Optimal Sites for Upper Extremity Amputation: Comparison Between Surgeons and Prosthetists
Abstract
1. Introduction
2. Methods
3. Prosthetic Device Types
4. Review of Surgeons’ Versus Prosthetists’ Recommended Amputation Lengths
4.1. Digit Amputation
4.1.1. Surgical Recommendations
4.1.2. Prosthetist Recommendations
4.2. Partial Hand/Transcarpal Amputation
4.2.1. Surgical Recommendations
4.2.2. Prosthetist Recommendations
4.3. Wrist Disarticulation
4.3.1. Surgical Recommendations
4.3.2. Prosthetist Recommendations
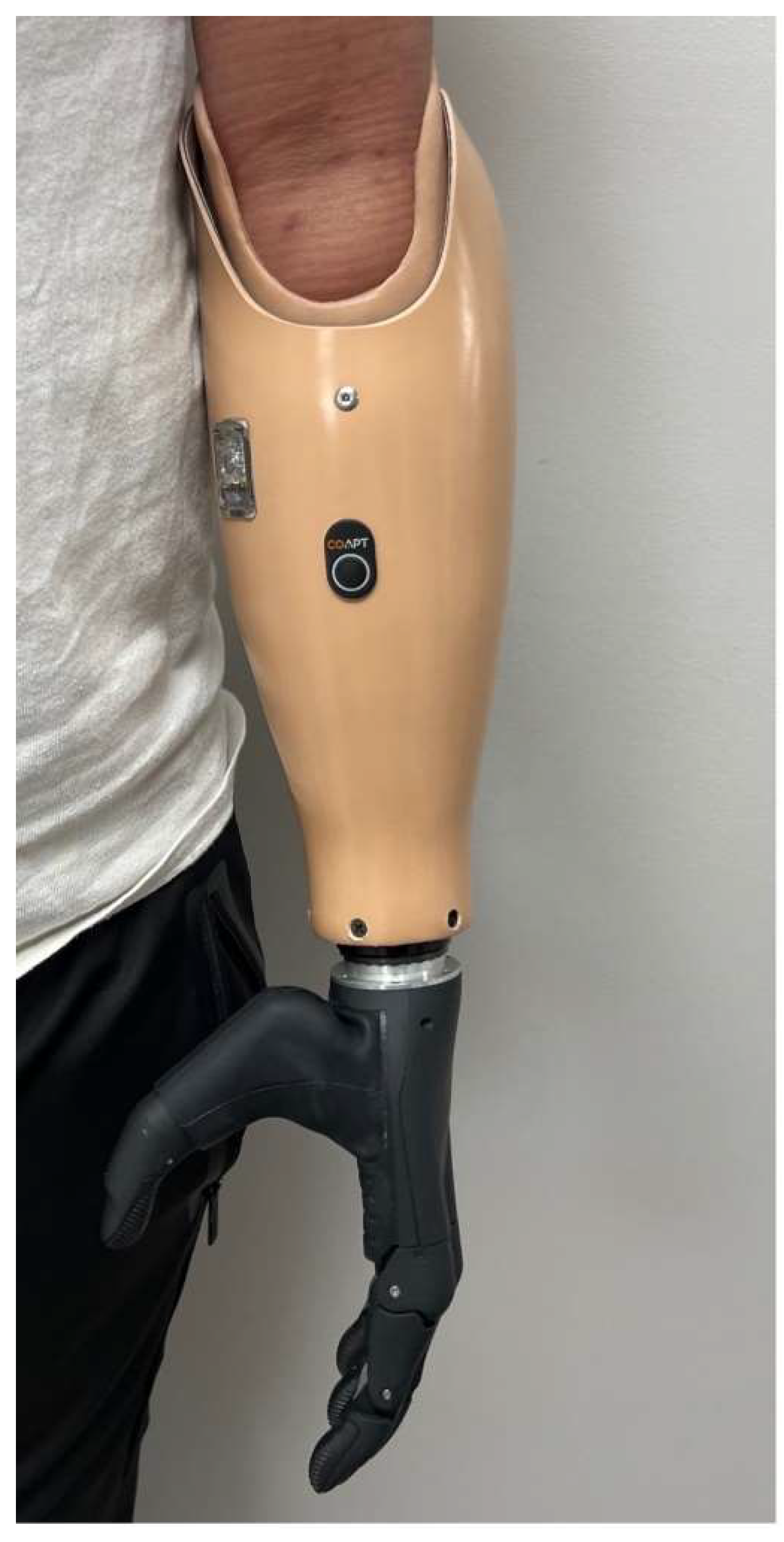
4.4. Transradial Amputation
4.4.1. Surgical Recommendations
4.4.2. Prosthetist Recommendations
4.5. Elbow Disarticulation
4.5.1. Surgical Recommendations
4.5.2. Prosthetist Recommendations
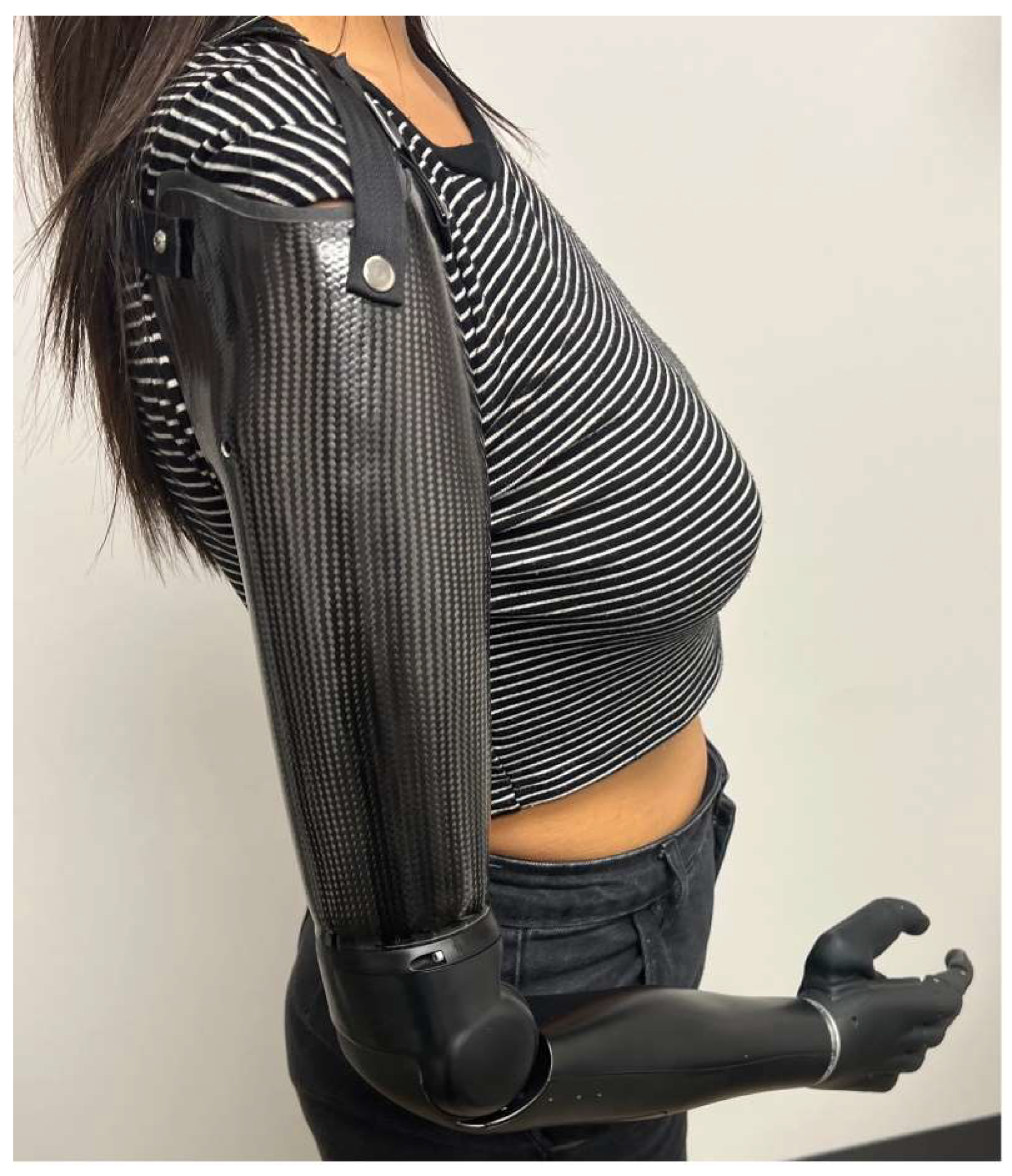
4.6. Transhumeral Amputation
4.6.1. Surgical Recommendations
4.6.2. Prosthetist Recommendations
4.7. Shoulder Disarticulation
4.7.1. Surgical Recommendations
4.7.2. Prosthetist Recommendations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ziegler-Graham, K.; MacKenzie, E.J.; Ephraim, P.L.; Travison, T.G.; Brookmeyer, R. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Arch. Phys. Med. Rehabil. 2008, 89, 422–429. [Google Scholar] [CrossRef] [PubMed]
- Bowker, J.H.; Michael, J.W. Atlas of Limb Prosthetics: Surgical, Prosthetic, and Rehabilitation Principles; Mosby Inc.: Maryland, MO, USA, 1992. [Google Scholar]
- Behrend, C.; Reizner, W.; Marchessault, J.A.; Hammert, W.C. Update on advances in upper extremity prosthetics. J. Hand Surg. Am. 2011, 36, 1711–1717. [Google Scholar] [CrossRef] [PubMed]
- Tennent, D.J.; Wenke, J.C.; Rivera, J.C.; Krueger, C.A. Characterisation and outcomes of upper extremity amputations. Injury 2014, 45, 965–969. [Google Scholar] [CrossRef] [PubMed]
- Ro, J.-S.; Leigh, J.-H.; Jeon, I.; Bang, M.S. Trends in burden of work-related upper limb amputation in South Korea, 2004–2013: A nationwide retrospective cohort study. BMJ Open 2019, 9, e032793. [Google Scholar] [CrossRef] [PubMed]
- Østlie, K.; Magnus, P.; Skjeldal, O.H.; Garfelt, B.; Tambs, K. Mental health and satisfaction with life among upper limb amputees: A Norwegian population-based survey comparing adult acquired major upper limb amputees with a control group. Disabil. Rehabil. 2011, 33, 1594–1607. [Google Scholar] [CrossRef] [PubMed]
