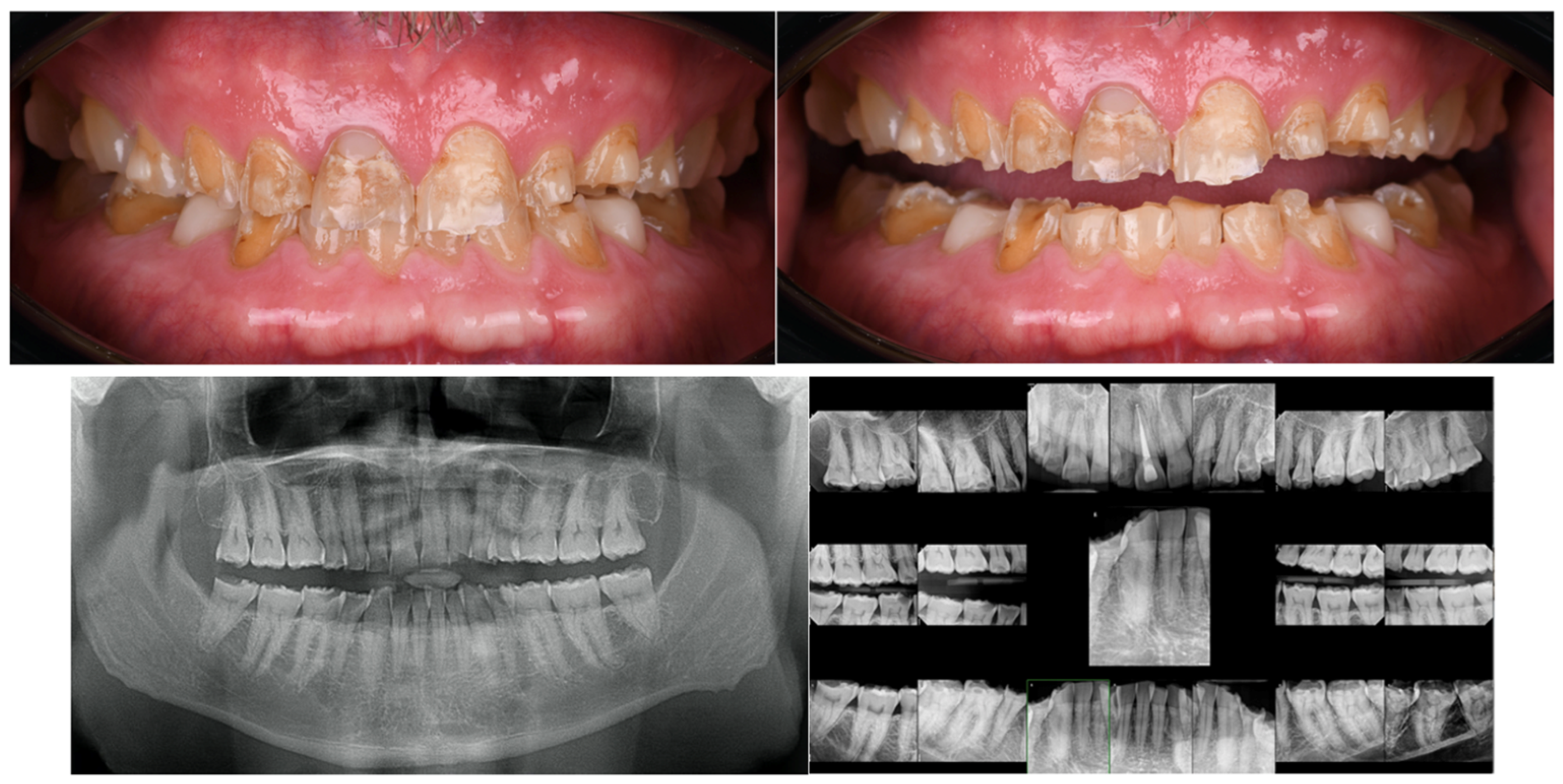
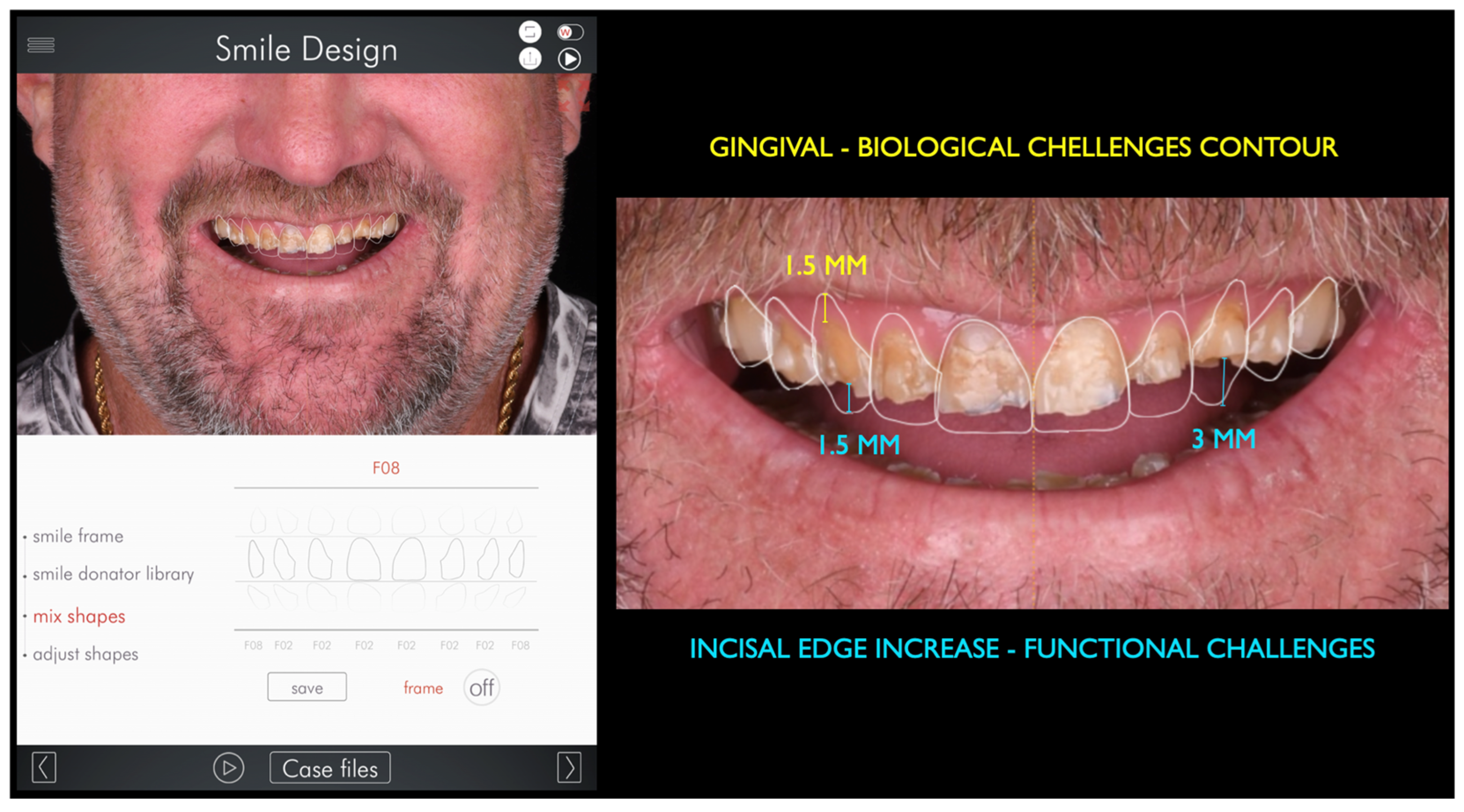
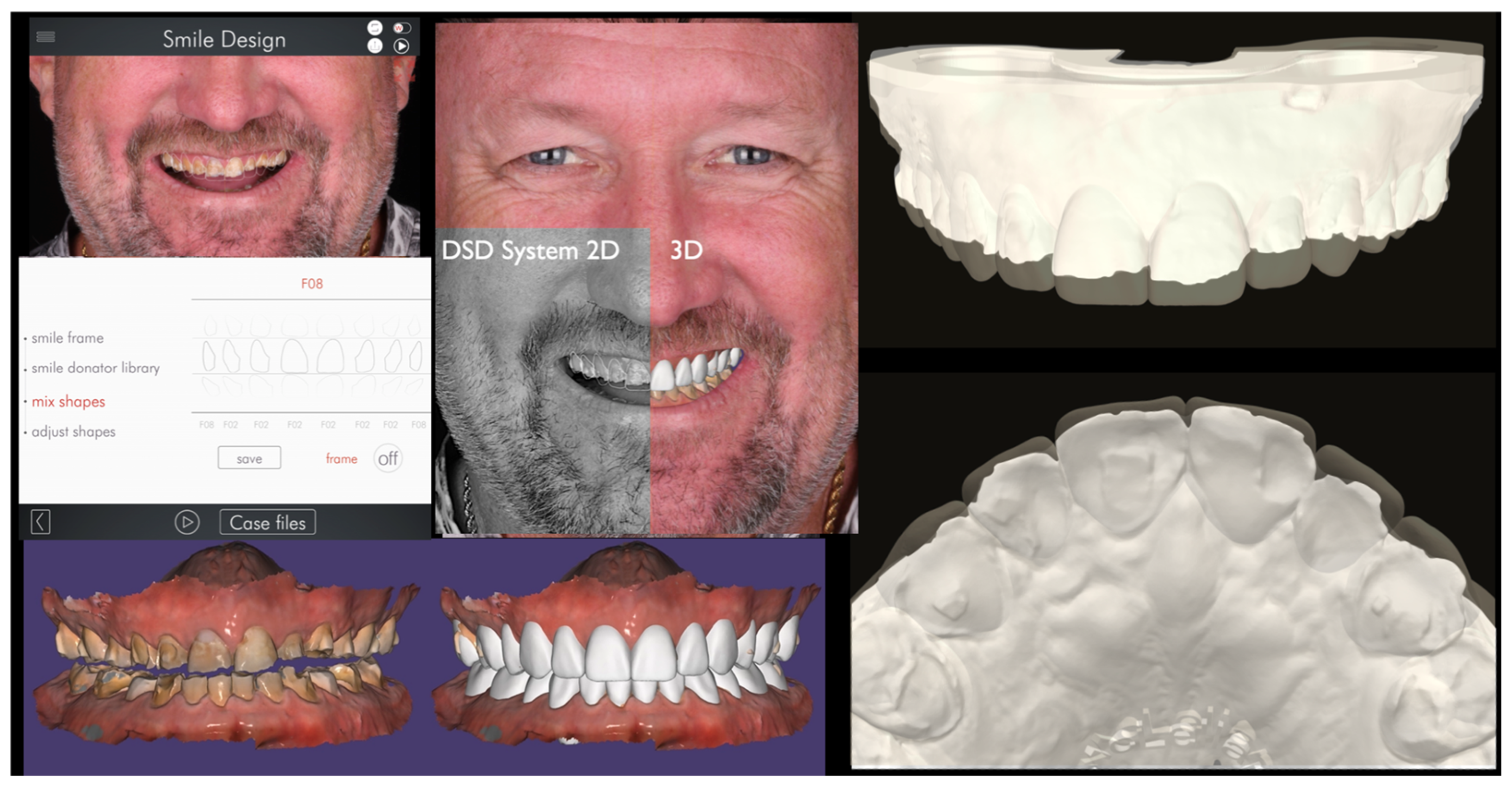
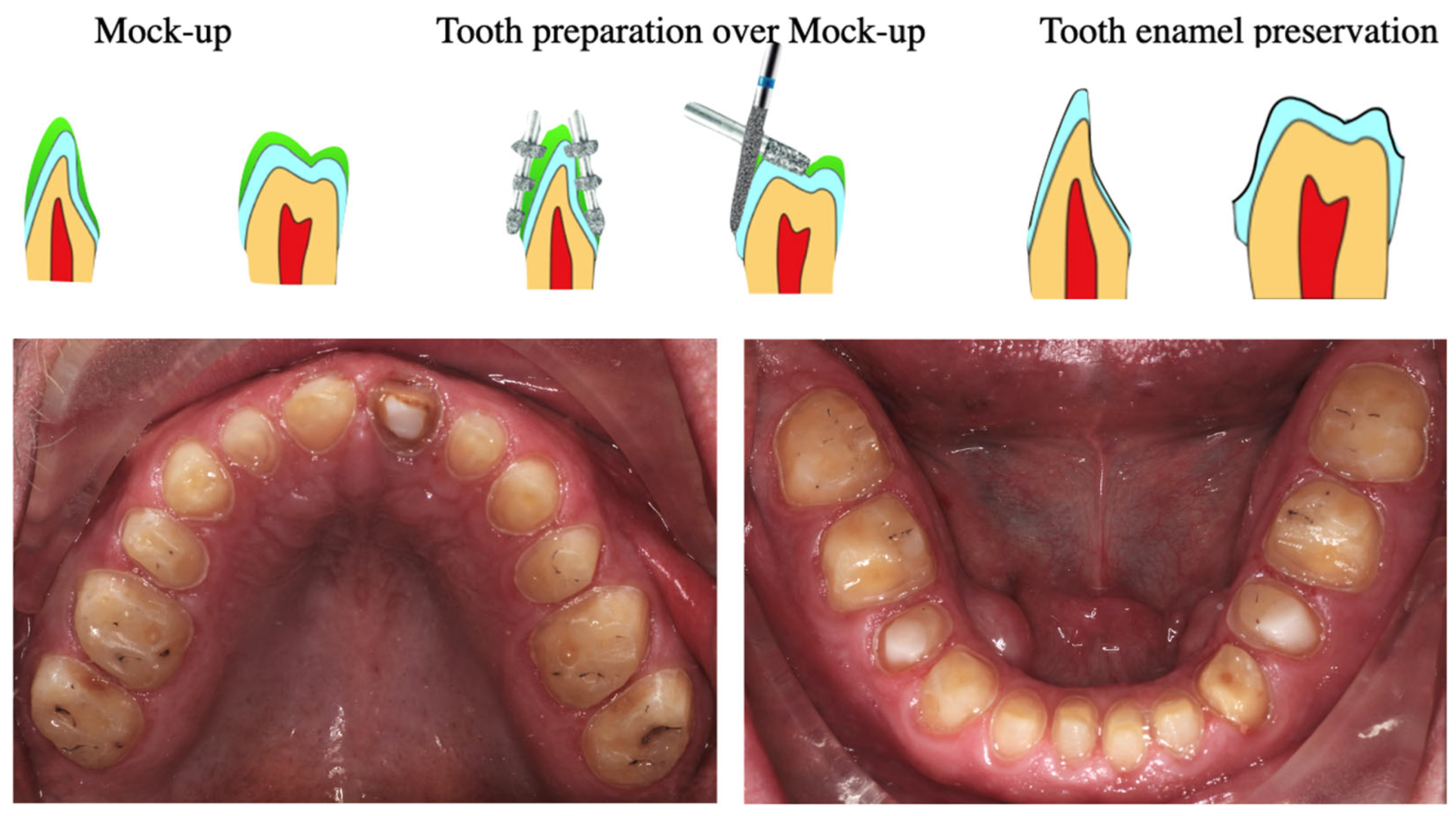
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cunha-Cruz, J.; Pashova, H.; Packard, J.D.; Zhou, L.; Hilton, T.J.; for Northwest PRECEDENT. Tooth wear: Prevalence and associated factors in general practice patients. Community Dent. Oral Epidemiol. 2010, 38, 228–234. [Google Scholar] [CrossRef]
- Sperber, G.H. Dental Wear: Attrition, Erosion, and Abrasion-A Palaeo-Odontological Approach. Dent. J. 2017, 5, 19. [Google Scholar] [CrossRef]
- Mehta, S.B.; Loomans, B.A.C.; van Sambeek, R.M.F.; Pereira-Cenci, T.; O’Toole, S. Managing tooth wear with respect to quality of life: An evidence-based decision on when to intervene. Br. Dent. J. 2023, 234, 455–458. [Google Scholar] [CrossRef]
- Yang, J.; Cai, D.; Wang, F.; He, D.; Ma, L.; Jin, Y.; Que, K. Non-carious cervical lesions (NCCLs) in a random sampling community population and the association of NCCLs with occlusive wear. J. Oral Rehabil. 2016, 43, 960–966. [Google Scholar] [CrossRef] [PubMed]
- Wetselaar, P.; Vermaire, J.H.; Visscher, C.M.; Lobbezoo, F.; Schuller, A.A. The Prevalence of Tooth Wear in the Dutch Adult Population. Caries Res. 2016, 50, 543–550. [Google Scholar] [CrossRef]
- Marró, M.L.; Aránguiz, V.; Ramirez, V.; Lussi, A. Prevalence of erosive tooth wear in Chilean adults, 2016: A cross-sectional study. J. Oral Rehabil. 2020, 47, 467–472. [Google Scholar] [CrossRef]
- Al-Khalifa, K.S. The Prevalence of Tooth Wear in an Adult Population from the Eastern Province of Saudi Arabia. Clin. Cosmet. Investig. Dent. 2020, 12, 525–531. [Google Scholar] [CrossRef] [PubMed]
- Afrashtehfar, K.I.; Manfredini, D. Five things to know about bruxism. J. N. J. Dent. Assoc. 2013, 84, 26. [Google Scholar]
