Effects of the Combined Abdominal Draw-In Maneuver and Manual Resistance on Lumbopelvic Muscle Activity and Anterior Pelvic Tilt During Prone Hip Extension
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Surface Electromyography (EMG) Recording and Data Processing
2.3. Measurement of Anterior Pelvic Tilt Angle
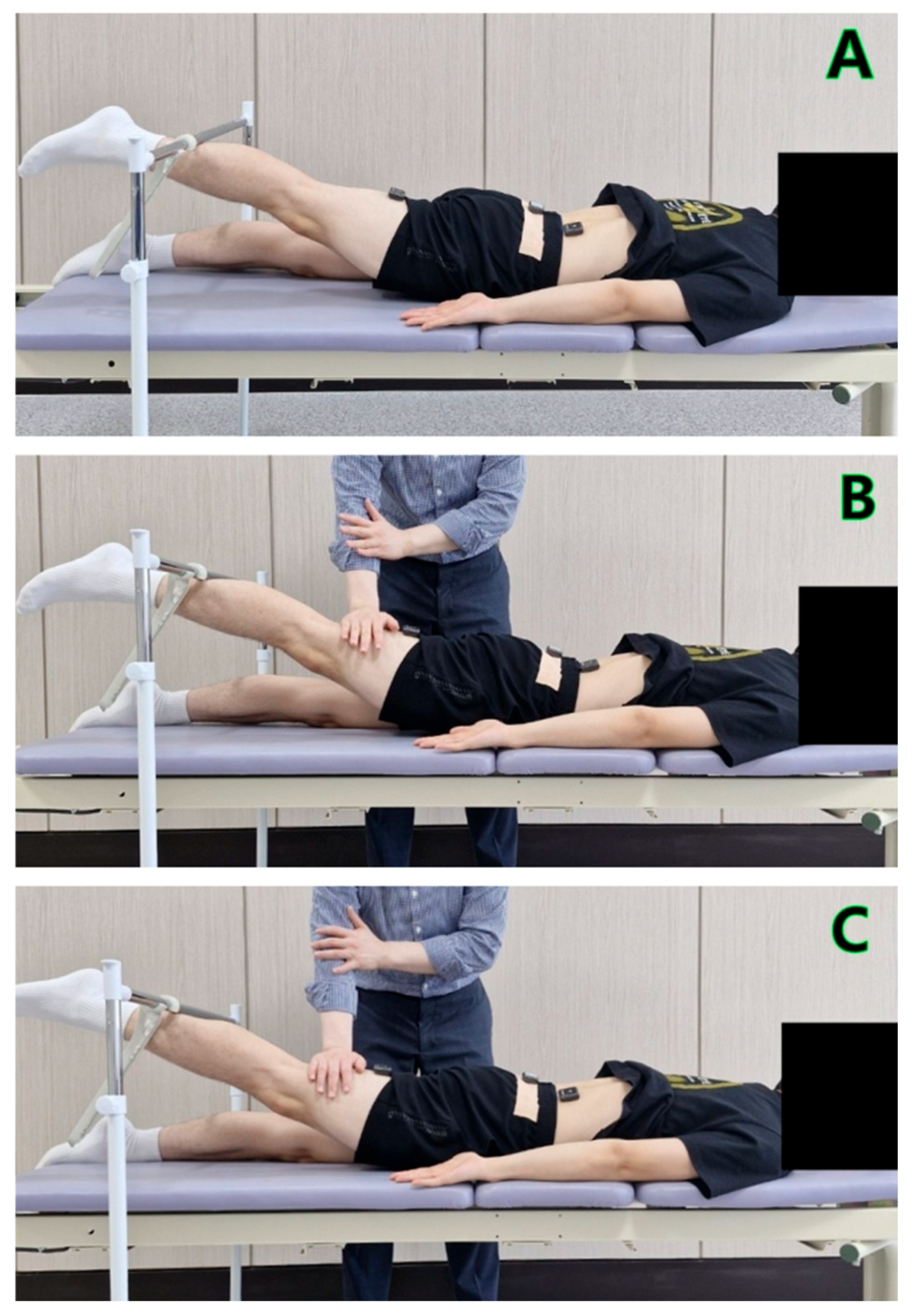
2.4. Experimental Procedures
2.5. Statistical Analyses
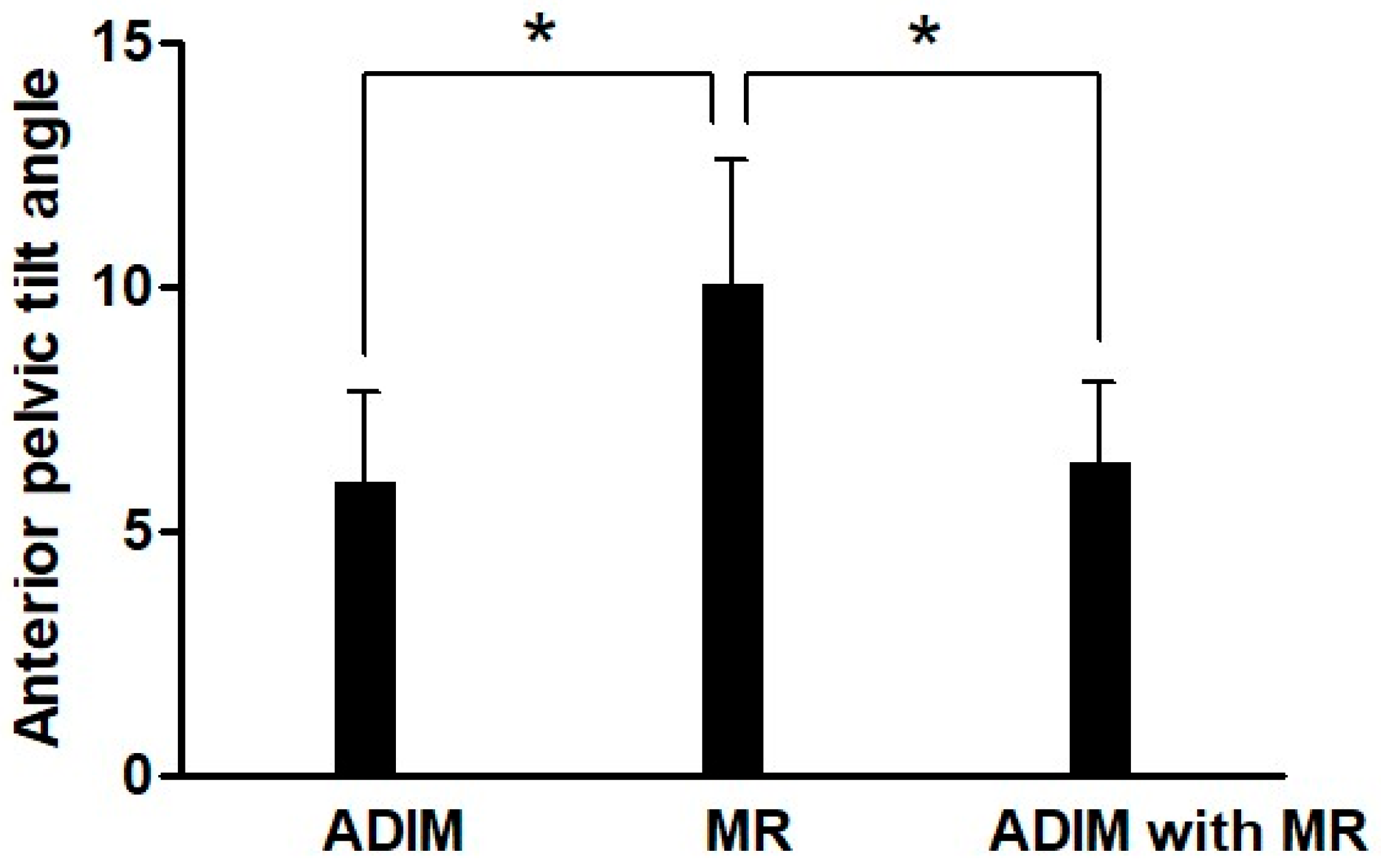
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| PHE | Prone Hip Extension |
| GM | Gluteus Maximus |
| ES | Erector Spinae |
| IO | Internal Oblique |
| TrA | Tranversus Abdominis |
| ADIM | Abdominal Draw-In Maneuver |
| MR | Manual Resistance |
References
- Park, K.Y.; Jeon, I.C.; Hwang, U.J.; Jung, S.H.; Ha, S.M.; Yim, S.Y. Effects of abdominal drawing-in maneuver with or without prior iliopsoas stretching on gluteus maximus activity during prone hip extension. J. Back Musculoskelet. Rehabil. 2022, 35, 331–339. [Google Scholar] [CrossRef]
- Tateuchi, H.; Taniguchi, M.; Mori, N.; Ichihashi, N. Balance of hip and trunk muscle activity is associated with increased anterior pelvic tilt during prone hip extension. J. Electromyogr. Kinesiol. 2012, 22, 391–397. [Google Scholar] [CrossRef]
- Ryan, N.; Bruno, P. The clinical utility of the prone hip extension test in the diagnosis of motor control impairments associated with low back pain: A cross-sectional study using motion capture and electromyography. Clin. Biomech. 2024, 118, 106317. [Google Scholar] [CrossRef]
- Oh, J.S.; Cynn, H.S.; Won, J.H.; Kwon, O.Y.; Yi, C.H. Effects of performing an abdominal drawing-in maneuver during prone hip extension exercises on hip and back extensor muscle activity and amount of anterior pelvic tilt. J. Orthop. Sports Phys. Ther. 2007, 37, 320–324. [Google Scholar] [CrossRef]
- Ludwig, O.; Dindorf, C. Muscular Strategies for Correcting the Pelvic Position to Improve Posture-An Exploratory Study. J. Funct. Morphol. Kinesiol. 2024, 9, 25. [Google Scholar] [CrossRef]