- Flaubert, J.L.; Spicer, C.M.; Jette, A.M. The Promise of Assistive Technology to Enhance Activity and Work Participation; The National Academic Press: Washington, DC, USA, 2017. [Google Scholar]
- Jang, C.H.; Yang, H.S.; Yang, H.E.; Lee, S.Y.; Kwon, J.W.; Yun, B.D.; Choi, J.Y.; Kim, S.N.; Jeong, H.W. A survey on activities of daily living and occupations of upper extremity amputees. Ann. Rehabil. Med. 2011, 35, 907–921. [Google Scholar] [CrossRef] [PubMed]
- Raichle, K.A.; Hanley, M.A.; Molton, I.; Kadel, N.J.; Campbell, K.; Phelps, E.; Ehde, D.; Smith, D.G. Prosthesis use in persons with lower-and upper-limb amputation. J. Rehabil. Res. Dev. 2008, 45, 961. [Google Scholar] [CrossRef] [PubMed]
- Resnik, L.; Borgia, M.; Clark, M. Function and quality of life of unilateral major upper limb amputees: Effect of prosthesis use and type. Arch. Phys. Med. Rehabil. 2020, 101, 1396–1406. [Google Scholar] [CrossRef] [PubMed]
- Tintle, L.S.M.; Baechler, L.M.F.; Nanos, C.G.P., III; Forsberg, L.J.A.; Potter, M.B.K. Traumatic and trauma-related amputations: Part II: Upper extremity and future directions. J. Bone Jt. Surg. 2010, 92, 2934–2945. [Google Scholar] [CrossRef] [PubMed]
- Wright, T.W.; Hagen, A.D.; Wood, M.B. Prosthetic usage in major upper extremity amputations. J. Hand Surg. 1995, 20, 619–622. [Google Scholar] [CrossRef] [PubMed]
- Biddiss, E.A.; Chau, T.T. Upper limb prosthesis use and abandonment: A survey of the last 25 years. Prosthet. Orthot. Int. 2007, 31, 236–257. [Google Scholar] [CrossRef] [PubMed]
- Biddiss, E.A.; Chau, T.T. Multivariate prediction of upper limb prosthesis acceptance or rejection. Disabil. Rehabil. Assist. Technol. 2008, 3, 181–192. [Google Scholar] [CrossRef] [PubMed]
- Biddiss, E.; Chau, T. Upper-limb prosthetics: Critical factors in device abandonment. Am. J. Phys. Med. Rehabil. 2007, 86, 977–987. [Google Scholar] [CrossRef] [PubMed]
- Solarz, M.K.; Thoder, J.J.; Rehman, S. Management of major traumatic upper extremity amputations. Orthop. Clin. 2016, 47, 127–136. [Google Scholar] [CrossRef] [PubMed]
- Lake, C. Partial hand amputation: Prosthetic management. Atlas Amputations Limb Defic. Surg. Prosthet. Rehabil. Princ. 2004, 3, 209–217. [Google Scholar]
