Evaluation of Mandibular Bone Alterations by Panoramic Radiography: A Potential Tool in the Identification of Signs of Osteopenia and Osteoporosis
Abstract
1. Introduction
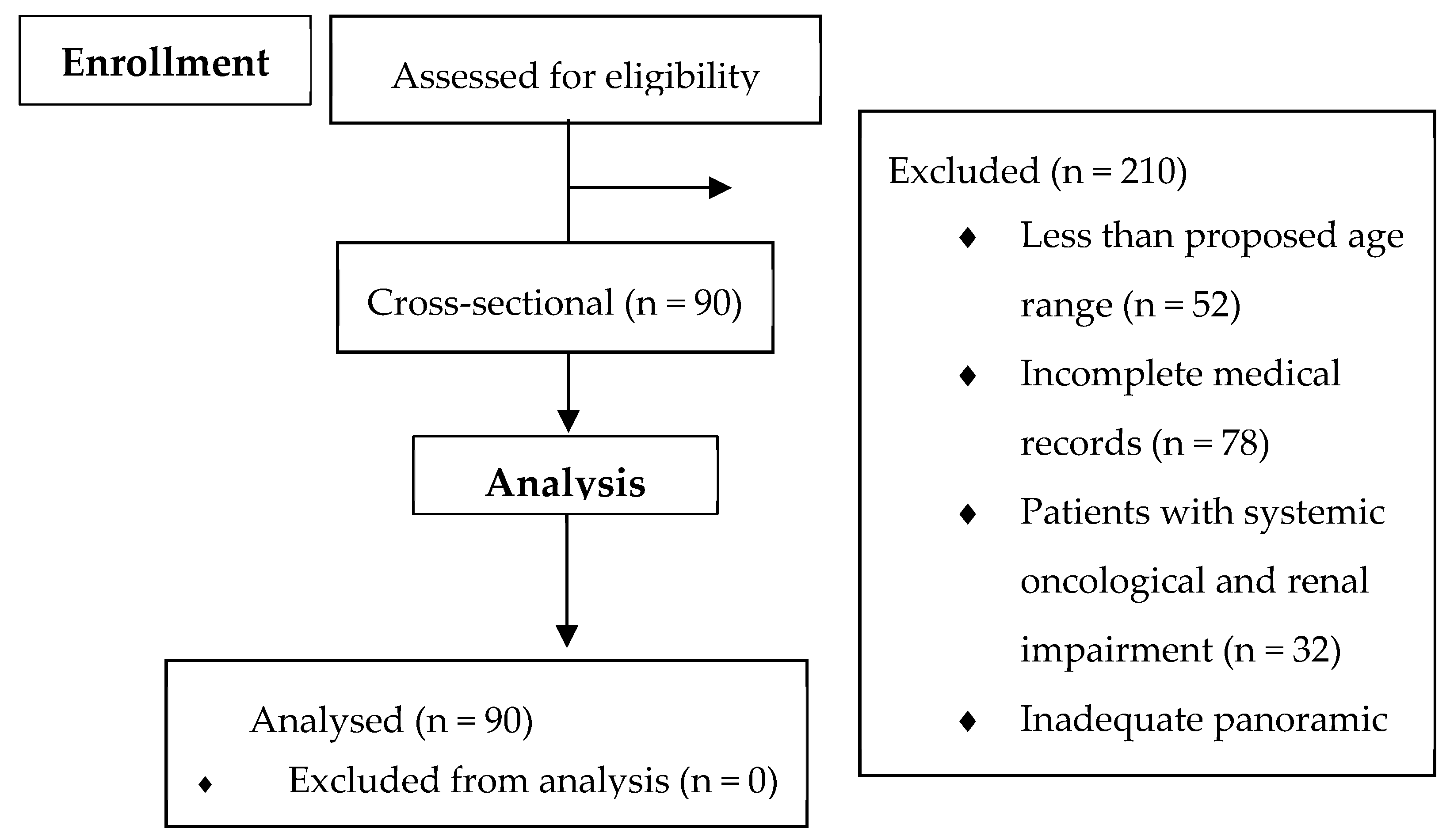
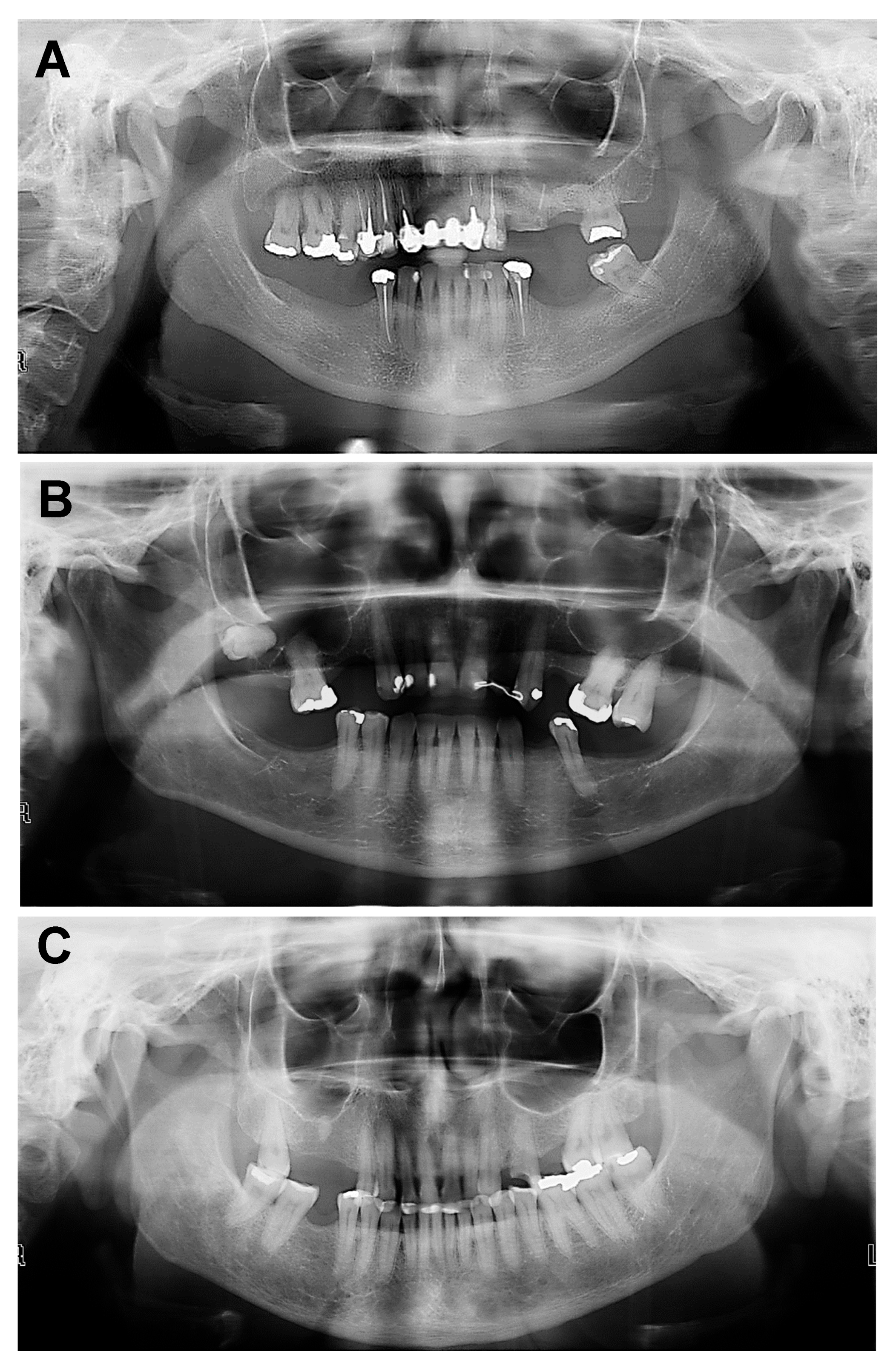
2. Materials and Methods
Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Alapati, S.; Reddy, R.S.; Tapapudi, R.; Katha, R.; Bodu, N.K.; Chennoju, S. Identifying risk groups for osteoporosis by digital pano-ramic radiography. Contemp. Clin. Dent. 2015, 6, 253–257. [Google Scholar] [CrossRef] [PubMed]
- Alman, A.C.; Johson, L.R.; Calverley, D.C.; Grunwald, G.K.; Lezotte, D.C.; Hokason, J.E. Diagnostic capabilities of fractal dimension and mandibular cortical width to identify men and women with decreased bone mineral density. Osteoporos. Int. 2012, 23, 1631–1636. [Google Scholar] [CrossRef] [PubMed]
- Carmo, J.Z.B.; Medeiros, S.F. Mandibular inferior cortex erosion on dental panoramic radiograph as a sign of low bone mineral density in postmenopausal women. Rev. Bras. Ginecol. Obstet. 2017, 39, 663–669. [Google Scholar] [CrossRef]
- Loures, M.A.R.; Zerbini, C.A.F.; Danowski, J.S.; Pereira, R.M.R.; Moreira, C.; Paula, A.P.; Castro, C.H.M.; Szejnfeld, V.L.; Mendonça, L.M.C.; Randominiski, S.C.; et al. Guidelines of the Brazilian Society of Rheumatology for the diagnosis and treatment of osteoporosis in men. Rev. Bras. Reumatol. Engl. Ed. 2017, 57, 497–514. [Google Scholar] [CrossRef]
- Thiele, S.; Hannemann, A.; Winzer, M.; Baschant, U.; Weidner, H.; Nauck, M.; Thakker, R.V.; Bornhäuser, M.; Hofbauer, L.C.; Rauner, M. Regulation of sclerostin in glucocorticoid-induced osteoporosis (GIO) in mice and humans. Endocr. Connect. 2019, 8, 923–934. [Google Scholar] [CrossRef]
- Mupparapu, M.; Akintoye, S.O. Application of Panoramic Radiography in the Detection of Osteopenia and Osteoporosis-Current State of the Art. Curr. Osteoporos. Rep. 2023, 21, 354–359. [Google Scholar] [CrossRef]
- Herrera, A.; Lobo-Escobar, A.; Mateo, J.; Gil, J.; Ibarz, E.; Gracia, L. Male osteoporosis: A review. World J. Orthop. 2012, 3, 223–234. [Google Scholar] [CrossRef] [PubMed]
- Kavitha, M.S.; Samopa, F.; Asano, A.; Taguchi, A.; Sanada, M. Computer-aided measurement of mandibular cortical width on den-tal panoramic radiographs for identifying osteoporosis. J. Investig. Clin. Dent. 2012, 3, 36–44. [Google Scholar] [CrossRef]
