A Standardized Protocol for Analyzing Masticatory Muscle Activity at Different Levels of Mouth Opening Using Electromagnetic Articulography and Surface Electromyography: A Proof-of-Concept Study
Abstract
1. Introduction
2. Materials and Methods
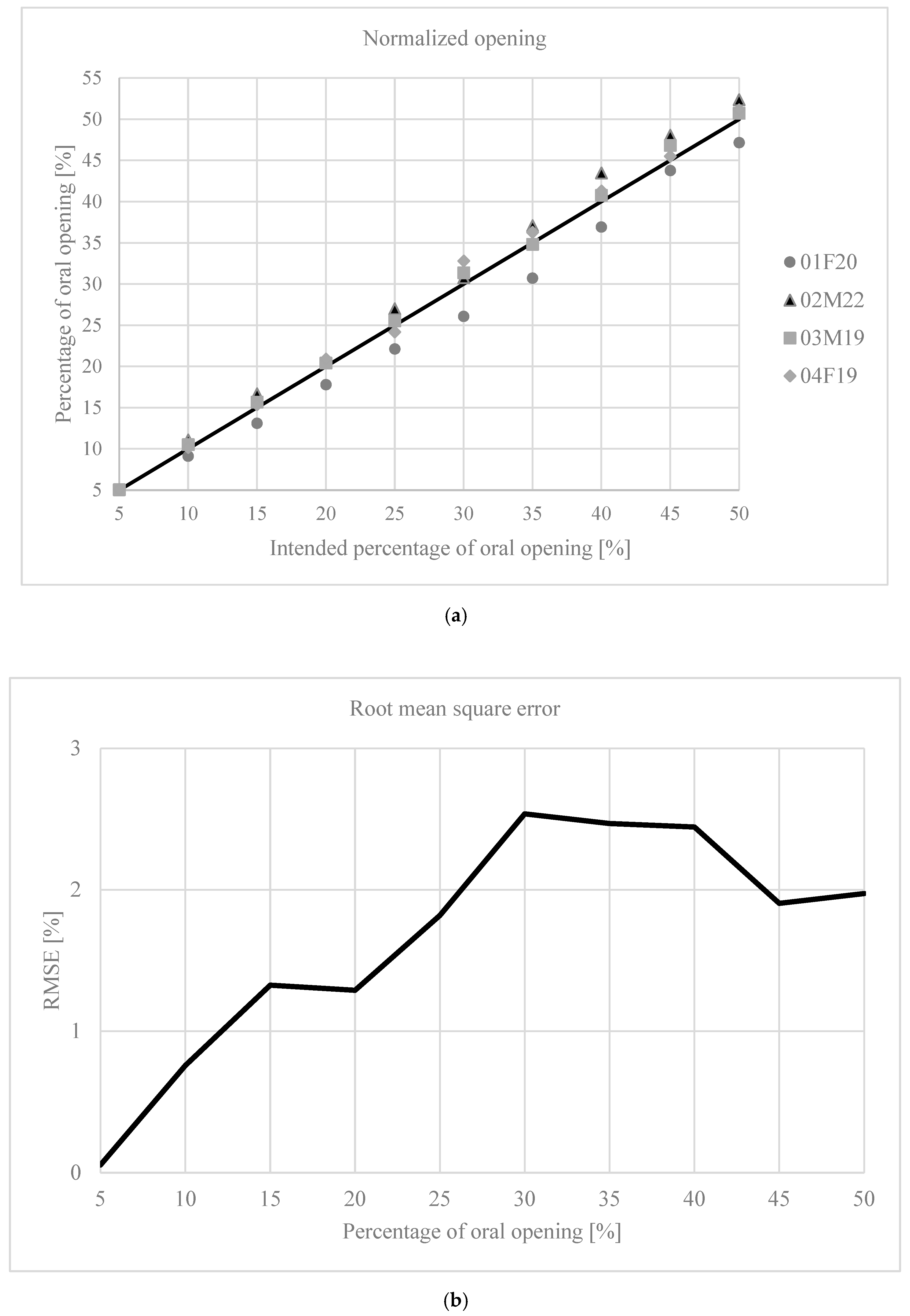
2.1. Normalization of Mouth Opening
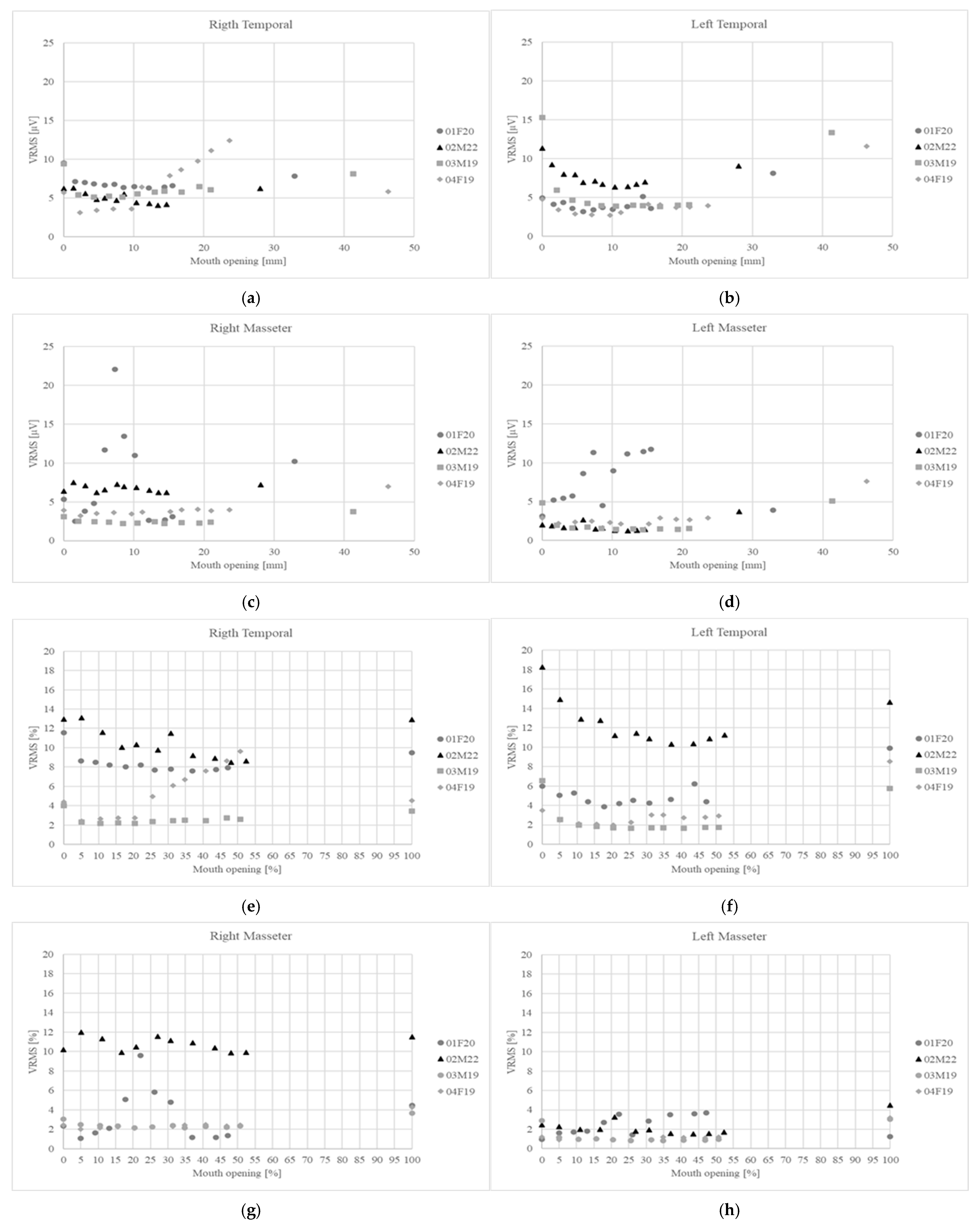
2.2. Normalization of Muscular Activity
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| EMA | Electromagnetic Articulography |
| sEMG | Surface Electromyography |
| MMO | Maximum Mouth Opening |
References
- Zieliński, G.; Gawda, P. Surface Electromyography in Dentistry—Past, Present and Future. JCM 2024, 13, 1328. [Google Scholar] [CrossRef]
- Suvinen, T.I.; Kemppainen, P. Review of Clinical EMG Studies Related to Muscle and Occlusal Factors in Healthy and TMD Subjects. J. Oral Rehabil. 2007, 34, 631–644. [Google Scholar] [CrossRef]
- Garnick, J.; Ramfjord, S.P. Rest Position. J. Prosthet. Dent. 1962, 12, 895–911. [Google Scholar] [CrossRef]
- Gross, M.D.; Ormianer, Z.; Moshe, K.; Gazit, E. Integrated Electromyography of the Masseter on Incremental Opening and Closing with Audio Biofeedback: A Study on Mandibular Posture. Int. J. Prosthodont. 1999, 12, 419–425. [Google Scholar]
- Terebesi, S.; Giannakopoulos, N.N.; Brüstle, F.; Hellmann, D.; Türp, J.C.; Schindler, H.J. Small Vertical Changes in Jaw Relation Affect Motor Unit Recruitment in the Masseter. J. Oral Rehabil. 2016, 43, 259–268. [Google Scholar] [CrossRef] [PubMed]
- Okeson, J.P. Management of Temporomandibular Disorders and Occlusion, 5th ed.; Mosby: St. Louis, MO, USA, 2003; ISBN 978-0-323-01477-9. [Google Scholar]
- Michelotti, A.; Farella, M.; Vollaro, S.; Martina, R. Mandibular Rest Position and Electrical Activity of the Masticatory Muscles. J. Prosthet. Dent. 1997, 78, 48–53. [Google Scholar] [CrossRef] [PubMed]
- Suvinen, T.I.; Reade, P.C.; Könönen, M.; Kemppainen, P. Vertical Jaw Separation and Masseter Muscle Electromyographic Activity: A Comparative Study between Asymptomatic Controls & Patients with Temporomandibular Pain & Dysfunction. J. Oral Rehabil. 2003, 30, 765–772. [Google Scholar] [CrossRef]
- Majewski, R.F.; Gale, E.N. Electromyographic Activity of Anterior Temporal Area Pain Patients and Non-Pain Subjects. J. Dent. Res. 1984, 63, 1228–1231. [Google Scholar] [CrossRef] [PubMed]
