The Effects of Neuromuscular Training on Electromyography, Lower Extremity Kinematics, and Ground Reaction Force During an Unanticipated Side-Cut on Recreational Female Hockey Players
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Intervention and Implementation
2.3. Test Protocol
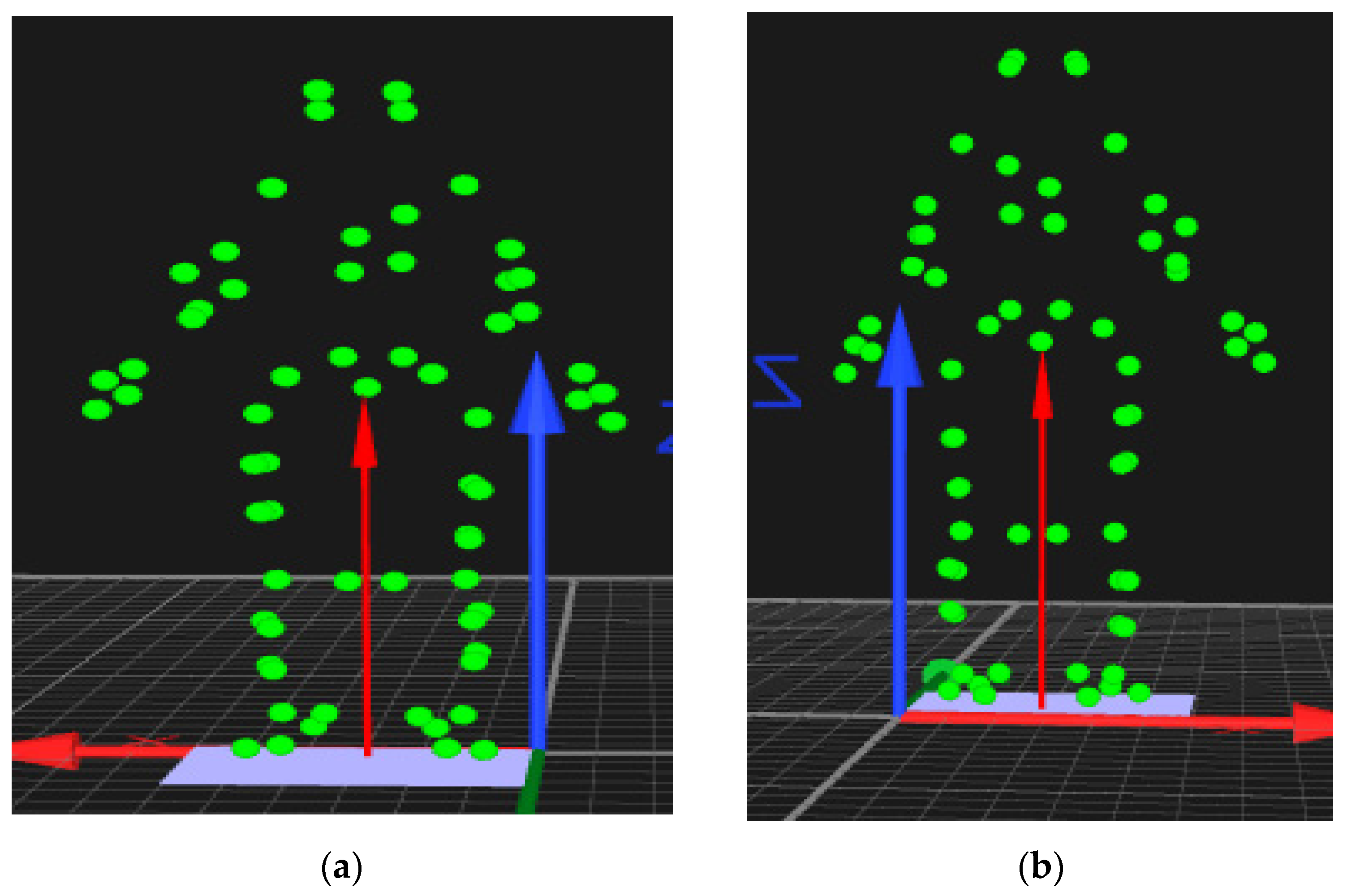
2.4. Unanticipated Side-Cut (USC)
3. Data Collection and Processing
3.1. EMG
3.2. Kinematic Data
3.3. Kinetics
3.4. Statistical Analysis
4. Results
4.1. EMG
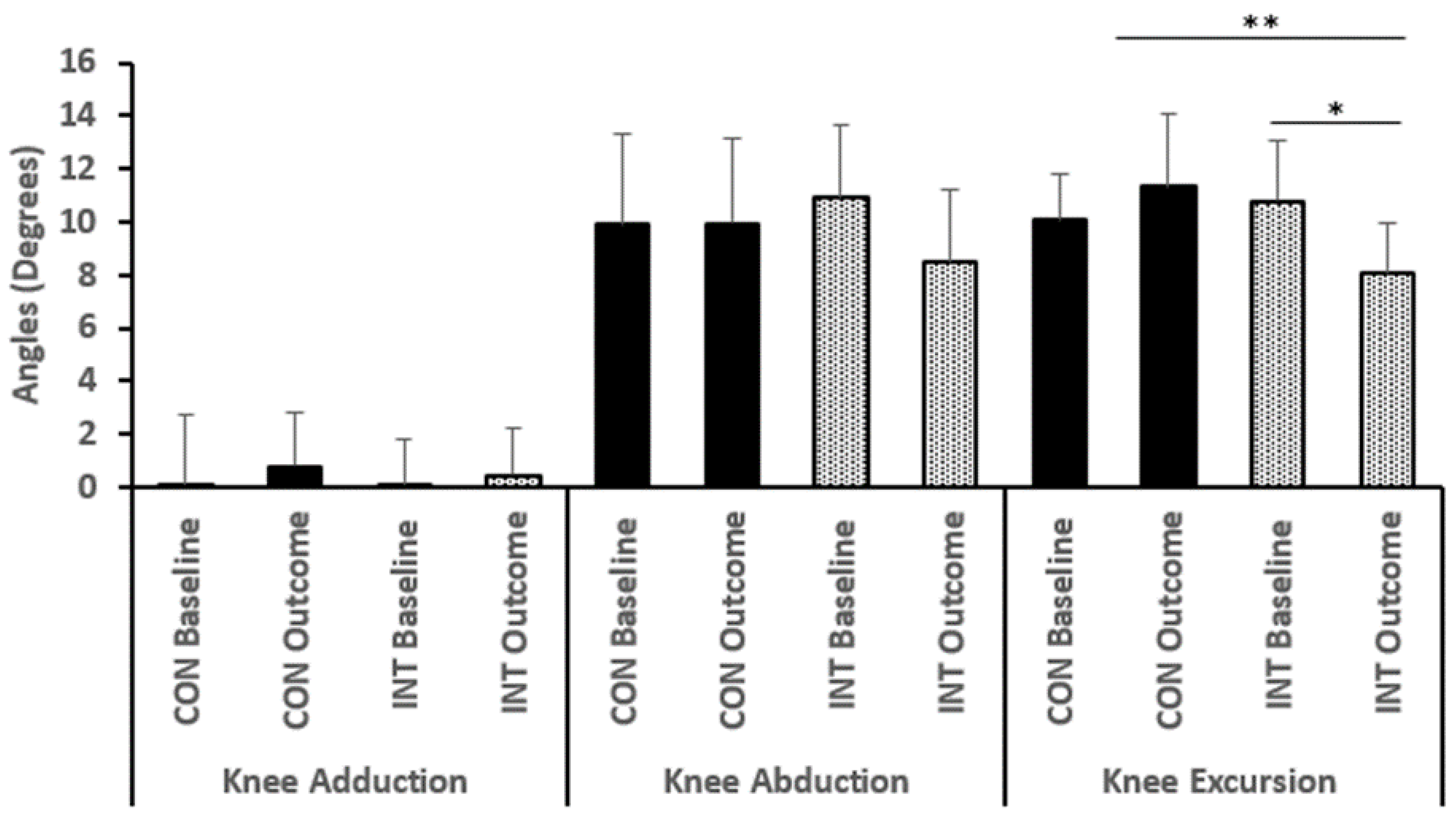
4.2. EMG Results, Kinematics Results, Kinetics Results
4.3. Kinetics
5. Discussion
5.1. EMG
5.2. Kinematics
5.3. Kinetics
5.4. Limitations and Future Studies
6. Summary
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hiepen, L.; Bosserhoff, N.; Schaudig, F.; Heitzer, F.; Jäger, M.; Mayer, C. Functional Knee Stability in Elite Field Hockey Depends on Playing Class and Gender. Sports Med. Int. Open 2024, 9, a24172488. [Google Scholar] [CrossRef]
- Barboza, S.D.; Nauta, J.; van der Pols, M.J.; van Mechelen, W.; Verhagen, E.A.L.M. Injuries in Dutch elite field hockey players: A prospective cohort study. Scand. J. Med. Sci. Sports 2018, 28, 1708–1714. [Google Scholar] [CrossRef] [PubMed]
- Hollander, K.; Wellmann, K.; Eulenburg, C.; Braumann, K.; Junge, A.; Zech, A.; Schiller, F. Epidemiology of injuries in outdoor and indoor hockey players over one season: A prospective cohort study. Br. J. Sports Med. 2018, 52, 1091–1096. [Google Scholar] [CrossRef] [PubMed]
- Rees, H.; McCarthy Persson, U.; Delahunt, E.; Boreham, C.; Blake, C. Epidemiology of injuries in senior men’s field hockey: A two-season prospective observational injury surveillance study. J. Sports Sci. 2020, 38, 2842–2849. [Google Scholar] [CrossRef]
- Silvers-Granelli, H.J.; Cohen, M.; Espregueira-Mendes, J.; Mandelbaum, B. Hamstring muscle injury in the athlete: State of the art. J. ISAKOS 2021, 6, 170–181. [Google Scholar] [CrossRef]
- Dick, R.; Hertel, J.; Agel, M.A.; Grossman, J.; Marshall, S.W. Descriptive Epidemiology of Collegiate Men’s Basketball Injuries, National Collegiate Athletic Association Injury Surveillance System, 1988–1989 Through 2003–2004. J. Athl. Train. 2010, 42, 194–201. [Google Scholar]
