Preliminary Effects of Extended Reality-Based Rehabilitation on Gross Motor Function, Balance, and Psychosocial Health in Children with Cerebral Palsy
Abstract
1. Introduction
2. Materials and Methods
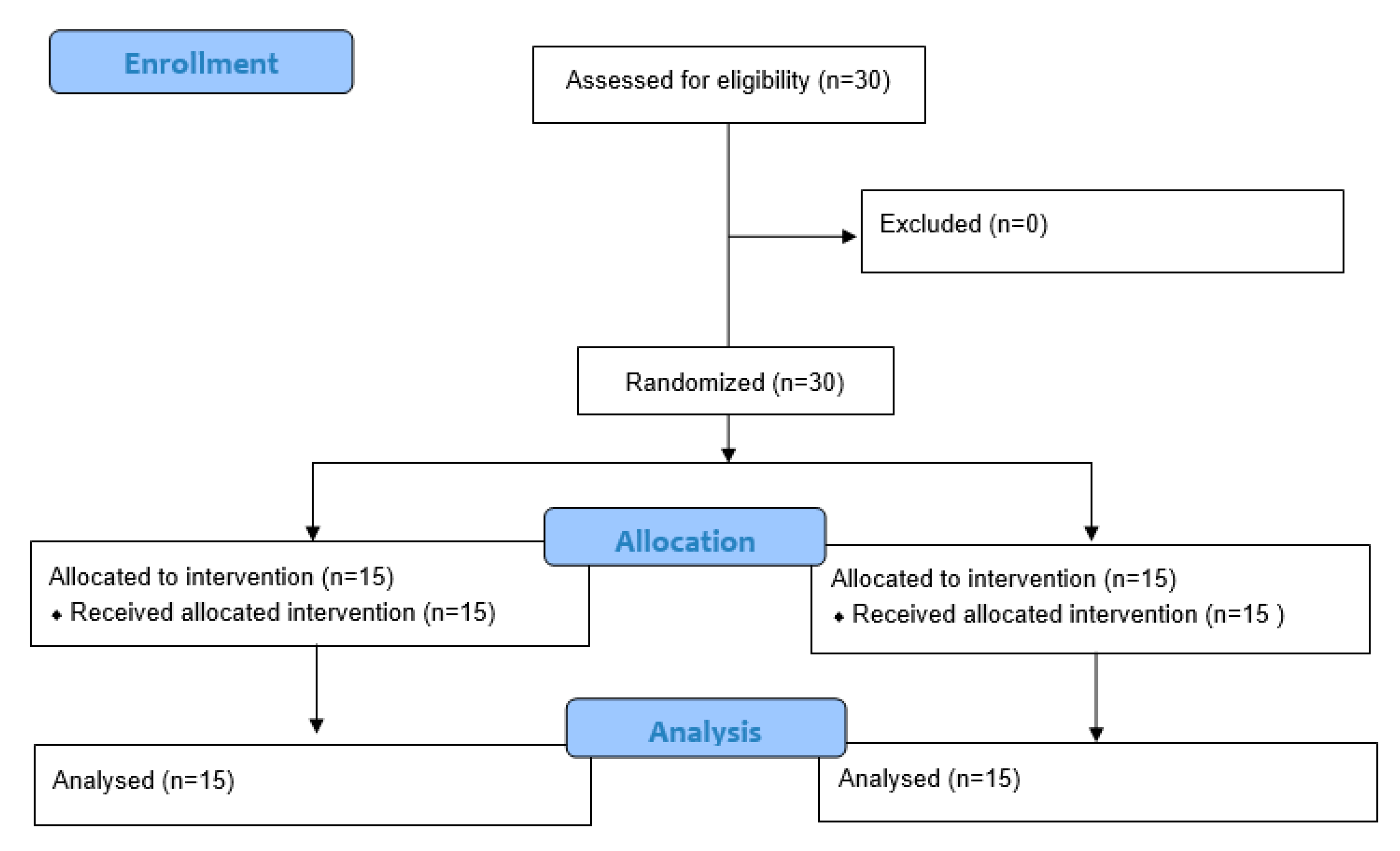
2.1. Study Participants
2.2. Experimental Procedure
2.3. Outcome Measurements
2.4. Intervention
2.5. Statistical Analysis
3. Results
3.1. Demographic Characteristics of Participants (N = 30)
3.2. Clinical Outcome Measurements
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CP | Cerebral palsy |
| XR | Extended reality |
| VR | Virtual reality |
| AR | Augmented reality |
| MR | Mixed reality |
| GMFCS | Gross motor function classification system |
| XRT | Extended reality training group |
| CPT | Conventional physical therapy group |
| ADL | Activities daily living |
| GMFM | 88-Gross motor function measure-88 |
| PBS | Pediatric balance scale |
| PSI | Parenting stress index, fourth edition |
| PedsQL | Pediatric quality of life inventory |
| NDT | Neurodevelopmental treatment |
References
- Laube, W.; Sengoelge, M. Cerebral Palsy Link to Sensorimotor System, Cognition, Emotion and Nociplastic Pain. Children 2025, 12, 702. [Google Scholar] [CrossRef] [PubMed]
- Pettersson, K.; Rodby-Bousquet, E. Living Conditions and Social Outcomes in Adults with Cerebral Palsy. Front. Neurol. 2021, 12, 749389. [Google Scholar] [CrossRef] [PubMed]
- Jiang, B.; Walstab, J.; Reid, S.M.; Davis, E.; Reddihough, D. Quality of Life in Young Adults with Cerebral Palsy. Disabil. Health J. 2016, 9, 673–681. [Google Scholar] [CrossRef] [PubMed]
- Anttila, H.; Autti-Rämö, I.; Suoranta, J.; Mäkelä, M.; Malmivaara, A. Effectiveness of Physical Therapy Interventions for Children with Cerebral Palsy: A Systematic Review. BMC Pediatr. 2008, 8, 14. [Google Scholar] [CrossRef] [PubMed]