- Loomans, B.; Opdam, N.; Attin, T.; Bartlett, D.; Edelhoff, D.; Frankenberger, R.; Benic, G.; Ramseyer, S.; Wetselaar, P.; Sterenborg, B.; et al. Severe Tooth Wear: European Consensus Statement on Management Guidelines. J. Adhes. Dent. 2017, 19, 111–119. [Google Scholar] [PubMed]
- Dallari, G.; Scalzo, I.; Rosati, R.M.; Sampaio, C.S.; Hirata, R. Full-mouth adhesive rehabilitation of a severe case of erosion treated with v-shaped veneers. J. Esthet. Restor. Dent. 2021, 33, 422–431. [Google Scholar] [CrossRef]
- Vailati, F.; Gruetter, L.; Belser, U.C. Adhesively restored anterior maxillary dentitions affected by severe erosion: Up to 6-year results of a prospective clinical study. Eur. J. Esthet. Dent. 2013, 8, 506–530. [Google Scholar]
- Calamita, M.; Coachman, C.; Sesma, N.; Kois, J. Occlusal vertical dimension: Treatment planning decisions and management considerations. Int. J. Esthet. Dent. 2019, 14, 166–181. [Google Scholar] [PubMed]
- Lanis, A.; Gallucci, G.; Pedrinaci, I. Full mouth oral rehabilitation of a severely worn dentition based on a fully digital workflow. J. Esthet. Restor. Dent. 2023, 35, 596–608. [Google Scholar] [CrossRef] [PubMed]
- Stawarczyk, B.; Meinen, J.; Wuersching, S.N. Two-body wear of novel monolithic lithium-silicate ceramic materials and their corresponding different antagonists. J. Dent. 2024, 144, 104952. [Google Scholar] [CrossRef] [PubMed]
- Luna-Domínguez, C.R.; Luna-Domínguez, J.H.; Blatz, M. Full-mouth rehabilitation in a completely digital workflow using partially adhesive monolithic zirconia restorations. J. Esthet. Restor. Dent. 2023, 35, 1050–1057. [Google Scholar] [CrossRef]