- Bates, T.J.; Fergason, J.R.; Pierrie, S.N. Technological advances in prosthesis design and rehabilitation following upper extremity limb loss. Curr. Rev. Musculoskelet. Med. 2020, 13, 485–493. [Google Scholar] [CrossRef] [PubMed]
- Carey, S.L.; Lura, D.J.; Highsmith, M.J. Differences in myoelectric and body-powered upper-limb prostheses: Systematic literature review. J. Rehabil. Res. Dev. 2015, 52, 247–262. [Google Scholar] [CrossRef] [PubMed]
- Kejlaa, G. Consumer concerns and the functional value of prostheses to upper limb amputees. Prosthet. Orthot. Int. 1993, 17, 157–163. [Google Scholar] [CrossRef] [PubMed]
- Williams, T.W., III. Progress on stabilizing and controlling powered upper-limb prostheses. J. Rehabil. Res. Dev. 2011, 48, ix. [Google Scholar] [CrossRef] [PubMed]
- Resnik, L.; Meucci, M.R.; Lieberman-Klinger, S.; Fantini, C.; Kelty, D.L.; Disla, R.; Sasson, N. Advanced upper limb prosthetic devices: Implications for upper limb prosthetic rehabilitation. Arch. Phys. Med. Rehabil. 2012, 93, 710–717. [Google Scholar] [CrossRef] [PubMed]
- Uellendahl, J.E. Upper extremity myoelectric prosthetics. Phys. Med. Rehabil. Clin. N. Am. 2000, 11, 639–652. [Google Scholar] [CrossRef]
- Silcox, D., 3rd; Rooks, M.D.; Vogel, R.R.; Fleming, L.L. Myoelectric prostheses. A long-term follow-up and a study of the use of alternate prostheses. JBJS 1993, 75, 1781–1789. [Google Scholar] [CrossRef] [PubMed]
- Hafshejani, M.K.; Javanshir, M.; Kamali, K.; Ghasemi, M.; Emami, M.; Esmaeeli, S.; Langari, A.; Sattari Naeini, M. The comparison of psychological and social adaptation below elbow amputation men using a mechanical and myoelectric prosthesis by using of TAPES questionnaire. Life Sci. J. 2012, 9, 5583–5587. [Google Scholar]
- Simon, A.M.; Lock, B.A.; Stubblefield, K.A. Patient training for functional use of pattern recognition–controlled prostheses. JPO J. Prosthet. Orthot. 2012, 24, 56–64. [Google Scholar] [CrossRef] [PubMed]
- Huang, M.E.; Levy, C.E.; Webster, J.B. Acquired limb deficiencies. 3. Prosthetic components, prescriptions, and indications. Arch. Phys. Med. Rehabil. 2001, 82, S17–S24. [Google Scholar] [CrossRef] [PubMed]
- Lotze, M.; Grodd, W.; Birbaumer, N.; Erb, M.; Huse, E.; Flor, H. Does use of a myoelectric prosthesis prevent cortical reorganization and phantom limb pain? Nat. Neurosci. 1999, 2, 501–502. [Google Scholar] [CrossRef] [PubMed]