- Davis, D.L.; Roberts, A.; Calderon, R.; Kim, S.; Ryan, A.S.; Sanses, T.V.D. Gluteal muscle fatty infiltration, fall risk, and mobility limitation in older women with urinary incontinence: A pilot study. Skelet. Radiol. 2023, 52, 47–55. [Google Scholar] [CrossRef] [PubMed]
- Kim, T.; Woo, Y.; Kim, Y. Effect of abdominal drawing-in maneuver during hip extension on the muscle onset time of gluteus maximus, hamstring, and lumbar erector spinae in subjects with hyperlordotic lumbar angle. J. Physiol. Anthropol. 2014, 33, 34. [Google Scholar] [CrossRef] [PubMed]
- McConnell, J. Recalcitrant chronic low back and leg pain—A new theory and different approach to management. Man. Ther. 2002, 7, 183–192. [Google Scholar] [CrossRef]
- Jeon, I.C.; Kwon, O.Y.; Weon, J.H.; Hwang, U.J.; Jung, S.H. Comparison of Hip- and Back-Muscle Activity and Pelvic Compensation in Healthy Subjects During 3 Different Prone Table Hip-Extension Exercises. J. Sport. Rehabil. 2017, 26, 216–222. [Google Scholar] [CrossRef] [PubMed]
- Miyachi, R.; Sano, A.; Tanaka, N.; Tamai, M.; Miyazaki, J. Relationship between lumbar spine motor control ability and perceptual awareness during prone hip extension movement in people with low back pain. J. Med. Investig. 2022, 69, 38–44. [Google Scholar] [CrossRef]
- Grenier, S.G.; McGill, S.M. Quantification of lumbar stability by using 2 different abdominal activation strategies. Arch. Phys. Med. Rehabil. 2007, 88, 54–62. [Google Scholar] [CrossRef]
- Kim, D.W.; Kim, T.H. Effects of abdominal hollowing and abdominal bracing during side-lying hip abduction on the lateral rotation and muscle activity of the pelvis. J. Exerc. Rehabil. 2018, 14, 226–230. [Google Scholar] [CrossRef]
- García-Vaquero, M.P.; Moreside, J.M.; Brontons-Gil, E.; Peco-González, N.; Vera-Garcia, F.J. Trunk muscle activation during stabilization exercises with single and double leg support. J. Electromyogr. Kinesiol. 2012, 22, 398–406. [Google Scholar] [CrossRef]
- Puntumetakul, R.; Saiklang, P.; Tapanya, W.; Chatprem, T. The Effects of Core Stabilization Exercise with the Abdominal Drawing-in Maneuver Technique versus General Strengthening Exercise on Lumbar Segmental Motion in Patients with Clinical Lumbar Instability: A Randomized Controlled Trial with 12-Month Follow-Up. Int. J. Environ. Res. Public Health 2021, 18, 7811. [Google Scholar] [CrossRef]