- Ferrando-Cascales, Á.; Astudillo-Rubio, D.; Pascual-Moscardó, A. A facially driven complete-mouth rehabilitation with ultrathin CAD-CAM composite resin veneers for a patient with severe tooth wear: A minimally invasive approach. J. Prosthet. Dent. 2020, 123, 537–547. [Google Scholar] [CrossRef]
- Jurado, C.A.; Lee, D.; Cortes, D.; Kaleinikova, Z.; Hernandez, A.I.; Donato, M.V.; Tsujimoto, A. Fracture Resistance of Chairside CAD/CAM Molar Crowns Fabricated with Different Lithium Disilicate Ceramic Materials. Int. J. Prosthodont. 2023, 36, 722–729. [Google Scholar] [CrossRef]
- Stefanelli, L.V.; Franchina, A.; Pranno, A.; Pellegrino, G.; Ferri, A.; Pranno, N.; Di Carlo, S.; De Angelis, F. Use of Intraoral Scanners for Full Dental Arches: Could Different Strategies or Overlapping Software Affect Accuracy? Int. J. Environ. Res. Public Health 2021, 18, 9946. [Google Scholar] [CrossRef]
- Fouda, A.M.; Atta, O.; Özcan, M.; Stawarczyk, B.; Glaum, R.; Bourauel, C. An investigation on fatigue, fracture resistance, and color properties of aesthetic CAD/CAM monolithic ceramics. Clin. Oral Investig. 2023, 27, 2653–2665. [Google Scholar] [CrossRef]
- Jurado, C.A.; Afrashtehfar, K.I.; Hyer, J.; Alhotan, A. Effect of sintering on the translucency of CAD-CAM lithium disilicate restorations: A comparative in vitro study. J. Prosthodont. 2023, 32, 861–866. [Google Scholar] [CrossRef]
- Alikhasi, M.; Yousefi, P.; Afrashtehfar, K.I. Smile Design: Mechanical Considerations. Dent. Clin. N. Am. 2022, 66, 477–487. [Google Scholar] [CrossRef]
- Passos, L.; de Vasconcellos, A.B.; Kanashiro, L.; Kina, S. The natural CAD/CAM anterior implant single tooth restoration: A novel digital workflow. J. Esthet. Restor. Dent. 2023, 35, 1194–1204. [Google Scholar] [CrossRef]