- Passos, J.S.; Gomes-Filho, I.S.; Sarmento, V.A.; Sampaio, D.S.; Gonçalves, F.P.; Coelho, J.M.; Cruz, S.S.; Trindade, S.C.; Cerqueira, E.M. Women with low bone mineral density and dental panoramic radiography. Menopause 2012, 19, 704–709. [Google Scholar] [CrossRef] [PubMed]
- Barnsley, J.; Buckland, G.; Chan, P.E.; Ong, A.; Ramos, A.S.; Baxter, M.; Laskou, F.; Dennison, E.M.; Cooper, C.; Patel, H.P. Pathophysiology and treatment of osteoporosis: Challenges for clinical practice in older people. Aging Clin. Exp. Res. 2021, 33, 759–773. [Google Scholar] [CrossRef]
- Föger-Samwald, U.; Dovjak, P.; Azizi-Semrad, U.; Kerschan-Schindl, K.; Pietschmann, P. Osteoporosis: Pathophysiology and therapeutic options. EXCLI J. 2020, 20, 1017–1037. [Google Scholar] [CrossRef]
- Akintoye, S.O.; Lam, T.; Shi, S.; Brahim, J.; Collins, M.T.; Robey, P.G. Skeletal site-specifc characterization of orofacial and iliac crest human bone marrow stromal cells in same individuals. Bone 2006, 38, 758–768. [Google Scholar] [CrossRef]
- Akintoye, S.O. The distinctive jaw and alveolar bone regeneration. Oral Dis. 2018, 24, 49–51. [Google Scholar] [CrossRef] [PubMed]
- Kanis, J.A.; Cooper, C.; Rizoli, R.; Reginster, J.Y. European guidance for the diagnosis and management of osteoporosis in post-menopausal women. Osteoporos. Int. 2019, 30, 3–44. [Google Scholar] [CrossRef]
- Nakamoto, T.; Taguchi, A.; Verdonschot, R.G.; Kakimoto, N. Improvement of region of interest extraction and scanning method of computer-aided diagnosis system for osteoporosis using panoramic radiographs. Oral Radiol. 2019, 35, 143–151. [Google Scholar] [CrossRef] [PubMed]
- Nakamoto, T.; Taguchi, A.; Ohtsuka, M.; Suei, Y.; Fujita, M.; Tanimoto, K.; Tsuda, M.; Sanada, M.; Ohama, K.; Takahashi, J.; et al. Dental panoramic radiograph as a tool to detect postmenopausal women with low bone mineral density: Untrained general dental practitioners’ diagnostic performance. Osteoporos. Int. 2003, 14, 659–664. [Google Scholar] [CrossRef]
- Nakamoto, T.; Taguchi, A.; Ohtsuka, M.; Suei, Y.; Fujita, M.; Tsuda, M.; Sanada, M.; Kudo, Y.; Asano, A.; Tanimoto, K. A computer-aided diagnosis system to screen for osteoporosis using dental panoramic radiographs. Dentomaxillofac. Radiol. 2008, 37, 274–281. [Google Scholar] [CrossRef]