- Te Velde, A.; Morgan, C.; Finch-Edmondson, M.; McNamara, L.; McNamara, M.; Paton, M.C.B.; Stanton, E.; Webb, A.; Badawi, N.; Novak, I. Neurodevelopmental Therapy for Cerebral Palsy: A Meta-Analysis. Pediatrics 2022, 149, e2021055061. [Google Scholar] [CrossRef] [PubMed]
- Ravi, D.K.; Kumar, N.; Singhi, P. Effectiveness of Virtual Reality Rehabilitation for Children and Adolescents with Cerebral Palsy: An Updated Evidence-Based Systematic Review. Physiotherapy 2017, 103, 245–258. [Google Scholar] [CrossRef] [PubMed]
- Demers, M.; Fung, K.; Subramanian, S.K.; Lemay, M.; Robert, M.T. Integration of Motor Learning Principles into Virtual Reality Interventions for Individuals with Cerebral Palsy: Systematic Review. JMIR Serious Games 2021, 9, e23822. [Google Scholar] [CrossRef] [PubMed]
- Macchitella, L.; Accogli, G.; Barraco, G.; Nicolardi, V.; Pirani, G.; Ferrante, C.; Oliva, M.C.; Fanizza, I.; Gallo, I.; De Rinaldis, M. A Two-Step Neurorehabilitation Program Utilizing Extended Reality and Telerehabilitation for Children with Cerebral Palsy: A Pilot Study on Effectiveness, Adherence, and Technical Feasibility. Appl. Sci. 2024, 14, 11961. [Google Scholar] [CrossRef]
- Chang, H.J.; Ku, K.H.; Park, Y.S.; Park, J.G.; Cho, E.S.; Seo, J.S.; Kim, C.W.; Hwi O, S. Effects of Virtual Reality-Based Rehabilitation on Upper Extremity Function among Children with Cerebral Palsy. Healthcare 2020, 8, 391. [Google Scholar] [CrossRef] [PubMed]
- AlSaif, A.A.; Alsenany, S. Effects of Interactive Games on Motor Performance in Children with Spastic Cerebral Palsy. J. Phys. Ther. Sci. 2015, 27, 2001–2003. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Wang, X.; Chen, R.; Zhang, J. The Effects of Virtual Reality Training on Balance, Gross Motor Function, and Daily Living Ability in Children with Cerebral Palsy: Systematic Review and Meta-Analysis. JMIR Serious Games 2022, 10, e38972. [Google Scholar] [CrossRef] [PubMed]