- Manns, A.; Miralles, R.; Santander, H.; Valdivia, J. Influence of the Vertical Dimension in the Treatment of Myofascial Pain-Dysfunction Syndrome. J. Prosthet. Dent. 1983, 50, 700–709. [Google Scholar] [CrossRef]
- Akbulut, N.; Altan, A.; Akbulut, S.; Atakan, C. Evaluation of the 3 Mm Thickness Splint Therapy on Temporomandibular Joint Disorders (TMDs). Pain Res. Manag. 2018, 2018, 3756587. [Google Scholar] [CrossRef]
- Singh, B.P.; Singh, N.; Jayaraman, S.; Kirubakaran, R.; Joseph, S.; Muthu, M.S.; Jivnani, H.; Hua, F. Occlusal Interventions for Managing Temporomandibular Disorders. Cochrane Database Syst. Rev. 2024, 2024, CD012850. [Google Scholar] [CrossRef]
- Nota, A.; Caruso, S.; Ehsani, S.; Ferrazzano, G.F.; Gatto, R.; Tecco, S. Short-Term Effect of Orthodontic Treatment with Clear Aligners on Pain and sEMG Activity of Masticatory Muscles. Medicina 2021, 57, 178. [Google Scholar] [CrossRef]
- Woźniak, K.; Szyszka-Sommerfeld, L.; Lichota, D. The Electrical Activity of the Temporal and Masseter Muscles in Patients with TMD and Unilateral Posterior Crossbite. BioMed. Res. Int. 2015, 2015, 259372. [Google Scholar] [CrossRef]
- Ribeiro, A.B.; Pita, M.S.; Ribeiro, A.B.; Garcia, A.R.; Junqueira Zuim, P.R. Effect of Short-Term Increase in Occlusal Vertical Dimension on Masticatory Muscle Electrical Activities and Pressure-to-Pain Threshold: A Crossover Clinical Study. J. Prosthet. Dent. 2022, 128, 970–976. [Google Scholar] [CrossRef]
- Madhavan, S.; Dhanraj, M.; Jain, A.R. Methods of Recording Mandibular Movements—A Review. Drug Invent. Today 2018, 10, 1254–1259. [Google Scholar]
- Manns, A.; Miralles, R.; Cumsille, F. Influence of Vertical Dimension on Masseter Muscle Electromyographic Activity in Patients with Mandibular Dysfunction. J. Prosthet. Dent. 1985, 53, 243–247. [Google Scholar] [CrossRef] [PubMed]
- Shigemitsu, R.; Ogawa, T.; Sato, E.; Oliveira, A.S.; Rasmussen, J. Kinematic Classification of Mandibular Movements in Patients with Temporomandibular Disorders Based on PCA. Comput. Biol. Med. 2025, 184, 109441. [Google Scholar] [CrossRef] [PubMed]
- Tian, S.; Dai, N.; Li, L.; Li, W.; Sun, Y.; Cheng, X. Three-Dimensional Mandibular Motion Trajectory-Tracking System Based on BP Neural Network. Math. Biosci. Eng. 2020, 17, 5709–5726. [Google Scholar] [CrossRef]