- Klemetti, E.; Kolmakov, S.; Kroger, H. Pantomography in assessment of osteoporosis risk group. Scand. Dent. Res. 1994, 102, 8–72. [Google Scholar] [CrossRef]
- Ensrud, K.E.; Lui, L.Y.; Taylor, B.C.; Schousboe, J.T.; Donaldson, M.G.; Fink, H.A.; Cauley, J.A.; Hillier, T.A.; Browner, W.S.; Cummings, S.R. A comparison of prediction models for fractures in older women: Is more better? Arch. Intern. Med. 2009, 169, 2087–2094. [Google Scholar] [CrossRef]
- Kanis, J.A.; Johnell, O.; Oden, A.; Johansson, H.; McCloskey, E. FRAX and the assessment of fracture probability in men and women from the UK. Osteoporos. Int. 2008, 19, 385–397. [Google Scholar] [CrossRef]
- Lewiecki, E.M.; Gordon, C.M.; Baim, S.; Leonard, M.B.; Bishop, N.J.; Bianchi, M.L.; Kalkward, H.J.; Langman, C.B.; Plotkin, H.; Rauch, F.; et al. International Society for Clinical Densitometry 2007 Adult and Pediatric Official Positions. Bone 2008, 43, 1115–1121. [Google Scholar] [CrossRef] [PubMed]
- Cosman, F.; Beur, S.J.; Leboff, M.S.; Lewiecki, E.M.; Tanner, B.; Randall, D.; Lindsay, R. Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos. Int. 2015, 26, 2045–2047. [Google Scholar] [CrossRef] [PubMed]
- Kanis, J.A. Diagnosis of osteoporosis and assessment of fracture risk. Lancet 2002, 359, 1929–1936. [Google Scholar] [CrossRef]
- Kinalski, M.A.; Boscato, N.; Damian, M.F. The accuracy of panoramic radiography as a screening of bone mineral density in women: A systematic review. Dentomaxillofac. Radiol. 2020, 49, 20190149. [Google Scholar] [CrossRef]
- Dagistan, S.; Bilge, O.M. Comparison of antegonial index, mental index, panoramic mandibular index and mandibular cortical index values in the panoramic radiographs of normal males and male patients with osteoporosis. Dentomaxillofac. Radiol. 2010, 39, 290–294. [Google Scholar] [CrossRef]
- Peycheva, S.; Lalabonova, H.; Daskalov, H. Early detection of osteoporosis in patients over 55 using orthopantomography. J. IMAB 2012, 18, 229–231. [Google Scholar] [CrossRef][Green Version]
- Watanabe, P.C.; Dias, F.C.; Issa, J.P.; Monteiro, S.A.; De-Paula, F.J.; Tiossi, R. Elongated styloid process and atheroma in panoramic radiography and its relationship with systemic osteoporosis and osteopenia. Osteoporos. Int. 2010, 21, 831–836. [Google Scholar] [CrossRef]