- Bouffard, J.; Vincent, C.; Boulianne, É.; Lajoie, S.; Mercier, C. Interactions between the phantom limb sensations, prosthesis use, and rehabilitation as seen by amputees and health professionals. JPO J. Prosthet. Orthot. 2012, 24, 25–33. [Google Scholar] [CrossRef]
- Madusanka, D.; Wijayasingha, L.; Gopura, R.; Amarasinghe, Y.; Mann, G. A review on hybrid myoelectric control systems for upper limb prosthesis. In Proceedings of the 2015 Moratuwa Engineering Research Conference (MERCon), Moratuwa, Sri Lanka, 7–8 April 2015; pp. 136–141. [Google Scholar]
- Childress, D.S. Upper-limb prosthetics: Control of limb prostheses. In Atlas of Limb Prosthetics: Surgical, Prosthetic, and Rehabilitation Principles; American Academy of Orthopaedic Surgeons: Rosemont, IL, USA, 1992. [Google Scholar]
- Billock, J. Upper limb prosthetic management hybrid design approaches. Clin. Prosthet. Orthot. 1985, 9, 23–25. [Google Scholar]
- Zhang, H.L.J.; Liu, S.; Zhang, W.; Lu, Y.; Yang, S.; Yin, R.; Shen, D. Flexible Under-Actuated Bionic Hand. CN110216700B. 2018. Available online: https://patents.google.com/patent/CN110216700B/en?oq=CN110216700B%2c+++华东理工大学%2c+仿生假肢手 (accessed on 13 July 2025).
- Liu, S.; Zhang, H.; Yin, R.; Chen, A.; Zhang, W. Flexure hinge based fully compliant prosthetic finger. In Proceedings of the SAI Intelligent Systems Conference (IntelliSys) 2016, London, UK, 21–22 September 2016; Springer: Berlin/Heidelberg, Germany, 2018; Volume 2, pp. 839–849. [Google Scholar]
- Reavey, P.L.; Stranix, J.T.; Muresan, H.; Soares, M.; Thanik, V. Disappearing digits: Analysis of national trends in amputation and replantation in the United States. Plast. Reconstr. Surg. 2018, 141, 857e–867e. [Google Scholar] [CrossRef] [PubMed]
- Win, T.S.; Henderson, J. Management of traumatic amputations of the upper limb. BMJ 2014, 348, g255. [Google Scholar] [CrossRef] [PubMed]
- Banerjee, S.N. Rehabilitation Management of Amputees; Williams & Wilkins: Philadelphia, PA, USA, 1982. [Google Scholar]
- Ovadia, S.A.; Askari, M. Upper extremity amputations and prosthetics. In Seminars in Plastic Surgery; Thieme Medical Publishers: New York, NY, USA, 2015; pp. 055–061. [Google Scholar]
- Dellon, A.L. The moving two-point discrimination test: Clinical evaluation of the quickly adapting fiber/receptor system. J. Hand Surg. 1978, 3, 474–481. [Google Scholar] [CrossRef] [PubMed]
