The Detection of Gait Events Based on Smartphones and Deep Learning
Abstract
1. Introduction
- (1)
- This study is the first to employ built-in smartphone sensors combined with deep learning to detect gait events, providing a novel approach for portable gait analysis.
- (2)
- The proposed model in this study applies to different walking speeds, and the detection time errors of different deep learning models are compared.
- (3)
- The external application effects of this method are remotely assessed in different elderly populations in daily home environments.
- (4)
- The clinical significance of this method is evaluated in a population with cerebral small vessel disease.
2. Materials and Methods
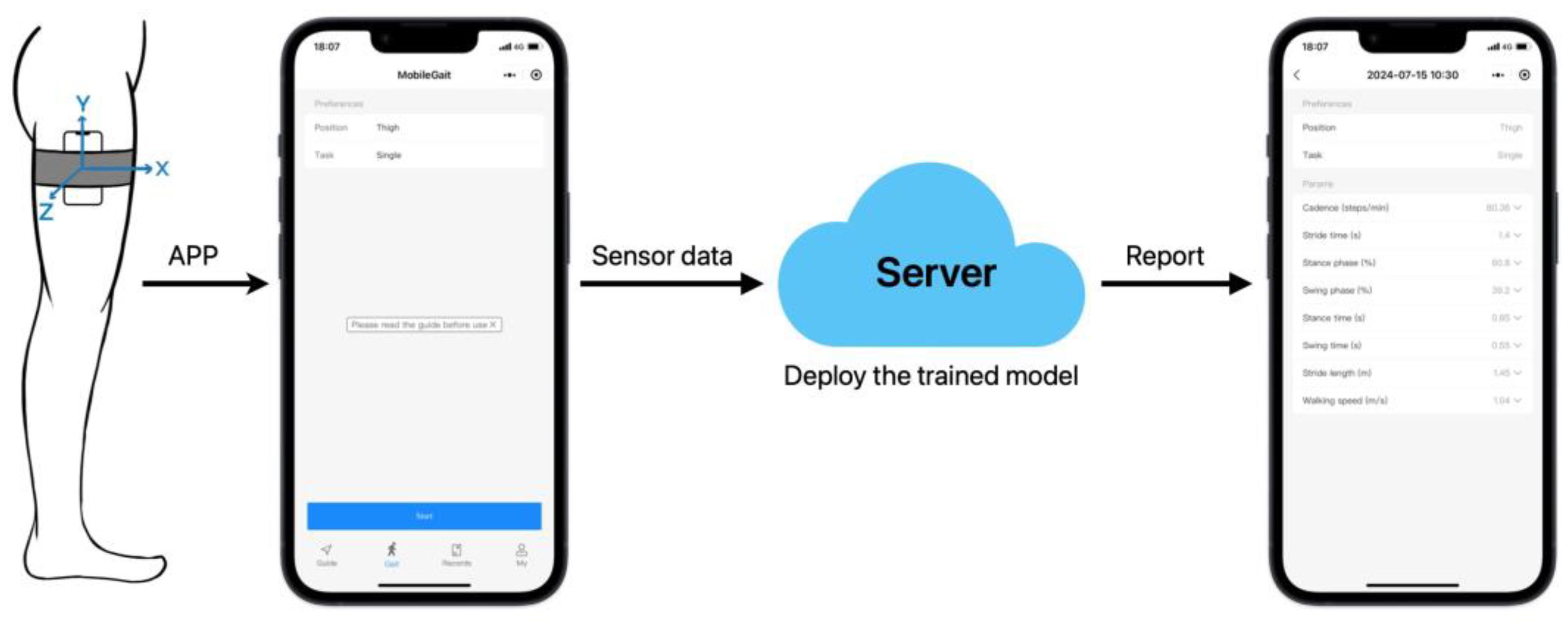
2.1. Software Platform
2.2. Participants
2.3. Experimental Design
3. Experiments and Results
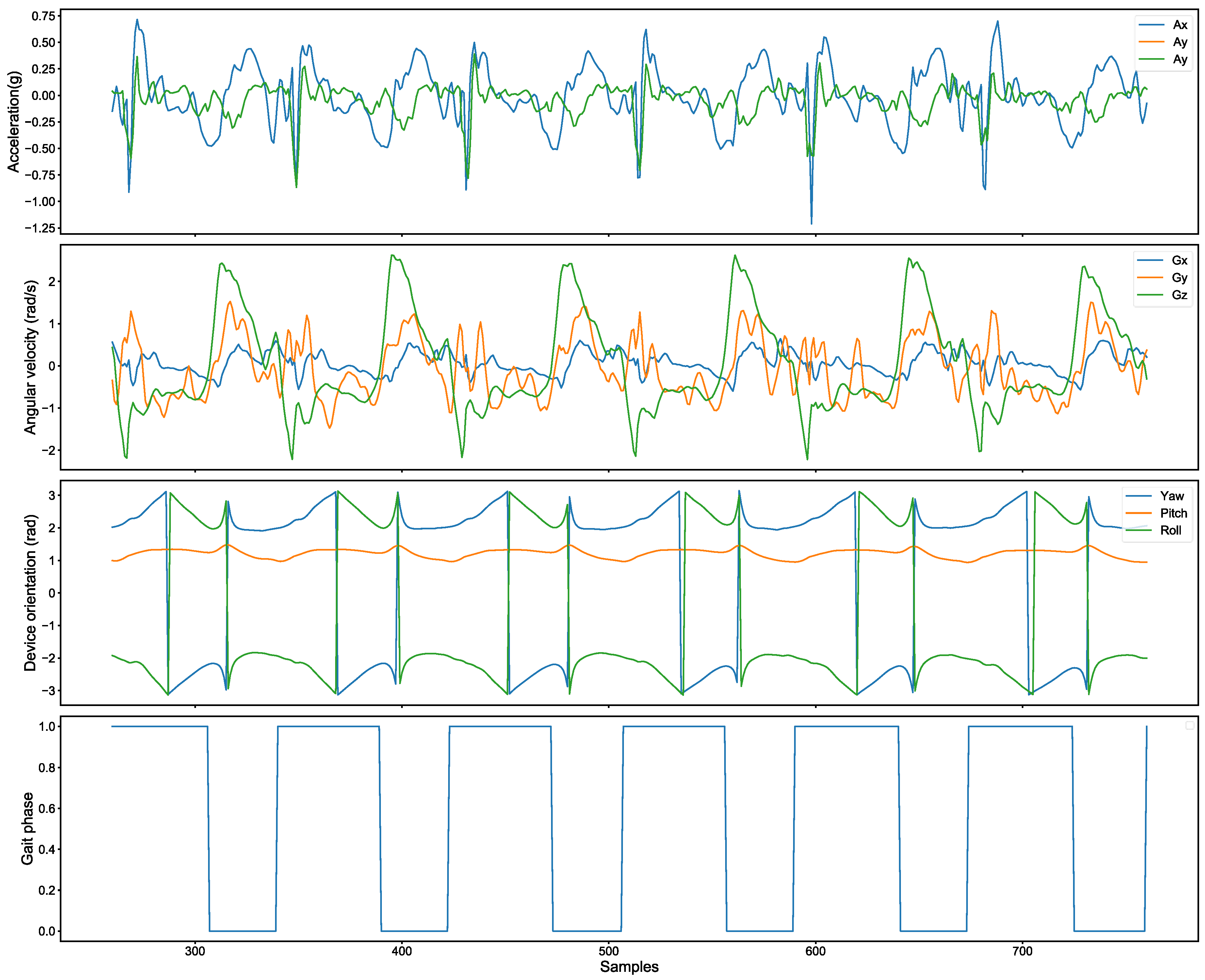
3.1. Data Collection and Processing
3.2. Building Dataset
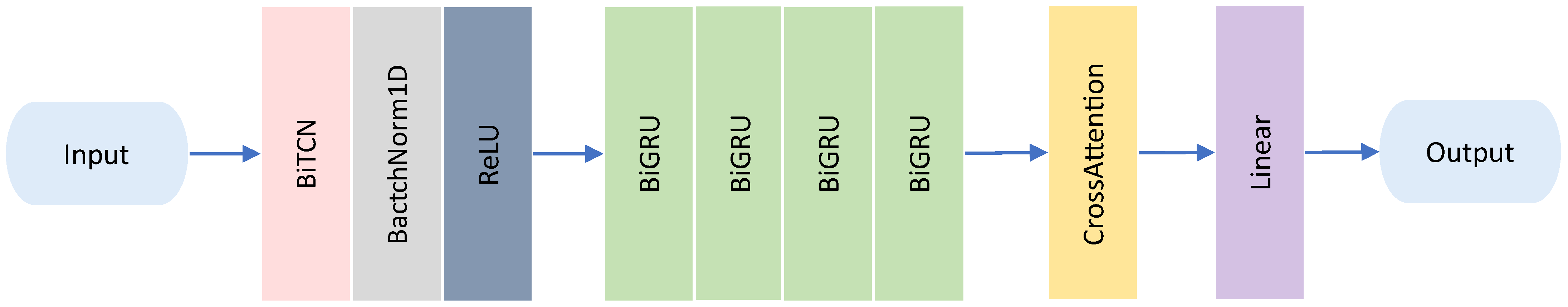
3.3. Deep Learning Models
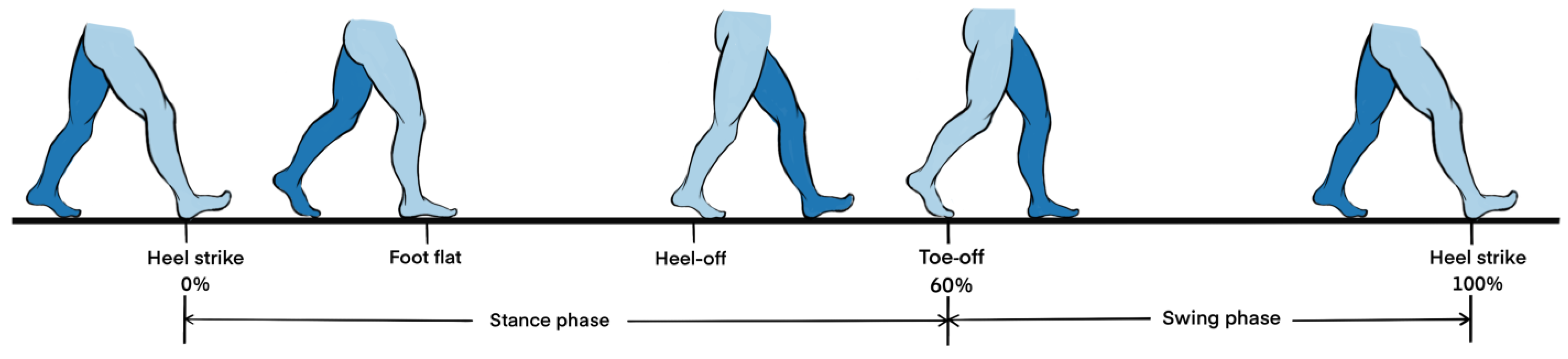
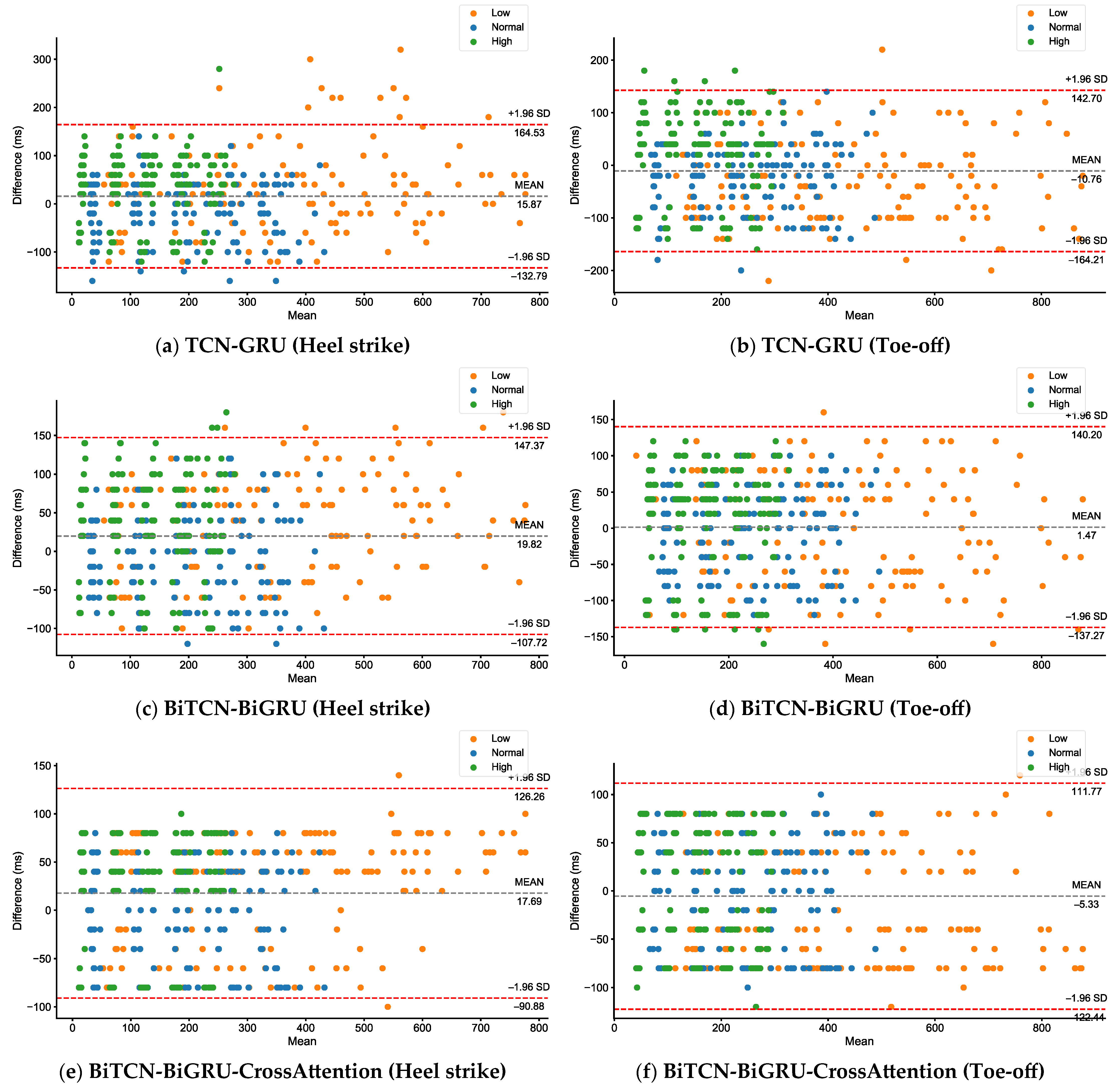
3.4. Error Measurement
3.5. Calculation of Gait Parameters
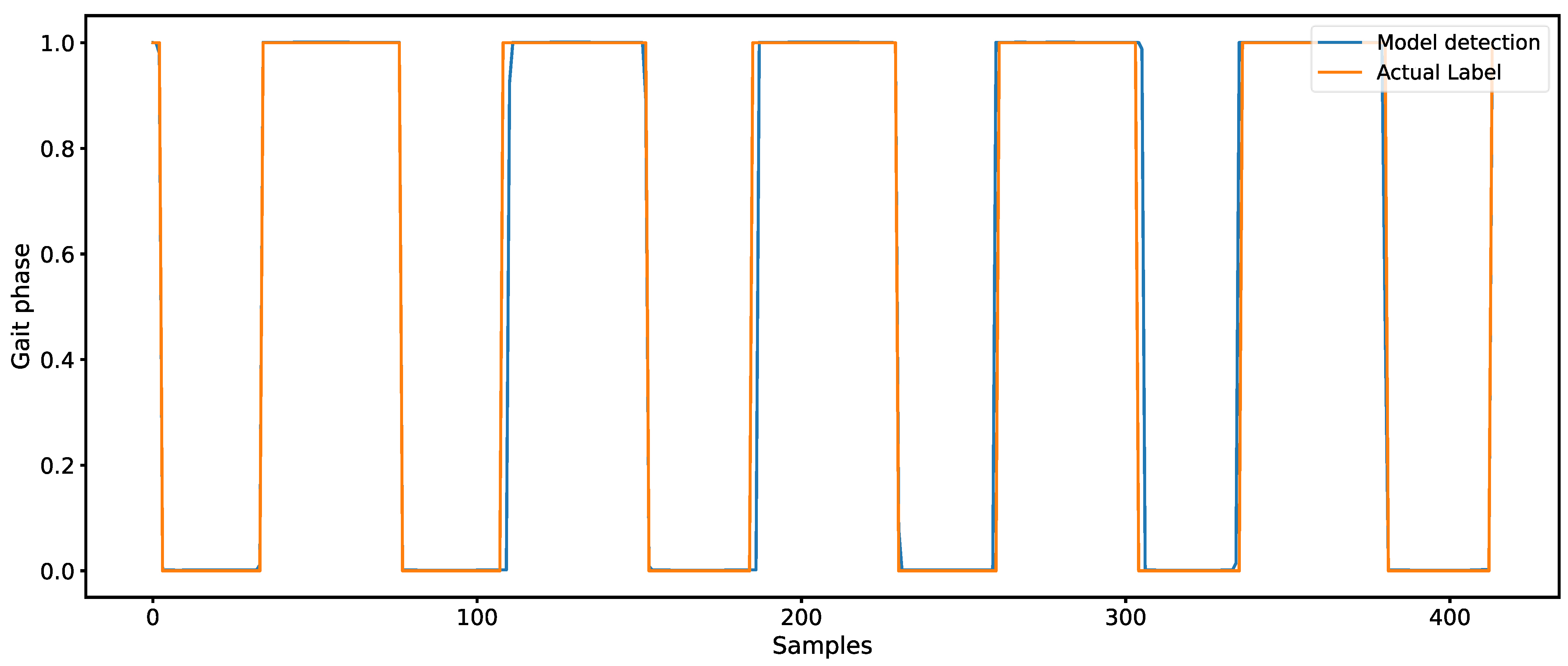
3.6. Result
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hansen, A.H.; Childress, D.S.; Meier, M.R. A simple method for determination of gait events. J. Biomech. 2002, 35, 135–138. [Google Scholar] [CrossRef] [PubMed]
- Borzelli, D.; Marchis, C.D.; Quercia, A. Muscle Synergy Analysis as a Tool for Assessing the Effectiveness of Gait Rehabilitation Therapies: A Methodological Review and Perspective. Bioengineering 2024, 11, 793. [Google Scholar] [CrossRef]
