Why Hoop Tension Matters: A Biomechanical Perspective on Medial Meniscus Posterior Root Tears—A Narrative Review
Abstract
1. Introduction
2. Medial Meniscus
2.1. Anatomy
2.2. Functions and Biomechanics of Normal Medial Meniscus
3. Hoop Tension
3.1. Structural and Material Contributors
3.2. Alteration of the Hoop Tension by Tear Type
- (1)
- Horizontal tear
- (2)
- Radial tear
- (3)
- Root tear
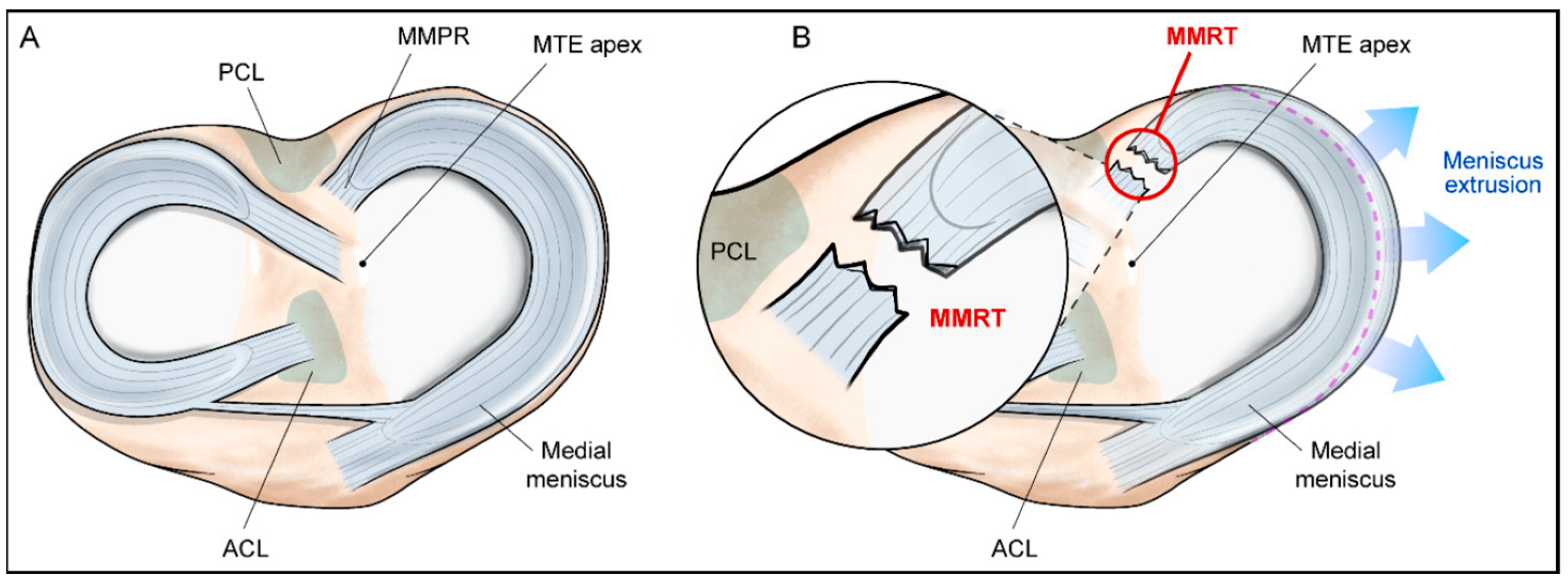
4. Medial Meniscus Posterior Root Tear
4.1. Anatomy of Roots of Medial Meniscus
4.2. Definition and Classification
4.3. Biomechanical Alteration
- (1)
- Cadaver study
- (2)
- FEA study
- (3)
- Biomechanical restoration following root repair
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Gee, S.M.; Tennent, D.J.; Cameron, K.L.; Posner, M.A. The burden of meniscus injury in young and physically active populations. Clin. Sports Med. 2020, 39, 13–27. [Google Scholar] [CrossRef] [PubMed]
- Snoeker, B.A.M.; Bakker, E.W.P.; Kegel, C.A.T.; Lucas, C. Risk Factors for Meniscal Tears: A Systematic Review Including Meta-analysis. J. Orthop. Sports Phys. Ther. 2013, 43, 352–367. [Google Scholar] [CrossRef]
- Kuczyński, N.; Boś, J.; Białoskórska, K.; Aleksandrowicz, Z.; Turoń, B.; Zabrzyńska, M.; Bonowicz, K.; Gagat, M. The Meniscus: Basic Science and Therapeutic Approaches. J. Clin. Med. 2025, 14, 2020. [Google Scholar] [CrossRef] [PubMed]
- Cinque, M.E.; Chahla, J.; Moatshe, G.; Faucett, S.C.; Krych, A.J.; LaPrade, R.F. Meniscal root tears: A silent epidemic. Br. J. Sports Med. 2018, 52, 872–876. [Google Scholar] [CrossRef] [PubMed]
- Krakowski, P.; Karpiński, R.; Jonak, J.; Maciejewski, R. Evaluation of diagnostic accuracy of physical examination and MRI for ligament and meniscus injuries. J. Phys. Conf. Ser. 2021, 1736, 012027. [Google Scholar] [CrossRef]
- Krakowski, P.; Nogalski, A.; Jurkiewicz, A.; Karpiński, R.; Maciejewski, R.; Jonak, J. Comparison of diagnostic accuracy of physical examination and MRI in the most common knee injuries. Appl. Sci. 2019, 9, 4102. [Google Scholar] [CrossRef]
- Choi, E.S.; Park, S.J. Clinical Evaluation of the Root Tear of the Posterior Horn of the Medial Meniscus in Total Knee Arthroplasty for Osteoarthritis. Knee Surg. Relat. Res. 2015, 27, 90–94. [Google Scholar] [CrossRef]
- Dzidzishvili, L.; López, T., II; Guerrero, C.C.; Calvo, E. Developing an experimental model of early knee osteoarthritis after medial meniscus posterior root release: An in vivo study. J. Exp. Orthop. 2022, 9, 66. [Google Scholar] [CrossRef]
- Okazaki, Y.; Furumatsu, T.; Hiranaka, T.; Kintaka, K.; Takihira, S.; Kamatsuki, Y.; Tetsunaga, T.; Ozaki, T. Medial meniscus posterior root repair prevents the progression of subchondral insufficiency fracture of the knee. J. Orthop. Sci. 2021, 26, 1051–1055. [Google Scholar] [CrossRef]
