Controlled Mandibular Repositioning: A Novel Approach for Treatment of TMDs
Abstract
1. Introduction
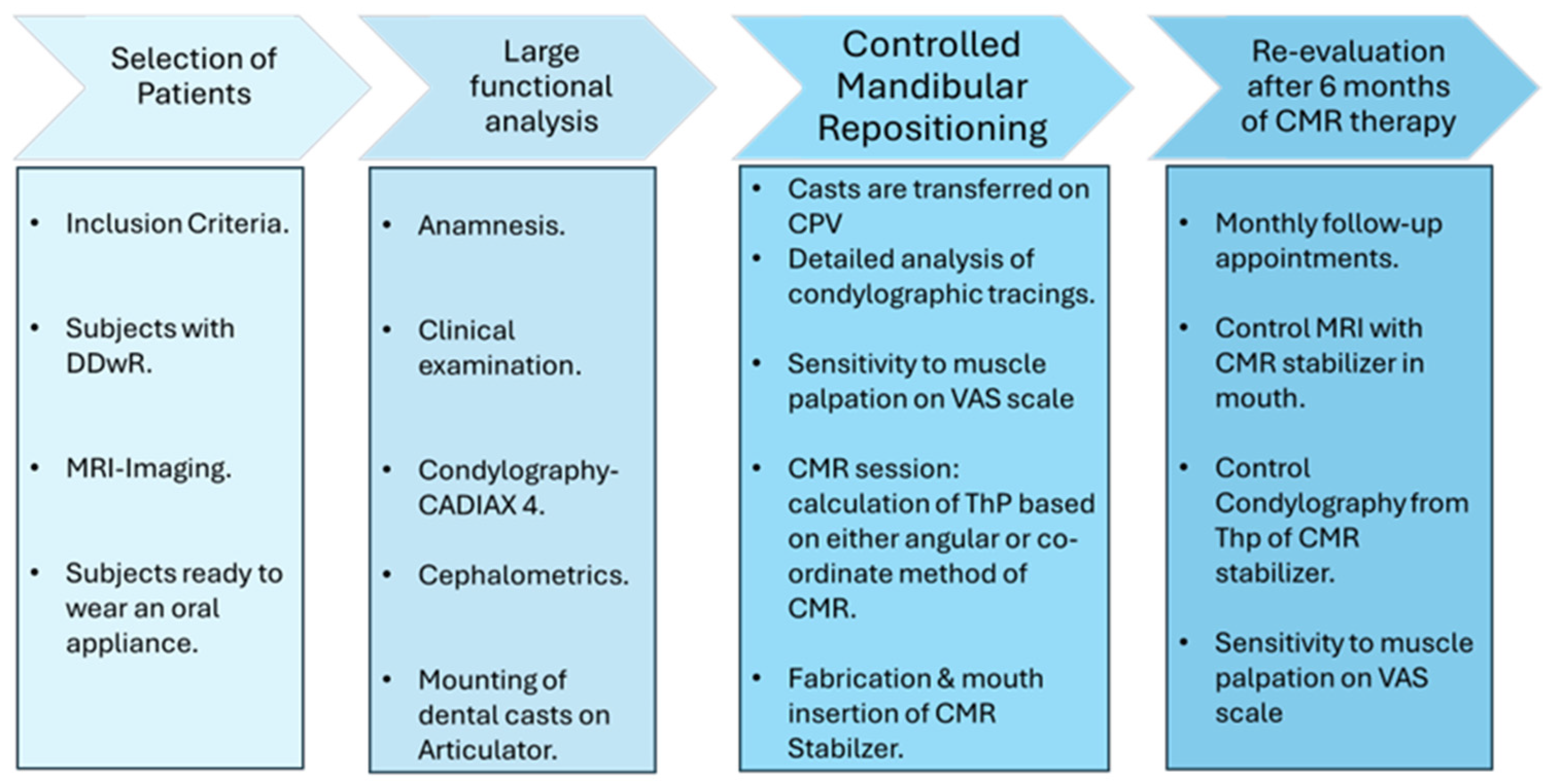
2. Materials and Methods
2.1. Selection of Patients
2.2. Condylography: CADIAX® 4 (Computerized Condylography) (Gamma-Dental Klosterneuburg, Austria)
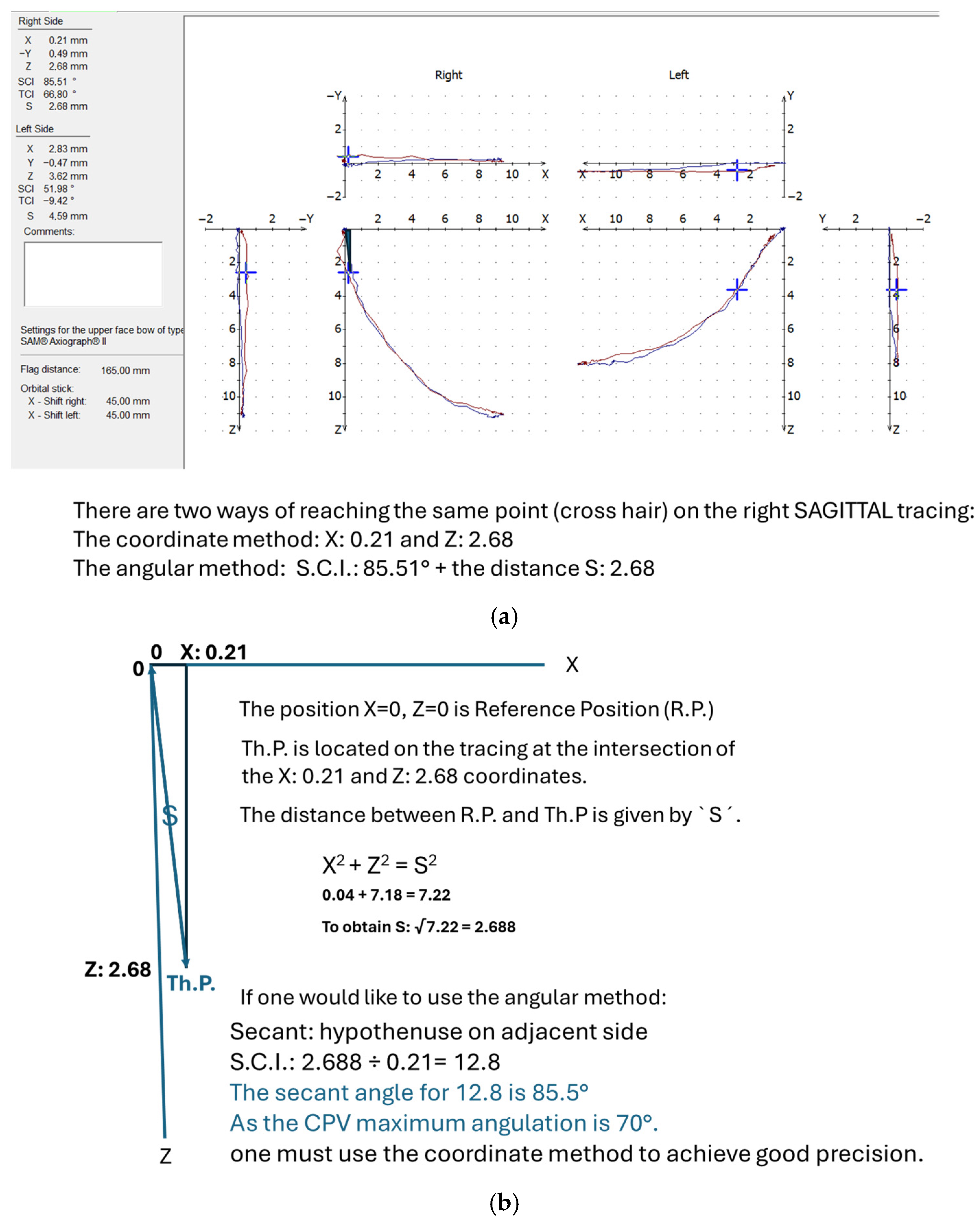
2.3. Controlled Mandibular Repositioning Method: Condylar Position Variator (CPV) (Gamma-Dental Klosterneuburg, Austria)
2.4. Controlled Mandibular Repositioning Method
3. Results
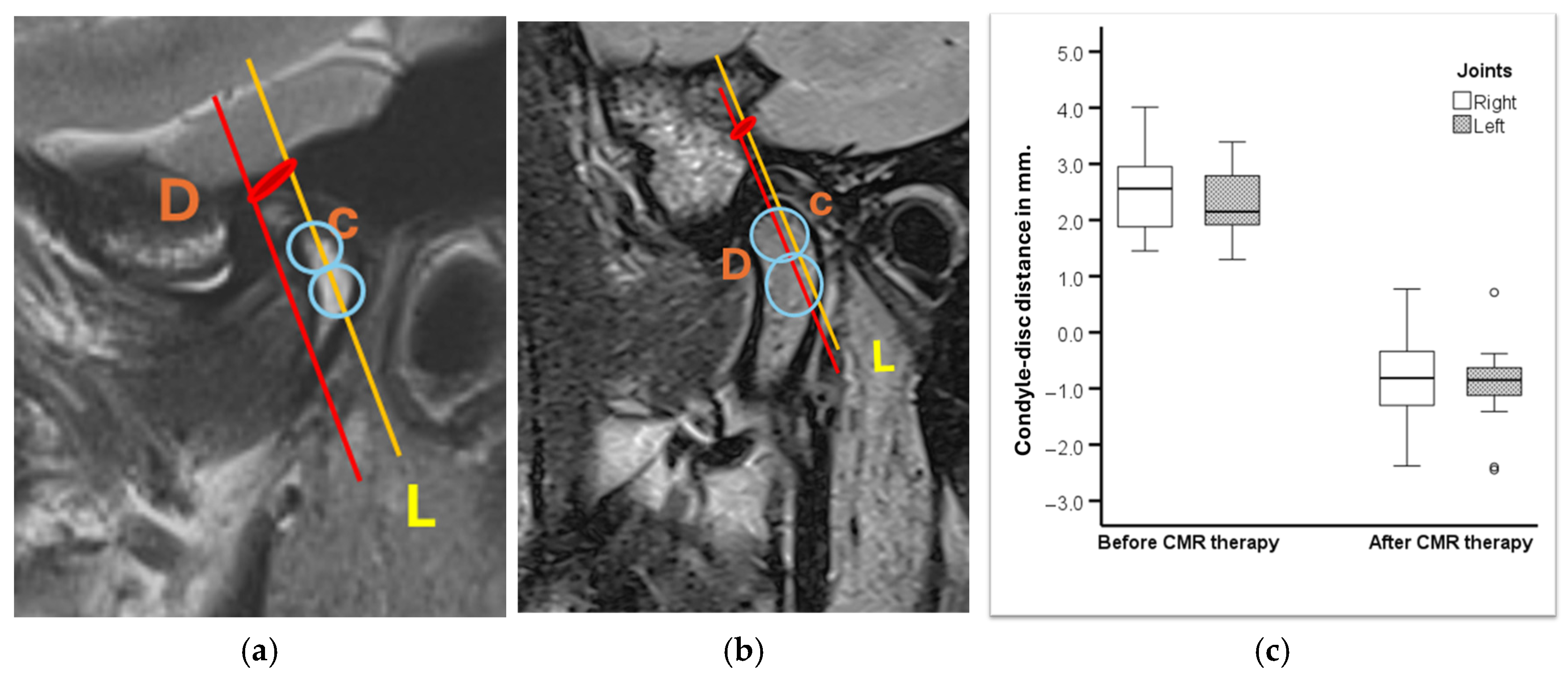
3.1. MRI Evaluation of Therapeutic Position (Figure 8)
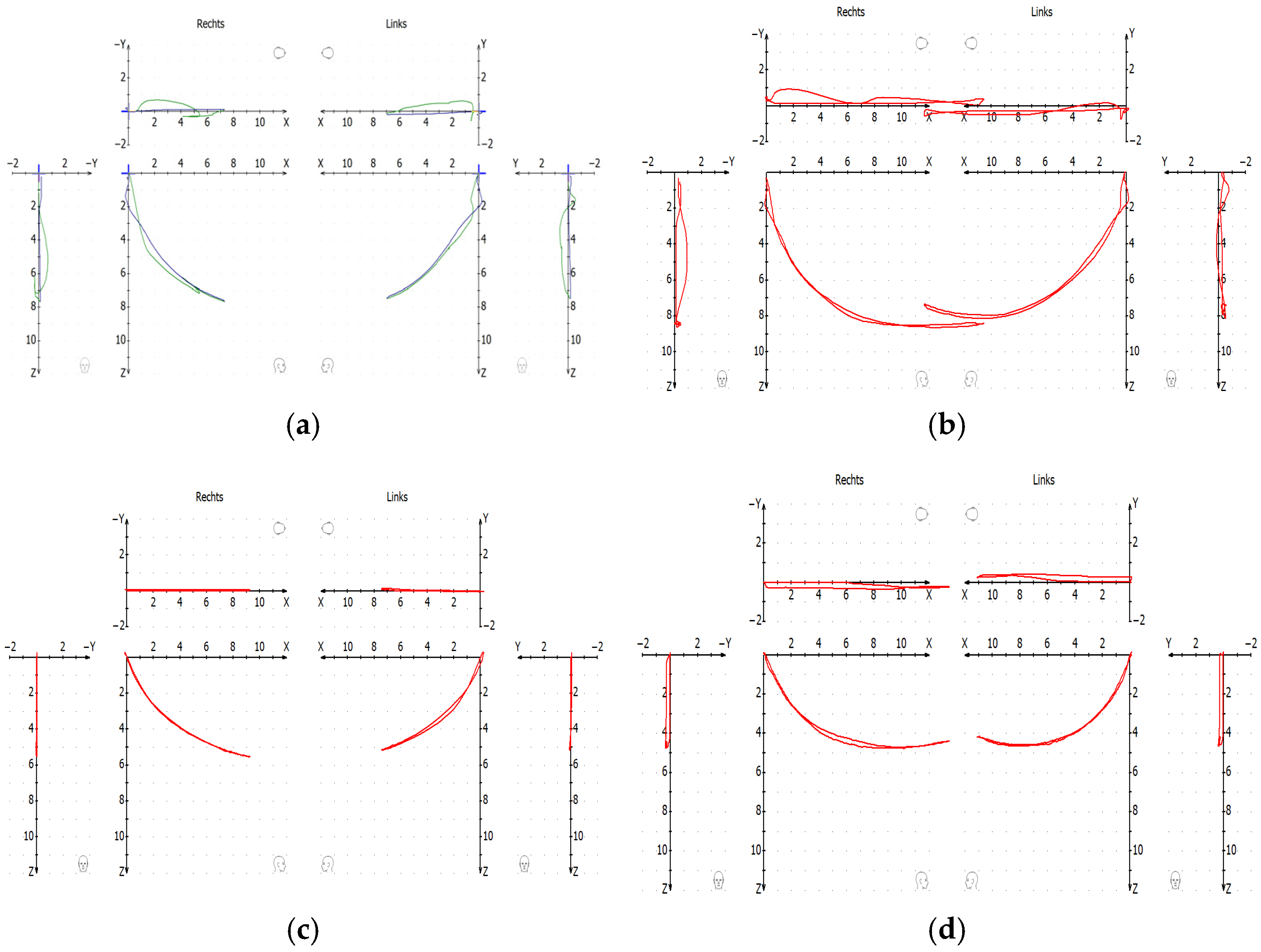
3.2. Evaluation with Control Condylography
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| TMDs | Temporomandibular joint disorders |
| DDwR | Disc displacement with reduction |
| ARS | Anterior Repositioning Splint |
| Th.P | Therapeutic Position |
| CMR | Controlled Mandibular Repositioning |
| CPV | Condylar Position Variator |
| Rp | Reference Position |
| ICP | Intercuspal Position |
| SCI | Sagittal Condylar Inclination |
| OPG | Orthopantogram |
| CBCT | Cone Beam Computer Tomography |
| CADIAX | Computerized Axiography/Condylography |
References
- Schiffman, E.; Ohrbach, R.; Truelove, E.; Look, J.; Anderson, G.; Goulet, J.-P.; List, T.; Svensson, P.; Gonzalez, Y.; Lobbezoo, F.; et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: Recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group. J. Oral Facial Pain Headache 2014, 28, 6–27. [Google Scholar] [CrossRef]
- Zieliński, G.; Pająk-Zielińska, B.; Ginszt, M. A Meta-Analysis of the Global Prevalence of Temporomandibular Disorders. J. Clin. Med. 2024, 13, 1365. [Google Scholar] [CrossRef]
- Minervini, G.; Franco, R.; Marrapodi, M.M.; Fiorillo, L.; Cervino, G.; Cicciù, M. Prevalence of temporomandibular disorders in children and adolescents evaluated with Diagnostic Criteria for Temporomandibular Disorders: A systematic review with meta-analysis. J. Oral Rehabil. 2023, 50, 522–530. [Google Scholar] [CrossRef]
- Iodice, G.; Cimino, R.; Vollaro, S.; Lobbezoo, F.; Michelotti, A. Prevalence of temporomandibular disorder pain, jaw noises and oral behaviours in an adult Italian population sample. J. Oral Rehabil. 2019, 46, 691–698. [Google Scholar] [CrossRef]