- Diabetes Prevention Program Research Group. Long-term effects of lifestyle intervention or metformin on diabetes development and microvascular complications over 15-year follow-up: The diabetes prevention program outcomes study. Lancet Diabetes Endocrinol. 2015, 3, 866–875. [Google Scholar] [CrossRef]
- Leslie, W.D.; Morin, S.N.; Lix, L.M.; Majumdar, S.R. Does diabetes modify the effect of FRAX risk factors for predicting major oste-oporotic and hip fracture? Osteoporos. Int. 2014, 25, 2817–2824. [Google Scholar] [CrossRef]
- Mazziotti, G.; Canalis, E.; Giustina, A. Drug-induced osteoporosis: Mechanisms and clinical implications. Am. J. Med. Sci. 2010, 123, 877–884. [Google Scholar] [CrossRef]
- Giustina, A.; Mazziotti, G.; Canalis, E. Growth hormone, insulin-like growth factors, and the skeleton. Endocr. Rev. 2008, 29, 535–559. [Google Scholar] [CrossRef] [PubMed]
- Bauer, D.C.; Ettinger, B.; Nevitt, M.C.; Stone, K.L. Risk for fracture in women with low serum levels of thyroid-stimulating hormone. Ann. Intern. Med. 2001, 134, 561–568. [Google Scholar] [CrossRef] [PubMed]
- Woo, J.; Kwok, T.; Leung, J.; Tang, N. Dietary intake, blood pressure and osteoporosis. J. Hum. Hypertens. 2009, 23, 451–455. [Google Scholar] [CrossRef] [PubMed]
- Kaya, E.; Gunec, H.G.; Gokyay, S.S.; Kutal, S.; Gulum, S.; Ates, H.F. Proposing a CNN method for primary and permanent tooth detection and enumeration on pediatric dental radiographs. J. Clin. Pediatr. Dent. 2022, 46, 293–298. [Google Scholar] [CrossRef]
- Pascadopoli, M.; Zampetti, P.; Nardi, M.G.; Pellegrini, M.; Scribante, A. Smartphone applications in dentistry: A scoping review. Dent. J. 2023, 11, 243. [Google Scholar] [CrossRef] [PubMed]
- Seki, K.; Nagasaki, M.; Yoshino, T.; Yano, M.; Kawamoto, A.; Shimizu, O. Radiographical Diagnostic Evaluation of Mandibular Cortical Index Classification and Mandibular Cortical Width in Female Patients Prescribed Antiosteoporosis Medication: A Retrospective Cohort Study. Diagnostics 2024, 14, 1009. [Google Scholar] [CrossRef]
| Classification | Definition |
|---|---|
| C1 | (Normal)—Smooth and regular cortical |
| C2 | (Osteopenia)—Cortical with semilunar defects (lacunar resorption) |
| C3 | (Osteoporosis)—Clearly porous cortical layer and its thickness is tapered and reduced |