- Tamura, M.; Furumatsu, T.; Kitayama, T.; Yokoyama, Y.; Okazaki, Y.; Kawada, K.; Ozaki, T. The preoperative flexion tear gap affects postoperative meniscus stability after pullout repair for medial meniscus posterior root tear. Knee Surg. Relat. Res. 2025, 37, 16. [Google Scholar] [CrossRef]
- Tamura, M.; Furumatsu, T.; Yokoyama, Y.; Higashihara, N.; Kawada, K.; Ozaki, T. Superior outcomes of pullout repairs for medial meniscus posterior root tears in partial tear compared to complete radial tear. Knee Surg. Relat. Res. 2024, 36, 8. [Google Scholar] [CrossRef] [PubMed]
- Thamrongskulsiri, N.; Pholkerd, P.; Limskul, D.; Tanpowpong, T.; Kuptniratsaikul, S.; Itthipanichpong, T. Clinical and Radiographic Outcomes of Arthroscopic Medial Meniscus Posterior Root Repair Using Soft Suture Anchor without Posterior Portal Technique. Clin. Orthop. Surg. 2024, 16, 906–916. [Google Scholar] [CrossRef]
- Faucett, S.C.; Geisler, B.P.; Chahla, J.; Krych, A.J.; Kurzweil, P.R.; Garner, A.M.; Liu, S.; LaPrade, R.F.; Pietzsch, J.B. Meniscus Root Repair vs Meniscectomy or Nonoperative Management to Prevent Knee Osteoarthritis After Medial Meniscus Root Tears: Clinical and Economic Effectiveness. Am. J. Sports Med. 2019, 47, 762–769. [Google Scholar] [CrossRef]
- Kumar, K.V.A.; Thavasianantham, K.; Pandian, P.; Pandian, H.; Pradeep, E.; Mohideen, S. Functional and Radiological Outcome of Meniscal Repair and Conservative Management for Medial Meniscal Root Tear—A Prospective Comparative Study. J. Orthop. Case Rep. 2024, 14, 223–228. [Google Scholar] [CrossRef]
- Hayashi, M.; Isaji, Y.; Kurasawa, Y.; Kitagawa, T. Effectiveness of Meniscus Root Tear Repair Versus Conservative Therapy and Adjunct Therapies: A Systematic Review. Cureus 2024, 16, e75645. [Google Scholar] [CrossRef]
- Elnewishy, A.; Elsenosy, A.M.; Nahas, S.; Abdalla, M.; Symeon, N.; Teama, H. A Systematic Review and Meta-Analysis of Medial Meniscus Root Tears: Is Surgery the Key to Better Outcomes? Cureus 2024, 16, e75199. [Google Scholar] [CrossRef] [PubMed]
- Krych, A.J.; Lamba, A.; Wang, A.S.; Boos, A.M.; Camp, C.L.; Levy, B.A.; Stuart, M.J.; Hevesi, M. Nonoperative Management of Degenerative Medial Meniscus Posterior Root Tears: Poor Outcomes at a Minimum 10-Year Follow-up. Am. J. Sports Med. 2023, 51, 2603–2607. [Google Scholar] [CrossRef] [PubMed]
- Hantouly, A.T.; Aminake, G.; Khan, A.S.; Ayyan, M.; Olory, B.; Zikria, B.; Al-Khelaifi, K. Meniscus root tears: State of the art. Int. Orthop. 2024, 48, 955–964. [Google Scholar] [CrossRef]
- Moon, H.S.; Choi, C.H.; Jung, M.; Chung, K.; Jung, S.H.; Kim, Y.H.; Kim, S.H. Medial Meniscus Posterior Root Tear: How Far Have We Come and What Remains? Medicina 2023, 59, 1181. [Google Scholar] [CrossRef]