- De Godoi Gonçalves, D.A.; Dal Fabbro, A.L.; Campos, J.A.D.B.; Bigal, M.E.; Speciali, J.G. Symptoms of temporomandibular disorders in the population: An epidemiological study. J. Orofac. Pain 2010, 24, 270–278. [Google Scholar]
- Naeije, M.; Te Veldhuis, A.H.; Te Veldhuis, E.C.; Visscher, C.M.; Lobbezoo, F. Disc displacement within the human temporomandibular joint: A systematic review of a ‘noisy annoyance’. J. Oral Rehabil. 2013, 40, 139–158. [Google Scholar] [CrossRef] [PubMed]
- Bhargava, D.; Farías, C.C.; García, I.A.; Mercuri, L.G.; Bergman, S.; Pogrel, M.A.; Sidebottom, A.J.; Srouji, S.; Şentürk, M.F.; Elavenil, P.; et al. Recommendations on the use of oral orthotic occlusal appliance therapy for temporomandibular joint disorders: Current evidence and clinical practice. J. Maxillofac. Oral Surg. 2023, 22, 579–589. [Google Scholar] [CrossRef] [PubMed]
- Al-Moraissi, E.A.; Wolford, L.M.; Ellis, E.; Neff, A. The hierarchy of different treatments for arthrogenous temporomandibular disorders: A network meta-analysis of randomized clinical trials. J. Craniomaxillofac. Surg. 2020, 48, 9–23. [Google Scholar] [CrossRef] [PubMed]
- Albagieh, H.; Alomran, I.; Binakresh, A.; Alhatarisha, N.; Almeteb, M.; Khalaf, Y.; Alqublan, A.; Alqahatany, M. Occlusal splints-types and effectiveness in temporomandibular disorder management. Saudi Dent. J. 2023, 35, 70–79. [Google Scholar] [CrossRef]
- Crout, D.K. Anatomy of an occlusal splint. Gen. Dent. 2017, 65, 52–59. [Google Scholar] [PubMed]
- Maheshwari, K.; Srinivasan, R.; Singh, B.P.; Tiwari, B.; Kirubakaran, R. Effectiveness of anterior repositioning splint versus other occlusal splints in the management of temporomandibular joint disc displacement with reduction: A meta-analysis. J. Indian Prosthodont. Soc. 2024, 24, 15–24. [Google Scholar] [CrossRef]
- Fayed, M.M.S.; El-Mangoury, N.H.; El-Bokle, D.N.; Belal, A.I. Occlusal splint therapy and magnetic resonance imaging. World J. Orthod. 2004, 5, 133–140. [Google Scholar]