- Agel, J.; Olson, D.E.; Dick, R.; Arendt, E.A.; Marshall, S.W.; Sikka, R.S. Descriptive Epidemiology of Collegiate Women’s Basketball Injuries, National Collegiate Athletic Association Injury Surveillance System, 1988–1989 Through 2003–2004. J. Athl. Train. 2007, 42, 202–210. [Google Scholar]
- Beynnon, B.D.; Vacek, P.M.; Murphy, D.; Alosa, D.; Paller, D. First-time inversion Ankle Ligament Trauma. The effects of Sex, Level of Competition, and Sport on the incidence of Injury. Am. J. Sports Med. 2001, 33, 1485–1491. [Google Scholar] [CrossRef]
- Johnston, T.; Kaliarntas, K.; Brown, S.J.; Taylor, C. Noncontact Injuries, Rates, Mechanism and Occurrence in Field Hockey in Scotland. Euro. J. Sports Exerc. Sci. 2023, 11, 30–37. [Google Scholar]
- Ekstrand, J.; Hägglund, M.; Waldén, M. Injury incidence and injury patterns in professional football: The UEFA injury study. Br. J. Sports Med. 2011, 45, 553–558. [Google Scholar] [CrossRef] [PubMed]
- Al Attar, W.S.A.; Soomro, N.; Sinclair, P.J.; Pappas, E.; Sanders, R.H. Effect of injury prevention programs that include the Nordic hamstring exercise on hamstring injury rates in soccer players: A systematic review and meta-analysis. Sports Med. 2017, 47, 907–916. [Google Scholar] [CrossRef]
- Stergiou, M.; Calvo, A.L.; Forelli, F. Effectiveness of Neuromuscular Training in Preventing Lower Limb Soccer Injuries: A Systematic Review and Meta-Analysis. J. Clin. Med. 2025, 14, 1714. [Google Scholar] [CrossRef] [PubMed]
- Steinberg, N.; Dar, G.; Dunlop, M.; Gaida, J.E. The relationship of hip muscle performance to leg, ankle and foot injuries: A systematic review. Phys Sportsmed. 2017, 45, 49–63. [Google Scholar] [CrossRef]
- Soligard, T.; Myklebust, G.; Steffen, K.; Holme, I.; Silvers, H.; Bizzini, M.; Junge, A.; Dvorak, J.; Bahr, R.; Andersen, T.E. Comprehensive warm-up programme to prevent injuries in young female footballers: Cluster randomised controlled trial. BMJ 2008, 337, a2469. [Google Scholar] [CrossRef]