- Al-Wahadni, A.; Abu Rashed, B.O.; Al-Fodeh, R.; Tabanjah, A.; Hatamleh, M. Marginal and Internal Gaps, Surface Roughness and Fracture Resistance of Provisional Crowns Fabricated with 3D Printing and Milling Systems. Oper. Dent. 2023, 48, 464–471. [Google Scholar] [CrossRef]
- Young Kim, R.J.; Cho, S.M.; Jung, W.S.; Park, J.M. Trueness and surface characteristics of 3-dimensional printed casts made with different technologies. J. Prosthet. Dent. 2024, 132, 1324.e1–1324.e11. [Google Scholar] [CrossRef] [PubMed]
- Garaicoa, J.; Jurado, C.A.; Afrashtehfar, K.I.; Alhotan, A.; Fischer, N.G. Digital Full-Mouth Reconstruction Assisted by Facial and Intraoral Scanners: A Case Report and Technique Description. Appl. Sci. 2023, 13, 1917. [Google Scholar] [CrossRef]
- Azpiazu-Flores, F.X.; Lee, D.J.; Jurado, C.A.; Nurrohman, H. 3D-Printed Overlay Template for Diagnosis and Planning Complete Arch Implant Prostheses. Healthcare 2023, 11, 1062. [Google Scholar] [CrossRef]
- Khorsandi, D.; Fahimipour, A.; Abasian, P.; Saber, S.S.; Seyedi, M.; Ghanavati, S.; Ahmad, A.; De Stephanis, A.A.; Taghavinezhaddilami, F.; Leonova, A.; et al. 3D and 4D printing in dentistry and maxillofacial surgery: Printing techniques, materials, and applications. Acta Biomater. 2021, 122, 26–49. [Google Scholar] [CrossRef]
- Gracis, S.; Thompson, V.P.; Ferencz, J.L.; Silva, N.R.; Bonfante, E.A. A new classification system for all-ceramic and ceramic-like restorative materials. Int. J. Prosthodont. 2015, 28, 227–235. [Google Scholar] [CrossRef]
- Lupu, I.C.; Tatarciuc, M.S.; Vitalariu, A.M.; Bobu, L.; Diaconu, D.A.; Vasluianu, R.I.; Stamatin, O.; Cretu, C.I.; Dima, A.M. Bonding Strategies for Zirconia Fixed Restorations: A Scoping Review of Surface Treatments, Cementation Protocols, and Long-Term Durability. Biomimetics 2025, 10, 632. [Google Scholar] [CrossRef] [PubMed]
