Comparative Assessment of the Mechanical Response to Different Screw Dimensions in Scaphoid Fracture Fixation
Abstract
1. Introduction
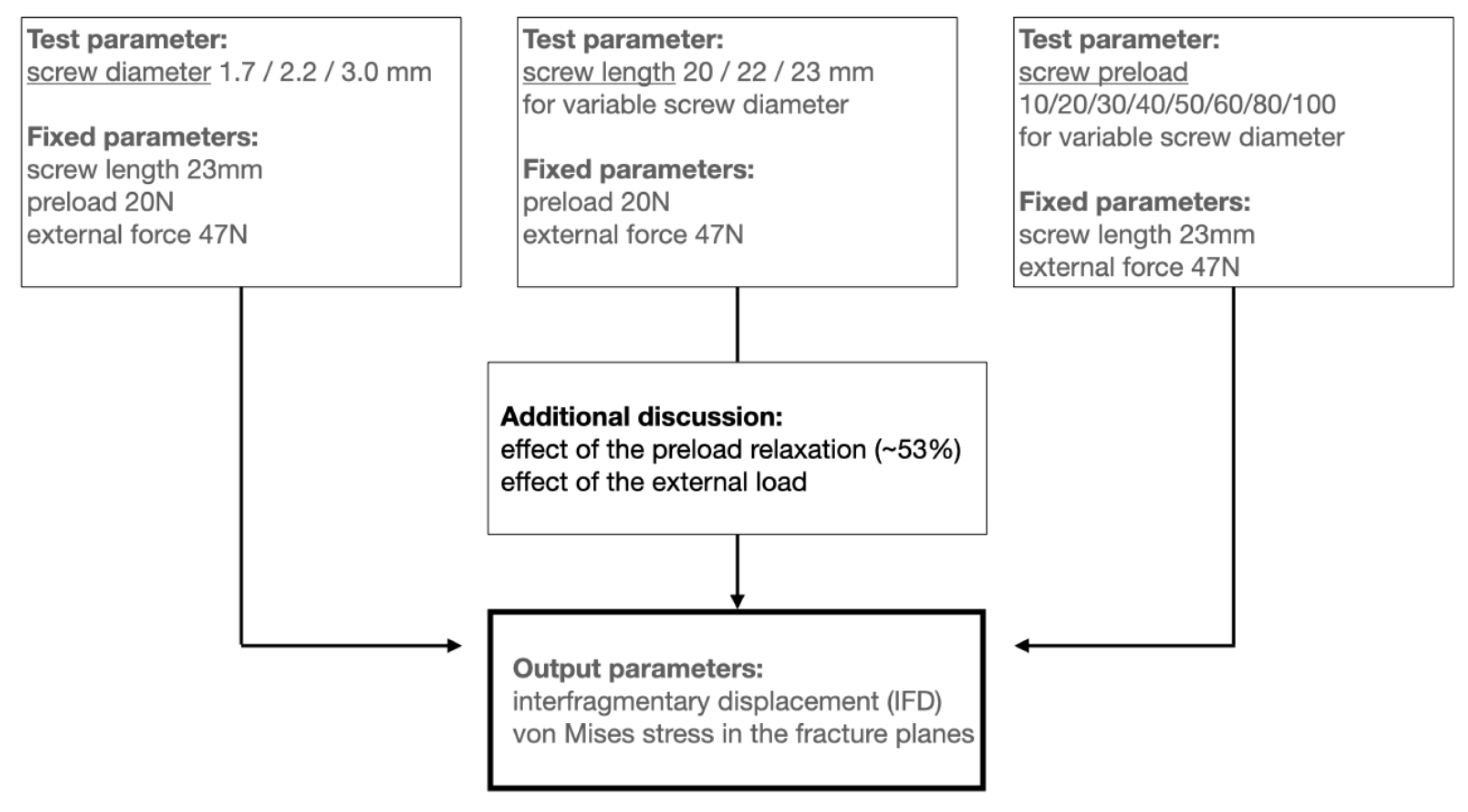
2. Methods
2.1. Geometry
2.2. Validation
2.3. Loading and Boundary Conditions
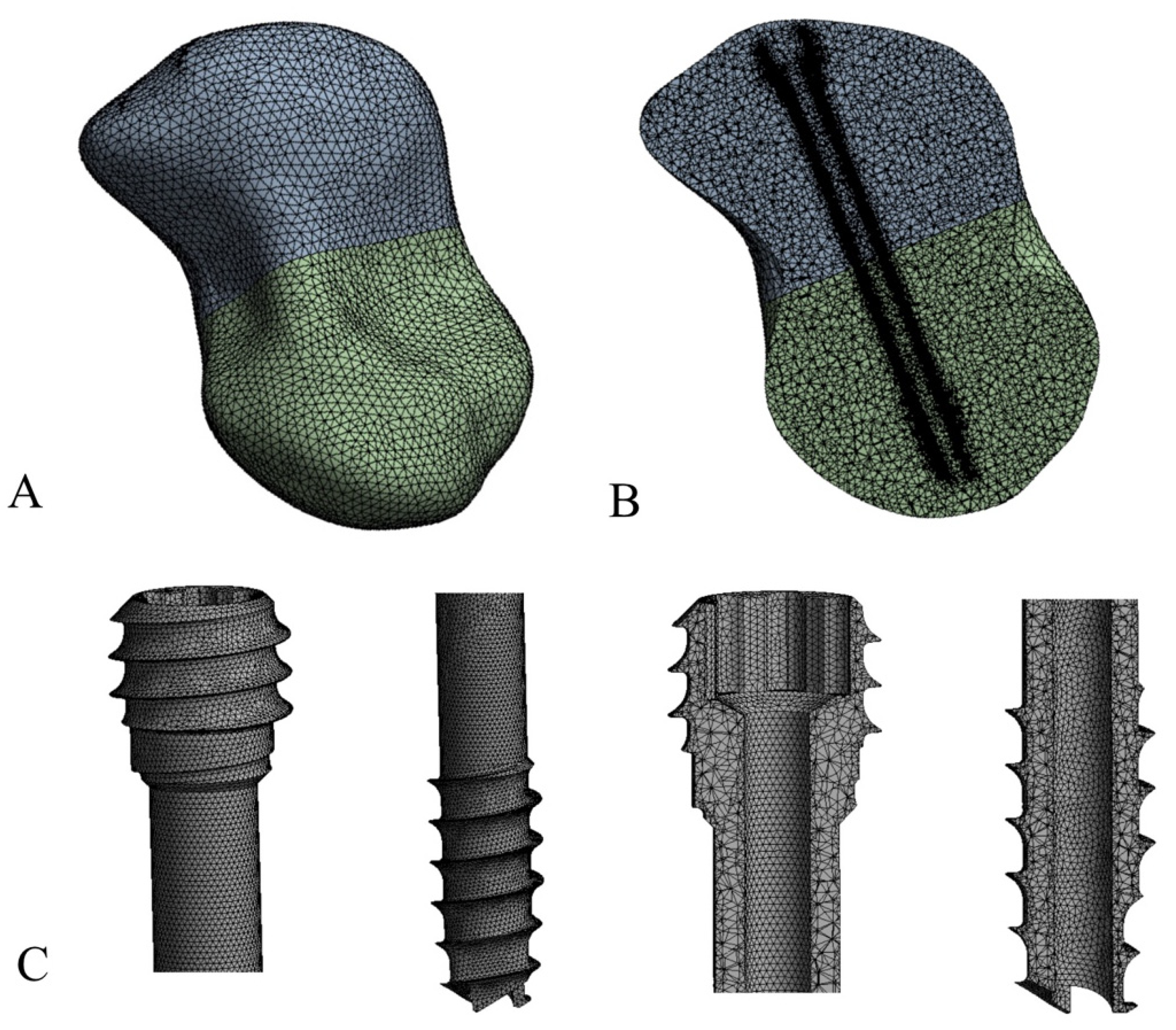
2.4. Finite Element Model Analysis
3. Results
3.1. What Is the Relative Benefit of a Larger Screw for Stability in Mid-Waist Scaphoid Fractures?
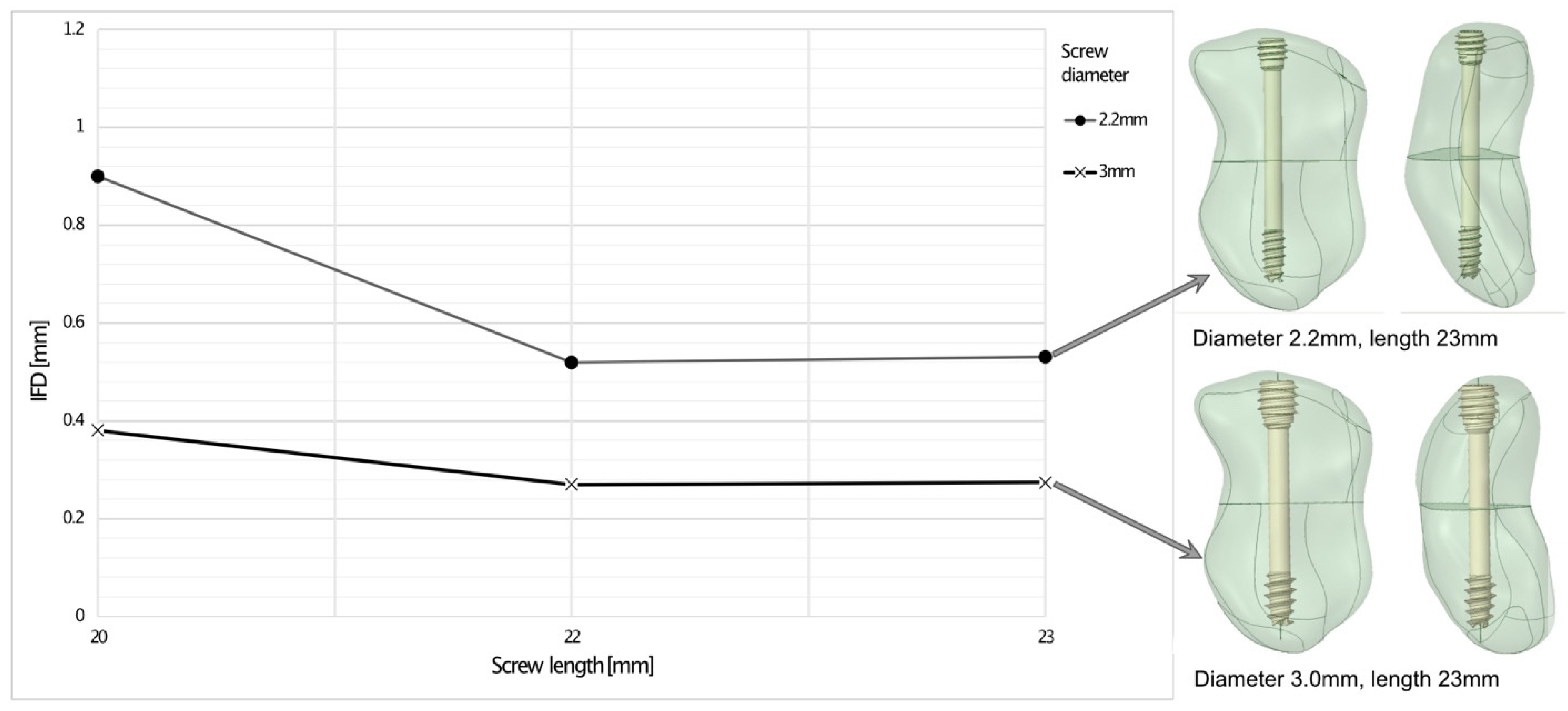
3.2. Does Screw Length Affect Biomechanical Stability When Placed Along the Scaphoid’s Axis at the Fracture Plane?
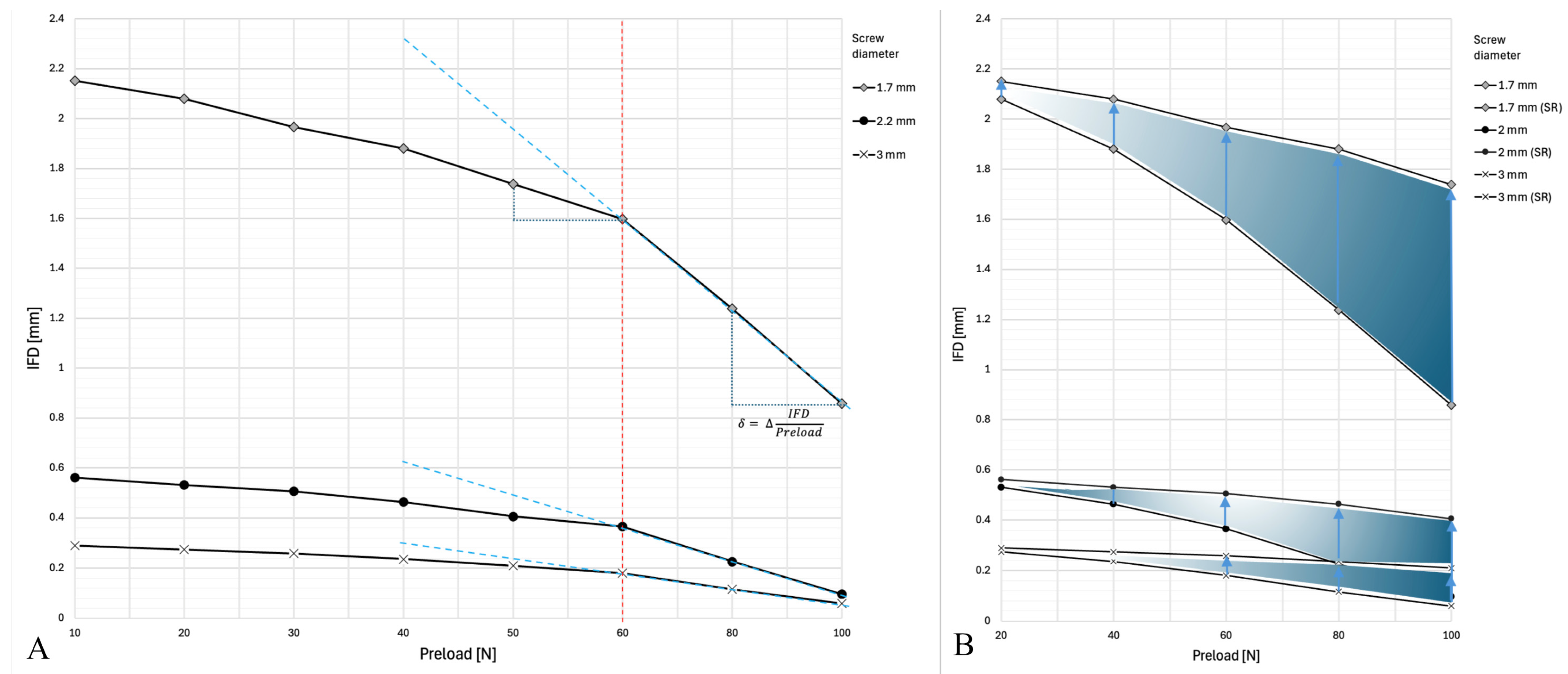
3.3. What Is the Reference Preload Range for Fixing Scaphoid Fractures?
4. Discussion
5. Conclusions
- Based on this study, there is no need to use a screw with a diameter greater than 2.2 mm for biomechanically sufficient fixation of a scaphoid waist fracture, because this may compromise intraosseous perfusion.
- The screw length should not exceed 1.5 times the mid-waist diameter and must be countersunk.
- The ideal preload is approximately 60 N. However, it cannot currently be measured in situ and therefore depends on the surgeon’s experience.
- A scaphoid mid-waist fracture fixed with a single screw in an early healing stage cannot withstand external loads equivalent to gripping an object weighing 0.5 kg or more.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
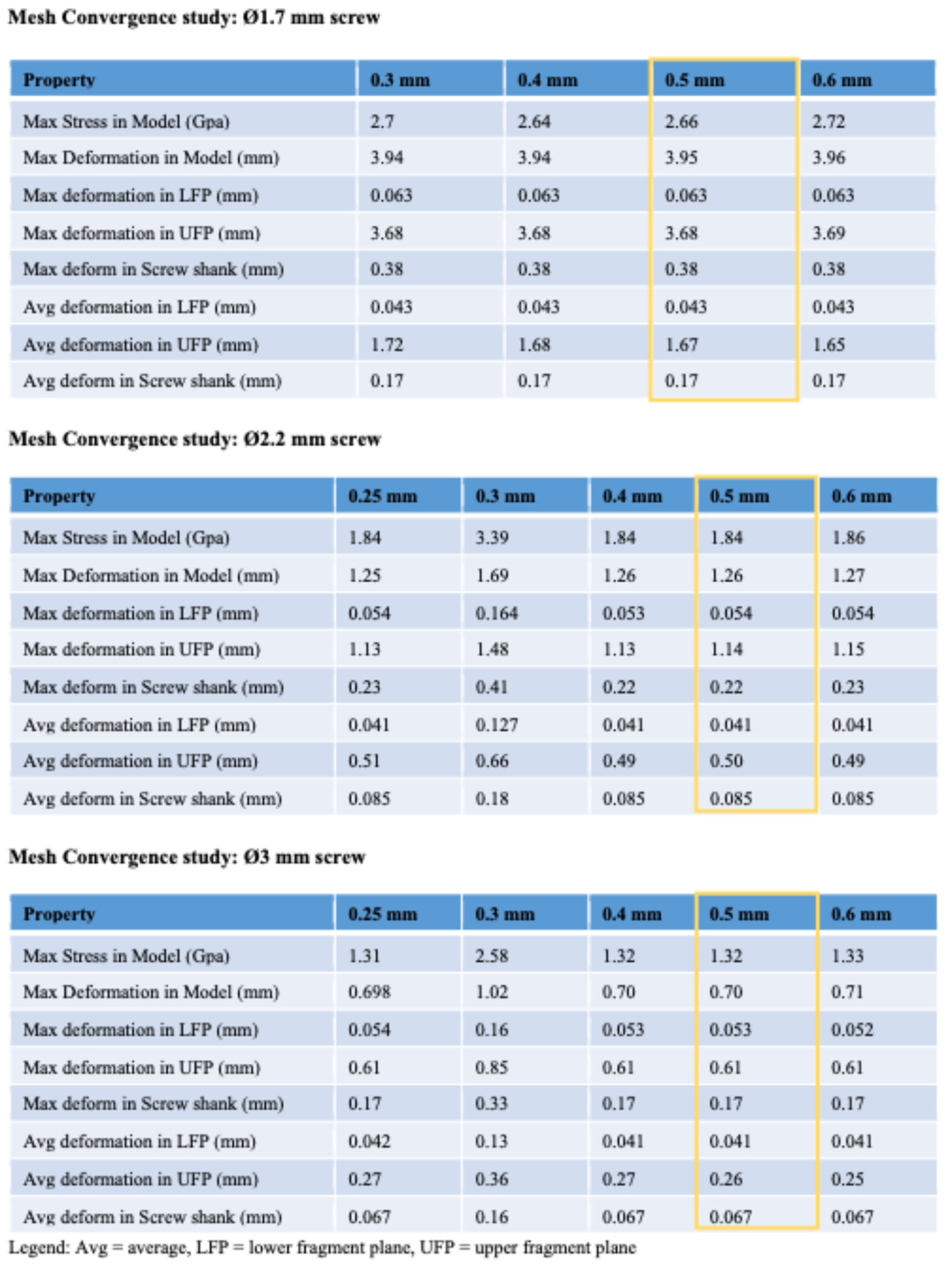 |
References
- Duckworth, A.D.; Jenkins, P.J.; Aitken, S.A.; Clement, N.D.; Court-Brown, C.M.; McQueen, M.M. Scaphoid fracture epidemiology. J. Trauma Acute Care Surg. 2012, 72, E41–E45. [Google Scholar] [CrossRef] [PubMed]