- Huang, I.-Y.; Wu, J.-H.; Kao, Y.-H.; Chen, C.-M.; Chen, C.-M.; Yang, Y.-H. Splint therapy for disc displacement with reduction of the temporomandibular joint. part I: Modified mandibular splint therapy. Kaohsiung J. Med. Sci. 2011, 27, 323–329. [Google Scholar] [CrossRef] [PubMed]
- Clark, G.T. A critical evaluation of orthopedic interocclusal appliance therapy: Design, theory, and overall effectiveness. J. Am. Dent. Assoc. 1984, 108, 359–364. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.-N.; Cui, S.-J.; Zhou, Y.-H.; Wang, X.-D. An Overview of Anterior Repositioning Splint Therapy for Disc Displacement-related Temporomandibular Disorders. Curr. Med. Sci. 2021, 41, 626–634. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Fu, K.; Li, Y.; Zhang, Z. Positional changes of temporomandibular joint disk and condyle with insertion of anterior repositioning splint. Hua Xi Kou Qiang Yi Xue Za Zhi 2009, 27, 408–412. [Google Scholar]
- Shen, P.; Chen, X.; Xie, Q.; Zhang, S.; Yang, C. Assessment of occlusal appliance for the reposition of temporomandibular joint anterior disc displacement with reduction. J. Craniofac. Surg. 2019, 30, 1140–1143. [Google Scholar] [CrossRef]
- Li, H.; Shen, D.; Chen, Z.; Li, J. Step-back anterior repositioning splint retraction for temporomandibular joint disc displacement with reduction in adult patients. J. Oral Rehabil. 2023, 50, 965–971. [Google Scholar] [CrossRef]
- Lassmann, Ł.; Nowak, Z.; Żółtowska, A. Sagittal condylar guidance angle measurement methods: A systematic review. J. Prosthet. Dent. 2024, 132, 81–92. [Google Scholar] [CrossRef]
- Prasad, K.D.; Shetty, M.; Chandy, B.K. Evaluation of condylar inclination of dentulous subjects determined by axiograph and to compare with manual programming of articulators using protrusive interocclusal record. Contemp. Clin. Dent. 2015, 6, 371–374. [Google Scholar] [CrossRef]
- Peng, T.; Yang, Z.; Ma, T.; Zhang, M.; Ren, G. Comparative evaluation of the volume of occlusal adjustment of repositioning occlusal devices designed by using an average value digital articulator and the jaw movement analyzer. J. Prosthet. Dent. 2025, 133, 1268–1274. [Google Scholar] [CrossRef]