- Mitchell, U.H.; Owen, P.J.; Rantalainen, T.; Belavý, D.L. Increased Joint Mobility Is Associated With Impaired Transversus Abdominis Contraction. J. Strength Cond. Res. 2022, 36, 2472–2478. [Google Scholar] [CrossRef]
- Chaitow, L. Muscle Energy Techniques, 2nd ed.; Churchill Livingstone: London, UK, 2001. [Google Scholar]
- Sahrmann. Diagnosis Treatment Movement Impairment Syndrome; Mosby Inc.: New York, NY, USA, 2002. [Google Scholar]
- Sharma, R.; Singh, G.; Kothiyal, S.; Verma, S. Enhancing core stability and strength through abdominal drawing-in maneuver training using a sphygmomanometer: A narrative review. J. Bodyw. Mov. Ther. 2025, 43, 228–236. [Google Scholar] [CrossRef]
- de Oliveira, F.C.L.; Larivière, C.; Dallaire, M.; Mecheri, H.; Ngomo, S.; da Silva, R.A. Immediate Effect of Lumbosacral Orthosis and Abdominal Drawing-In Maneuver on Postural Control in Adults With Nonspecific Chronic Low Back Pain. J. Manip. Physiol. Ther. 2022, 45, 425–435. [Google Scholar] [CrossRef]
- Kisner, C.; Colby, L.A. Therapeutic Exercise: Foundations and Techniques, 6th ed.; F.A. Davis Co.: Philadelphia, PA, USA, 2012. [Google Scholar]
- McPherson, S.L.; Watson, T. Training of transversus abdominis activation in the supine position with ultrasound biofeedback translated to increased transversus abdominis activation during upright loaded functional tasks. PM&R 2014, 6, 612–623. [Google Scholar] [CrossRef]
- Kendall, F.; McCreary, E.; Provance, P. Muscles: Testing and Function with Posture and Pain; Lippincott Williams & Wilkin: Baltimore, MD, USA, 2005. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Lawrence Erlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Suehiro, T.; Mizutani, M.; Ishida, H.; Kobara, K.; Osaka, H.; Watanabe, S. Individuals with chronic low back pain demonstrate delayed onset of the back muscle activity during prone hip extension. J. Electromyogr. Kinesiol. 2015, 25, 675–680. [Google Scholar] [CrossRef] [PubMed]