- Shiga, H.; Itoh, Y.; Yokoyama, M.; Komino, M.; Nakajima, K.; Kobayashi, Y. Effect of Occlusal Interference on the Masticatory Movement Path. J. Jpn. Acad. Occulusion Health 2022, 28, 1–6. [Google Scholar]
- D’Attilio, M.; Di Carlo, B.; Caroccia, F.; Moscagiuri, F.; d’Angelo, D.M.; Chiarelli, F.; Festa, F.; Breda, L. Clinical and Instrumental TMJ Evaluation in Children and Adolescents with Juvenile Idiopathic Arthritis: A Case—Control Study. Appl. Sci. 2021, 11, 5380. [Google Scholar] [CrossRef]
- Zawawi, K.H.; Al-Badawi, E.A.; Lobo, S.L.; Melis, M.; Mehta, N.R. An Index for the Measurement of Normal Maximum Mouth Opening. J. Can. Dent. Assoc. 2003, 69, 737–741. [Google Scholar]
- Hawwa, M.M. Mouth Opening Range for Jordanian Population and Its Relation to Gender, Age, Height, and Weight. Saint’s Int. Dent. J. 2022, 6, 12–15. [Google Scholar] [CrossRef]
- Diong, J.; Kishimoto, K.C.; Butler, J.E.; Héroux, M.E. Muscle Electromyographic Activity Normalized to Maximal Muscle Activity, Not to Mmax, Better Represents Voluntary Activation. PLoS ONE 2022, 17, e0277947. [Google Scholar] [CrossRef]
- Sinclair, J.; Taylor, P.J.; Hebron, J.; Brooks, D.; Hurst, H.T.; Atkins, S. The Reliability of Electromyographic Normalization Methods for Cycling Analyses. J. Hum. Kinet. 2015, 46, 19–27. [Google Scholar] [CrossRef]
- Kulchutisin, P.; Sowithayasakul, T.; Pumklin, J.; Piyapattamin, T. Electromyographic Evaluations of Masticatory Muscle Activity between Patients with Skeletal Class I and III Relationships. Eur. J. Dent. 2023, 17, 910–916. [Google Scholar] [CrossRef]
- Ferrario, V.F.; Sforza, C.; Miani, A.; D’Addona, A.; Barbini, E. Electromyographic Activity of Human Masticatory Muscles in Normal Young People. Statistical Evaluation of Reference Values for Clinical Applications. J. Oral Rehabil. 1993, 20, 271–280. [Google Scholar] [CrossRef] [PubMed]
- Matsui, M.Y.; Giannasi, L.C.; Batista, S.R.F.; Amorim, J.B.O.; Oliveira, C.S.; Oliveira, L.V.F.; Gomes, M.F. Differences between the Activity of the Masticatory Muscles of Adults with Cerebral Palsy and Healthy Individuals While at Rest and in Function. Arch. Oral Biol. 2017, 73, 16–20. [Google Scholar] [CrossRef] [PubMed]