- Shaffer, B.; Kennedy, S.; Klimkiewicz, J.; Yao, L. Preoperative sizing of meniscal allografts in meniscus transplantation. Am. J. Sports Med. 2000, 28, 524–533. [Google Scholar] [CrossRef]
- McDermott, I.D.; Sharifi, F.; Bull, A.M.; Gupte, C.M.; Thomas, R.W.; Amis, A.A. An anatomical study of meniscal allograft sizing. Knee Surg. Sports Traumatol. Arthrosc. 2004, 12, 130–135. [Google Scholar] [CrossRef] [PubMed]
- Stein, G.; Koebke, J.; Faymonville, C.; Dargel, J.; Müller, L.P.; Schiffer, G. The relationship between the medial collateral ligament and the medial meniscus: A topographical and biomechanical study. Surg. Radiol. Anat. 2011, 33, 763–766. [Google Scholar] [CrossRef]
- Rashmi, B.N.; Dakshayani, K.R.; Vadiraja, N. Morphometric Study of Menisci of Knee Joints in Adult Cadavers. Int. J. Anat. Res. 2016, 4, 2973–2978. [Google Scholar] [CrossRef]
- Bloecker, K.; Wirth, W.; Hudelmaier, M.; Burgkart, R.; Frobell, R.; Eckstein, F. Morphometric differences between the medial and lateral meniscus in healthy men—A three-dimensional analysis using magnetic resonance imaging. Cells Tissues Organs 2012, 195, 353–364. [Google Scholar] [CrossRef] [PubMed]
- Fukubayashi, T.; Kurosawa, H. The contact area and pressure distribution pattern of the knee. A study of normal and osteoarthrotic knee joints. Acta Orthop. Scand. 1980, 51, 871–879. [Google Scholar] [CrossRef]
- Melrose, J.; Smith, S.; Cake, M.; Read, R.; Whitelock, J. Comparative spatial and temporal localisation of perlecan, aggrecan and type I, II and IV collagen in the ovine meniscus: An ageing study. Histochem. Cell Biol. 2005, 124, 225–235. [Google Scholar] [CrossRef] [PubMed]
- Fox, A.J.; Bedi, A.; Rodeo, S.A. The basic science of human knee menisci: Structure, composition, and function. Sports Health 2012, 4, 340–351. [Google Scholar] [CrossRef]
- Markes, A.R.; Hodax, J.D.; Ma, C.B. Meniscus Form and Function. Clin. Sports Med. 2020, 39, 1–12. [Google Scholar] [CrossRef]
- Jones, R.S.; Keene, G.C.; Learmonth, D.J.; Bickerstaff, D.; Nawana, N.S.; Costi, J.J.; Pearcy, M.J. Direct measurement of hoop strains in the intact and torn human medial meniscus. Clin. Biomech. 1996, 11, 295–300. [Google Scholar] [CrossRef]
- Brindle, T.; Nyland, J.; Johnson, D.L. The meniscus: Review of basic principles with application to surgery and rehabilitation. J. Athl. Train. 2001, 36, 160–169. [Google Scholar]
- Yanagishita, M. Function of Proteoglycans in the Extracellular-Matrix. Acta Pathol. Jpn. 1993, 43, 283–293. [Google Scholar] [CrossRef] [PubMed]
- Scott, P.G.; Nakano, T.; Dodd, C.M. Isolation and characterization of small proteoglycans from different zones of the porcine knee meniscus. Biochim. Biophys. Acta 1997, 1336, 254–262. [Google Scholar] [CrossRef] [PubMed]