- Hove, L.M. Epidemiology of scaphoid fractures in Bergen, Norway. Scand. J. Plast. Reconstr. Surg. Hand Surg. 1999, 33, 423–426. [Google Scholar] [CrossRef] [PubMed]
- Sward, E.M.; Schriever, T.U.; Franko, M.A.; Bjorkman, A.C.; Wilcke, M.K. The epidemiology of scaphoid fractures in Sweden: A nationwide registry study. J. Hand Surg. Eur. Vol. 2019, 44, 697–701. [Google Scholar] [CrossRef] [PubMed]
- Clementson, M.; Bjorkman, A.; Thomsen, N.O.B. Acute scaphoid fractures: Guidelines for diagnosis and treatment. EFORT Open Rev. 2020, 5, 96–103. [Google Scholar] [CrossRef] [PubMed]
- Dias, J.J.; Brealey, S.D.; Fairhurst, C.; Amirfeyz, R.; Bhowal, B.; Blewitt, N.; Brewster, M.; Brown, D.; Choudhary, S.; Coapes, C.; et al. Surgery versus cast immobilisation for adults with a bicortical fracture of the scaphoid waist (SWIFFT): A pragmatic, multicentre, open-label, randomised superiority trial. Lancet 2020, 396, 390–401. [Google Scholar] [CrossRef] [PubMed]
- Kawamura, K.; Chung, K.C. Treatment of scaphoid fractures and nonunions. J. Hand Surg. Am. 2008, 33, 988–997. [Google Scholar] [CrossRef] [PubMed]
- Sabbagh, M.D.; Morsy, M.; Moran, S.L. Diagnosis and Management of Acute Scaphoid Fractures. Hand Clin. 2019, 35, 259–269. [Google Scholar] [CrossRef] [PubMed]
- Clay, N.R.; Dias, J.J.; Costigan, P.S.; Gregg, P.J.; Barton, N.J. Need the thumb be immobilised in scaphoid fractures? A randomised prospective trial. J. Bone Jt. Surg. Br. 1991, 73, 828–832. [Google Scholar] [CrossRef] [PubMed]
- Slade, J.F., 3rd; Dodds, S.D. Minimally invasive management of scaphoid nonunions. Clin. Orthop. Relat. Res. 2006, 445, 108–119. [Google Scholar] [CrossRef] [PubMed]