- Bonanno, M.; Nunzio, A.M.D.; Quartarone, A. Gait Analysis in Neurorehabilitation: From Research to Clinical Practice. Bioengineering 2023, 10, 785. [Google Scholar] [CrossRef]
- Grouios, G.; Ziagkas, E.; Loukovitis, A.; Chatzinikolaou, K.; Koidou, E. Accelerometers in Our Pocket: Does Smartphone Accelerometer Technology Provide Accurate Data? Sensors 2022, 23, 192. [Google Scholar] [CrossRef]
- Zhong, R.; Rau, P.-L.P. A Mobile Phone–Based Gait Assessment App for the Elderly: Development and Evaluation. JMIR Mhealth Uhealth 2020, 8, e14453. [Google Scholar] [CrossRef]
- Tang, S.T.; Tai, C.H.; Yang, C.Y.; Lin, J.H. Feasibility of Smartphone-Based Gait Assessment for Parkinson’s Disease. J. Med. Biol. Eng. 2020, 40, 582–591. [Google Scholar] [CrossRef]
- Tao, S.; Zhang, H.; Kong, L.; Sun, Y.; Zhao, J. Validation of gait analysis using smartphones: Reliability and validity. Digit Health 2024, 10, 20552076241257054. [Google Scholar] [CrossRef] [PubMed]
- Furrer, M.; Bichsel, L.; Niederer, M.; Baur, H.; Schmid, S. Validation of a smartphone-based measurement tool for the quantification of level walking. Gait Posture 2015, 42, 289–294. [Google Scholar] [CrossRef] [PubMed]
- Silsupadol, P.; Teja, K.; Lugade, V. Reliability and validity of a smartphone-based assessment of gait parameters across walking speed and smartphone locations: Body, bag, belt, hand, and pocket. Gait Posture 2017, 58, 516–522. [Google Scholar] [CrossRef]
- Manor, B.; Yu, W.; Zhu, H. Smartphone App–Based Assessment of Gait During Normal and Dual-Task Walking: Demonstration of Validity and Reliability. JMIR Mhealth Uhealth 2018, 6, e36. [Google Scholar] [CrossRef]