- McDevitt, C.A.; Webber, R.J. The ultrastructure and biochemistry of meniscal cartilage. Clin. Orthop. Relat. Res. 1990, 252, 8–18. [Google Scholar] [CrossRef]
- Hellio Le Graverand, M.P.; Ou, Y.; Schield-Yee, T.; Barclay, L.; Hart, D.; Natsume, T.; Rattner, J.B. The cells of the rabbit meniscus: Their arrangement, interrelationship, morphological variations and cytoarchitecture. J. Anat. 2001, 198, 525–535. [Google Scholar] [CrossRef]
- Gee, S.M.; Posner, M. Meniscus Anatomy and Basic Science. Sports Med. Arthrosc. Rev. 2021, 29, e18–e23. [Google Scholar] [CrossRef]
- Crawford, M.D.; Hellwinkel, J.E.; Aman, Z.; Akamefula, R.; Singleton, J.T.; Bahney, C.; LaPrade, R.F. Microvascular Anatomy and Intrinsic Gene Expression of Menisci From Young Adults. Am. J. Sports Med. 2020, 48, 3147–3153. [Google Scholar] [CrossRef]
- Arnoczky, S.P.; Warren, R.F. Microvasculature of the human meniscus. Am. J. Sports Med. 1982, 10, 90–95. [Google Scholar] [CrossRef]
- Tramś, E.; Kamiński, R. Molecular Biology of Meniscal Healing: A Narrative Review. Int. J. Mol. Sci. 2024, 25, 768. [Google Scholar] [CrossRef] [PubMed]
- Shrive, N.G.; O’Connor, J.J.; Goodfellow, J.W. Load-bearing in the knee joint. Clin. Orthop. Relat. Res. 1978, 131, 279–287. [Google Scholar] [CrossRef]
- Greis, P.E.; Bardana, D.D.; Holmstrom, M.C.; Burks, R.T. Meniscal injury: I. Basic science and evaluation. J. Am. Acad. Orthop. Surg. 2002, 10, 168–176. [Google Scholar] [CrossRef]
- Fox, A.J.; Wanivenhaus, F.; Burge, A.J.; Warren, R.F.; Rodeo, S.A. The human meniscus: A review of anatomy, function, injury, and advances in treatment. Clin. Anat. 2015, 28, 269–287. [Google Scholar] [CrossRef] [PubMed]
- Zhang, A.L.; Miller, S.L.; Coughlin, D.G.; Lotz, J.C.; Feeley, B.T. Tibiofemoral contact pressures in radial tears of the meniscus treated with all-inside repair, inside-out repair and partial meniscectomy. Knee 2015, 22, 400–404. [Google Scholar] [CrossRef]
- Koh, J.L.; Yi, S.J.; Ren, Y.; Zimmerman, T.A.; Zhang, L.Q. Tibiofemoral Contact Mechanics with Horizontal Cleavage Tear and Resection of the Medial Meniscus in the Human Knee. J. Bone Jt. Surg. Am. 2016, 98, 1829–1836. [Google Scholar] [CrossRef]
- Beamer, B.S.; Walley, K.C.; Okajima, S.; Manoukian, O.S.; Perez-Viloria, M.; DeAngelis, J.P.; Ramappa, A.J.; Nazarian, A. Changes in Contact Area in Meniscus Horizontal Cleavage Tears Subjected to Repair and Resection. Arthroscopy 2017, 33, 617–624. [Google Scholar] [CrossRef]
- Bhatia, S.; LaPrade, C.M.; Ellman, M.B.; LaPrade, R.F. Meniscal root tears: Significance, diagnosis, and treatment. Am. J. Sports Med. 2014, 42, 3016–3030. [Google Scholar] [CrossRef] [PubMed]