- Hackney, L.A.; Dodds, S.D. Assessment of scaphoid fracture healing. Curr. Rev. Musculoskelet. Med. 2011, 4, 16–22. [Google Scholar] [CrossRef] [PubMed]
- Luria, S.; Hoch, S.; Liebergall, M.; Mosheiff, R.; Peleg, E. Optimal fixation of acute scaphoid fractures: Finite element analysis. J. Hand Surg. Am. 2010, 35, 1246–1250. [Google Scholar] [CrossRef] [PubMed]
- McCallister, W.V.; Knight, J.; Kaliappan, R.; Trumble, T.E. Central placement of the screw in simulated fractures of the scaphoid waist: A biomechanical study. J. Bone Jt. Surg. Am. 2003, 85, 72–77. [Google Scholar] [CrossRef] [PubMed]
- Dodds, S.D.; Panjabi, M.M.; Slade, J.F., 3rd. Screw fixation of scaphoid fractures: A biomechanical assessment of screw length and screw augmentation. J. Hand Surg. Am. 2006, 31, 405–413. [Google Scholar] [CrossRef] [PubMed]
- Gareb, B.; van Munster, V.D.M.; Dijkstra, P.U.; Bos, R.R.M.; Vissink, A.; van Bakelen, N.B.; van Minnen, B. Reliability and accuracy of the torque applied to osteosynthesis screws by maxillofacial surgeons and residents. Sci. Rep. 2022, 12, 14411. [Google Scholar] [CrossRef] [PubMed]
- Rothenfluh, E.; Jain, S.; Guggenberger, R.; Taylor, W.R.; Hosseini Nasab, S.H. The influence of partial union on the mechanical strength of scaphoid fractures: A finite element study. J. Hand Surg. Eur. Vol. 2023, 48, 435–444. [Google Scholar] [CrossRef] [PubMed]
- Oftadeh, R.; Perez-Viloria, M.; Villa-Camacho, J.C.; Vaziri, A.; Nazarian, A. Biomechanics and mechanobiology of trabecular bone: A review. J. Biomech. Eng. 2015, 137, 010802. [Google Scholar] [CrossRef] [PubMed]
- Bohler, L.; Trojan, E.; Jahna, H. The results of treatment of 734 fresh, simple fractures of the scaphoid. J. Hand Surg. Br. 2003, 28, 319–331. [Google Scholar] [CrossRef] [PubMed]