- Aljohani, A.O.; Sghaireen, M.G.; Abbas, M.; Alzarea, B.K.; Srivastava, K.C.; Shrivastava, D.; Issrani, R.; Mathew, M.; Alsharari, A.H.L.; Alsharari, M.A.D.; et al. Comparative Evaluation of Condylar Guidance Angles Measured Using Arcon and Non-Arcon Articulators and Panoramic Radiographs—A Systematic Review and Meta-Analysis. Life 2023, 13, 1352. [Google Scholar] [CrossRef] [PubMed]
- Gu, X.; Hu, T.; Zhang, Z.; He, F.; Shi, J.; Yang, H. Comparison of the accuracy of an ultrasonic-based jaw tracking device with conventional electronic tracking device. J. Adv. Prosthodont. 2025, 17, 47–58. [Google Scholar] [CrossRef]
- Celar, A.G.; Tamaki, K. Accuracy of recording horizontal condylar inclination and Bennett angle with the Cadiax compact. J. Oral Rehabil. 2002, 29, 1076–1081. [Google Scholar] [CrossRef]
- Schmid-Schwap, M.; Briedl, J.G.; Robinson, S.; Piehslinger, E. Correlation between disk morphology on MRI and time curves using electronic axiography. Cranio 2005, 23, 22–29. [Google Scholar] [CrossRef]
- Wagner, A.; Seemann, R.; Schicho, K.; Ewers, R.; Piehslinger, E. A comparative analysis of optical and conventional axiography for the analysis of temporomandibular joint movements. J. Prosthet. Dent. 2003, 90, 503–509. [Google Scholar] [CrossRef]
- Gsellmann, B.; Schmid-Schwap, M.; Piehslinger, E.; Slavicek, R. Lengths of condylar pathways measured with computerized axiography (CADIAX) and occlusal index in patients and volunteers. J. Oral Rehabil. 1998, 25, 146–152. [Google Scholar] [CrossRef]
- Piehslinger, E.; Čelar, A.G.; Čelar, R.M.; Slavicek, R. Computerized axiography: Principles and methods. CRANIO® 1991, 9, 344–355. [Google Scholar] [CrossRef]
- Zokaris, N.; Greven, M.; Tzakis, M.; Psarras, V. Computerized Axiographic Findings in a Cohort of Migraine Patients: A Cross-Sectional Study. Dent. J. 2024, 12, 204. [Google Scholar] [CrossRef] [PubMed]
- Ahlers, M.O.; Petersen, T.; Katzer, L.; Jakstat, H.A.; Roehl, J.C.; Türp, J.C. Condylar motion analysis: A controlled, blinded clinical study on the interindividual reproducibility of standardized evaluation of computer-recorded condylar movements. Sci. Rep. 2023, 13, 11721. [Google Scholar] [CrossRef] [PubMed]
- Schierz, O.; Klinger, N.; Schön, G.; Reissmann, D.R. The reliability of computerized condylar path angle assessment. Int. J. Comput. Dent. 2014, 17, 35–51. [Google Scholar] [PubMed]