- Seitz, A.M.; Schwer, J.; de Roy, L.; Warnecke, D.; Ignatius, A.; Dürselen, L. Knee Joint Menisci Are Shock Absorbers: A Biomechanical In-Vitro Study on Porcine Stifle Joints. Front. Bioeng. Biotechnol. 2022, 10, 837554. [Google Scholar] [CrossRef]
- Voloshin, A.S.; Wosk, J. Shock absorption of meniscectomized and painful knees: A comparative in vivo study. J. Biomed. Eng. 1983, 5, 157–161. [Google Scholar] [CrossRef] [PubMed]
- Levy, I.M.; Torzilli, P.A.; Warren, R.F. The effect of medial meniscectomy on anterior-posterior motion of the knee. J. Bone Jt. Surg. Am. 1982, 64, 883–888. [Google Scholar] [CrossRef]
- Allen, C.R.; Wong, E.K.; Livesay, G.A.; Sakane, M.; Fu, F.H.; Woo, S.L. Importance of the medial meniscus in the anterior cruciate ligament-deficient knee. J. Orthop. Res. 2000, 18, 109–115. [Google Scholar] [CrossRef]
- Petersen, W.; Tillmann, B. Collagenous fibril texture of the human knee joint menisci. Anat. Embryol. 1998, 197, 317–324. [Google Scholar] [CrossRef]
- Makris, E.A.; Hadidi, P.; Athanasiou, K.A. The knee meniscus: Structure-function, pathophysiology, current repair techniques, and prospects for regeneration. Biomaterials 2011, 32, 7411–7431. [Google Scholar] [CrossRef] [PubMed]
- LaPrade, R.F.; Engebretsen, A.H.; Ly, T.V.; Johansen, S.; Wentorf, F.A.; Engebretsen, L. The anatomy of the medial part of the knee. J. Bone Jt. Surg. Am. 2007, 89, 2000–2010. [Google Scholar] [CrossRef]
- Mahmood, F.; Clarke, J.; Riches, P. The ionic contribution of proteoglycans to mechanical stiffness of the meniscus. Med. Eng. Phys. 2019, 64, 23–27. [Google Scholar] [CrossRef]
- Korhonen, R.K.; Laasanen, M.S.; Toyras, J.; Rieppo, J.; Hirvonen, J.; Helminen, H.J.; Jurvelin, J.S. Comparison of the equilibrium response of articular cartilage in unconfined compression, confined compression and indentation. J. Biomech. 2002, 35, 903–909. [Google Scholar] [CrossRef]
- Joshi, M.D.; Suh, J.K.; Marui, T.; Woo, S.L. Interspecies variation of compressive biomechanical properties of the meniscus. J. Biomed. Mater. Res. 1995, 29, 823–828. [Google Scholar] [CrossRef]
- Xue, A.; Mao, Z.; Zhu, X.; Yang, Q.; Wang, P.; Mao, Z.; Du, M.; Ma, X.; Jiang, D.; Fan, Y.; et al. Biomechanical effects of the medial meniscus horizontal tear and the resection strategy on the rabbit knee joint under resting state: Finite element analysis. Front. Bioeng. Biotechnol. 2023, 11, 1164922. [Google Scholar] [CrossRef]
- Brown, M.J.; Farrell, J.P.; Kluczynski, M.A.; Marzo, J.M. Biomechanical Effects of a Horizontal Medial Meniscal Tear and Subsequent Leaflet Resection. Am. J. Sports Med. 2016, 44, 850–854. [Google Scholar] [CrossRef]
- Bedi, A.; Kelly, N.H.; Baad, M.; Fox, A.J.; Brophy, R.H.; Warren, R.F.; Maher, S.A. Dynamic contact mechanics of the medial meniscus as a function of radial tear, repair, and partial meniscectomy. J. Bone Jt. Surg. Am. 2010, 92, 1398–1408. [Google Scholar] [CrossRef] [PubMed]