- Shahar, R.T.; Agmon, M. Gait Analysis Using Accelerometry Data from a Single Smartphone: Agreement and Consistency between a Smartphone Application and Gold-Standard Gait Analysis System. Sensors 2021, 21, 7497. [Google Scholar] [CrossRef]
- Shema-Shiratzky, S.; Beer, Y.; Mor, A.; Elbaz, A. Smartphone-based inertial sensors technology—Validation of a new application to measure spatiotemporal gait metrics. Gait Posture 2022, 93, 102–106. [Google Scholar] [CrossRef]
- La, R.M.; Rabinovich, M.I.; Huerta, R.; Abarbanel, H.D.I.; Fortuna, L. Slow regularization through chaotic oscillation transfer in an unidirectional chain of Hindmarsh–Rose models. Phys. Lett. A 2000, 266, 88–93. [Google Scholar]
- Zhao, Q.; Qiu, X.; Liu, W.; Nian, Z.; Chen, T. Application of a WeChat Mini Program to provide pharmaceutical care for cancer pain patients: A randomized controlled trial. Digit Health 2024, 10, 20552076241255654. [Google Scholar] [CrossRef]
- Fazekas, F.; Chawluk, J.B.; Alavi, A.; Hurtig, H.I.; Zimmerman, R.A. MR signal abnormalities at 1.5 T in Alzheimer’s dementia and normal aging. Am. J. Roentgenol. 1987, 149, 351–356. [Google Scholar] [CrossRef] [PubMed]
- Trojaniello, D.; Cereatti, A.; Pelosin, E. Estimation of step-by-step spatio-temporal parameters of normal and impaired gait using shank-mounted magneto-inertial sensors: Application to elderly, hemiparetic, parkinsonian and choreic gait. J. Neuroeng. Rehabil. 2014, 11, 152. [Google Scholar] [CrossRef] [PubMed]
- Warmerdam, E.; Orth, M.; Pohlemann, T.; Ganse, B. Gait Analysis to Monitor Fracture Healing of the Lower Leg. Bioengineering 2023, 10, 255. [Google Scholar] [CrossRef]
