Two-Year Clinical Performance of Ultra-Thin No-Prep Veneers from 5Y-TZP Zirconia: A Retrospective Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Characteristics, Participants and Design
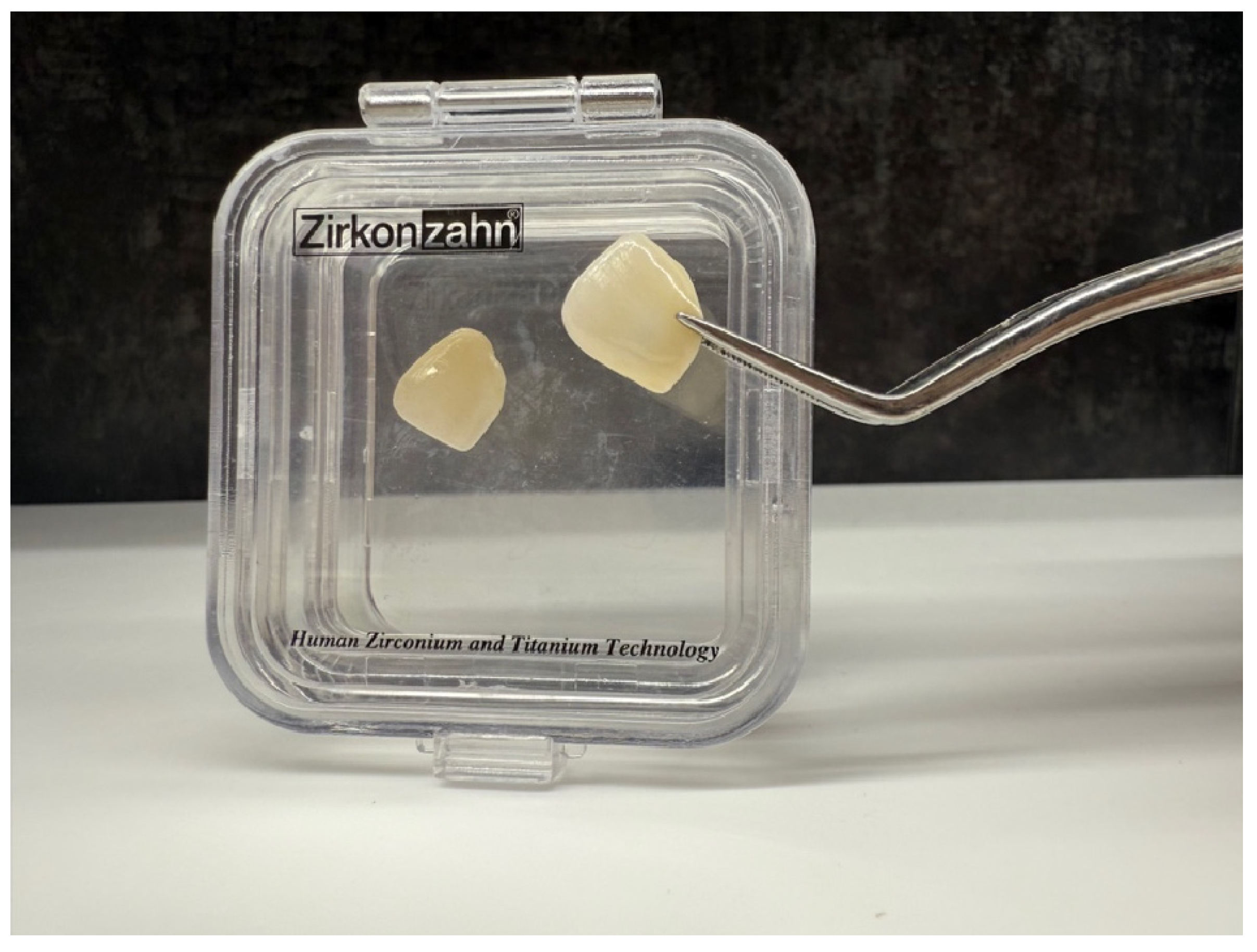
2.2. Pre-Treatment and Laboratory Procedures
2.3. Clinical Try-In and Luting Procedure
2.4. Occlusal Adjustment and Polishing
2.5. Evaluation
3. Results
3.1. Esthetic Parameters
3.2. Functional Parameters
3.3. Biological Parameters
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Alam, B.F.; Najmi, M.A.; Qasim, S.B.; Almulhim, K.S.; Ali, S. A bibliometric analysis of minimally invasive dentistry: A review of the literature from 1994 to 2021. J. Prosthet. Dent. 2023, 130, 179–186. [Google Scholar] [CrossRef]
- Peumans, M.; De Munck, J.; Fieuws, S.; Lambrechts, P.; Vanherle, G.; Van Meerbeek, B. A prospective ten-year clinical trial of porcelain veneers. J. Adhes. Dent. 2004, 6, 65–76. [Google Scholar]
- Chai, S.Y.; Bennani, V.; Aarts, J.M.; Lyons, K. Incisal preparation design for ceramic veneers: A critical review. J. Am. Dent. Assoc. 2018, 149, 25–37. [Google Scholar] [CrossRef]
- Strassler, H.E. Minimally invasive porcelain veneers: Indications for a conservative esthetic dentistry treatment modality. Gen. Dent. 2007, 55, 686–694. [Google Scholar] [PubMed]
- Javeri, D. Considerations for planning esthetic treatment with veneers involving no or minimal preparation. J. Am. Dent. Assoc. 2007, 138, 331–337. [Google Scholar] [CrossRef] [PubMed]
- De Angelis, F.; D’Arcangelo, C.; Angelozzi, R.; Vadini, M. Retrospective clinical evaluation of a no-prep porcelain veneer protocol. J. Prosthet. Dent. 2023, 129, 40–48. [Google Scholar] [CrossRef]
- Koutayas, S.O.; Vagkopoulou, T.; Pelekanos, S.; Koidis, P.; Strub, J.R. Zirconia in dentistry: Part 2. Evidence-based clinical breakthrough. Eur. J. Esthet. Dent. 2009, 4, 348–380. [Google Scholar]
- Sarmento, H.R.; Campos, F.; Sousa, R.S.; Machado, J.P.B.; Souza, R.O.A.; Bottino, M.A.; Özcan, M. Influence of air-particle deposition protocols on the surface topography and adhesion of resin cement to zirconia. Acta Odontol. Scand. 2013, 72, 346–353. [Google Scholar] [CrossRef] [PubMed]
- Alves, M.L.L.; Campos, F.; Bergoli, C.D.; Bottino, M.A.; Özcan, M.; Souza, R.O.A. Effect of adhesive cementation strategies on the bonding of Y-TZP to human dentin. Oper. Dent. 2016, 41, 276–283. [Google Scholar] [CrossRef]
- Queiroz, J.R.C.; Duarte, D.A.; Souza, R.O.A.; Fissmer, S.F.; Massi, M.; Bottino, M.A. Deposition of SiOx thin films on Y-TZP by reactive magnetron sputtering: Influence of plasma parameters on the adhesion properties between Y-TZP and resin cement for application in dental prosthesis. Mater. Res. 2011, 14, 212–216. [Google Scholar] [CrossRef]