- Al-Thobity, A.M.; Alkhaltham, N.; Aldhafiri, R.; Almasoud, N.N.; A Al-Harbi, F.; Khan, S.Q.; Gad, M.M. Effect of occlusal splint therapy on condylar movements recorded using an electronic pantograph: A prospective clinical study. J. Int. Soc. Prev. Community Dent. 2022, 12, 532–539. [Google Scholar] [CrossRef] [PubMed]
- Singh, D.; Landry, A.; Schmid-Schwap, M.; Piehslinger, E.; Gahleitner, A.; Chen, J.; Rausch-Fan, X. Clinical and MRI-Based Assessment of Patients with Temporomandibular Disorders Treated by Controlled Mandibular Repositioning. Diagnostics 2024, 14, 572. [Google Scholar] [CrossRef] [PubMed]
- Piehslinger, E.; Bigenzahn, W.; Celar, A.; Slavicek, R. The effect of occlusal splint therapy on different curve parameters of axiographic TMJ tracings. Cranio 1995, 13, 35–41. [Google Scholar] [CrossRef]
- Slavicek, R. The Masticatory Organ; Gamma Medizinisch-Wissenschaftliche Fortbildungs-GmbH: Klosterneuburg, Austria, 2002. [Google Scholar]
- Zhang, Q.; Ye, Z.; Wu, Y.; Zhu, Y.; Liu, J.; Yang, W.; Ye, C.; Han, S.L.R.; Wang, J.; Xiong, X. Nonlinear Relationship between Temporomandibular Joint Disc Displacement Distance and Disc Length: A Magnetic Resonance Imaging Analysis. J. Clin. Med. 2022, 11, 7160. [Google Scholar] [CrossRef]
- Ahangari, A.H.; Torabi, K.; Pour, S.R.; Ghodsi, S. Evaluation of the Cadiax Compact® II accuracy in recording preadjusted condylar inclinations on fully adjustable articulator. J. Contemp. Dent. Pract. 2012, 13, 504–508. [Google Scholar] [CrossRef]
- Bernhardt, O.; Küppers, N.; Rosin, M.; Meyer, G. Comparative tests of arbitrary and kinematic transverse horizontal axis recordings of mandibular movements. J. Prosthet. Dent. 2003, 89, 175–179. [Google Scholar] [CrossRef]
- Sadat-Khonsari, R.; Fenske, C.; Kahl-Nieke, B.; Kirsch, I.; Jüde, H.D. Mandibular instantaneous centers of rotation in patients with and without temporomandibular dysfunction. J. Orofac. Orthop. 2003, 64, 256–264. [Google Scholar] [CrossRef]
- Talmaceanu, D.; Bolog, N.; Leucuta, D.; Tig, I.A.; Buduru, S. Diagnostic use of computerized axiography in TMJ disc displacements. Exp. Ther. Med. 2022, 23, 213. [Google Scholar] [CrossRef]