- Arshad, M.Z.; Jamsrandorj, A.; Kim, J.; Mun, K.-R. Gait Events Prediction Using Hybrid CNN-RNN-Based Deep Learning Models through a Single Waist-Worn Wearable Sensor. Sensors 2022, 22, 8226. [Google Scholar] [CrossRef]
- Ho, N.-H.; Truong, P.; Jeong, G.-M. Step-Detection and Adaptive Step-Length Estimation for Pedestrian Dead-Reckoning at Various Walking Speeds Using a Smartphone. Sensors 2016, 16, 1423. [Google Scholar] [CrossRef]
- Fadillioglu, C.; Stetter, B.J.; Ringhof, S. Automated gait event detection for a variety of locomotion tasks using a novel gyroscope-based algorithm. Gait Posture 2020, 81, 102–108. [Google Scholar] [CrossRef]
- González, R.C.; López, A.M.; Rodriguez-Uría, J.; Alvarez, D.; Alvarez, J.C. Real-time gait event detection for normal subjects from lower trunk accelerations. Gait Posture 2010, 31, 322–325. [Google Scholar] [CrossRef]
- Soaz, C.; Diepold, K. Step Detection and Parameterization for Gait Assessment Using a Single Waist-Worn Accelerometer. IEEE T Bio-Med. Eng. 2016, 63, 933–942. [Google Scholar] [CrossRef]
- Pepa, L.; Verdini, F.; Spalazzi, L. Gait parameter and event estimation using smartphones. Gait Posture 2017, 57, 217–223. [Google Scholar] [CrossRef]
- Hoang, T.; Nguyen, T.D.; Luong, C.; Do, S.; Deokjai, C. Adaptive Cross-Device Gait Recognition Using a Mobile Accelerometer. J. Inf. Process Syst. 2013, 9, 333–348. [Google Scholar] [CrossRef]
- Montero-Odasso, M.M.; Sarquis-Adamson, Y.; Speechley, M. Association of dual-task gait with incident dementia in mild cognitive impairment: Results from the gait and brain study. JAMA Neurol. 2017, 74, 857–865. [Google Scholar] [CrossRef] [PubMed]
- Montero-Odasso, M.; Oteng-Amoakoet, A.; Speechley, M. The motor signature of mild cognitive impairment: Results from the gait and brain study. J. Gerontol. A-Biol. 2014, 69, 1415–1421. [Google Scholar] [CrossRef] [PubMed]