- Souza, R.; Barbosa, F.; Araújo, G.; Miyashita, E.; Bottino, M.A.; Melo, R.; Zhang, Y. Ultrathin monolithic zirconia veneers: Reality or future? Report of a clinical case and one-year follow-up. Oper. Dent. 2018, 43, 3–11. [Google Scholar] [CrossRef]
- Yu, F.; Xiang, F.; Zhao, J.; Lin, N.; Sun, Z.; Zheng, Y. Clinical outcomes of self-glazed zirconia veneers produced by 3D gel deposition: A retrospective study. BMC Oral Health 2024, 24, 457. [Google Scholar] [CrossRef]
- Thoma, D.S.; Sailer, I.; Ioannidis, A.; Zwahlen, M.; Makarov, N.; Pjetursson, B.E. A systematic review of the survival and complication rates of resin-bonded fixed dental prostheses after a mean observation period of at least 5 years. Clin. Oral Implants Res. 2017, 28, 1421–1432. [Google Scholar] [CrossRef]
- Kern, M.; Passia, N.; Sasse, M.; Yazigi, C. Ten-year outcome of zirconia ceramic cantilever resin-bonded fixed dental prostheses and the influence of the reasons for missing incisors. J. Dent. 2017, 65, 51–55. [Google Scholar] [CrossRef] [PubMed]
- Soleimani, F.; Jalali, H.; Mostafavi, A.S.; Zeighami, S.; Memarian, M. Retention and clinical performance of zirconia crowns: A comprehensive review. Int. J. Dent. 2020, 2020, 8846534. [Google Scholar] [CrossRef] [PubMed]
- Cho, J.H.; Kim, S.J.; Shim, J.S.; Lee, K.W. Effect of zirconia surface treatment using nitric acid-hydrofluoric acid on the shear bond strengths of resin cements. J. Adv. Prosthodont. 2017, 9, 77–84. [Google Scholar] [CrossRef]
- Anh, N.V.; Son, T.M.; Ngoc, V.T.N.; Ha, P.T.; Hung, D.T.; Nga, M.H.; Tra, N.T. Shear bond strength of MDP-containing light-cured veneer adhesive system to zirconia with different surface preparations. J. Adhes. Sci. Technol. 2024, 38, 2336–2349. [Google Scholar] [CrossRef]
- Marquillier, T.; Doméjean, S.; Le Clerc, J.; Chemla, F.; Gritsch, K.; Maurin, J.C.; Millet, P.; Pérard, M.; Grosgogeat, B.; Dursun, E. The use of FDI criteria in clinical trials on direct dental restorations: A scoping review. J. Dent. 2018, 68, 1–9. [Google Scholar] [CrossRef]
- Śmielak, B.; Armata, O.; Bociong, K. Clinical longevity and trend analysis of 801 ultrathin ceramic veneers: A clinical cohort study. J. Prosthet. Dent. 2024, 131, 1084–1092. [Google Scholar] [CrossRef]
- Nejatidanesh, F.; Savabi, G.; Amjadi, M.; Abbasi, M.; Savabi, O. Five-year clinical outcomes and survival of chairside CAD/CAM ceramic laminate veneers—A retrospective study. J. Prosthodont. Res. 2018, 62, 462–467. [Google Scholar] [CrossRef]