- Manns, A.; Miralles, R.; Guerrero, F. The Changes in Electrical Activity of the Postural Muscles of the Mandible upon Varying the Vertical Dimension. J. Prosthet. Dent. 1981, 45, 438–445. [Google Scholar] [CrossRef]
- Montero, J.; Castillo-Oyagüe, R.; Lynch, C.D.; Albaladejo, A.; Castaño, A. Self-Perceived Changes in Oral Health-Related Quality of Life after Receiving Different Types of Conventional Prosthetic Treatments: A Cohort Follow-up Study. J. Dent. 2013, 41, 493–503. [Google Scholar] [CrossRef]
- Schiffman, E.; Ohrbach, R.; Truelove, E.; Look, J.; Anderson, G.; Goulet, J.-P.; List, T.; Svensson, P.; Gonzalez, Y.; Lobbezoo, F.; et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: Recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group. J. Oral Facial Pain Headache 2014, 28, 6–27. [Google Scholar] [CrossRef]
- Farfán, N.C.; Lezcano, M.F.; Navarro-Cáceres, P.E.; Sandoval-Vidal, H.P.; Martinez-Gomis, J.; Muñoz, L.; Marinelli, F.; Fuentes, R. Characterization of Mandibular Border Movements and Mastication in Each Skeletal Class Using 3D Electromagnetic Articulography: A Preliminary Study. Diagnostics 2023, 13, 2405. [Google Scholar] [CrossRef]
- Lezcano, M.F.; Dias, F.; Arias, A.; Fuentes, R. Accuracy and Reliability of AG501 Articulograph for Mandibular Movement Analysis: A Quantitative Descriptive Study. Sensors 2020, 20, 6324. [Google Scholar] [CrossRef]
- Szyszka-Sommerfeld, L.; Machoy, M.; Lipski, M.; Woźniak, K. Electromyography as a Means of Assessing Masticatory Muscle Activity in Patients with Pain-Related Temporomandibular Disorders. Pain Res. Manag. 2020, 2020, 9750915. [Google Scholar] [CrossRef]
- Lindauer, S.J.; Gay, T.; Rendell, J. Effect of Jaw Opening on Masticatory Muscle EMG-Force Characteristics. J. Dent. Res. 1993, 72, 51–55. [Google Scholar] [CrossRef]
- Rugh, J.D.; Drago, C.J. Vertical Dimension: A Study of Clinical Rest Position and Jaw Muscle Activity. J. Prosthet. Dent. 1981, 45, 670–675. [Google Scholar] [CrossRef]
- Plesh, O.; McCall, W.D.; Gross, A. The Effect of Prior Jaw Motion on the Plot of Electromyographic Amplitude versus Jaw Position. J. Prosthet. Dent. 1988, 60, 369–373. [Google Scholar] [CrossRef]
- Zieliński, G.; Gawda, P. Defining Effect Size Standards in Temporomandibular Joint and Masticatory Muscle Research. Med. Sci. Monit. 2025, 31, e948365. [Google Scholar] [CrossRef]