- Ko, J.; Kim, M. Reliability and Responsiveness of the Gross Motor Function Measure-88 in Children with Cerebral Palsy. Phys. Ther. 2013, 93, 393–400. [Google Scholar] [CrossRef] [PubMed]
- Franjoine, M.R.; Gunther, J.S.; Taylor, M.J. Pediatric Balance Scale: A Modified Version of the Berg Balance Scale for the School-Age Child with Mild to Moderate Motor Impairment. Pediatr. Phys. Ther. 2003, 15, 114–128. [Google Scholar] [CrossRef] [PubMed]
- Ottenbacher, K.J.; Hsu, Y.; Granger, C.V.; Fiedler, R.C. The Reliability of the Functional Independence Measure: A Quantitative Review. Arch. Phys. Med. Rehabil. 1996, 77, 1226–1232. [Google Scholar] [CrossRef] [PubMed]
- Ríos, M.; Zekri, S.; Alonso-Esteban, Y.; Navarro-Pardo, E. Parental Stress Assessment with the Parenting Stress Index (PSI): A Systematic Review of Its Psychometric Properties. Children 2022, 9, 1649. [Google Scholar] [CrossRef] [PubMed]
- Varni, J.W.; Limbers, C.A. The Pediatric Quality of Life Inventory: Measuring Pediatric Health-Related Quality of Life from the Perspective of Children and Their Parents. Pediatr. Clin. N. Am. 2009, 56, 843–863. [Google Scholar] [CrossRef] [PubMed]
- Zanon, M.A.; Pacheco, R.L.; de Latorraca, C.O.C.; Martimbianco, A.L.C.; Pachito, D.V.; Riera, R. Neurodevelopmental Treatment (Bobath) for Children with Cerebral Palsy: A Systematic Review. J. Child. Neurol. 2019, 34, 679–686. [Google Scholar] [CrossRef] [PubMed]
- Lovell, B.; Wetherell, M.A. Do Virtual Reality Relaxation Experiences Alleviate Stress in Parents of Children with Autism? A Pilot Study. J. Child. Fam. Stud. 2024, 33, 2134–2141. [Google Scholar] [CrossRef]