- Kelly, V.E.; Eusterbrock, A.J.; Shumway-Cook, A. A Review of Dual-Task Walking Deficits in People with Parkinson′s Disease: Motor and Cognitive Contributions, Mechanisms, and Clinical Implications. Parkinsons Dis. 2012, 2012, 918719. [Google Scholar] [PubMed]
- Nonnekes, J.; Snijderset, A.H.; Nuttal, P.J.G. Freezing of gait: A practical approach to management. Lancet Neurol. 2015, 14, 768–778. [Google Scholar] [CrossRef]
- Creaby, M.W.; Cole, M.H. Gait characteristics and falls in Parkinson’s disease: A systematic review and meta-analysis. Parkinsonism Relat. D 2018, 57, 1–8. [Google Scholar] [CrossRef]
- Prins, N.D.; Scheltens, P. White matter hyperintensities, cognitive impairment and dementia: An update. Nat. Rev. Neurol. 2015, 11, 157–165. [Google Scholar] [CrossRef]
- Kim, Y.J.; Kwon, H.K.; Lee, J.M. Gray and white matter changes linking cerebral small vessel disease to gait disturbances. Neurology 2016, 86, 1199–1207. [Google Scholar] [CrossRef]
- Laat, K.F.; Norden, A.G.W.; Gons, R.A.R. Gait in elderly with cerebral small vessel disease. Stroke 2010, 41, 1652–1658. [Google Scholar] [CrossRef] [PubMed]
- Wardlaw, J.M.; Debette, S.; Jokinen, H. ESO Guideline on covert cerebral small vessel disease. Eur. Stroke J. 2021, 6, 111–162. [Google Scholar] [CrossRef] [PubMed]
- Wardlaw, J.M.; Smith, C.; Dichgans, M. Small vessel disease: Mechanisms and clinical implications. Lancet Neurol. 2019, 18, 684–696. [Google Scholar] [CrossRef] [PubMed]
- Ghanavati, T.; Smitt, M.S.; Lord, S.R. Deep white matter hyperintensities, microstructural integrity and dual task walking in older people. Brain Imaging Behav. 2018, 12, 1488–1496. [Google Scholar] [CrossRef]