- Acar, B.; Kose, O.; Kati, Y.A.; Egerci, O.F.; Turan, A.; Yuksel, H.Y. Comparison of volar versus dorsal screw fixation for scaphoid waist fractures: A finite element analysis. Orthop. Traumatol. Surg. Res. 2018, 104, 1107–1113. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.; Giugale, J.; Tiedeken, N.; Debski, R.E.; Fowler, J.R. Impact of Screw Length on Proximal Scaphoid Fracture Biomechanics. J. Wrist Surg. 2019, 8, 360–365. [Google Scholar] [CrossRef] [PubMed]
- Viegas, S.F.; Patterson, R.; Peterson, P.; Roefs, J.; Tencer, A.; Choi, S. The effects of various load paths and different loads on the load transfer characteristics of the wrist. J. Hand Surg. Am. 1989, 14, 458–465. [Google Scholar] [CrossRef] [PubMed]
- Erhart, J.; Unger, E.; Schefzig, P.; Varga, P.; Trulson, I.; Gormasz, A.; Trulson, A.; Reschl, M.; Hagmann, M.; Vecsei, V.; et al. Rotational Stability of Scaphoid Osteosyntheses: An In Vitro Comparison of Small Fragment Cannulated Screws to Novel Bone Screw Sets. PLoS ONE 2016, 11, e0156080. [Google Scholar] [CrossRef] [PubMed]
- Gruszka, D.; Herr, R.; Hely, H.; Hofmann, P.; Klitscher, D.; Hofmann, A.; Rommens, P.M. Impact of Different Screw Designs on Durability of Fracture Fixation: In Vitro Study with Cyclic Loading of Scaphoid Bones. PLoS ONE 2016, 11, e0145949. [Google Scholar] [CrossRef] [PubMed]
- Varga, P.; Zysset, P.K.; Schefzig, P.; Unger, E.; Mayr, W.; Erhart, J. A finite element analysis of two novel screw designs for scaphoid waist fractures. Med. Eng. Phys. 2016, 38, 131–139. [Google Scholar] [CrossRef] [PubMed]
