3D Photogrammetry-Driven Craniofacial Analysis in Orthodontics: A Scoping Review of Recent Applications
Abstract
1. Introduction
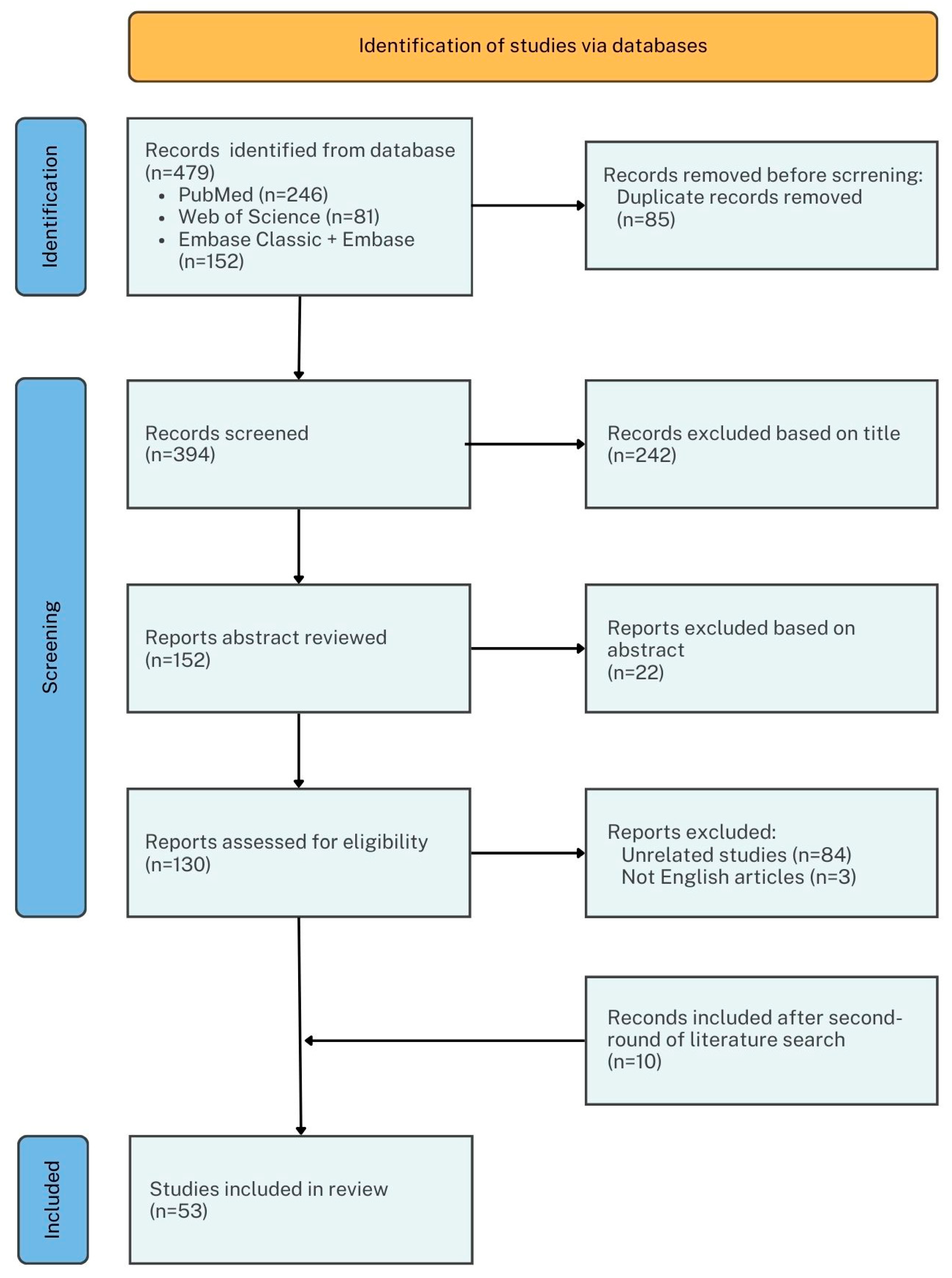
2. Materials and Methods
2.1. Protocol
2.2. Eligibility Criteria
2.3. Information Sources and Search
2.4. Study Selection
2.5. Data Extraction and Synthesis
3. Results
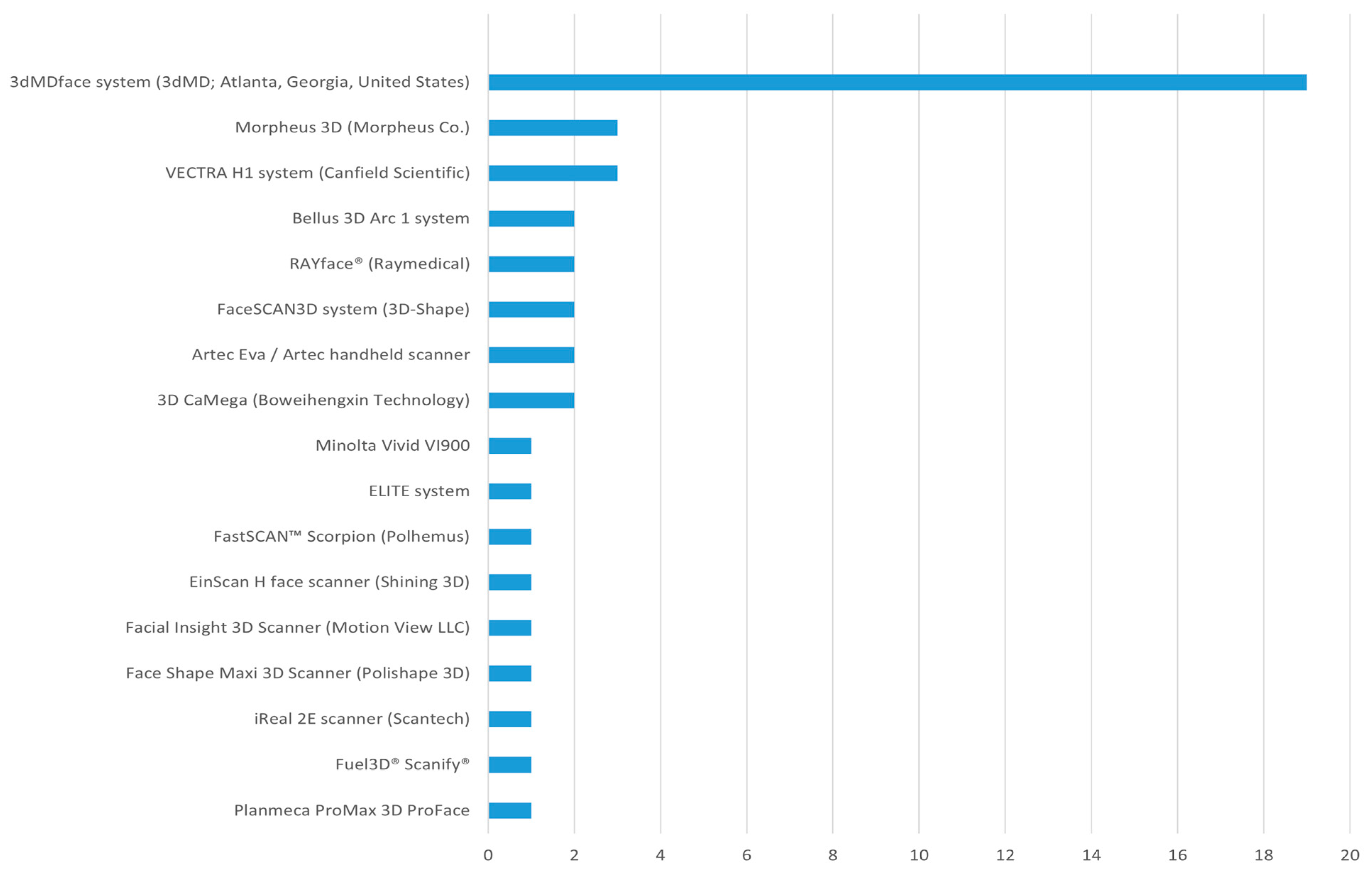
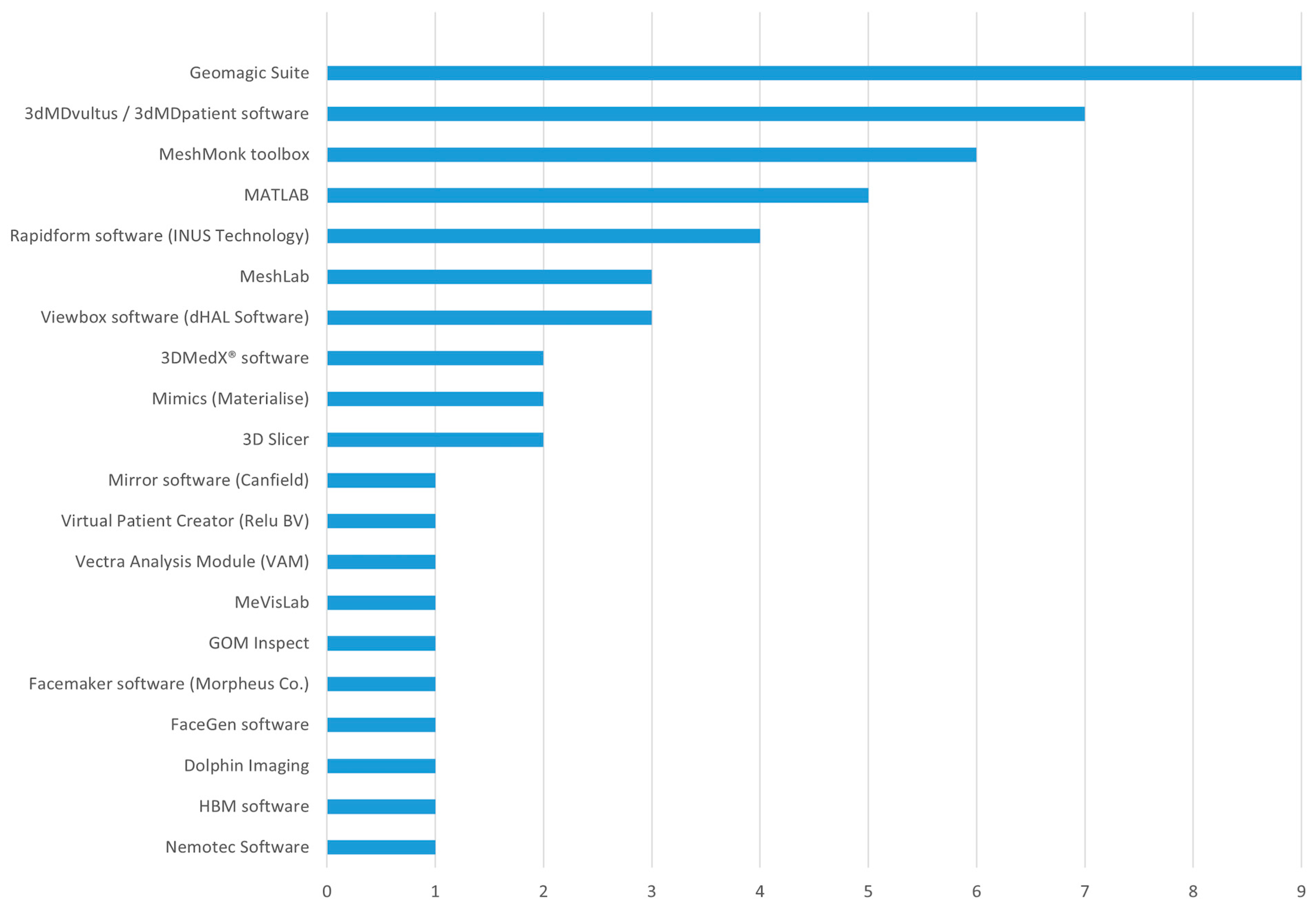
3.1. Selections and Characteristics of Included Studies
3.2. Normative Facial Anthropometry
3.3. Orthodontic Problem Finding
3.4. Orthodontic Treatment Optimization
3.5. Treatment Outcome Evaluation
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| 2D | Two-dimensional |
| 3D | Three-dimensional |
| CBCT | Cone beam computed tomography |
| PRISMA-ScR | Systematic Reviews and Meta-Analyses extension for Scoping Reviews |
| IT | Imaging tools |
| S | Software |
References
- Gao, P.C.; Zhao, Z.Q.; Chen, Y.L.; Zhao, Y.; Xie, L.Z.; Yan, B.; Wang, L. Accuracy of three-dimensional camera system based on stereophotography on photographic acquisition of deformity facial images. Hua Xi Kou Qiang Yi Xue Za Zhi 2019, 37, 174–179. [Google Scholar]
- Aljawad, H.; Lim, H.J.; Lee, K.C. Anthropometric Comparison of 3-Dimensional Facial Scan Taken with a Low-Cost Facial Scanner with Cone-Beam Computed Tomography Scan. J. Craniofac. Surg. 2023, 34, 1456–1458. [Google Scholar] [CrossRef]
- Gašparović, B.; Morelato, L.; Lenac, K.; Mauša, G.; Zhurov, A.; Katić, V. Comparing Direct Measurements and Three-Dimensional (3D) Scans for Evaluating Facial Soft Tissue. Sensors 2023, 23, 2412. [Google Scholar] [CrossRef]
- Spalj, S.; Slaj, M.; Varga, S.; Strujic, M.; Slaj, M. Perception of orthodontic treatment need in children and adolescents. Eur. J. Orthod. 2010, 32, 387–394. [Google Scholar] [CrossRef] [PubMed]
- Angelieri, F.; Cevidanes, L.H.; Franchi, L.; Gonçalves, J.R.; Benavides, E.; McNamara, J.A., Jr. Midpalatal suture maturation: Classification method for individual assessment before rapid maxillary expansion. Am. J. Orthod. Dentofac. Orthop. 2013, 144, 759–769. [Google Scholar] [CrossRef] [PubMed]
- Kau, C.H.; Richmond, S.; Incrapera, A.; English, J.; Xia, J.J. Three-dimensional surface acquisition systems for the study of facial morphology and their application to maxillofacial surgery. Int. J. Med. Robot. 2007, 3, 97–110. [Google Scholar] [CrossRef]
- Doan, J.; Finlay, N.; Lee, A.; Ethell, T.; Gandedkar, N.; Darendeliler, M.A. The accuracy (trueness and precision) of Bellus3DARC-7 and an in-vivo analysis of intra and inter-examiner reliability of digital and manual anthropometry. Aust. Orthod. J. 2023, 39, 141–157. [Google Scholar] [CrossRef]
- Andrews, J.; Alwafi, A.; Bichu, Y.M.; Pliska, B.T.; Mostafa, N.; Zou, B. Validation of three-dimensional facial imaging captured with smartphone-based photogrammetry application in comparison to stereophotogrammetry system. Heliyon 2023, 9, e15834. [Google Scholar] [CrossRef]
- Barone, S.; Antonelli, A.; Salviati, M.; Greco, V.; Bennardo, F.; Becker, K.; Giudice, A.; Simeone, M. Accuracy Assessment of EM3D App-Based 3D Facial Scanning Compared to Cone Beam Computed Tomography. Dent. J. 2024, 12, 342. [Google Scholar] [CrossRef]
- Pellitteri, F.; Scisciola, F.; Cremonini, F.; Baciliero, M.; Lombardo, L. Accuracy of 3D facial scans: A comparison of three different scanning system in an in vivo study. Prog. Orthod. 2023, 24, 44. [Google Scholar] [CrossRef]
- Mao, B.; Li, J.; Tian, Y.; Zhou, Y. The accuracy of a three-dimensional face model reconstructing method based on conventional clinical two-dimensional photos. BMC Oral. Health 2022, 22, 413. [Google Scholar] [CrossRef]
- Pan, F.; Liu, J.; Cen, Y.; Chen, Y.; Cai, R.; Zhao, Z.; Liao, W.; Wang, J. Accuracy of RGB-D camera-based and stereophotogrammetric facial scanners: A comparative study. J. Dent. 2022, 127, 104302. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Bhaskar, E.; Kau, C.H. A Comparison of 3D Facial Features in a Population from Zimbabwe and United States. Eur. J. Dent. 2020, 14, 100–106. [Google Scholar] [CrossRef]
- Kau, C.H.; Wang, J.; Davis, M. A Cross-Sectional Study to Understand 3D Facial Differences in a Population of African Americans and Caucasians. Eur. J. Dent. 2019, 13, 485–496. [Google Scholar] [CrossRef]
- Rajbhoj, A.A.; Matthews, H.; Doucet, K.; Claes, P.; Willems, G.; Begnoni, G.; Cadenas de Llano-Pérula, M. Age- and sex-related differences in 3D facial shape and muscle pressure in subjects with normal occlusion. Comput. Biol. Med. 2022, 151, 106325. [Google Scholar] [CrossRef]
- Mengoa, M.G.R.; Garcia, A.; Fioravanti, K.S.; Neppelenbroek, K.H.; Oliveira, T.M.; Sforza, C.; Soares, S. Facial morphology analysis of Caucasian Brazilian adult women using stereophotogrammetry. Braz. Oral. Res. 2024, 38, e105. [Google Scholar] [PubMed]
- Cenzato, N.; Farronato, M.; Tartaglia, F.C.; Giannini, L.; Inchingolo, A.M.; Dipalma, G.; Maspero, C.; Inchingolo, F. Soft Tissue Facial Morphology in Growing Patients with Different Occlusal Classes. J. Pers. Med. 2024, 14, 1042. [Google Scholar] [CrossRef]
- Menéndez López-Mateos, M.L.; Carreño-Carreño, J.; Palma, J.C.; Alarcón, J.A.; Menéndez López-Mateos, C.; Menéndez-Núñez, M. Three-dimensional photographic analysis of the face in European adults from southern Spain with normal occlusion: Reference anthropometric measurements. BMC Oral. Health 2019, 19, 196. [Google Scholar] [CrossRef] [PubMed]
- Tanikawa, C.; Akcam, M.O.; Takada, K. Quantifying faces three-dimensionally in orthodontic practice. J. Craniomaxillofac. Surg. 2019, 47, 867–875. [Google Scholar] [CrossRef]
- Fan, Y.; He, W.; Chen, G.; Song, G.; Matthews, H.; Claes, P.; Jiang, R.; Xu, T. Facial asymmetry assessment in skeletal Class III patients with spatially-dense geometric morphometrics. Eur. J. Orthod. 2022, 44, 155–162. [Google Scholar] [CrossRef] [PubMed]
- Gkantidis, N.; Opacic, J.; Kanavakis, G.; Katsaros, C.; Halazonetis, D. Facial asymmetry and midsagittal plane definition in 3D: A bias-free, automated method. PLoS ONE 2023, 18, e0294528. [Google Scholar] [CrossRef] [PubMed]