- Al-Johani, H.; Haider, J.; Silikas, N.; Satterthwaite, J. Effect of repeated firing on the topographical, optical, and mechanical properties of fully crystallized lithium silicate-based ceramics. J. Prosthet. Dent. 2024, 131, 741.e1–741.e11. [Google Scholar] [CrossRef]
- Güth, J.F.; Magne, P. Optical integration of CAD/CAM materials. Int. J. Esthet. Dent. 2016, 11, 394–409. [Google Scholar] [PubMed]
- Segundo, Â.R.T.C.; Saraiva, S.; de Castro, C.; Sesma, N.; Bohner, L.; Andretti, F.L.; Coachman, C. CAD-CAM natural restorations-Reproducing nature using a digital workflow. J. Esthet. Restor. Dent. 2023, 35, 993–1000. [Google Scholar] [CrossRef] [PubMed]
- Ates, S.M.; Yesil Duymus, Z. Influence of Tooth Preparation Design on Fitting Accuracy of CAD-CAM Based Restorations. J. Esthet. Restor. Dent. 2016, 28, 238–246. [Google Scholar] [CrossRef] [PubMed]
- Delavy, J.; Lopez, C.; Franchini, L.; Rocca, G.T.; Saratti, C.M. Myocentric relation in an additive esthetic rehabilitation within a fully digital workflow. Int. J. Esthet. Dent. 2024, 19, 74–90. [Google Scholar]
- Badalotti, G.; Lenz, U.; Balen, P.L.; de Oliveira, G.R.; Bacchi, A. A conservative full-mouth ceramic rehabilitation for a severely worn dentition. Int. J. Esthet. Dent. 2023, 18, 366–376. [Google Scholar]
- Sailer, I.; Makarov, N.A.; Thoma, D.S.; Zwahlen, M.; Pjetursson, B.E. All-ceramic or metal-ceramic tooth-supported fixed dental prostheses (FDPs)? A systematic review of the survival and complication rates. Part I: Single crowns (SCs). Dent. Mater. 2015, 31, 603–623. [Google Scholar] [CrossRef]
- Cervino, G.; Fiorillo, L.; Arzukanyan, A.V.; Spagnuolo, G.; Cicciù, M. Dental Restorative Digital Workflow: Digital Smile Design from Aesthetic to Function. Dent. J. 2019, 7, 30. [Google Scholar] [CrossRef]