| Gender | n (%) | Mean (Standard Deviation) |
|---|---|---|
| Women | 78 (86%) | 57.34 (8.56) |
| Male | 12 (14%) | 68.50 (10.77) |
| Total | 90 (100%) | 58.86 (9.57) |
| Score | Total | Women | Male |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| C1 | 39 (43) | 33 (84) | 6 (16) |
| C2 | 47 (52) | 43 (91) | 4 (9) |
| C3 | 4 (5) | 2 (50) | 2 (50) |
| Total | 90 (100) | 78 (86) | 12 (14) |
| Score | TB | ET | SAH | DM | TD |
|---|---|---|---|---|---|
| C1 | 6 | 1 | 5 | 8 | 2 |
| C2 | 3 | 0 | 18 | 9 | 0 |
| C3 | 0 | 0 | 1 | 0 | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alves-Silva, E.G.; Fachetti Ribeiro, B.; Silva, C.F.; de Kássia-Alves, R.; Arruda-Vasconcelos, R.; Louzada, L.M.; Almeida-Gomes, R.F.; Santos, J.M.M.; Gomes, B.P.F.A. Evaluation of Mandibular Bone Alterations by Panoramic Radiography: A Potential Tool in the Identification of Signs of Osteopenia and Osteoporosis. Bioengineering 2025, 12, 746. https://doi.org/10.3390/bioengineering12070746
Alves-Silva EG, Fachetti Ribeiro B, Silva CF, de Kássia-Alves R, Arruda-Vasconcelos R, Louzada LM, Almeida-Gomes RF, Santos JMM, Gomes BPFA. Evaluation of Mandibular Bone Alterations by Panoramic Radiography: A Potential Tool in the Identification of Signs of Osteopenia and Osteoporosis. Bioengineering. 2025; 12(7):746. https://doi.org/10.3390/bioengineering12070746
Chicago/Turabian StyleAlves-Silva, Esdras Gabriel, Betania Fachetti Ribeiro, Camila Fontes Silva, Rita de Kássia-Alves, Rodrigo Arruda-Vasconcelos, Lidiane Mendes Louzada, Rebecca F. Almeida-Gomes, João Miguel Marques Santos, and Brenda P. F. A. Gomes. 2025. "Evaluation of Mandibular Bone Alterations by Panoramic Radiography: A Potential Tool in the Identification of Signs of Osteopenia and Osteoporosis" Bioengineering 12, no. 7: 746. https://doi.org/10.3390/bioengineering12070746
APA StyleAlves-Silva, E. G., Fachetti Ribeiro, B., Silva, C. F., de Kássia-Alves, R., Arruda-Vasconcelos, R., Louzada, L. M., Almeida-Gomes, R. F., Santos, J. M. M., & Gomes, B. P. F. A. (2025). Evaluation of Mandibular Bone Alterations by Panoramic Radiography: A Potential Tool in the Identification of Signs of Osteopenia and Osteoporosis. Bioengineering, 12(7), 746. https://doi.org/10.3390/bioengineering12070746