- Thorborg, K.; Krommes, K.K.; Esteve, E.; Clausen, M.B.; Bartels, E.M.; Rathleff, M.S. Effect of specific exercise-based football injury prevention programmes on the overall injury rate in football: A systematic review and meta-analysis of the FIFA 11 and 11+ programmes. Br. J. Sports Med. 2017, 51, 562–571. [Google Scholar] [CrossRef]
- Barboza, S.D.; Nauta, J.; Emery, C.; van Mechelen, W.; Gouttebarge, V.; Verhagen, E. A Warm-Up Program to Reduce Injuries in Youth Field Hockey Players: A Quasi-Experiment. J. Athl. Train. 2019, 54, 374–383. [Google Scholar] [CrossRef]
- Weir, G.; Alderson, J.A.; Elliott, B.C.; Lee, S.; Devaprakash, D.; Starre, K.; Goodman, C.; Cooke, J.; Rechichi, C.; Armstrong, J.; et al. A 2-yr Biomechanically Informed ACL Injury Prevention Training Intervention in Female Field Hockey Players. Transl. J. Am. Coll. Sports Med. 2019, 4, 206–214. [Google Scholar] [CrossRef]
- Myer, G.D.; Faigenbaum, A.D.; Ford, K.R.; Best, T.M.; Bergeron, M.F.; Hewett, T.E. When to Initiate Integrative Neuromuscular Training to Reduce Sports-Related Injuries and Enhance Health in Youth? Curr. Sports Med. Rep. 2011, 10, 155–166. [Google Scholar] [CrossRef] [PubMed]
- Petushek, E.J.; Sugimoto, D.; Stoolmiller, M.; Smith, G.; Myer, G.D. Evidence-Based Best-Practice Guidelines for Preventing Anterior Cruciate Ligament Injuries in Young Female Athletes: A Systematic Review and Meta-analysis. Am. J. Sports Med. 2019, 47, 1744–1753. [Google Scholar] [CrossRef]
- Parsons, J.L.; Alexander, M.J.L. Modifying Spike Jump Landing Biomechanics in Female Adolescent Volleyball Athletes Using Video and Verbal Feedback. J. Strength Cond. Res. 2012, 26, 1076–1084. [Google Scholar] [CrossRef] [PubMed]
- Sugimoto, D.; Myer, G.D.; Barber Foss, K.D.; Pepin, M.J.; Micheli, L.J.; Hewett, T.E. Critical components of neuromuscular training to reduce ACL injury risk in female athletes: Meta-regression analysis. Br. J. Sports Med. 2016, 50, 1259–1266. [Google Scholar] [CrossRef] [PubMed]