- Kuzmanovic Pficer, K.; Dodic, S.; Lazic, V.; Trajkovic, G.; Milic, N.; Milicic, B. Occlusal stabilization splint for patients with temporomandibular disorders: Meta-analysis of short and long term effects. PLoS ONE 2017, 12, e0171296. [Google Scholar] [CrossRef]
- Zhang, L.; Xu, L.; Wu, D.; Yu, C.; Fan, S.; Cai, B. Effectiveness of exercise therapy versus occlusal splint therapy for the treatment of painful temporomandibular disorders: A systematic review and meta-analysis. Ann. Palliat. Med. 2021, 10, 6122–6132. [Google Scholar] [CrossRef] [PubMed]
- Pihut, M.; Gorecka, M.; Ceranowicz, P.; Wieckiewicz, M. The Efficiency of Anterior Repositioning Splints in the Management of Pain Related to Temporomandibular Joint Disc Displacement with Reduction. Pain Res. Manag. 2018, 2018, 9089286. [Google Scholar] [CrossRef] [PubMed]
- Ma, Z.; Xie, Q.; Yang, C.; Zhang, S.; Shen, Y.; Abdelrehem, A. Can anterior repositioning splint effectively treat temporomandibular joint disc displacement? Sci. Rep. 2019, 9, 534. [Google Scholar] [CrossRef]
- Okeson, J.P. Long-term treatment of disk-interference disorders of the temporomandibular joint with anterior repositioning occlusal splints. J. Prosthet. Dent. 1988, 60, 611–616. [Google Scholar] [CrossRef] [PubMed]





| No. Patients | Joints with ADDwR | Females | Males | Age in Years Mean ± SD Range | Excluded Joints |
|---|---|---|---|---|---|
| 20 | 37 | 18 | 2 | 28.7 ± 6.4 (18–41) | 3 * |
| Before | After | t | p | |||
|---|---|---|---|---|---|---|
| Mean ± SD | Min–Max | Mean ± SD | Min–Max | |||
| Right (n = 18) | 2.50 ± 0.67 | 1.45–4.01 | −0.82 ± 0.71 | −2.38–0.77 | −13.533 | <0.001 |
| Left (n = 19) | 2.33 ± 0.58 | 1.30–3.39 | −0.94 ± 0.70 | −2.45–0.71 | −16.136 | <0.001 |
| Correlation | r | p | n | |
|---|---|---|---|---|
| MRI with Th.P in CPV (s) | all Joints | 0.361 | 0.028 | 37 |
| MRI with Th.P in CPV (s) | <70° | 0.419 | 0.027 | 28 |
| MRI with Th.P (z) in CPV | >70° | −0.732 | 0.025 | 9 |
| MRI with Th.P (x) in CPV | >70° | −0.573 | 0.107 | 9 |
| MRI with Th.P CPV (s) (n = 37) | Percentage % | r | p | n |
|---|---|---|---|---|
| SCI < 70° (angular method) | 75.6% | 0.419 | 0.027 | 28 |