- Lyu, L.; Zhang, M.J.; Wen, A.N.; Wang, S.; Zhao, Y.J.; Yong, W.; Yu, T.T.; Liu, D. 3D facial mask for facial asymmetry diagnosis. Heliyon 2024, 10, e26734. [Google Scholar] [CrossRef]
- Zhu, Y.; Fu, X.; Zhang, L.; Zheng, S.; Wen, A.; Xiao, N.; Wang, Y.; Zhao, Y. A mathematical algorithm of the facial symmetry plane: Application to mandibular deformity 3D facial data. J. Anat. 2022, 240, 556–566. [Google Scholar] [CrossRef] [PubMed]
- Dindaroğlu, F.; Fırıncıoğulları, E.C.; Duran, G.S. Three-dimensional evaluation of social smile asymmetry in patients with unilateral impacted maxillary canine: A 3D stereophotogrammetry study. Clin. Oral. Investig. 2023, 27, 6915–6924. [Google Scholar] [CrossRef]
- Li, H.; Cao, T.; Zhou, H.; Hou, Y. Lip position analysis of young women with different skeletal patterns during posed smiling using 3-dimensional stereophotogrammetry. Am. J. Orthod. Dentofac. Orthop. 2019, 155, 64–70. [Google Scholar] [CrossRef]
- Cho, S.W.; Byun, S.H.; Yi, S.; Jang, W.S.; Kim, J.C.; Park, I.Y.; Yang, B.E. Sagittal Relationship between the Maxillary Central Incisors and the Forehead in Digital Twins of Korean Adult Females. J. Pers. Med. 2021, 11, 203. [Google Scholar] [CrossRef]
- Wang, T.; Nie, K.; Fan, Y.; Chen, G.; Xu, K.; Han, B.; Pei, Y.; Song, G.; Xu, T. Network analysis of three-dimensional hard-soft tissue relationships in the lower 1/3 of the face: Skeletal Class I-normodivergent malocclusion versus Class II-hyperdivergent malocclusion. BMC Oral. Health 2024, 24, 996. [Google Scholar] [CrossRef]
- Coppola, G.; Hänggi, D.; Cassina, G.; Verna, C.; Gkantidis, N.; Kanavakis, G. Three-dimensional video recordings: Accuracy, reliability, clinical and research guidelines—Reliability assessment of a 4D camera. Orthod. Craniofac. Res. 2024, 27, 803–812. [Google Scholar] [CrossRef]
- Fiorillo, G.; Garrisi, L.; Mandelli, A.; Arnò, F.; Mandelli, G.; Gastaldi, G. Design and manufacturing of a fully digital protraction facemask. AJO-DO Clin. Companion 2024, 4, 165–173. [Google Scholar] [CrossRef]
- Akan, B.; Veli, İ. Evaluation of soft-tissue changes in young adults treated with the Forsus fatigue-resistant device. Am. J. Orthod. Dentofac. Orthop. 2020, 157, 481–489.e482. [Google Scholar] [CrossRef]
- Yüksel Coşkun, E.; Esenlik, E. A Prospective Study Comparing Adolescent and Post-Adolescent Periods Regarding Effects of Activator Appliance in Patients with Class II Mandibular Retrognathia by Using 3dMDface Analysis and Cephalometry. Med. Sci. Monit. 2020, 26, e921401. [Google Scholar] [CrossRef]
- Hou, S.Y.; Zhou, W.; Dai, H.; Wong, H.M.; Wen, Y.F.; Zhou, J. Soft tissue facial changes among adult females during alignment stage of orthodontic treatment: A 3D geometric morphometric study. BMC Oral. Health 2021, 21, 57. [Google Scholar] [CrossRef]
- Jindanil, T.; Burlacu-Vatamanu, O.E.; Meyns, J.; Meewis, J.; Fontenele, R.C.; Perula, M.C.L.; Jacobs, R. Automated orofacial virtual patient creation: A proof of concept. J. Dent. 2024, 150, 105387. [Google Scholar] [CrossRef]
- Ponnusamy, A.; Goonewardene, M.S.; Mian, A.; Eastwood, P.; Rea, A.; Islam, S. Facial soft tissue norms in Caucasians using an innovative three-dimensional approach. Australas. Orthod. J. 2020, 36, 45–54. [Google Scholar] [CrossRef]
- Dong, T.; Ye, N.; Yuan, L.; Wu, S.; Xia, L.; Fang, B. Assessing the Influence of Chin Asymmetry on Perceived Facial Esthetics with 3-Dimensional Images. J. Oral. Maxillofac. Surg. 2020, 78, 1389–1396. [Google Scholar] [CrossRef] [PubMed]
- Fastuca, R.; Beccarini, T.; Rossi, O.; Zecca, P.A.; Caprioglio, A. Influence of facial components in class III malocclusion esthetic perception of orthodontists, patients, and laypersons. J. Orofac. Orthop. 2022, 83, 48–58. [Google Scholar] [CrossRef] [PubMed]
- Feng, J.; Yu, H.; Yin, Y.; Yan, Y.; Wang, Z.; Bai, D.; Han, X. Esthetic evaluation of facial cheek volume: A study using 3D stereophotogrammetry. Angle Orthod. 2019, 89, 129–137. [Google Scholar] [CrossRef] [PubMed]
- Denadai, R.; Chou, P.Y.; Su, Y.Y.; Lin, H.H.; Ho, C.T.; Lo, L.J. The Impacts of Orthognathic Surgery on the Facial Appearance and Age Perception of Patients Presenting Skeletal Class III Deformity: An Outcome Study Using the FACE-Q Report and Surgical Professional-Based Panel Assessment. Plast. Reconstr. Surg. 2020, 145, 1035–1046. [Google Scholar] [CrossRef]
- Denadai, R.; Chou, P.Y.; Su, Y.Y.; Lo, C.C.; Lin, H.H.; Ho, C.T.; Lo, L.J. Facial Appearance and Psychosocial Features in Orthognathic Surgery: A FACE-Q- and 3D Facial Image-Based Comparative Study of Patient-, Clinician-, and Lay-Observer-Reported Outcomes. J. Clin. Med. 2019, 8, 909. [Google Scholar] [CrossRef]
- Güler, Ö.; Malkoç, S. Comparison of facial soft tissue changes after treatment with 3 different functional appliances. Am. J. Orthod. Dentofac. Orthop. 2020, 158, 518–526. [Google Scholar] [CrossRef]
- Akan, B.; Gökçe, G.; Şahan, A.O.; Veli, İ. Tooth-borne versus tooth-bone-borne rapid maxillary expanders according to a stereophotogrammetric evaluation of facial soft tissues: A randomized clinical trial. Orthod. Craniofac. Res. 2021, 24, 438–448. [Google Scholar] [CrossRef]
- Liu, Z.Y.; Yu, J.; Dai, F.F.; Jiang, R.P.; Xu, T.M. Three-dimensional changes in lip vermilion morphology of adult female patients after extraction and non-extraction orthodontic treatment. Korean J. Orthod. 2019, 49, 222–234. [Google Scholar] [CrossRef]
- Marino Merlo, M.; Quiroga Souki, B.; Nieri, M.; Bonanno, A.; Giuntini, V.; McNamara, J.A., Jr.; Franchi, L. Comparison of the effects on facial soft tissues produced by rapid and slow maxillary expansion using stereophotogrammetry: A randomized clinical trial. Prog. Orthod. 2024, 25, 1. [Google Scholar] [CrossRef] [PubMed]
- Sitaropoulou, V.; Yilmaz, H.N.; Yilmaz, B.; Kucukkeles, N. Three-dimensional evaluation of treatment results of the Alt-RAMEC and facemask protocol in growing patients. J. Orofac. Orthop. 2020, 81, 407–418. [Google Scholar] [CrossRef] [PubMed]