- Park, H.S.; Park, S.W.; Oh, J.K. Effect of adding abdominal bracing to spinal stabilization exercise on lumbar lordosis angle, extensor strength, pain, and function in patients with non-specific chronic low back pain: A prospective randomized pilot study. Medicine 2023, 102, e35476. [Google Scholar] [CrossRef] [PubMed]
- Folland, J.P.; Williams, A.G. The adaptations to strength training: Morphological and neurological contributions to increased strength. Sports Med. 2007, 37, 145–168. [Google Scholar] [CrossRef]
- Rong, W.; Soh, K.G.; Samsudin, S.; Zhao, Y.; Wang, X.; Zhang, X.; Cao, L. Effect of resistance training on kinetic and kinematic indicators in jump athletes: A systematic review. BMC Sports Sci. Med. Rehabil. 2025, 17, 210. [Google Scholar] [CrossRef]
- Elgueta-Cancino, E.; Evans, E.; Martinez-Valdes, E.; Falla, D. The Effect of Resistance Training on Motor Unit Firing Properties: A Systematic Review and Meta-Analysis. Front. Physiol. 2022, 13, 817631. [Google Scholar] [CrossRef] [PubMed]
- Van Hooren, B.; Aagaard, P.; Blazevich, A.J. Optimizing Resistance Training for Sprint and Endurance Athletes: Balancing Positive and Negative Adaptations. Sports Med. 2024, 54, 3019–3050. [Google Scholar] [CrossRef] [PubMed]
- Campbell, A.; Kemp-Smith, K.; O’Sullivan, P.; Straker, L. Abdominal Bracing Increases Ground Reaction Forces and Reduces Knee and Hip Flexion During Landing. J. Orthop. Sports Phys. Ther. 2016, 46, 286–292. [Google Scholar] [CrossRef]
- Chan, M.K.; Chow, K.W.; Lai, A.Y.; Mak, N.K.; Sze, J.C.; Tsang, S.M. The effects of therapeutic hip exercise with abdominal core activation on recruitment of the hip muscles. BMC Musculoskelet. Disord. 2017, 18, 313. [Google Scholar] [CrossRef]
- O’Sullivan, P.; Dankaerts, W.; Burnett, A.; Straker, L.; Bargon, G.; Moloney, N.; Perry, M.; Tsang, S. Lumbopelvic kinematics and trunk muscle activity during sitting on stable and unstable surfaces. J. Orthop. Sports Phys. Ther. 2006, 36, 19–25. [Google Scholar] [CrossRef]
- Cho, M.; Lee, M.; Jeong, T.; Chung, Y. Effect of lower limb resistance exercise with abdominal draw-in on stroke survivors: A pilot study. NeuroRehabilitation 2024, 55, 29–39. [Google Scholar] [CrossRef]