- Andriacchi, T.P.; Mündermann, A. The role of ambulatory mechanics in the initiation and progression of knee osteoarthritis. Curr. Opin. Rheumatol. 2006, 18, 514–518. [Google Scholar] [CrossRef]
- Wang, S.; Hase, K.; Kita, S.; Ogaya, S. Biomechanical effects of medial meniscus radial tears on the knee joint during gait: A concurrent finite element musculoskeletal framework investigation. Front. Bioeng. Biotechnol. 2022, 10, 957435. [Google Scholar] [CrossRef]
- Allaire, R.; Muriuki, M.; Gilbertson, L.; Harner, C.D. Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy. J. Bone Jt. Surg. Am. 2008, 90, 1922–1931. [Google Scholar] [CrossRef] [PubMed]
- LaPrade, C.M.; Foad, A.; Smith, S.D.; Turnbull, T.L.; Dornan, G.J.; Engebretsen, L.; Wijdicks, C.A.; LaPrade, R.F. Biomechanical consequences of a nonanatomic posterior medial meniscal root repair. Am. J. Sports Med. 2015, 43, 912–920. [Google Scholar] [CrossRef]
- Kim, J.G.; Lee, Y.S.; Bae, T.S.; Ha, J.K.; Lee, D.H.; Kim, Y.J.; Ra, H.J. Tibiofemoral contact mechanics following posterior root of medial meniscus tear, repair, meniscectomy, and allograft transplantation. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 2121–2125. [Google Scholar] [CrossRef]
- Johannsen, A.M.; Civitarese, D.M.; Padalecki, J.R.; Goldsmith, M.T.; Wijdicks, C.A.; LaPrade, R.F. Qualitative and quantitative anatomic analysis of the posterior root attachments of the medial and lateral menisci. Am. J. Sports Med. 2012, 40, 2342–2347. [Google Scholar] [CrossRef]
- LaPrade, C.M.; Ellman, M.B.; Rasmussen, M.T.; James, E.W.; Wijdicks, C.A.; Engebretsen, L.; LaPrade, R.F. Anatomy of the anterior root attachments of the medial and lateral menisci: A quantitative analysis. Am. J. Sports Med. 2014, 42, 2386–2392. [Google Scholar] [CrossRef]
- LaPrade, C.M.; James, E.W.; Cram, T.R.; Feagin, J.A.; Engebretsen, L.; LaPrade, R.F. Meniscal Root Tears:A Classification System Based on Tear Morphology. Am. J. Sports Med. 2015, 43, 363–369. [Google Scholar] [CrossRef] [PubMed]
- Padalecki, J.R.; Jansson, K.S.; Smith, S.D.; Dornan, G.J.; Pierce, C.M.; Wijdicks, C.A.; Laprade, R.F. Biomechanical consequences of a complete radial tear adjacent to the medial meniscus posterior root attachment site: In situ pull-out repair restores derangement of joint mechanics. Am. J. Sports Med. 2014, 42, 699–707. [Google Scholar] [CrossRef] [PubMed]
- Brusalis, C.M.; Chastain, K.L.; Uppstrom, T.J.; Steineman, B.D.; Gomoll, A.H.; Maher, S.A.; Strickland, S.M. Medial Meniscus Posterior Root Tears Lead to Changes in Joint Contact Mechanics at Low Flexion Angles During Simulated Gait. Am. J. Sports Med. 2024, 52, 109–115. [Google Scholar] [CrossRef]