- Nike, E.; Radzins, O.; Pirttiniemi, P.; Vuollo, V.; Slaidina, A.; Abeltins, A. Evaluation of facial soft tissue asymmetric changes in Class III patients after orthognathic surgery using three-dimensional stereophotogrammetry. Int. J. Oral. Maxillofac. Surg. 2023, 52, 361–370. [Google Scholar] [CrossRef]
- Shi, Y.; Liu, S.; Shao, X.; Zong, C.; Bai, S.; Yang, Y.; Liu, Y.; Shang, H.; Tian, L. Facial changes in patients with skeletal class III deformity after bimaxillary surgery: An evaluation based on three-dimensional photographs registered with computed tomography. Br. J. Oral. Maxillofac. Surg. 2022, 60, 1404–1410. [Google Scholar] [CrossRef]
- Mao, B.; Tian, Y.; Li, J.; Zhou, Y.; Wang, X. A quantitative analysis of facial changes after orthodontic treatment with vertical control in patients with idiopathic condylar resorption. Orthod. Craniofac. Res. 2023, 26, 402–414. [Google Scholar] [CrossRef]
- Alkhayer, A.; Becsei, R.; Hegedűs, L.; Párkányi, L.; Piffkó, J.; Braunitzer, G.; Segatto, E. Evaluation of the Soft Tissue Changes after Rapid Maxillary Expansion Using a Handheld Three-Dimensional Scanner: A Prospective Study. Int. J. Environ. Res. Public Health 2021, 18, 3379. [Google Scholar] [CrossRef]
- Shen, L.H.; Xie, T.Y.; Jiang, R.P.; Jiang, Y.R.; Chen, G.; Xu, T.M.; Han, B. Measurement of three-dimensional changes in lip vermilion in adult female patients after orthodontic extraction: A retrospective longitudinal study. Head Face Med. 2021, 17, 9. [Google Scholar] [CrossRef]
- Da Pozzo, F.; Gibelli, D.; Beltramini, G.A.; Dolci, C.; Giannì, A.B.; Sforza, C. The Effect of Orthognathic Surgery on Soft-Tissue Facial Asymmetry: A Longitudinal Three-Dimensional Analysis. J. Craniofac. Surg. 2020, 31, 1578–1582. [Google Scholar] [CrossRef]
- Chen, Y.H.; Baan, F.; Bruggink, R.; Ko, E.W.; Bergé, S.; Xi, T. Clockwise versus counterclockwise rotation in bimaxillary surgery: 3D analysis of facial soft tissue outcomes. Oral. Maxillofac. Surg. 2024, 28, 693–703. [Google Scholar] [CrossRef]
- Keardkhong, P.; Chen, Y.F.; Yao, C.F.; Chen, Y.A.; Liao, Y.F.; Chen, Y.R. Comparison of regional soft tissue changes after bimaxillary rotational surgery between class III deformity with overbite and open bite: A 3D imaging analysis. Biomed. J. 2023, 46, 100562. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.A.; Chang, Y.J.; Lee, S.H.; An, H.J.; Park, K.H. Three-dimensional soft tissue changes according to skeletal changes after mandibular setback surgery by using cone-beam computed tomography and a structured light scanner. Prog. Orthod. 2019, 20, 25. [Google Scholar] [CrossRef] [PubMed]
- Rongo, R.; Nissen, L.; Leroy, C.; Michelotti, A.; Cattaneo, P.M.; Cornelis, M.A. Three-dimensional soft tissue changes in orthodontic extraction and non-extraction patients: A prospective study. Orthod. Craniofac. Res. 2021, 24 (Suppl. S2), 181–192. [Google Scholar] [CrossRef]
- Choi, T.H.; Kim, S.H.; Yun, P.Y.; Kim, Y.K.; Lee, N.K. Soft Tissue Changes After Clockwise Rotation of Maxillo-Mandibular Complex in Class III Patients: Three-Dimensional Stereophotogrammetric Evaluation. J. Craniofac. Surg. 2021, 32, 612–615. [Google Scholar] [CrossRef]
- Yang, G.; Lyu, L.; Wen, A.; Zhao, Y.; Wang, Y.; Li, J.; Yan, H.; Zhang, M.; Yu, Y.; Yu, T.; et al. Comparison of Mirroring and Overlapping Analysis and Three-Dimensional Soft Tissue Spatial Angle Wireframe Template in Evaluating Facial Asymmetry. Bioengineering 2025, 12, 79. [Google Scholar] [CrossRef]
- Mao, B.; Tian, Y.; Xiao, Y.; Li, J.; Zhou, Y.; Wang, X. Classification of skeletal discrepancies by machine learning based on three-dimensional facial scans. Int. J. Oral. Maxillofac. Surg. 2025, 54, 747–756. [Google Scholar] [CrossRef]
- Nguyen, K.T.; Farella, M.; Bennani, V.; Mei, L. Effect of Biomechanical Properties of Perioral Soft Tissues on Lip Response to Simulated Protraction of Upper Front Teeth. J. Oral. Rehabil. 2025, 52, 632–640. [Google Scholar] [CrossRef]
- Berends, B.; Bielevelt, F.; Baan, F.; Schreurs, R.; Maal, T.; Xi, T.; de Jong, G. Soft-tissue prediction based on 3D photographs for virtual surgery planning of orthognathic surgery. Comput. Biol. Med. 2025, 194, 110529. [Google Scholar] [CrossRef]
- Simões, J.C.M.; Garcia, D.M.; De Mello-Filho, F.V.; De Felício, C.M.; Trawitzki, L.V.V. Masticatory function and three-dimensional facial morphology of soft tissues: One year after orthognathic surgery. Arch. Oral. Biol. 2025, 169, 106103. [Google Scholar] [CrossRef]
- Chiang, W.C.; Chen, H.L.; Lin, H.H. Automated 3D facial smile attractiveness assessment before and after orthognathic surgery using transfer learning: A preliminary study. J. Plast. Reconstr. Aesthet. Surg. 2025, 106, 193–202. [Google Scholar] [CrossRef]
- Hu, J.; Wang, C.; Li, Q. Characteristics of skeletal Class II adolescents with favorable facial attractiveness outcomes based on 3D photos after Twin-block treatment. J. Stomatol. Oral. Maxillofac. Surg. 2025, 126, 102310. [Google Scholar] [CrossRef]
- Molla, N.; Oh, H.; Heo, G.; Catunda, R.; Lagravère, M. Comparison of soft tissue facial changes in patients 7–11 years of age with and without maxillary expansion utilizing CBCTs and 3D facial scans: A preliminary study. Int. Orthod. 2025, 23, 100998. [Google Scholar] [CrossRef]
- Nike, E.; Radzins, O.; Vuollo, V.; Slaidina, A.; Abeltins, A. Changes in Facial Soft Tissue Asymmetry in Class II Patients One Year After Orthognathic Surgery. J. Clin. Med. 2025, 14, 2912. [Google Scholar] [CrossRef]
- Pellitteri, F.; Albertini, P.; Brucculeri, L.; Cremonini, F.; Guiducci, D.; Falconi, V.; Lombardo, L. Soft tissue changes during orthopedic therapy: An in vivo 3-dimensional facial scan study. Am. J. Orthod. Dentofac. Orthop. 2025, 167, 154–165. [Google Scholar] [CrossRef]
- Kwon, S.M.; Hwang, J.J.; Jung, Y.H.; Cho, B.H.; Lee, K.J.; Hwang, C.J.; Choi, S.H. Similarity index for intuitive assessment of three-dimensional facial asymmetry. Sci. Rep. 2019, 9, 10959. [Google Scholar] [CrossRef]