- Sá, T.C.M.; de Carvalho, M.F.F.; de Sá, J.C.M.; Magalhaes, C.S.; Moreira, A.N.; Yamauti, M. Esthetic rehabilitation of anterior teeth with different thicknesses of porcelain laminate veneers: An 8-year follow-up clinical evaluation. Eur. J. Dent. 2018, 12, 590–593. [Google Scholar] [CrossRef][Green Version]
- Breschi, L.; Mazzoni, A.; Ruggeri, A.; Cadenaro, M.; Di Lenarda, R.; De Stefano, D.E. Dental adhesion review: Aging and stability of the bonded interface. Dent. Mater. 2008, 24, 90–101. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, V.A.; Vo, T.N.N.; Tong, M.S.; Nguyen, T.N.T.; Nguyen, T.T. Clinical performance of zirconia veneers bonded with MDP-containing polymeric adhesives: A one-year randomized controlled trial. Polymers 2025, 17, 1213. [Google Scholar] [CrossRef]
- Fawakhiri, H.A.; Abboud, S.; Kanout, S. A three-year controlled clinical trial comparing high-translucency zirconia (cubic zirconia) with lithium disilicate glass ceramic (e.max). Clin. Exp. Dent. Res. 2023, 9, 1078–1088. [Google Scholar] [CrossRef]
- Klein, P.; Spitznagel, F.A.; Zembic, A.; Prott, L.S.; Pieralli, S.; Bongaerts, B.; Metzendorf, M.I.; Langner, R.; Gierthmuehlen, P.C. Survival and complication rates of feldspathic, leucite-reinforced, lithium disilicate and zirconia ceramic laminate veneers: A systematic review and meta-analysis. J. Esthet. Restor. Dent. 2024, 36, 601–619. [Google Scholar] [CrossRef]
- Beier, U.S.; Kapferer, I.; Burtscher, D.; Dumfahrt, H. Clinical performance of porcelain laminate veneers for up to 20 years. Int. J. Prosthodont. 2012, 25, 79–85. [Google Scholar]
- Layton, D.M.; Walton, T.R. The up to 21-year clinical outcome and survival of feldspathic porcelain veneers: Accounting for clustering. Int. J. Prosthodont. 2012, 25, 604–612. [Google Scholar]
- Guess, P.C.; Stappert, C.F. Midterm results of a five-year prospective clinical investigation of extended ceramic veneers. Dent. Mater. 2008, 24, 804–813. [Google Scholar] [CrossRef] [PubMed]
- Ma, L.; Guess, P.C.; Zhang, Y. Load-bearing properties of minimally invasive monolithic lithium disilicate and zirconia occlusal onlays: Finite element and theoretical analyses. Dent. Mater. 2013, 29, 742–751. [Google Scholar] [CrossRef]
- Kim, H.K. Optical and mechanical properties of highly translucent dental zirconia. Materials 2020, 13, 3395. [Google Scholar] [CrossRef] [PubMed]


| Parameter | 1 (Very Good) | 95% CI (Very Good) | 2 (Good) | 3 (Satisfactory) | 4 (Unsatisfactory) | 5 (Poor) |
|---|---|---|---|---|---|---|
| Surface luster | 164 (81.59%) | 75.6–86.4 | 37 (18.41%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Surface color match | 193 (96.02%) | 92.0–98.0 | 8 (3.98%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Marginal color match | 194 (96.52%) | 92.6–98.4 | 7 (3.48%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Color and translucency stability | 160 (79.60%) | 73.5–84.7 | 41 (20.40%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Anatomical form | 201 (100%) | 98.1–100.0 | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Parameter | 1 (Very Good) | 95% CI (Very Good) | 2 (Good) | 3 (Satisfactory) | 4 (Unsatisfactory) | 5 (Poor) |