- Xu, Z.; Li, Y.; Rao, J.; Jin, Y.; Huang, Y.; Xu, X.; Liu, Y.; Tian, S. Biomechanical assessment of disease outcome in surgical interventions for medial meniscal posterior root tears: A finite element analysis. BMC Musculoskelet. Disord. 2022, 23, 1093. [Google Scholar] [CrossRef]
- Yang, Q.; Zhu, X.Y.; Bao, J.Y.; Zhang, J.; Xue, A.Q.; Wang, D.Y.; Mao, Z.M.; Tang, J.W.; Jiang, D.; Fan, Y.; et al. Medial meniscus posterior root tears and partial meniscectomy significantly increase stress in the knee joint during dynamic gait. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 2289–2298. [Google Scholar] [CrossRef]
- Jones, B.W.; Willson, J.D.; DeVita, P.; Wedge, R.D. Tibiofemoral Load Magnitude and Distribution During Load Carriage. J. Appl. Biomech. 2023, 39, 432–439. [Google Scholar] [CrossRef] [PubMed]
- Berk, A.N.; Cregar, W.M.; Wang, S.; Habet, N.A.; Ifarraguerri, A.M.; Trofa, D.P.; Piasecki, D.P.; Fleischli, J.E.; Saltzman, B.M. The Effect of Lower Limb Alignment on Tibiofemoral Joint Contact Biomechanics after Medial Meniscus Posterior Root Repair: A Finite-Element Analysis. J. Am. Acad. Orthop. Surg. 2024, 32, e558–e567. [Google Scholar] [CrossRef]
- Steineman, B.D.; LaPrade, R.F.; Haut Donahue, T.L. Nonanatomic Placement of Posteromedial Meniscal Root Repairs: A Finite Element Study. J. Biomech. Eng. 2020, 142, 081004. [Google Scholar] [CrossRef]
- Takahashi, A.; Umehara, J.; Kamimura, M.; Aizawa, T.; Itoi, E. Obesity is a risk factor for osteoarthritis progression and spontaneous osteoporosis is a risk for the development of spontaneous osteonecrosis in patients with medial meniscus posterior root tear. J. Orthop. Sci. 2021, 26, 844–849. [Google Scholar] [CrossRef]
- Kim, Y.M.; Joo, Y.B.; An, B.K.; Song, J.H. Age and Meniscal Extrusion Are Determining Factors of Osteoarthritis Progression after Conservative Treatments for Medial Meniscus Posterior Root Tear. J. Pers. Med. 2022, 12, 2004. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.Y.; Bin, S.I.; Kim, J.M.; Lee, B.S.; Oh, S.M.; Park, M.H. Tear gap and severity of osteoarthritis are associated with meniscal extrusion in degenerative medial meniscus posterior root tears. Orthop. Traumatol. Surg. Res. 2019, 105, 1395–1399. [Google Scholar] [CrossRef] [PubMed]
- Moldovan, F. Recent Trends in Bioprinting. Procedia Manuf. 2019, 32, 95–101. [Google Scholar] [CrossRef]
- Cucchiarini, M.; McNulty, A.L.; Mauck, R.L.; Setton, L.A.; Guilak, F.; Madry, H. Advances in combining gene therapy with cell and tissue engineering-based approaches to enhance healing of the meniscus. Osteoarthr. Cartil. 2016, 24, 1330–1339. [Google Scholar] [CrossRef]
- Bilgen, B.; Jayasuriya, C.T.; Owens, B.D. Current Concepts in Meniscus Tissue Engineering and Repair. Adv. Healthc. Mater. 2018, 7, e1701407. [Google Scholar] [CrossRef]