| Authors | Year of Publication | Sample Size | Aim | Imaging Tools (IT) and Software(S) Used | Parameters Measured |
|---|---|---|---|---|---|
| Bhaskar, E. and C. H. Kau [14] | 2020 | 301 | Determination of the differences in three-dimensional (3D) facial features in a population from Zimbabwe and the United States. | IT: 3dMDfaceTM system (3dMD; Atlanta, GA, USA) S: Rapidform software 2006, INUS Technology, Seoul, Republic of Korea (RF6) | Average faces of two genders were formed by aligning the facial scans. Linear measurements, color histograms, surface areas, and shapes. |
| Kau, C. H. et al. [15] | 2019 | 371 | Determination of gender dimorphism and facial morphological changes from adolescence to adulthood in African American and Caucasian populations. | IT: 3dMDface system (3dMD; Atlanta, GA, USA)/a laser-scanning system consisting of two high-resolution Minolta Vivid VI900 3D cameras (Konica Minolta, Osaka, Japan) S: Rapidform software 2006, INUS Technology, Seoul, Republic of Korea (RF6) | Images were combined to produce a male and female average face where linear measurements, color histograms, surface areas, and shapes were calculated. |
| Rajbhoj, A. A. et al. [16] | 2022 | 129 | Deriving descriptive statistics of 3D facial shape, lip and cheek muscle pressure in subjects of European descent with normal dental occlusion. | IT: VECTRA H1 imaging system (Canfield Scientific, Fairfield, NJ, USA) S; MeshLab (CNR-ISTI, Pisa, Italy), MeVisLab (MeVis Medical Solutions, Bremen, Germany) | Average faces derived from male and female children, adolescent and adults with orthodontically untreated normal occlusion were generated. |
| Mengoa, M. G. R. et al. [17] | 2024 | 84 | Evaluation and comparison of facial metrics in women aged 20–65 years using a 3D stereophotogrammetry system to establish standardized values for facial metric variations in different age subgroups. | IT: Vectra H1 3D stereophotogrammetry equipment (Canfield Scientific, Inc., Fairfield, CT, USA) S; Vectra Analysis Module Software (VAM elaboration, Canfield Scientific Inc. Fairfield, CT, USA) | Twenty-one landmarks were identified. Linear and angular measurements were obtained to calculate a mean value with standard deviation. |
| Cenzato, N. et al. [18] | 2024 | 269 | Analyzing the three-dimensional morphology of the faces of growing patients with Class I and II occlusions, focusing on children aged between 6 and 9 years old. | IT&S: ELITE system | Sixteen landmarks were identified to calculate angular and linear measurement, and distance ratios. |
| Menéndez López-Mateos, M.L. et al. [19] | 2019 | 100 | Analysis of faces of a sample of healthy European adults from southern Spain with normal occlusion in order to establish reference facial soft tissue anthropometric parameters in this specific geographic-ethnic population, as well as to analyze sexual dimorphism. | IT: Panmeca ProMax 3D ProFace (Planmeca USA, Inc.; Roselle, IL, USA) S: Nemotec Arnetts FAB Software, version 10.0 (Software Nemotec SL, Madrid, Spain) | Thirty landmarks described by FARKAS were identified to measure the height and width of face, nose, occlusal area, orolabial area and chin. Angular measurements and ratio measurements were made based on the identified landmarks. Mean value and standard deviation of each measurement were found. |
| Tanikawa, C. et al. [20] | 2019 | 200 | Quantifying and visualizing the 3D configuration of the soft tissues of the face at rest to facilitate a quantitative and instantaneous understanding of a patient’s static facial characteristics. | IT: 3dMDface system (3dMD; Atlanta, GA, USA) S: HBM software (National Institute of Advanced Industrial Science and Technology, Japan) | A wire mesh fitting was conducted based on the assignment of landmarks to each 3D facial image. Three-dimensional normative faces and the standard deviations for different measurements were found based on the mesh. Developed a system to compare the 3D normative face with patient’s own scan. |
| Author | Year of Publication | Sample Size | Aim | Imaging Tools (IT) and Software (S) Used | Method |
|---|---|---|---|---|---|
| Fan, Y. et al. [21] | 2022 | 86 | Facial asymmetry assessment in skeletal Class III patients with spatially dense geometric morphometrics. | IT: 3dMD imaging system (3dMD Inc., Atlanta, GA, USA) S: Meshmonk toolbox | The pointwise surface-to-surface distance between original and mirror face was measured and visualized for the whole face after robust Procrustes superimposition. The degree of overall asymmetry in an individual was scored using a root-mean-squared-error. |
| Gkantidis, N. et al. [22] | 2023 | 20 | Facial asymmetry and midsagittal plane definition in 3D: A bias-free, automated method. | IT: 3dMD stereophotogrammetric camera (3dMDface system, 3dMD Inc., Atlanta, GA, USA) S: Viewbox 4 software (Version 4.1.0.1 BETA 64, dHAL Software, Kifissia, Greece) | midsagittal plane of the face was automatically defined at the midpoints of the contralateral corresponding vertices of the superimposed models and color coded distance maps were constructed. |
| Lyu, L. et al. [23] | 2024 | / | Design an objective method for identifying asymmetry issues. | IT: Bellus 3D Arc 1 system (Bellus3D, Inc., Campbell, CA, USA) | Used 3D facial images and landmark-based anthropometric analysis to construct an average model to create 3D facial mask to evaluate asymmetry. |
| Zhu, Y. J. et al. [24] | 2022 | 30 | Investigating and evaluating a novel mathematical algorithm based on power function weighted Procrustes analysis to determine 3D facial SRPs for patients with mandibular deviation. | IT: Face Scan 3D sensor system (3D-Shape Corp., Erlangen, Germany) S: Geomagic Studio 2013 (3D Systems Inc., Rock Hill, SC, USA) | Statistics and measurement analyses were used to comprehensively evaluate the clinical suitability of the power function weighted Procrustes analysis to construct the 3D symmetry reference plane. |