- Gersie, T.; Bitter, T.; Wolfson, D.; Freeman, R.; Verdonschot, N.; Janssen, D. Quantification of long-term nonlinear stress relaxation of bovine trabecular bone. J. Mech. Behav. Biomed. Mater. 2024, 152, 106434. [Google Scholar] [CrossRef] [PubMed]
- Rugg, A.L.; Requist, M.R.; Johnson, B.W.; Son, M.M.; Alvarez, A.; Latt, L.D. Mechanical Effects of Lag Screw Retightening in a Simulated Hindfoot Arthrodesis Model. Foot Ankle Orthop. 2021, 6, 24730114211015203. [Google Scholar] [CrossRef] [PubMed]
- Heinzelmann, A.D.; Archer, G.; Bindra, R.R. Anthropometry of the human scaphoid. J. Hand Surg. Am. 2007, 32, 1005–1008. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.; Hofmeister, E.P.; Renninger, C.; Kroonen, L.T. Anthropometry of the Human Scaphoid Waist by Three-Dimensional Computed Tomography. J. Surg. Orthop. Adv. 2015, 24, 184–187. [Google Scholar] [PubMed]
- Mandaleson, A.; Tham, S.K.; Lewis, C.; Ackland, D.C.; Ek, E.T. Scaphoid Fracture Fixation in a Nonunion Model: A Biomechanical Study Comparing 3 Types of Fixation. J. Hand Surg. Am. 2018, 43, 221–228. [Google Scholar] [CrossRef] [PubMed]
- Beutel, B.G.; Melamed, E.; Hinds, R.M.; Gottschalk, M.B.; Capo, J.T. Mechanical Evaluation of Four Internal Fixation Constructs for Scaphoid Fractures. Hand 2016, 11, 72–77. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.C.; Lin, K.J.; Chen, W.C.; Wei, H.W.; Lin, K.P.; Tsai, C.L. Larger screw diameter may not guarantee greater pullout strength for headless screws—A biomechanical study. Biomed. Tech. 2017, 62, 257–261. [Google Scholar] [CrossRef] [PubMed]
- Ezquerro, F.; Jimenez, S.; Perez, A.; Prado, M.; de Diego, G.; Simon, A. The influence of wire positioning upon the initial stability of scaphoid fractures fixed using Kirschner wires A finite element study. Med. Eng. Phys. 2007, 29, 652–660. [Google Scholar] [CrossRef] [PubMed]