- Anh, N.V.; Ngoc, V.T.N.; Son, T.M.; Hai, H.V.; Tra, N.T. Comparison of the Marginal and Internal Fit of Ceramic Laminate Veneers Fabricated with Four Different CAM Techniques. Int. J. Prosthodont. 2025, 38, 324–330. [Google Scholar] [CrossRef] [PubMed]
- Shembesh, M.; Ali, A.; Finkelman, M.; Weber, H.P.; Zandparsa, R. An In Vitro Comparison of the Marginal Adaptation Accuracy of CAD/CAM Restorations Using Different Impression Systems. J. Prosthodont. 2017, 26, 581–586. [Google Scholar] [CrossRef] [PubMed]
- Gold, S.A.; Ferracane, J.L.; da Costa, J. Effect of Crystallization Firing on Marginal Gap of CAD/CAM Fabricated Lithium Disilicate Crowns. J. Prosthodont. 2018, 27, 63–66. [Google Scholar] [CrossRef] [PubMed]
- Rokhshad, R.; Tehrani, A.M.; Nahidi, R.; Zarbakhsh, A. Fit of removable partial denture frameworks fabricated from 3D printed patterns versus the conventional method: An in vitro comparison. J. Prosthet. Dent. 2024, 131, 1144–1149. [Google Scholar] [CrossRef]
- Soni, M.; Soni, P.; Soni, P.; Chokhandre, S.; Moni, M.; Gupta, S. The Role of Digital Workflow in Customizing the Prosthetic Solutions: A Literature Review. J. Pharm. Bioallied Sci. 2025, 17, S1095–S1097. [Google Scholar] [CrossRef]
- Fasbinder, D.J. Digital dentistry: Innovation for restorative treatment. Compend. Contin. Educ. Dent. 2010, 31, 2–11; quiz 12. [Google Scholar] [PubMed]
- Brawek, P.K.; Wolfart, S.; Endres, L.; Kirsten, A.; Reich, S. The clinical accuracy of single crowns exclusively fabricated by digital workflow--the comparison of two systems. Clin. Oral Investig. 2013, 17, 2119–2125. [Google Scholar] [CrossRef] [PubMed]