| Yang, G. et al. [57] | 2025 | 24 | Evaluating the accuracy and efficacy of a new wireframe template methodology in analyzing three-dimensional facial soft tissue asymmetry. | IT: Bellus 3D Arc 1 system (Bellus3D, Inc., Campbell, CA, USA) S: Geomagic Studio 2015 (Geomagic, Inc., Morrisville, NC, USA)/MeshLab (MeshLab 2020.12, 3D)/Procrustes Analysis (PA) algorithm software MATLAB R2019b (The MathWorks, Inc., Natick, MA, USA), Open-Source Nonrigid (OSN) software MATLAB R2019b, MATLAB R2019b, Open-Source Rigid Software (OSS) MATLAB R2019b, and OSN alignment program MeshMonk | Wireframe template was established by identifying 34 facial landmarks and then forming a template on the face, and the angle asymmetry index was automatically scored using the template. |
| Dindaroğlu, F. et al. [25] | 2023 | 20 | Evaluating social smile asymmetry in patients with unilateral impacted maxillary canine on 3D stereophotogrammetric images. | IT: Fuel3D® Scanify® S: Geomagic Essentials 2 reverse engineering software | Tissues around the smile area were divided into cheek, upper lip lateral and medial, and lower lip lateral and medial. Deviation margins and the total percentages of meshes deviations were calculated. |
| Li, H. et al. [26] | 2019 | 50 | Exploring the internal relationship between posed smile characteristics, lip position, and skeletal patterns in young women. | IT: 3dMDface system (3dMD; Atlanta, GA, USA) S: Geomagic Control software (3D Systems, Research Triangle Park, NC, USA) | Each subject was scanned with a posed smile. Interlabial gap, intercommissural width, and smile index were calculated. The changes in the lip landmarks in the vertical, sagittal, and coronal directions were investigated. |
| Cho, S. W. et al. [27] | 2021 | 50 | Evaluating and comparing the sagittal relationship between the maxillary central incisors and the forehead before and after orthodontic treatment. | IT: RAYface® (Raymedical, Seongnam, Republic of Korea) S: Asahi Alphard 3030® (Asahi Roentgen Ind., Co., Ltd., Kyoto, Japan). | Superimposition of the CBCT and 3D facial scan was carried out on the identical program to create a digital twin for facial analysis. Trichion/superion, glabella, maxillary incisor are located. |
| Wang, T. et al. [28] | 2024 | 52 | Clarifying the hard-soft tissue relationships of the lower 1/3 of the face in skeletal Class II-hyperdivergent patients compared with those in Class I-normodivergent patients using network analysis. | IT: 3dMD imaging system (3dMD, Atlanta, GA, USA), NewTom Scanner (NewTom AG, Marburg, Germany) S: Geomagic Studio 11.0 software (Raindrop Geomagic, Inc., NC, USA) | Cone-beam computed tomography and three-dimensional facial scans were taken and superimposed, on which landmarks were identified manually, and their coordinate values were used for network analysis. |
| B. Mao et al. [58] | 2025 | 435 | Using machine learning (ML) to classify sagittal and vertical skeletal discrepancies in 3D facial scans, as well as to evaluate shape variability. | IT: 3D optical FaceSCAN3D system (3D-Shape, Erlangen, Germany) S: MATLAB (MATLAB R2018b; The MathWorks Inc., Natick, MA, USA), using the MeshMonk toolbox | Sixty-three facial landmarks were determined and geometric measurements formed by these points along with demographic characteristics were used in the machine learning models for sagittal and vertical classification. |
| Coppola, G. et al. [29] | 2024 | / | Compare various recording speeds for three standardized movements using the 3dMDface camera system, to assess its accuracy and reliability. | IT: 3dMD imaging system (3dMD, Atlanta, GA, USA), UR5e Universals Robots, Universal Robots GmbH, München, Germany S: Viewbox 4 Software (version 4.1.0.1 BETA 64, dHAL software, Kifisia, Greece) | A linear and two circular movements were performed using a 3D-printed cube mounted on a robotic arm, accuracy and reliability were evaluated. |
| Author | Year of Publication | Sample Size | Aim | Imagining Tools (IT) and Software(S) Used | Method |
|---|---|---|---|---|---|
| Fiorillo, G. et al. [30] | 2024 | / | Describing the fully digital workflow for the production design and manufacturing of a fully digital protraction facemask. | / | Shell mask is virtually drawn and finished to guarantee 22 support zones on the forehead, cheekbones, and chin. The mask is prototyped by stereolithography using biocompatible resins. |
| Akan, B. and İ. Veli [31] | 2020 | 20 | Evaluating the effects of the Forsus fatigue-resistant device EZ2 appliance (3M Unitek, Monrovia, Calif) on facial soft tissues. | IT: 3dMD Face (3dMD Ltd., Atlanta, GA, USA) S: 3dMD Vultus software (3dMD, Atlanta, GA, USA)/SAS 9.3 Software (SAS Institute, Cary, NC, USA) | Three-dimensional facial scanning images were obtained with 3dMD Face. Cephalometric radiographic images were taken before placement of the appliance (T0), immediately after removal (T1), and at the 6-month (T2) follow-up after the removal of the appliance. |
| Yüksel Coşkun, E. and E. Esenlik [32] | 2020 | 32 | Comparing adolescent and post-adolescent growth periods regarding the effectiveness of conventional activator appliance in patients. | IT: 3dMDface system (3dMDface LLC, Atlanta, GA, USA) S: 3dMDface Vultus® software (3dMDface Vultus® software version 2.3.0.2, 3dMDface, Atlanta, GA, USA) | Projections of the lips and the chin and volumetric measurements of the lip and the mandibular area were assessed using three-dimensional photogrammetry. |
| Hou, S. Y. et al. [33] | 2021 | 43 | Investigating changes in facial morphology during the first six months of orthodontic treatment among adult females receiving orthodontic treatment. | IT: Morpheus 3D, Republic of Korea S: IDAV Landmark Editor v.3.0.0.6 /MeshMonk toolbox of MATLAB (R2018b) | Spatially dense facial landmarks were digitized. An anthropometric mask was mapped to each facial image resulting in 3D facial quasi-landmarks. Three-dimensional geometric morphometrics and multivariate statistics were used to investigate changes. |