|---|---|---|---|---|---|---|
| Fractures (marginal/other surfaces) | 194 (96.52%) | 92.6–98.4 | 5 (2.49%) | 2 (0.99%) | 0 (0%) | 0 (0%) |
| Marginal adaptation | 169 (84.08%) | 78.3–88.6 | 31 (15.42%) | 1 (0.50%) | 0 (0%) | 0 (0%) |
| Occlusal contour and wear | 201 (100%) | 98.1–100.0 | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Proximal contacts | 201 (100%) | 98.1–100.0 | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Patient’s view | 201 (100%) | 98.1–100.0 | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Parameter | 1 (Very Good) | 95% CI (Very Good) | 2 (Good) | 3 (Satisfactory) | 4 (Unsatisfactory) | 5 (Poor) |
|---|---|---|---|---|---|---|
| Vitality/pulp and hypersensitivity | 198 (98.51%) | 95.5–99.5 | 3 (1.49%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Caries/non-carious lesions | 201 (100%) | 98.1–100.0 | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Fractures of tooth | 201 (100%) | 98.1–100.0 | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Periodontal response | 103 (51.24%) | 44.4–58.0 | 78 (38.81%) | 14 (6.97%) | 6 (2.98%) | 0 (0%) |
| Oral mucosa | 201 (100%) | 98.1–100.0 | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| General oral health | 201 (100%) | 98.1–100.0 | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Taraszkiewicz-Sulik, K.; Wiśniewski, P.; Cywoniuk, E.; Sierpińska, T. Two-Year Clinical Performance of Ultra-Thin No-Prep Veneers from 5Y-TZP Zirconia: A Retrospective Study. Bioengineering 2025, 12, 976. https://doi.org/10.3390/bioengineering12090976
Taraszkiewicz-Sulik K, Wiśniewski P, Cywoniuk E, Sierpińska T. Two-Year Clinical Performance of Ultra-Thin No-Prep Veneers from 5Y-TZP Zirconia: A Retrospective Study. Bioengineering. 2025; 12(9):976. https://doi.org/10.3390/bioengineering12090976
Chicago/Turabian StyleTaraszkiewicz-Sulik, Katarzyna, Patryk Wiśniewski, Edyta Cywoniuk, and Teresa Sierpińska. 2025. "Two-Year Clinical Performance of Ultra-Thin No-Prep Veneers from 5Y-TZP Zirconia: A Retrospective Study" Bioengineering 12, no. 9: 976. https://doi.org/10.3390/bioengineering12090976
APA StyleTaraszkiewicz-Sulik, K., Wiśniewski, P., Cywoniuk, E., & Sierpińska, T. (2025). Two-Year Clinical Performance of Ultra-Thin No-Prep Veneers from 5Y-TZP Zirconia: A Retrospective Study. Bioengineering, 12(9), 976. https://doi.org/10.3390/bioengineering12090976