- Sugimoto, D.; Myer, G.D.; Foss, K.D.; Hewett, T.E. Dosage effects of neuromuscular training intervention to reduce anterior cruciate ligament injuries in female athletes: Meta- and sub-group analyses. Sports Med. 2014, 44, 551–562. [Google Scholar] [CrossRef]
- Harry, J.R.; Lanier, R.; Nunley, B.; Blinch, J. Focus of attention effects on lower extremity biomechanics during vertical jump landings. Hum. Mov. Sci. 2019, 68, 102521. [Google Scholar] [CrossRef]
- Donnelly, C.J.; Elliott, B.C.; Ackland, T.R.; Doyle, T.L.A.; Beiser, T.F.; Finch, C.F.; Cochrane, J.L.; Dempsey, A.R.; Lloyd, D.G. An anterior cruciate ligament injury prevention framework: Incorporating the recent evidence. Res. Sports Med. 2012, 20, 239–262. [Google Scholar] [CrossRef]
- Hoffman, T.C.; Glasziou, P.P.; Boutron, I.; Milne, R.; Perera, R.; Moher, D.; Altman, D.G.; Barbour, V.; MacDonal, H.; Johnston, M.; et al. Better reporting of interventions: Template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014, 348, g1687. [Google Scholar] [CrossRef] [PubMed]
- Hewett, T.E.; Lindenfeld, T.N.; Riccobene, J.V.; Noyes, F.R. The Effect of Neuromuscular Training on the Incidence of Knee Injury in Female Athletes. Am. J. Sports Med. 1999, 27, 699–706. [Google Scholar] [CrossRef]
- Hewett, T.E.; Myer, G.D.; Ford, K.R.; Heidt, R.S., Jr.; Colosimo, A.J.; McLean, S.G.; van den Bogert, A.J.; Paterno, M.V.; Succop, P. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: A prospective study. Am. J. Sports Med. 2005, 33, 492–501. [Google Scholar] [CrossRef] [PubMed]
- Lephart, S.M.; Abt, J.P.; Ferris, C.M.; Sell, T.C.; Nagai, T.; Myers, J.B.; Irrgang, J.J. Neuromuscular and biomechanical characteristic changes in high school athletes: A plyometric versus basic resistance program. Br. J. Sports Med. 2005, 39, 932–938. [Google Scholar] [CrossRef]
- Myer, G.D.; Ford, K.R.; Paterno, M.V.; Nick, T.G.; Hewett, T.E. The Effects of Generalized Joint Laxity on Risk of Anterior Cruciate Ligament Injury in Young Female Athletes. Am. J. Sports Med. 2008, 36, 1073–1080. [Google Scholar] [CrossRef]