| Category | Details |
|---|---|
| Length | Approx. 45.7 mm |
| Width (Posterior horn) | 12.6–17.4 mm |
| Width (Midbody) | 9.3–12.2 mm |
| Width (Anterior horn) | 7.6–9.0 mm |
| Thickness | 5.2–6.9 mm (wedge-shaped) |
| Surface Area Coverage | 51–74% of medial tibial plateau |
| Subcategory | Key Component | Role |
|---|---|---|
| Primary structures | Collagen fiber layers (superficial/lamellar/central or circumferential) Collagen crosslinking | Provides a circumferential tensile framework and resists fiber separation under load |
| Macrostructural constraint | Meniscal root attachments Meniscocapsular connections | Prevents radial extrusion Preserves the circumferential stress loop |
| Material composition | Proteoglycans (with GAG [glycosaminoglycan] chains) Interstitial fluid | Maintains hydration and internal pressure to support compressive load sharing |
| Viscoelastic response | Time- and rate-dependent tissue properties | Modulates internal stress and maintains tension stability during prolonged loading |
| Tear Type | Research Method | Tear Site | Hoop Tension Disruption | Peak Contact Pressure | Contact Area | Load Shift |
|---|---|---|---|---|---|---|
| Horizontal, localized [57] | cadaver | Posterior 1/3 | Minimal or preserved | insignificant | insignificant | n.s. |
| Horizontal, extensive [44] | cadaver | AH to PH | Severe | ↑ | ↓ | suggested |
| Radial, 30–60% [58] | cadaver | Between body and PH | Mild | insignificant | insignificant | None or mild |
| Radial, 90% [58] | cadaver | Between body and PH | Severe | ↑↑ | ↓ | Posterocentral |
| Root [62] | cadaver | Posterior root attachment | Near Complete | ↑↑ | ↓↓ | n.s. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, M.S.; In, Y.; Kim, H.; Jeong, J.; Sohn, S. Why Hoop Tension Matters: A Biomechanical Perspective on Medial Meniscus Posterior Root Tears—A Narrative Review. Bioengineering 2025, 12, 638. https://doi.org/10.3390/bioengineering12060638
Kim MS, In Y, Kim H, Jeong J, Sohn S. Why Hoop Tension Matters: A Biomechanical Perspective on Medial Meniscus Posterior Root Tears—A Narrative Review. Bioengineering. 2025; 12(6):638. https://doi.org/10.3390/bioengineering12060638
Chicago/Turabian StyleKim, Man Soo, Yong In, Hyungtae Kim, Juyoung Jeong, and Sueen Sohn. 2025. "Why Hoop Tension Matters: A Biomechanical Perspective on Medial Meniscus Posterior Root Tears—A Narrative Review" Bioengineering 12, no. 6: 638. https://doi.org/10.3390/bioengineering12060638
APA StyleKim, M. S., In, Y., Kim, H., Jeong, J., & Sohn, S. (2025). Why Hoop Tension Matters: A Biomechanical Perspective on Medial Meniscus Posterior Root Tears—A Narrative Review. Bioengineering, 12(6), 638. https://doi.org/10.3390/bioengineering12060638