- Dellon, A.L. “Think nerve” in upper extremity reconstruction. Clin. Plast. Surg. 1989, 16, 617–627. [Google Scholar] [CrossRef] [PubMed]
- Dumanian, G.; Souza, J.; Kuiken, T. Treatment of the upper extremity amputee. In Plastic Surgery: Volume 6: Hand and Upper Extremity; Elsevier: Amsterdam, The Netherlands, 2018; pp. 894–904. [Google Scholar]
- Graham, W.P.; Kilgore, E.S.; Whitaker, L.A. Transarticular digital joint amputations: Preservation of the articular cartilage. Hand 1973, 5, 58–62. [Google Scholar] [CrossRef] [PubMed]
- Graham, E.M.; Hendrycks, R.; Baschuk, C.M.; Atkins, D.J.; Keizer, L.; Duncan, C.C.; Mendenhall, S.D. Restoring Form and Function to the Partial Hand Amputee: Prosthetic Options from the Fingertip to the Palm. Hand Clin. 2021, 37, 167–187. [Google Scholar] [CrossRef] [PubMed]
- Denduluri, S.K.; Rees, A.; Nord, K.M.; Loeffler, B.J.; Gaston, R.G. The Starfish Procedure for Independent Digital Control of a Myoelectric Prosthesis. Tech. Hand Up. Extrem. Surg. 2023, 27, 61–67. [Google Scholar] [CrossRef] [PubMed]
- Grier, A.J.; Loeffler, B.J.; Gaston, R.G. Starfish Procedure. Hand Clin. 2021, 37, 447–455. [Google Scholar] [CrossRef] [PubMed]
- Odeyemi, J.; Ogbeyemi, A.; Wong, K.; Zhang, W. On automated object grasping for intelligent prosthetic hands using machine learning. Bioengineering 2024, 11, 108. [Google Scholar] [CrossRef] [PubMed]
- Pasquina, P.F.; Cooper, R.A. Care of the Combat Amputee; Office of the Surgeon General, United States Army: Falls Church, VA, USA, 2009. [Google Scholar]
- Maduri, P.; Akhondi, H. Upper Limb Amputation; StatPearls Publishing: Treasure Island, FL, USA, 2019. [Google Scholar]
- Fitzgibbons, P.; Medvedev, G. Functional and clinical outcomes of upper extremity amputation. JAAOS J. Am. Acad. Orthop. Surg. 2015, 23, 751–760. [Google Scholar] [CrossRef] [PubMed]
- Lake, C.; Dodson, R. Progressive upper limb prosthetics. Phys. Med. Rehabil. Clin. 2006, 17, 49–72. [Google Scholar] [CrossRef] [PubMed]
- Schultz, A.E.; Baade, S.P.; Kuiken, T.A. Expert opinions on success factors for upper-limb prostheses. J. Rehabil. Res. Dev. 2007, 44, 483. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, T.W.; Williamson, M.L.; Elliott, T.R.; Jackson, W.T.; Kearns, N.T.; Ryan, T. Psychological distress among persons with upper extremity limb loss. Br. J. Health Psychol. 2019, 24, 746–763. [Google Scholar] [CrossRef] [PubMed]