- Dafkou, K.; Kellis, E.; Ellinoudis, A.; Sahinis, C. The Effect of Additional External Resistance on Inter-Set Changes in Abdominal Muscle Thickness during Bridging Exercise. J. Sports Sci. Med. 2020, 19, 102–111. [Google Scholar] [PubMed]
| Characteristics | Mean ± SD |
|---|---|
| Age (year) | 23.36 ± 1.81 |
| Height (cm) | 174.21 ± 3.62 |
| Weight (kg) | 67.38 ± 4.51 |
| BMI | 23.23 ± 1.28 |
| Muscle Activity (%MVIC) | ADIM | MR | ADIM Combined with MR | F | p |
|---|---|---|---|---|---|
| Gluteus maximus | 22.97 ± 6.29 a,b | 66.91 ± 9.09 c | 74.77 ± 7.63 | 361.70 | <0.001 * |
| Erector spinae | 28.88 ± 7.34 a,b | 77.40 ± 8.12 c | 68.40 ± 8.60 | 263.59 | <0.001 * |
| Internal oblique | 22.87 ± 6.32 a,b | 40.22 ± 7.01 c | 57.67 ± 8.79 | 359.64 | <0.001 * |
| Hamstring | 39.03 ± 8.74 a,b | 80.54 ± 7.95 | 77.38 ± 8.03 | 236.63 | <0.001 * |
| Gluteus maximus/ Erector spinae ratio | 0.82 ± 0.33 b | 0.86 ± 0.16 c | 1.11 ± 0.18 | 11.22 | 0.001 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, D.-W.; Shin, Y.-J. Effects of the Combined Abdominal Draw-In Maneuver and Manual Resistance on Lumbopelvic Muscle Activity and Anterior Pelvic Tilt During Prone Hip Extension. Bioengineering 2025, 12, 1252. https://doi.org/10.3390/bioengineering12111252
Kim D-W, Shin Y-J. Effects of the Combined Abdominal Draw-In Maneuver and Manual Resistance on Lumbopelvic Muscle Activity and Anterior Pelvic Tilt During Prone Hip Extension. Bioengineering. 2025; 12(11):1252. https://doi.org/10.3390/bioengineering12111252
Chicago/Turabian StyleKim, Dong-Woo, and Young-Jun Shin. 2025. "Effects of the Combined Abdominal Draw-In Maneuver and Manual Resistance on Lumbopelvic Muscle Activity and Anterior Pelvic Tilt During Prone Hip Extension" Bioengineering 12, no. 11: 1252. https://doi.org/10.3390/bioengineering12111252
APA StyleKim, D.-W., & Shin, Y.-J. (2025). Effects of the Combined Abdominal Draw-In Maneuver and Manual Resistance on Lumbopelvic Muscle Activity and Anterior Pelvic Tilt During Prone Hip Extension. Bioengineering, 12(11), 1252. https://doi.org/10.3390/bioengineering12111252