- Zeltner, M.; Sailer, I.; Mühlemann, S.; Özcan, M.; Hämmerle, C.H.; Benic, G.I. Randomized controlled within-subject evaluation of digital and conventional workflows for the fabrication of lithium disilicate single crowns. Part III: Marginal and internal fit. J. Prosthet. Dent. 2017, 117, 354–362. [Google Scholar] [CrossRef] [PubMed]
- Benic, G.I.; Sailer, I.; Zeltner, M.; Gütermann, J.N.; Özcan, M.; Mühlemann, S. Randomized controlled clinical trial of digital and conventional workflows for the fabrication of zirconia-ceramic fixed partial dentures. Part III: Marginal and internal fit. J. Prosthet. Dent. 2019, 121, 426–431. [Google Scholar] [CrossRef] [PubMed]
- Sailer, I.; Mühlemann, S.; Fehmer, V.; Hämmerle, C.H.F.; Benic, G.I. Randomized controlled clinical trial of digital and conventional workflows for the fabrication of zirconia-ceramic fixed partial dentures. Part I: Time efficiency of complete-arch digital scans versus conventional impressions. J. Prosthet. Dent. 2019, 121, 69–75. [Google Scholar] [CrossRef] [PubMed]
- Tabesh, M.; Nejatidanesh, F.; Savabi, G.; Davoudi, A.; Savabi, O.; Mirmohammadi, H. Marginal adaptation of zirconia complete-coverage fixed dental restorations made from digital scans or conventional impressions: A systematic review and meta-analysis. J. Prosthet. Dent. 2021, 125, 603–610. [Google Scholar] [CrossRef] [PubMed]
- Rojas-Rueda, S.; Floriani, F.; Abuhammoud, S.; Mohammed, A.; Afrashtehfar, K.I.; Jurado, C.A. CAD-CAM Complete Dentures Manufactured Using Additive and Subtractive Manufacturing Techniques: A Feasible Clinical Approach for Managing Geriatric Patients With Advanced Residual Ridge Resorption. Case Rep. Dent. 2025, 2025, 9813868. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]




| Example of Commercial Name | Composition of Commercial Names | Advantages |
|---|---|---|