- Mehr, K. Surface Electromyography in Orthodontics—A Literature Review. Med. Sci. Monit. 2013, 19, 416–423. [Google Scholar] [CrossRef]
- Woda, A.; Pionchon, P.; Palla, S. Regulation of Mandibular Postures: Mechanisms and Clinical Implications. Crit. Rev. Oral Biol. Med. 2001, 12, 166–178. [Google Scholar] [CrossRef]
| Subject | VMVC—RT [µV] | VMVC—LT [µV] | VMVC—RM [µV] | VMVC—LM [µV] | MMO [mm] | ∆5% [mm] |
|---|---|---|---|---|---|---|
| 01F20 | 48.0 | 62.0 | 62.7 | 83.0 | 28.1 | 1.4 |
| 02M22 | 233.4 | 233.7 | 101.8 | 168.0 | 41.3 | 2.1 |
| 03M19 | 82.5 | 82.3 | 229.8 | 317.6 | 32.9 | 1.6 |
| 04F19 | 128.8 | 136.5 | 162.9 | 240.6 | 46.3 | 2.3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marinelli, F.; Venegas-Ocampo, C.; Alarcón-Apablaza, J.; Ruiz, J.; Schlotthauer, G.; Schneider, R.; Fuentes, R. A Standardized Protocol for Analyzing Masticatory Muscle Activity at Different Levels of Mouth Opening Using Electromagnetic Articulography and Surface Electromyography: A Proof-of-Concept Study. Bioengineering 2025, 12, 811. https://doi.org/10.3390/bioengineering12080811
Marinelli F, Venegas-Ocampo C, Alarcón-Apablaza J, Ruiz J, Schlotthauer G, Schneider R, Fuentes R. A Standardized Protocol for Analyzing Masticatory Muscle Activity at Different Levels of Mouth Opening Using Electromagnetic Articulography and Surface Electromyography: A Proof-of-Concept Study. Bioengineering. 2025; 12(8):811. https://doi.org/10.3390/bioengineering12080811
Chicago/Turabian StyleMarinelli, Franco, Camila Venegas-Ocampo, Josefa Alarcón-Apablaza, Joaquín Ruiz, Gastón Schlotthauer, Rosemarie Schneider, and Ramón Fuentes. 2025. "A Standardized Protocol for Analyzing Masticatory Muscle Activity at Different Levels of Mouth Opening Using Electromagnetic Articulography and Surface Electromyography: A Proof-of-Concept Study" Bioengineering 12, no. 8: 811. https://doi.org/10.3390/bioengineering12080811
APA StyleMarinelli, F., Venegas-Ocampo, C., Alarcón-Apablaza, J., Ruiz, J., Schlotthauer, G., Schneider, R., & Fuentes, R. (2025). A Standardized Protocol for Analyzing Masticatory Muscle Activity at Different Levels of Mouth Opening Using Electromagnetic Articulography and Surface Electromyography: A Proof-of-Concept Study. Bioengineering, 12(8), 811. https://doi.org/10.3390/bioengineering12080811