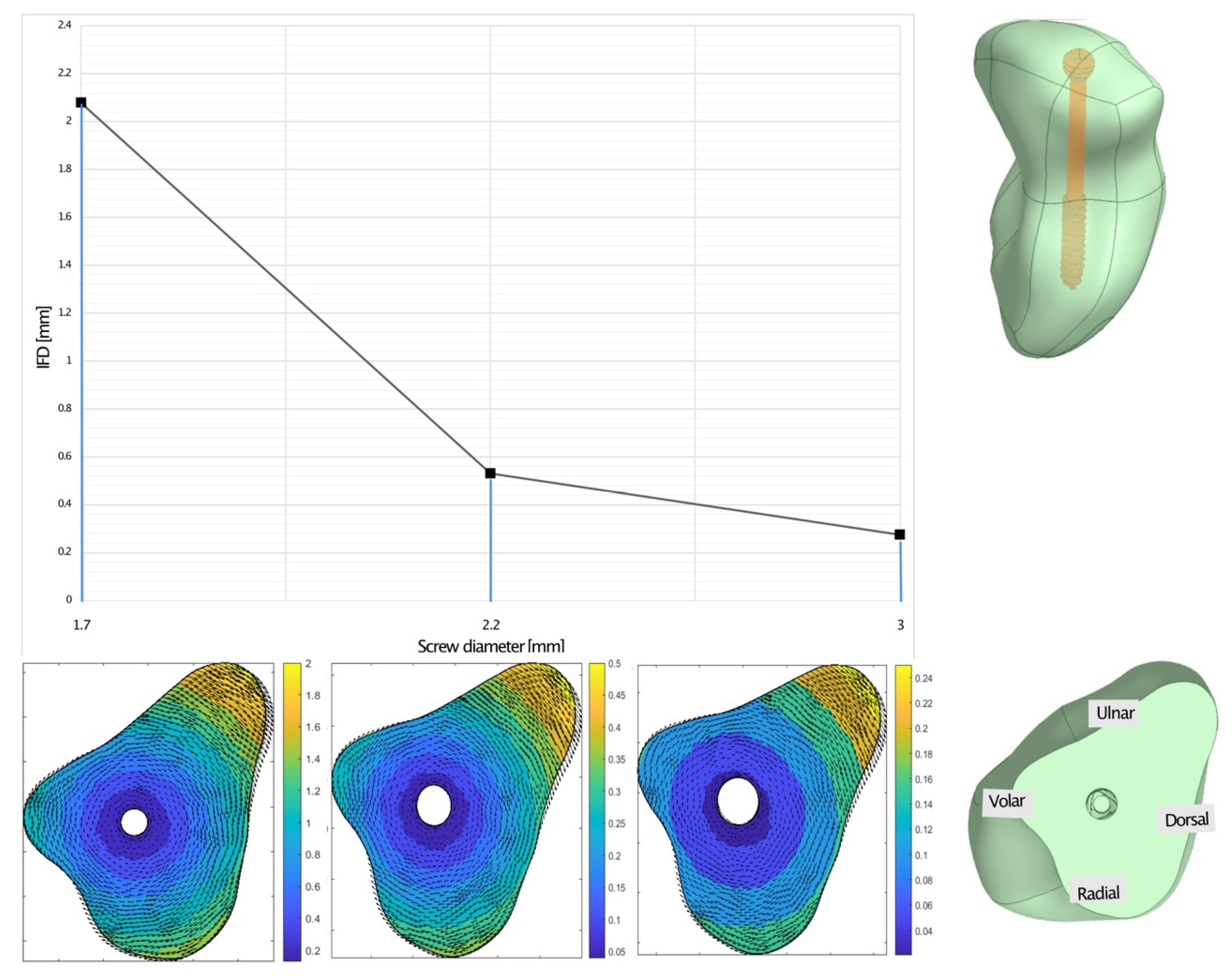

| IFD [mm] | Max. Stress UF [MPa] | Max. Stress LF [MPa] | ||
|---|---|---|---|---|
| Screw diameter [mm] | 1.7 | 2.0798 | 111.85 | 110.87 |
| 2.2 | 0.5306 | 37.01 | 52.41 | |
| 3.0 | 0.2743 | 27.74 | 38.69 | |
| IFD [mm] | Max. Stress UF [MPa] | Max. Stress LF [MPa] | |||
|---|---|---|---|---|---|
| Screw diameter and length [mm] | 2.2 | 20 | 0.9002 | 31.19 | 31.66 |
| 22 | 0.5197 | 36.95 | 51.79 | ||
| 23 | 0.5306 | 37.01 | 52.41 | ||
| 3.0 | 20 | 0.3805 | 28.16 | 49.58 | |
| 22 | 0.2701 | 27.24 | 37.96 | ||
| 23 | 0.2743 | 27.74 | 38.69 | ||
| IFD [mm] Under Preload [N] Variation | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| 10 | 20 | 30 | 40 | 50 | 60 | 80 | 100 | ||
| Screw diameter [mm] without and with SR | 1.7 | 2.1508 | 2.0798 | 1.9666 | 1.8803 | 1.7382 | 1.5971 | 1.2376 | 0.8581 |
| +SR | 2.1508 | 2.0798 | 1.9666 | 1.8803 | 1.7382 | ||||
| 2.2 | 0.5613 | 0.5306 | 0.5055 | 0.4636 | 0.4053 | 0.3649 | 0.2258 | 0.0969 | |
| +SR | 0.5613 | 0.5306 | 0.5055 | 0.4636 | 0.4053 | ||||
| 3.0 | 0.29 | 0.5306 | 0.5055 | 0.4636 | 0.21 | 0.1806 | 0.1154 | 0.0591 | |
| +SR | 0.29 | 0.2743 | 0.2584 | 0.2357 | 0.21 | ||||
| Max. stress UF [MPa] under preload [N] variation | |||||||||
| 10 | 20 | 30 | 40 | 50 | 60 | 80 | 100 | ||
| 1.7 | 108.38 | 111.85 | 114.08 | 116.8 | 118.57 | 118.49 | 117.22 | 111.48 | |
| 2.2 | 36.62 | 37.01 | 38.47 | 40.26 | 40.53 | 41.31 | 39.5 | 31.82 | |
| 3.0 | 26.98 | 27.74 | 28.33 | 28.65 | 28.67 | 28.92 | 26.75 | 22.21 | |