| Tetric CAD (Ivoclar, Schaan, Liechtenstein), Paradigm MZ100 (3M ESPE, St. Paul, MN, USA), Lava Ultimate (3M ESPE), Shofu Block HC (Shofu, Kyoto, Japan), Vita Enamic (Vita) |
|
|
| Ceramics | Example of Commercial Name | Minimal Material Thickness (mm) According to the Manufacture |
|---|---|---|
| Milled feldsphatic ceramics | Vitablocks Mark II (Vita Zahnfabrik, Bad Säckingen, Germany) |
|
| Milled Lithium disilicate ceramics | IPS e.max CAD (Ivoclar Vivadent, Schaan, Liechtenstein) |
|
| Milled zirconia |
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2026 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Alshabib, A.; Berger, J.; Garcia, E.; Jurado, C.A.; Cabral, G.; Baldotto, A.; Riquieri, H.; Alrabiah, M.; Floriani, F. A Comprehensive Digital Workflow for Enhancing Dental Restorations in Severe Structural Wear. Bioengineering 2026, 13, 77. https://doi.org/10.3390/bioengineering13010077
Alshabib A, Berger J, Garcia E, Jurado CA, Cabral G, Baldotto A, Riquieri H, Alrabiah M, Floriani F. A Comprehensive Digital Workflow for Enhancing Dental Restorations in Severe Structural Wear. Bioengineering. 2026; 13(1):77. https://doi.org/10.3390/bioengineering13010077
Chicago/Turabian StyleAlshabib, Abdulrahman, Jake Berger, Edgar Garcia, Carlos A. Jurado, Guilherme Cabral, Adriano Baldotto, Hilton Riquieri, Mohammed Alrabiah, and Franciele Floriani. 2026. "A Comprehensive Digital Workflow for Enhancing Dental Restorations in Severe Structural Wear" Bioengineering 13, no. 1: 77. https://doi.org/10.3390/bioengineering13010077
APA StyleAlshabib, A., Berger, J., Garcia, E., Jurado, C. A., Cabral, G., Baldotto, A., Riquieri, H., Alrabiah, M., & Floriani, F. (2026). A Comprehensive Digital Workflow for Enhancing Dental Restorations in Severe Structural Wear. Bioengineering, 13(1), 77. https://doi.org/10.3390/bioengineering13010077