| SCI > 70° (coordinate method) | 24.3% | −0.750 | 0.020 | 9 |
| Movements | Difference Between Excursive and Incursive Tracings Before CMR Treatment | Difference Between Excursive and Incursive Tracings After CMR Treatment | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Units: | 1 mm | 2 mm | 3 mm | 4 mm | 5 mm | 6 mm | 7 mm | 8 mm | 1 mm | 2 mm | 3 mm | 4 mm | 5 mm | 6 mm | 7 mm | 8 mm | |
| P/R Left | MEAN | 15.4 | 9.1 | 5.6 | 1.8 | 0.14 | 0.38 | −0.4 | −0.60 | 3.98 | 4.6 | 2.32 | 1.6 | 1.24 | 0.42 | 0.38 | 0.37 |
| STD | 11.40 | 7.83 | 8.6 | 3.2 | 3.03 | 2.7 | 2.82 | 2.873 | 13.7 | 3.48 | 2.95 | 2.06 | 1.89 | 1.35 | 1.59 | 1.44 | |
| P/R Right | MEAN | 15.84 | 7.3 | 1.2 | 1.9 | 1.6 | 0.95 | 0.54 | 0.278 | 7.1 | 3.04 | 1.98 | 1.49 | 0.96 | 0.67 | 1.19 | 1.44 |
| STD | 11.6 | 6.3 | 7.6 | 3.2 | 2.3 | 2.05 | 1.64 | 0.946 | 4.46 | 2.50 | 2.56 | 2.09 | 1.58 | 1.59 | 1.71 | 1.88 | |
| O/C left | MEAN | 12.06 | 7.2 | 3.1 | 1.7 | 0.4 | −0.25 | −0.50 | −0.24 | 15.54 | 17.75 | −0.10 | −0.37 | −0.55 | −1.7 | −0.09 | −0.52 |
| STD | 10.8 | 5.9 | 4.5 | 4.0 | 3.4 | 3.1 | 2.7 | 2.61 | 53.5 | 55.40 | 3.2 | 3.1 | 2.83 | 3.61 | 2.25 | 2.86 | |
| O/C right | MEAN | 5.84 | 8.7 | 3.5 | 1.2 | −0.35 | −0.6 | −0.85 | −0.56 | 3.39 | 1.2 | 0.16 | 0 | −0.10 | 0.32 | 0.13 | −0.27 |
| STD | 40.4 | 8.5 | 6.8 | 5.5 | 4.69 | 3.4 | 2.99 | 2.3 | 8.65 | 4.3 | 2.82 | 2.4 | 2.15 | 1.79 | 1.76 | 1.3 | |
| N = 20 Subjects | Protrusion–Retrusion Left | Protrusion–Retrusion Right | Open–close Left | Open–close Right |
|---|---|---|---|---|
| mm | Significance | Significance | Significance | Significance |
| 1 mm | * <0.01 | * <0.01 | * <0.01 | n.s. |
| 2 mm | n.s. | * <0.05 | * <0.01 | * <0.01 |
| 3 mm | n.s. | n.s. | * <0.01 | * <0.05 |
| 4 mm | n.s. | n.s. | * <0.05 | n.s. |
| 5 mm | n.s. | n.s. | n.s. | n.s. |
| 6 mm | n.s. | n.s. | * <0.05 | n.s. |
| 7 mm | n.s. | n.s. | n.s. | n.s. |
| 8 mm | n.s. | n.s. | n.s. | n.s. |
| 9 mm | n.s. | n.s. | n.s. | n.s. |
| 10 mm | n.s. | n.s. | n.s. | n.s. |
| Muscles | Left | Right | ||||
|---|---|---|---|---|---|---|
| RP | ICP | CMR | RP | ICP | CMR | |
| TubMaxillae | 3.5 ± 2.3 | 3.3 ± 2.2 | 0.1 ± 0.2 | 4.1 ± 2.4 | 4.3 ± 3.0 | 0.1 ± 0.3 |