- Pallavicini, F.; Orena, E.; Arnoldi, L.; Achille, F.; Stefanini, S.; Cassa, M.; Pepe, A.; Veronese, G.; Bernardelli, L.; Sforza, F. Effects and Acceptability of a 1-Week Home-Based Virtual Reality Training for Supporting the Management of Stress and Anxiety: Randomized Pilot Trial. JMIR Serious Games 2025, 13, e50326. [Google Scholar] [CrossRef] [PubMed]
- Björling, E.A.; Sonney, J.; Zade, H.; Rodriguez, S.; Pullmann, M.D.; Moon, S.H. Using Virtual Reality to Reduce Stress in Adolescents: Mixed Methods Usability Study. JMIR XR Spat. Comput. 2024, 1, e49171. [Google Scholar] [CrossRef]
- Carlier, S.; Van der Paelt, S.; Ongenae, F.; De Backere, F.; De Turck, F. Empowering Children with ASD and Their Parents: Design of a Serious Game for Anxiety and Stress Reduction. Sensors 2020, 20, 966. [Google Scholar] [CrossRef] [PubMed]
- Scherpbier, I.C.A.; Abrahamse, M.E.; Widdershoven, G.A.M.; Belleman, R.G.; Popma, A.; Lindauer, R.J.L. The Added Value of Virtual Reality to Parent–Child Interaction Therapy: A Qualitative Study with Parents and Therapists. BMC Digit. Health 2024, 2, 19. [Google Scholar] [CrossRef]

| CPT (n = 15) | XRT (n = 15) | p-Value | |
|---|---|---|---|
| Sex (male/female) | 10/5 | 12/3 | 0.41 |
| Age (years) | 14.23 ± 2.88 | 15.42 ± 3.16 | 0.35 |
| Body height (cm) | 128.63 ± 19.27 | 129.6 ± 14.23 | 0.25 |
| Body mass (kg) | 29.13 ± 14.08 | 31.43 ± 10.76 | 0.36 |
| GMFCS (I/II/III) a | 4/6/5 | 5/5/5 | 0.89 |
| CPT | XRT | p-Value | |||||
|---|---|---|---|---|---|---|---|
| Pre-Test | Post-Test | With Group (Effect Size) | Pre-Test | Post-Test | With Group (Effect Size) | Time × Group | |
| GMFM 88 a | 67.15 ± 18.42 | 71.12 ± 16.88 | 0.012 * (0.22) | 68.08 ± 17.78 | 72.83 ± 15.82 | 0.018 * (0.28) | 0.565 |
| PBS b | 28.12 ± 12.56 | 28.88 ± 10.23 | 0.04 * (0.1) | 16.68 ± 14.23 | 25.11 ± 8.88 | 0.001 * (0.71) | 0.092 |
| FIM c | 20.17 ± 8.21 | 20.90 ± 8.12 | 0.03 * (0.1) | 20.25 ± 5.21 | 21.02 ± 7.23 | 0.04 * (0.1) | 0.095 |