- Yoo, J.H.; Lim, B.O.; Ha, M.; Lee, S.W.; Oh, S.J.; Lee, Y.S.; Kim, J.G. A meta-analysis of the effect of neuromuscular training on the prevention of the anterior cruciate ligament injury in female athletes. Knee Surg. Sports Traumatol. Arthrosc. 2010, 18, 824–830. [Google Scholar] [CrossRef]
- Zazulak, B.T.; Hewett, T.E.; Reeves, N.P.; Goldberg, B.; Cholewicki, J. Deficits in Neuromuscular Control of the Trunk Predict Knee Injury Risk: Prospective Biomechanical-Epidemiologic Study. Am. J. Sports Med. 2007, 35, 1123–1130. [Google Scholar] [CrossRef]
- Benjaminse, A.; Gokeler, A.; Dowling, A.V.; Faigenbaum, A.; Ford, K.R.; Hewett, T.E.; Onate, J.A.; Otten, B.; Myer, G.D. Optimization of the anterior cruciate ligament injury prevention paradigm: Novel feedback techniques to enhance motor learning and reduce injury risk. J. Orthop. Sports Phys. 2015, 45, 170–182. [Google Scholar] [CrossRef]
- Steib, S.; Rahlf, A.L.; Pfeifer, K.; Zech, A. Dose-Response Relationship of Neuromuscular Training for Injury Prevention in Youth Athletes: A Meta-Analysis. Front. Physiol. 2017, 8, 920. [Google Scholar] [CrossRef]
- Borg, G.A. Psychophysical bases of perceived exertion. Med. Sci. Sports Exerc. 1982, 14, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Ford, K.R.; Myer, G.D.; Toms, H.E.; Hewitt, T.E. Gender Differences in the Kinematics of Unanticipated Cutting in Young Athletes. Med. Sci. Sports Exerc. 2005, 37, 124–129. [Google Scholar] [CrossRef]
- Hermans, H.J.; Freriks, B.; Merletti, R.; Stegeman, D.; Blok, J.; Rau, G.; Disselhorst-Klug, C.; Hagg. European Recommendations for Surface ElectroMyoGraphy, 2nd ed.; Roessingh Research and Development: Enschede, The Netherlands, 1999. [Google Scholar]
- Albertus-Kajee, Y.; Tucker, R.; Derman, W.; Lamberts, R.P.; Lambert, M.I. Alternative methods of normalizing EMG during running. J. Electromyogr. Kinesiol. 2011, 21, 579–586. [Google Scholar] [CrossRef] [PubMed]
- Burden, A.M. How should we normalize electromyograms obtained from healthy participants What we have learned from over 25 years of research. J. Electromyogr. Kinesiol. 2010, 20, 1023–1035. [Google Scholar] [CrossRef]