| MedPterygoid | 3.4 ± 3.0 | 3.5 ± 3.3 | 0.3 ± 0.5 | 3.1 ± 2.9 | 3.4 ± 2.9 | 0 ± 0 |
| Mylohyoid | 0.8 ± 1.7 | 0.5 ± 1.1 | 0 ± 0 | 0.4 ± 0.8 | 0.3 ± 0.7 | 0 ± 0 |
| SupMasseter | 2.1 ± 2.2 | 2.2 ± 1.9 | 0.1 ± 0.5 | 0.8 ± 1.0 | 1.5 ± 2 | 0 ± 0 |
| TempTendon | 2.2 ± 2.0 | 2.4 ± 2.1 | 0 ± 0 | 1.5 ± 1.3 | 2.2 ± 2.2 | 0 ± 0 |
| Digastric | 0.6 ± 1.0 | 0.7 ± 1.2 | 0 ± 0 | 0.4 ± 0.8 | 1.2 ± 1.6 | 0 ± 0 |
| Lateral Pole | 0.3 ± 0.8 | 0.6 ± 1.2 | 0 ± 0 | 0.9 ± 1.7 | 0.6 ± 0.9 | 0 ± 0 |
| DeepMasseter | 1.3 ± 1.5 | 1.7 ± 1.8 | 0.1 ± 0.3 | 1.3 ± 1.4 | 1.6 ± 1.5 | 0.1 ± 0.3 |
| TMLigament | 1.5 ± 1.6 | 2.2 ± 2.1 | 0.2 ± 0.6 | 1.8 ± 1.8 | 2.1 ± 2 | 0.1 ± 0.5 |
| RJSpace | 1.4 ± 1.3 | 1.0 ± 1.6 | 0.1 ± 0.5 | 1.1 ± 1.4 | 1.1 ± 1.7 | 0 ± 0 |
| OmoHyoid | 0.9 ± 1.5 | 1.2 ± 1.9 | 0.3 ± 0.7 | 1.0 ± 1.6 | 0.7 ± 1.5 | 0.3 ± 0.7 |
| U.Trapezius | 1.4 ± 2.0 | 2.3 ± 2.4 | 0.2 ± 0.5 | 1.8 ± 2.3 | 2.3 ± 2.4 | 0.2 ± 0.5 |
| PostTemporalis | 0.8 ± 1.7 | 1.1 ± 1.5 | 0.1 ± 0.5 | 1.0 ± 1.4 | 1.0 ± 1.6 | 0.1 ± 0.5 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Singh, D.; Landry, A.; Schmid-Schwap, M.; Piehslinger, E.; Gahleitner, A.; Holzinger, T.; Wang, Y.; Chen, J.; Rausch-Fan, X. Controlled Mandibular Repositioning: A Novel Approach for Treatment of TMDs. Bioengineering 2025, 12, 865. https://doi.org/10.3390/bioengineering12080865
Singh D, Landry A, Schmid-Schwap M, Piehslinger E, Gahleitner A, Holzinger T, Wang Y, Chen J, Rausch-Fan X. Controlled Mandibular Repositioning: A Novel Approach for Treatment of TMDs. Bioengineering. 2025; 12(8):865. https://doi.org/10.3390/bioengineering12080865
Chicago/Turabian StyleSingh, Diwakar, Alain Landry, Martina Schmid-Schwap, Eva Piehslinger, André Gahleitner, Thomas Holzinger, Yilin Wang, Jiang Chen, and Xiaohui Rausch-Fan. 2025. "Controlled Mandibular Repositioning: A Novel Approach for Treatment of TMDs" Bioengineering 12, no. 8: 865. https://doi.org/10.3390/bioengineering12080865
APA StyleSingh, D., Landry, A., Schmid-Schwap, M., Piehslinger, E., Gahleitner, A., Holzinger, T., Wang, Y., Chen, J., & Rausch-Fan, X. (2025). Controlled Mandibular Repositioning: A Novel Approach for Treatment of TMDs. Bioengineering, 12(8), 865. https://doi.org/10.3390/bioengineering12080865