| CPT | XRT | p-Value | |||||
|---|---|---|---|---|---|---|---|
| Pre-Test | Post-Test | With Group (Effect Size) | Pre-Test | Post-Test | With Group (Effect Size) | Time × Group | |
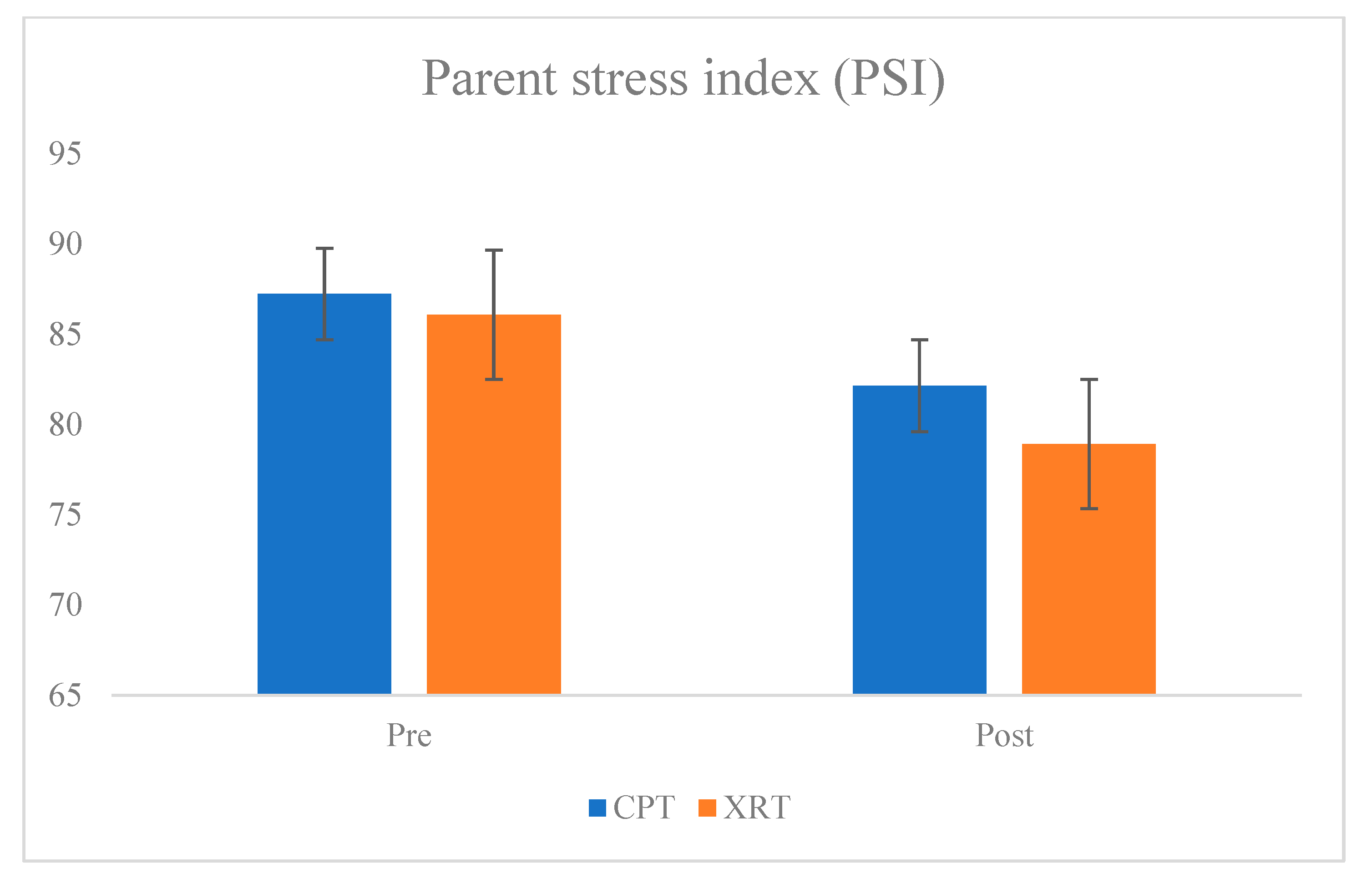
| PSI a | 87.23 ± 16.23 | 82.15 ± 14.88 | 0.01 * (0.3) | 86.08 ± 14.83 | 78.92 ± 10.83 | 0.001 * (0.55) | 0.107 |
| PedsQL b | 50.25 ± 18.21 | 44.80 ± 15.83 | 0.02 * (0.32) | 50.89 ± 16.22 | 44.48 ± 17.26 | 0.01 * (0.38) | 0.14 |
| Outcome Measure | F (Time × Group) | p-Value | Partial η2 |
|---|---|---|---|
| GMFM-88 a | 0.99 | 0.329 | 0.035 |
| PBS b | 1.24 | 0.274 | 0.043 |
| FIM c | 1.05 | 0.315 | 0.037 |
| PSI d | 3.76 | 0.065 | 0.059 |
| PedsQL e | 0.79 | 0.381 | 0.029 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lim, O.; Kim, Y.; Park, C. Preliminary Effects of Extended Reality-Based Rehabilitation on Gross Motor Function, Balance, and Psychosocial Health in Children with Cerebral Palsy. Bioengineering 2025, 12, 779. https://doi.org/10.3390/bioengineering12070779
Lim O, Kim Y, Park C. Preliminary Effects of Extended Reality-Based Rehabilitation on Gross Motor Function, Balance, and Psychosocial Health in Children with Cerebral Palsy. Bioengineering. 2025; 12(7):779. https://doi.org/10.3390/bioengineering12070779
Chicago/Turabian StyleLim, Onebin, Yunhwan Kim, and Chanhee Park. 2025. "Preliminary Effects of Extended Reality-Based Rehabilitation on Gross Motor Function, Balance, and Psychosocial Health in Children with Cerebral Palsy" Bioengineering 12, no. 7: 779. https://doi.org/10.3390/bioengineering12070779
APA StyleLim, O., Kim, Y., & Park, C. (2025). Preliminary Effects of Extended Reality-Based Rehabilitation on Gross Motor Function, Balance, and Psychosocial Health in Children with Cerebral Palsy. Bioengineering, 12(7), 779. https://doi.org/10.3390/bioengineering12070779