- Kuiken, T.A.; Dumanian, G.A.; Lipschutz, R.D.; Miller, L.A.; Stubblefield, K. The use of targeted muscle reinnervation for improved myoelectric prosthesis control in a bilateral shoulder disarticulation amputee. Prosthet. Orthot. Int. 2004, 28, 245–253. [Google Scholar] [CrossRef] [PubMed]
- Mereu, F.; Leone, F.; Gentile, C.; Cordella, F.; Gruppioni, E.; Zollo, L. Control strategies and performance assessment of upper-limb TMR prostheses: A review. Sensors 2021, 21, 1953. [Google Scholar] [CrossRef] [PubMed]
- Morgan, E.N.; Potter, B.K.; Souza, J.M.; Tintle, S.M.; Nanos, G.P., III. Targeted muscle reinnervation for transradial amputation: Description of operative technique. Tech. Hand Up. Extrem. Surg. 2016, 20, 166–171. [Google Scholar] [CrossRef] [PubMed]
- Souza, J.M.; Cheesborough, J.E.; Ko, J.H.; Cho, M.S.; Kuiken, T.A.; Dumanian, G.A. Targeted muscle reinnervation: A novel approach to postamputation neuroma pain. Clin. Orthop. Relat. Res. 2014, 472, 2984–2990. [Google Scholar] [CrossRef] [PubMed]
- Mathew, P.J.; Rakoczy, K.D.; Fullerton, N.; Dodds, S.D.; Hui-Chou, H.G. Elbow joint salvage in pediatric traumatic amputation with targeted muscle reinnervation, external tissue expansion, and free muscle flap–A case report. Orthoplastic Surg. 2022, 9, 9–13. [Google Scholar] [CrossRef]
- Luccia, N.D.; Marino, H. Case study: Fitting of electronic elbow on an elbow disarticulated patient by means of a new surgical technique. Prosthet. Orthot. Int. 2000, 24, 247–251. [Google Scholar] [CrossRef] [PubMed]
- Cheesborough, J.E.; Smith, L.H.; Kuiken, T.A.; Dumanian, G.A. Targeted muscle reinnervation and advanced prosthetic arms. In Seminars in Plastic Surgery; Thieme Medical Publishers: New York, NY, USA, 2015; pp. 062–072. [Google Scholar]
- Bowker, J.H.; Carneiro, R.S.; Clark, C.R.; Gailey, R.S.; Poonekar, P.D.; Mnaymneh, W.; Ouellette, E.A. Atlas of Limb Prosthetics: Surgical, Prosthetic, and Rehabilitation Principles, 2nd ed.; Mosby Year Book: St. Louis, MO, USA, 1992. [Google Scholar]
- Levine, E.A.; Warso, M.A.; McCoy, D.M.; TK, D.G. Forequarter amputation for soft tissue tumors. Am. Surg. 1994, 60, 367–370. [Google Scholar] [PubMed]