- Ma, R.; Zhào, H.; Wei, W.; Liu, Y.; Huang, Y. Gait characteristics under single-/dual-task walking conditions in elderly patients with cerebral small vessel disease: Analysis of gait variability, gait asymmetry and bilateral coordination of gait. Gait Posture 2022, 92, 65–70. [Google Scholar] [CrossRef]
- Roccetti, M.; Delnevo, G.; Casini, L.; Cappiello, G. Is bigger always better? A controversial journey to the center of machine learning design, with uses and misuses of big data for predicting water meter failures. J. Big Data 2019, 6, 70. [Google Scholar] [CrossRef]
| Participant | Feature | Age Range | |||||
|---|---|---|---|---|---|---|---|
| 20~29 | 30~39 | 40~49 | 50~59 | 60~69 | 70~79 | ||
| Health (N = 150) | Male | 11 | 14 | 13 | 16 | 14 | 13 |
| Female | 11 | 11 | 12 | 13 | 12 | 10 | |
| Age (years) | 25.55 ± 2.60 | 35.40 ± 2.65 | 45.08 ± 2.50 | 55.21 ± 2.61 | 64.65 ± 2.71 | 73.96 ± 2.33 | |
| Height (cm) | 171.55 ± 8.78 | 169.00 ± 6.23 | 169.40 ± 8.36 | 169.38 ± 7.52 | 167.85 ± 9.57 | 166.37 ± 9.41 | |
| Weight (kg) | 63.80 ± 9.50 | 64.96 ± 6.81 | 64.86 ± 6.57 | 63.50 ± 6.03 | 64.65 ± 2.71 | 62.96 ± 7.35 | |
| Elderly (N = 48) | Male | - | - | - | - | 6 | 20 |
| Female | - | - | - | - | 10 | 12 | |
| Age (years) | - | - | - | - | 64.25 ± 2.79 | 75.31 ± 3.21 | |
| Height (cm) | - | - | - | - | 163.75 ± 7.03 | 165.25 ± 7.49 | |
| Weight (kg) | - | - | - | - | 67.31 ± 12.82 | 63.97 ± 9.37 | |
| CSVD (N = 34) | Male | - | - | - | 1 | 7 | 16 |
| Female | - | - | - | 1 | 3 | 6 | |
| Age (years) | - | - | - | 58.50 ± 0.71 | 64.10 ± 2.69 | 74.91 ± 2.69 | |