| Jindanil, T. et al. [34] | 2024 | 20 | Constructing a virtual patient (VP) using facial scan, intraoral scan, and low-dose computed tomography scab based on an Artificial intelligence. | IT: iReal 2E structured light-based scanner (Scantech, Hangzhou, China)/Emerald S device (Planmeca, Helsinki, Finland)/SOMATOM Force unit (SIEMENS, Munich, Germany) S: Virtual Patient Creator (version 1.0.0 March 2022, Relu BV, Leuven, Belgium) | The accuracy of the virtual patients created using AI-driven, AI-refined and semiautomated registration was analyzed. User satisfaction was assessed through a survey on the virtual patient’s realism and usefulness for treatment planning and communication. |
| Ponnusamy, A. et al. [35] | 2020 | 375 | Establishment of the most pleasing computer-generated 3D facial form using a community-based sample population. | IT: 3dMD camera (3dMD Inc., GA, USA) | Seven average faces for each gender were generated, arranged from most concave to most convex profile and rated by dentists, oral surgeons, plastic surgeons, orthodontists and laypeople for attractiveness to find out most pleasant face. |
| Dong, T. et al. [36] | 2020 | 221 | Assessing the influence of chin asymmetry on perceived facial aesthetics, investigating the cognitive boundaries of chin asymmetry among orthodontists, general dentists, and laypersons, and providing quantitative reference for clinical treatment. | IT: 3dMDface system (3dMD, Atlanta, GA, USA) S: Geomagic Wrap 2015 (3D Systems) | Soft tissue pogonion point of the facial image were altered in 2 mm increments from 0 to 12 mm to produce 14 images and were rated by 66 orthodontists, 89 general dentists, and 66 laypersons to determine whether treatment was needed. |
| Fastuca, R. et al. [37] | 2022 | 105 | Investigating the influence of different facial components on the perception of facial attractiveness of patients in orthodontists, laypersons and patients with 2D and 3D. | S: FaceGen software (Singular Inversions Inc., Toronto, ON, Canada)/Dolphin Imaging & Management Solutions, Chatsworth, CA, USA | Four facial components were modified (face length, lip volume, nose size and cheekbone contour) and the resulting simulations were used to obtain 2D figures and 3D videos, which were evaluated in a survey by orthodontists, patients, and laypersons. |
| Feng, J. et al. [38] | 2019 | 30 | Investigating the influence of cheek volume on facial esthetics judged by orthodontists and non-specialists. | IT: 3dMDface system (3dMD, Atlanta, GA, USA) | A 25-year-old female’s natural and smiling face was captured by 3D stereophotogrammetry. Cheek volume of the 3D image was altered to different degrees three-dimensionally. |
| Nguyen, K. T. et al. [59] | 2025 | 34 | Investigating the upper lip changes induced by a simulated protraction of upper front teeth. | IT: 3dMDtrio, 3dMDLLC, Atlanta, GA, USA S: 3dMDpa-tient; 3dMD/Meshlab (Meshlab v1.3.4,ISTI—CNR, Pisa, Italy) | Simulated protraction of upper front teeth was achieved and stereophotogrammetry was used to assess lip changes in three dimensions. |
| Berends, B. et al. [60] | 2025 | 458 | Developing and validating a deep learning-based method to predict postoperative facial soft tissue outcomes in real time for various orthognathic procedures. | IT: 3 dMD’s 5-pod 3dMDhead systems (3dMDCranial, 3 dMD, Atlanta, GA, USA) International Inc, Hatfield, PA, USA) S: MeshMonk algorithm and DiffusionNets, 3DMedX® software (version: 1.2.40.0, 3D Lab Radboudumc, Nijmegen, The Netherlands) | A deep learning-based method was developed based on 3D photographs for the real-time prediction of the effects of maxilla, mandible, and chin displacements on facial soft tissue following orthognathic surgery. |
| Author | Year of Publications | Sample Size | Aim of Study | Imaging Tools (IT) and Software(S) Used | Method of Evaluation |
|---|---|---|---|---|---|
| Akan, B. and İ. Veli [31] | 2020 | 20 | Evaluating the effects of the Forsus fatigue-resistant device EZ2 appliance (3M Unitek, Monrovia, Calif) on facial soft tissues. | IT: 3dMD Face (3dMD Ltd., Atlanta, GA, USA) S: 3dMD Vultus software (3dMD, Atlanta, GA, USA)/SAS 9.3 Software (SAS Institute, Cary, NC, USA) | Three-dimensional facial scanning images were obtained with 3dMD Face. Cephalometric radiographic images were taken before placement of the appliance (T0), immediately after removal (T1), and at the 6-month (T2) follow-up after the removal of the appliance. |
| Yüksel Coşkun, E. and E. Esenlik [32] | 2020 | 32 | Comparing adolescent and post-adolescent growth periods regarding the effectiveness of conventional activator appliance in patients. | IT: 3dMDface system (3dMDface LLC, Atlanta, GA, USA) S: 3dMDface Vultus® software (3dMDface Vultus® software version 2.3.0.2, 3dMDface, Atlanta, GA, USA) | Projections of the lips and the chin and volumetric measurements of the lip and the mandibular area were assessed using three-dimensional photogrammetry. |
| Güler, Ö. and S. Malkoç [41] | 2020 | 60 | Evaluating the effects of three different fixed or removable functional appliances on the soft tissue changes in patients with Class II Division 1 malocclusion using 3-dimensional images. | IT&S: 3dMD Face system (3dMd, Atlanta, GA, USA) | Lower facial width, volumetric change in mandible, total facial height, convexity angle, and facial depth. |
| Akan, B. et al. [42] | 2021 | 32 | Evaluating the effects of tooth-borne and tooth-bone-borne rapid maxillary expansion on soft tissue with stereophotogrammetry. | IT: 3dMD Face imaging system (3dMD, Atlanta, GA, USA) S: 3dMDvultus analysis program (3dMD, Atlanta, GA, USA) | Changes in soft tissues before RME (T0) and post-retention (T1) period were evaluated by stereophotogrammetry. Linear and angular measurements were performed. |
| Liu, Z. Y. et al. [43] | 2019 | 47 | Investigating the three-dimensional lip vermilion changes after extraction and non-extraction orthodontic treatment in female adult patients and explore the correlation between lip vermilion changes and incisor changes. | IT: 3D CaMega; Boweihengxin Technology Inc., Beijing, China S: Rapidform 2009 software (Inus Technology) | Nine angles, seven distances, and the surface area of the lip vermilion were measured by using pre- and post-treatment three-dimensional facial scans. Linear and angular measurements of incisors were performed on lateral cephalograms. |