- Gart, M.S.; Souza, J.M.; Dumanian, G.A. Targeted muscle reinnervation in the upper extremity amputee: A technical roadmap. J. Hand Surg. 2015, 40, 1877–1888. [Google Scholar] [CrossRef] [PubMed]
- Kulkarni, A.; Luthringer, M.; Fried, A.; Mikosz, M.; Mauro, J.; Vella, G.R.; Lally, T.; Shah, A. Building a Multidisciplinary Clinic Dedicated to Upper-Extremity Limb Loss. J. Hand Surg. 2024, 49, 267–274. [Google Scholar] [CrossRef] [PubMed]





| Type | Advantages | Drawbacks | Examples |
|---|---|---|---|
| Passive Functional Prosthetics (PFPs) | High cosmesis Waterproof Lightweight | Minimal function | Vincent Passive Thumb, Titan Thumb, M-Thumb, Regal Prosthesis Ltd., Livingskin, Point Partial, Point Digit, Grip Lock, Point Digit, Grip Lock, Titan Full, Vincent Passive |
| Body-Powered (BP) Prosthetics | Durable Waterproof | Low cosmesis Heavy Lower fine motor control | Thumb Driver, PIP Driver, MCP Driver, Partial M-Finger, Robin-Aids, M-Fingers |
| Myoelectric (MYO) Prosthetics | Fine motor control Moderate cosmesis Lightweight | Fragile Expensive | Ossur iDigits, Vincent Partial Hand |
| Type of Terminal Device | Prosthetic Brand | Available Sizing |
|---|---|---|
| Myohands | COVVI | Small: 6.75″, Medium: 7.75″, Large: 7.75″ |
| Bebionic | Small: 6.50″, Medium: 7.50″, Large: 7.875 | |
| Taska | 7.75″ or 8.25″ | |
| Taska CX | 7.25″ | |
| Body-Powered Hook | Hosmer 5x | Adult: 4.9″ |
| Hosmer 99x | Adult Small: 3.9″ | |
| Myo Elbows | Utah Power U3 | 2.5″ to elbow center, 4″ to ulnar surface |
| Steeper Espire | 1.89″ | |
| Motion Arm | 1.5″ |
| Site of Amputation | Prosthetics Recommended | Minimum Residual Length | Maximum Residual Length | Other Considerations |
|---|---|---|---|---|
| Thumb | PFP or BP prosthesis | Preserve as much length as possible | ||
| Phalanges Distal to DIP | PFP | Preserve as much length as possible | ||
| Phalanges Proximal to DIP | PFP or BP prosthesis | Consider more proximal mid-phalanx amputation over disarticulation for digit symmetry | Ensure adequate soft tissue coverage to prevent painful stumps | Ray amputation can be considered in cases with central digit involvement |
| Metacarpals | PFP, BP, or MYO | Must retain enough length for functional grip | Consider thin flap coverage | Starfish procedure may be performed if MYO device desired |