| Height (cm) | - | - | - | 167.00 ± 7.07 | 171.00 ± 7.90 | 169.96 ± 8.22 | |
| Weight (kg) | - | - | - | 70.00 ± 14.14 | 69.95 ± 8.19 | 68.64 ± 8.11 | |
| Gait Events | Speed | Model | ||
|---|---|---|---|---|
| TCN-GRU | BiTCN-BiGRU | BiTCN-BiGRU-CrossAttention | ||
| Heel strike | Normal | 47.87 ± 1.99 | 45.47 ± 1.64 | 42.53 ± 1.25 |
| Low | 66.80 ± 3.14 | 62.93 ± 1.86 | 58.40 ± 1.07 | |
| High | 65.20 ± 1.92 | 61.73 ± 1.99 | 56.93 ± 1.22 | |
| Toe-off | Normal | 49.60 ± 2.15 | 47.73 ± 1.62 | 45.47 ± 1.45 |
| Low | 73.06 ± 2.28 | 67.73 ± 1.79 | 59.20 ± 1.13 | |
| High | 72.00 ± 2.14 | 65.46 ± 1.97 | 58.27 ± 1.09 | |
| Participant | Task and p | Gait Parameters | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Cadence (Steps/min) | Stride Time (s) | Stance Phase (%) | Swing Phase (%) | Stance Time (s) | Swing Time (s) | Stride Length (m) | Walking Speed (m/s) | ||
| Elderly (Health) | STW | 100.08 ± 3.79 | 1.18 ± 0.07 | 64.19 ± 1.52 | 35.81 ± 1.52 | 0.76 ± 0.06 | 0.42 ± 0.02 | 1.21 ± 0.17 | 1.04 ± 0.16 |
| VFT | 84.27 ± 7.10 | 1.44 ± 0.13 | 68.40 ± 1.44 | 31.60 ± 1.44 | 0.98 ± 0.10 | 0.45 ± 0.04 | 1.02 ± 0.14 | 0.72 ± 0.12 | |
| STW/VFT | 0.000 * | 0.000 * | 0.000 * | 0.000 * | 0.000 * | 0.000 * | 0.000 * | 0.000 * | |
| Elderly (MCI) | STW | 96.47 ± 5.78 | 1.22 ± 0.07 | 65.64 ± 2.24 | 34.36 ± 2.24 | 0.80 ± 0.07 | 0.42 ± 0.02 | 1.15 ± 0.14 | 0.94 ± 0.14 |
| VFT | 78.37 ± 8.40 | 1.55 ± 0.21 | 69.47 ± 2.16 | 30.53 ± 2.16 | 1.08 ± 0.15 | 0.47 ± 0.06 | 0.96 ± 0.16 | 0.63 ± 0.10 | |
| STW/VFT | 0.000 * | 0.002 * | 0.000 * | 0.000 * | 0.002 * | 0.003 * | 0.000 * | 0.000 * | |
| Elderly (PD) | STW | 96.23 ± 6.76 | 1.20 ± 0.10 | 65.00 ± 1.98 | 35.00 ± 1.98 | 0.78 ± 0.09 | 0.42 ± 0.02 | 1.00 ± 0.13 | 0.84 ± 0.15 |