| Marino Merlo, M. et al. [44] | 2024 | 28 | Comparing the effects on facial soft tissues produced by maxillary expansion generated by rapid maxillary expansion versus slow maxillary expansion. | IT: Face Shape Maxi 3D Scanner (Polishape 3D srl, Bari, Italy) S: 3D Slicer (open-source) | Difference in the facial tissue changes in the nasal area measured on facial 3D images captured immediately before application of the expander (T0) and after one year of retention, immediately after the expander removal (T1). (Nasal columella width, mouth width, nasal tip angle, upper lip angle, and lower lip angle). |
| Sitaropoulou, V. et al. [45] | 2020 | 36 | Evaluating the skeletal, dental, and soft tissue effects of the alternating rapid maxillary expansions and constrictions (Alt-RAMEC) protocol combined with a facemask in prepubertal patients. | IT: 3dMDface system (3dMD LLC, Atlanta, GA, USA) S: MIMICs version 17.0 (Materialize Interactive Medical Image Control Systems, Leuven, Belgium) | Soft tissue landmarks identified and compared on T0 and T1 3D scans. |
| Nike, E. et al. [46] | 2023 | 101 | Evaluation of facial soft tissue asymmetric changes in Class III patients after orthognathic surgery using three-dimensional stereophotogrammetry. | IT: 3dMDtrio stereophotogrammetry system (3dMD LLC, Atlanta, GA, USA) S: 3dMDvultus version 2.5.0.1 (3dMD LLC/3dMD Patient version 4.1 (3dMD LLC) | Three-dimensional photographs were acquired using the 3dMDtrio stereophotogrammetry system, and 21 anthropometric landmark positions were evaluated at three time points: before surgery (T0), 6 months (T1) and 12 months (T2) after surgery. |
| Shi, Y. et al. [47] | 2022 | 30 | Evaluating facial soft and hard tissue changes, individually and relative to each other, in patients with skeletal class III deformity after bimaxillary surgery using 3D photos obtained by white light scanning. | IT: Artec Eva hand-held 3D scanner S: CMF PROPLAN 3.0 (Materialise)/Artec studio 12.0 software | Three-dimensional color-coded map was analyzed to assess both skeletal and soft tissue changes between T0 and T1. Changes in the 3D coordinates of each anatomical landmark were analyzed using Student’s t-test. |
| Molla, N. et al. [64] | 2025 | 32 | Evaluate the effects of maxillary expansion over a period of 12 months on facial soft tissue measurements in children aged 7–11 years. | IT: Facial Insight 3D Scanner (Motion View LLC, Chattanooga, TN, USA) S: 3D Slicer software (version 4.11.20210226, Boston, MA, USA)/OrthoInsight 3D software (Version 7.7.5570; Motion View LLC, Chattanooga, TN, USA) | Soft tissue analysis after rapid maxillary expansion using landmarks and linear and angular measurements on 3D photographs. |
| Nike, E. et al. [65] | 2025 | 54 | Examine changes in facial soft tissue asymmetry over time in patients after Class II orthognathic surgery using 3D stereophotogrammetry. | IT: 3dMD Trio stereophotogrammetry system (3dMD LLC, Atlanta, GA, USA) S: 3dMD Vultus version 2.5.0.1 (3dMD LLC)/edited using 3dMD Patient version 4.1 software (3dMD LLC) | Evaluation of 21 anthropometric landmark positions was conducted before surgery (T0), 6 months (T1), and 12 months (T2) after surgery. |
| Pellitteri, F. et al. [66] | 2025 | 45 | Comparing the soft tissue changes in pretreatment and posttreatment facial scans of patients who had undergone various orthopedic treatments vs. a control group of untreated growing patients. | IT: EinScan H face scanner (70565; Shining 3D Technology GmbH, Stuttgart, Germany) S: Geometric Control X software (3D Systems, Rock Hill, SC) | After best-fit scan alignment, a 3-dimensional analysis of soft tissue changes was performed, comparing 3D reference points and 8 areas on T0 and T1 scans. |
| Mao, B. et al. [48] | 2023 | 19 | Investigating temporomandibular joint stability and 3D facial changes in class II hyperdivergent patients with stable idiopathic condylar resorption after orthodontic camouflage treatment. | IT: 3D optical FaceSCAN3D system (3D-Shape) S: MATLAB (MATLAB R2018b, MathWorks) with the MeshMonk toolbox | 3D facial heatmaps were used to illustrate facial changes, and the 3D deviations of landmarks were calculated. |
| Alkhayer, A. et al. [49] | 2021 | 25 | Assessing soft tissue changes in the face after six months of retention following Rapid Maxillary Expansion. | IT: structured-light 3D handheld scanner (Artec EvaTM; Artec Group, Luxembourg) S: Artec Eva V.12/GOM Inspect Evaluation Software, Capture 3D, Inc., Santa Ana, CA, USA | Linear and angular measurements were performed, and 3D deviation analyses were performed for six morphological regions of the face. |
| Shen, L. H. et al. [50] | 2021 | 42 | Evaluating 3D morphological changes after orthodontic extraction treatment in lip vermilion of adult females with dentoalveolar protrusion using a structured light-based scanner. | IT: 3D CaMega; Boweihengxin Technology Inc., Beijing, China S: Geomagic Qualify 12 (3D Systems, Rock Hill, SC, USA) | Six landmarks, three linear measurements and three area measurements were measured. The spatial deviations of three volumetric measurements (upper, lower, and total vermilion) were constructed for quantitative analysis. |
| Cho, S. W. et al. [27] | 2021 | 50 | Evaluating and comparing the sagittal relationship between the maxillary central incisors and the forehead before and after orthodontic treatment. | IT: RAYface® (Raymedical, Seongnam, Republic of Korea) S: Asahi Alphard 3030® (Asahi Roentgen Ind., Co., Ltd., Kyoto, Japan). | Superimposition of the CBCT and 3D facial scan was carried out on the identical program to create a digital twin for facial analysis. Trichion/superion, glabella, maxillary incisor were located. |