| Max. stress LF [MPa] under preload [N] variation | |||||||||
| 10 | 20 | 30 | 40 | 50 | 60 | 80 | 100 | ||
| 1.7 | 113.34 | 110.87 | 108.72 | 107.1 | 105.9 | 104.56 | 101.95 | 98.75 | |
| 2.2 | 53.24 | 52.41 | 50.34 | 48.54 | 46.93 | 45.45 | 41.25 | 32.73 | |
| 3.0 | 40.47 | 38.69 | 37.2 | 35.85 | 34.43 | 33.08 | 28.73 | 21.92 | |
| Previous Studies in the Field of Scaphoid Fracture Fixation | ||||
|---|---|---|---|---|
| Authors | Year | Exp. | FE | Scientific Question and Details |
| CC. Lin et al. [30] | 2017 | X | How do the dimension of headless compression screws alter pullout strength?
| |
| S. Patel et al. [19] | 2019 | X | What impact does screw length have on the biomechanics of proximal scaphoid fracture fixation?
| |
| D. Gruszka et al. [22] | 2016 | X | What is the impact of screw designs (four types) on the durability of fracture fixation?
| |
| J. Erhart et al. [21] | 2016 | X | Does an autorotational element to headless compression screws provide enhanced rotational stability in scaphoid fixations?
| |
| A. Mandaleson et al. [28] | 2018 | X | How does biomechanical stability compare across three different types of fixations for scaphoid fracture non-unions?
| |
| SD. Dodds et al. [13] | 2006 | X | How does screw length and augmentation of the screw with a K-wire influence biomechanical stability in scaphoid fracture fixation?
| |
| WV. McCallister et al. [12] | 2003 | X | How does central or eccentric placement of the screw influence stability in scaphoid fracture fixation?
| |
| S. Luria et al. [11] | 2010 | X | What is the optimal configuration of screw placement for scaphoid fracture fixation?
| |