| VFT | 77.63 ± 13.88 | 1.57 ± 0.39 | 69.63 ± 3.32 | 30.37 ± 3.32 | 1.10 ± 0.34 | 0.47 ± 0.06 | 0.86 ± 0.15 | 0.58 ± 0.18 | |
| STW/VFT | 0.000 * | 0.003 * | 0.000 * | 0.000 * | 0.003 * | 0.015 * | 0.000 * | 0.000 * | |
| CSVD | STW | 93.97 ± 8.98 | 1.29 ± 0.12 | 67.72 ± 2.65 | 32.28 ± 2.65 | 0.87 ± 0.10 | 0.42 ± 0.04 | 0.85 ± 0.17 | 0.67 ± 0.16 |
| VFT | 80.18 ± 10.85 | 1.53 ± 0.22 | 72.19 ± 3.257 | 27.81 ± 3.26 | 1.11 ± 0.191 | 0.42 ± 0.05 | 0.66 ± 0.17 | 0.44 ± 0.15 | |
| PTW | 85.87 ± 11.46 | 1.41 ± 0.18 | 70.43 ± 3.48 | 29.57 ± 3.48 | 1.00 ± 0.16 | 0.41 ± 0.05 | 0.72 ± 0.21 | 0.52 ± 0.18 | |
| STW/VFT | 0.000 * | 0.000 * | 0.000 * | 0.000 * | 0.000 * | 0.532 | 0.000 * | 0.000 * | |
| STW/PTW | 0.000 * | 0.000 * | 0.000 * | 0.000 * | 0.000 * | 0.779 | 0.000 * | 0.000 * | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xu, K.; Yu, W.; Yu, S.; Zheng, M.; Zhang, H. The Detection of Gait Events Based on Smartphones and Deep Learning. Bioengineering 2025, 12, 491. https://doi.org/10.3390/bioengineering12050491
Xu K, Yu W, Yu S, Zheng M, Zhang H. The Detection of Gait Events Based on Smartphones and Deep Learning. Bioengineering. 2025; 12(5):491. https://doi.org/10.3390/bioengineering12050491
Chicago/Turabian StyleXu, Kaiyue, Wenqiang Yu, Shui Yu, Minghui Zheng, and Hao Zhang. 2025. "The Detection of Gait Events Based on Smartphones and Deep Learning" Bioengineering 12, no. 5: 491. https://doi.org/10.3390/bioengineering12050491
APA StyleXu, K., Yu, W., Yu, S., Zheng, M., & Zhang, H. (2025). The Detection of Gait Events Based on Smartphones and Deep Learning. Bioengineering, 12(5), 491. https://doi.org/10.3390/bioengineering12050491