| Da Pozzo, F. et al. [51] | 2020 | 41 | Compare the severity of facial asymmetry of class III malocclusion patient with Class I occlusion patient, and pre-op vs. post-op. | IT: VECTRA system S: Mirror software (Canfield Scientific) | Images of the hemi-faces of the subjects were divided into thirds (upper, middle, lower), mirrored and superimposed to their contralateral ones. |
| Chen, Y. H. et al. [52] | 2024 | 37 | Comparing facial 3D soft tissue changes in subjects with Class III deformities who underwent bimaxillary clockwise and counterclockwise rotational orthognathic surgery. | IT: 3dMD facial, Atlantic, USA S: 3DMedX® | Preoperative and 9-month follow-up CBCT and 3D stereophotogrammetry were obtained, superimposed, and quantified for skeletal movements and soft tissue changes in six facial regions. |
| Keardkhong, P. et al. [53] | 2023 | 60 | Comparing regional soft tissue changes between patients with class III overbite and open bite deformities treated with bimaxillary surgery involving clockwise and counterclockwise mandibular setback. | IT: 3dMDface System (3dMD Inc., Atlanta, GA, USA) | Combined cone-beam CT scans and 3D facial photographs preoperative and at least 1-year postoperative were taken to assess the soft tissue change (superimposed 3D images for direct comparison). |
| Kim, K. A. et al. [54] | 2019 | 28 | Three-dimensional soft tissue changes according to skeletal changes after mandibular setback surgery by using cone-beam computed tomography and a structured light scanner. | IT: Morpheus 3D Neo; Morpheus, Gyoung-gi, Republic of Korea S: Morpheus 3D software | To use an identical 3D coordinate system, superimposition was performed, and nine skeletal and 18 soft tissue landmarks were identified. Changes in the landmarks and correlation coefficients and ratios between hard and soft tissue changes were evaluated. |
| Rongo, R. et al. [55] | 2021 | 46 | Assessing the soft tissue changes in orthodontic extraction and non-extraction patients on 3D stereophotogrammetric images. | IT: white-light scanner 3dMD (3dMD) S: 3dMDVultusSoftware | After placing 19 landmarks, 15 measurements were obtained Superimposition of 3D images visualized with color-coded maps to show changes. |
| Choi, T. H. et al. [56] | 2021 | 18 | Evaluating the linear, angular, and volumetric changes in soft tissue after clockwise repositioning of the maxillo-mandibular complex in skeletal class III patients using 3D stereophotogrammetry and to determine the correlation between changes in the skeletal and soft tissue variables. | IT: Morpheus 3D; Morpheus Co, Gyeonggi, Republic of Korea S: Facemaker software (Facemaker; Morpheus Co) | Lateral cephalograms and 3D photographs taken before and 6 months after surgery were compared. |
| Simões, J. C. M. et al. [61] | 2025 | 46 | Analyzing changes in masticatory function and 3D facial soft tissue in patients with Class II and Class III DFD after orthognathic surgery. | IT: FastSCAN™ Scorpion laser scanning system (Polhemus, Inc., Colchester, CT, USA) S: FastSCAN™/Geomagic Studio (Geomagic, Research Triangle Park, NC, USA) | Twelve patients who completed the treatment protocol were evaluated 12 months post-surgery (T2). The patient groups were compared with each other and with a control group (CG) of 25 healthy subjects. |
| Denadai, R. et al. [39] | 2020 | 70 | Evaluating the impacts of orthognathic surgery on the patient’s facial appearance and apparent age, from surgeon and laymen perspective. | IT: 3dMDface system (3dMD; Atlanta, GA, USA) | Seven blinded plastic surgeons rated all photographs for apparent facial aesthetic and age scales. The FACE-Q data from 57 matched normal individuals were adopted for comparative analyses. |
| Denadai, R. et al. [40] | 2019 | 84 | Evaluating orthognathic surgery outcomes using pre- and post-OGS patients’ FACE-Q reports, and a three-dimensional facial photograph-based panel assessment of facial appearance. | IT: 3dMDface system (3dMD; Atlanta, GA, USA) | Ninety-six blinded layperson and orthodontic and surgical professional raters and verified whether there were correlations between these outcome measurement tools. |
| Chiang, W.C. et al. [62] | 2025 | 135 | Assessing facial smile attractiveness before and after orthognathic surgery using a transfer learning model. | IT: 3dMDhand™ System Product Specifications (3dMD Inc, Atlanta, GA, USA) S: 3dMD Vultus (3dMD LLC)/3-matic (CAD Software, Materialise, Belgium)/MATLABsoftware (MathWorks, Natick, MA, USA) | A total of 38 evaluators, comprising plastic surgeons, orthodontists, and research assistants, were instructed to rate the facial smile attractiveness of 3D facial images using a 5-point Likert scale. |
| Hu, I. et al. [63] | 2025 | 86 | Investigating the hard tissue and soft tissue characteristics related to favorable facial attractiveness outcomes of Class II Twin-block treatment to select suitable patients for this therapy. | IT: 3dMD face, Atlanta, GA, USA S: 3dMD vultus program | Post-Twin-block treatment facial attractiveness was assessed by seven orthodontists using visual analog scale scores based on 3D photographs. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hung, P.K.; Liu, J.; Shan, Z. 3D Photogrammetry-Driven Craniofacial Analysis in Orthodontics: A Scoping Review of Recent Applications. Bioengineering 2025, 12, 1263. https://doi.org/10.3390/bioengineering12111263
Hung PK, Liu J, Shan Z. 3D Photogrammetry-Driven Craniofacial Analysis in Orthodontics: A Scoping Review of Recent Applications. Bioengineering. 2025; 12(11):1263. https://doi.org/10.3390/bioengineering12111263
Chicago/Turabian StyleHung, Pui Ki, Junqi Liu, and Zhiyi Shan. 2025. "3D Photogrammetry-Driven Craniofacial Analysis in Orthodontics: A Scoping Review of Recent Applications" Bioengineering 12, no. 11: 1263. https://doi.org/10.3390/bioengineering12111263
APA StyleHung, P. K., Liu, J., & Shan, Z. (2025). 3D Photogrammetry-Driven Craniofacial Analysis in Orthodontics: A Scoping Review of Recent Applications. Bioengineering, 12(11), 1263. https://doi.org/10.3390/bioengineering12111263