| F. Ezquerro et al. [31] | 2007 | X | How does the positioning of two wires influence biomechanical stability in scaphoid fracture fixation?
| |
| B. Acar et al. [18] | 2018 | X | Does dorsal or volar screw fixation have an impact on stability of scaphoid fracture fixation?
| |
| P. Varga et al. [23] | 2016 | X | Three different screw designs are proposed and evaluated with regard to their efficacy in scaphoid fracture fixation: (1) a single fully treaded screw (constant pitch), (2) a screw with an additional parallel, partially threaded component, and (3) a screw with an additional oblique (20°), interlocking component;
| |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rothenfluh, E.; Jain, S.; Taylor, W.R.; Hosseini Nasab, S.H. Comparative Assessment of the Mechanical Response to Different Screw Dimensions in Scaphoid Fracture Fixation. Bioengineering 2025, 12, 790. https://doi.org/10.3390/bioengineering12080790
Rothenfluh E, Jain S, Taylor WR, Hosseini Nasab SH. Comparative Assessment of the Mechanical Response to Different Screw Dimensions in Scaphoid Fracture Fixation. Bioengineering. 2025; 12(8):790. https://doi.org/10.3390/bioengineering12080790
Chicago/Turabian StyleRothenfluh, Esin, Sambhav Jain, William R. Taylor, and Seyyed Hamed Hosseini Nasab. 2025. "Comparative Assessment of the Mechanical Response to Different Screw Dimensions in Scaphoid Fracture Fixation" Bioengineering 12, no. 8: 790. https://doi.org/10.3390/bioengineering12080790
APA StyleRothenfluh, E., Jain, S., Taylor, W. R., & Hosseini Nasab, S. H. (2025). Comparative Assessment of the Mechanical Response to Different Screw Dimensions in Scaphoid Fracture Fixation. Bioengineering, 12(8), 790. https://doi.org/10.3390/bioengineering12080790