| Wrist | PFP, BP, or MYO prosthesis with low-profile wrist unit | Not ideal for prosthetics due to limb length discrepancy | Preserve ulnar styloid and extensor tendon | |
| Radius | BP or MYO prosthesis | Retain at least 4 cm of the ulna from the olecranon | Must allow room for terminal device + socket (~22.5 cm from lateral epicondyle) | If TMR is desired, at least 7–8 cm of distal radius should be resected |
| Elbow | BP or hybrid design | Not ideal for prosthetics due to limb length discrepancy | Humeral midshaft osteotomy can improve symmetry and control while preserving humeral condyles | |
| Humerus | Hybrid design with BP elbow and myoelectric hand | Retain at least 5–7 cm (or 25–30%) of humeral length from the acromion | Must allow room for terminal device + socket (~14 cm from acromion) | Humeral angle or midshaft osteotomy can improve suspension and rotational control |
| Shoulder | MYO prosthesis with X-Frame socket | Preserve scapula and deltoid for shoulder contour and prosthetic control | Ensure adequate soft tissue coverage for prosthetic suspension | TMR should be highly considered |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Apagüeño, B.; Munkwitz, S.E.; Mata, N.V.; Alessia, C.; Nayak, V.V.; Coelho, P.G.; Fullerton, N. Optimal Sites for Upper Extremity Amputation: Comparison Between Surgeons and Prosthetists. Bioengineering 2025, 12, 765. https://doi.org/10.3390/bioengineering12070765
Apagüeño B, Munkwitz SE, Mata NV, Alessia C, Nayak VV, Coelho PG, Fullerton N. Optimal Sites for Upper Extremity Amputation: Comparison Between Surgeons and Prosthetists. Bioengineering. 2025; 12(7):765. https://doi.org/10.3390/bioengineering12070765
Chicago/Turabian StyleApagüeño, Brandon, Sara E. Munkwitz, Nicholas V. Mata, Christopher Alessia, Vasudev Vivekanand Nayak, Paulo G. Coelho, and Natalia Fullerton. 2025. "Optimal Sites for Upper Extremity Amputation: Comparison Between Surgeons and Prosthetists" Bioengineering 12, no. 7: 765. https://doi.org/10.3390/bioengineering12070765
APA StyleApagüeño, B., Munkwitz, S. E., Mata, N. V., Alessia, C., Nayak, V. V., Coelho, P. G., & Fullerton, N. (2025). Optimal Sites for Upper Extremity Amputation: Comparison Between Surgeons and Prosthetists. Bioengineering, 12(7), 765. https://doi.org/10.3390/bioengineering12070765