- Winter, D.A. Biomechanics and Motor Control of Human Movement, 3rd ed.; Wiley: Hoboken, MJ, USA; Chichester, UK, 2005; ISBN 047144989X. [Google Scholar]
- Roewer, B.D.; Ford, K.R.; Myer, G.D.; Hewett, T.E. The ‘impact’ of force filtering cut-off frequency on the peak knee abduction moment during landing: Artefact or ‘artifiction’? Br. J. Sports Med. 2014, 48, 464–468. [Google Scholar] [CrossRef] [PubMed]
- Pappas, E.; Shiyko, M.P.; Ford, K.R.; Myer, G.D.; Hewett, T.E. Biomechanical Deficit Profiles Associated with ACL Injury Risk in Female Athletes. Med. Sci. Sports Exerc. 2016, 48, 107–113. [Google Scholar] [CrossRef]
- Neto, W.K.; Soares, E.G.; Vieira, T.L.; Aguiar, R.; Chola, T.A.; Sampaio, V.L.; Gama, E.F. Gluteus Maximus Activation During Common Strength and Hypertrophy Exercises: A Systematic Review. JSSM 2020, 19, 195–203. [Google Scholar]
- Boren, K.; Conrey, C.; Le Coguic, J.; Paprocki, L.; Voight, M.; Robinson, T.K. Electromyographic analysis of gluteus medius and gluteus maximus during rehabilitation exercises. IJSPT 2011, 6, 206–223. [Google Scholar]
- Khayambashi, K.; Ghoddosi, N.; Straub, R.K.; Powers, C.M. Hip muscle strength predicts non-contact anterior cruciate ligament injury in male and female athletes: A prospective study. Am. J. Sports Med. 2016, 44, 355–361. [Google Scholar] [CrossRef] [PubMed]
- Wilderman, D.R.; Ross, S.E.; Padua, D.A. Thigh Muscle Activity, Knee Motion, and Impact Force During Side-Step Pivoting in Agility-Trained Female Basketball players. J. Athl. Train. 2009, 44, 14–25. [Google Scholar] [CrossRef]
- van den Tillaar, R.; Solheim, J.A.B.; Bencke, J. Comparison of Hamstring Muscle Activation during High-Speed Running and various Hamstring Strengthening Exercises. Int. J. Sports Phys. Ther. 2017, 12, 718–727. [Google Scholar] [CrossRef] [PubMed]
- van Dyk, N.; Behan, F.P.; Whiteley, R. Including the Nordic hamstring exercise in injury prevention programmes halves the rate of hamstring injuries: A systematic review and meta-analysis of 8459 athletes. Br. J. Sports Med. 2019, 53, 1362–1370. [Google Scholar] [CrossRef]
- Zebis, M.K.; Benke, J.; Andersen, L.L.; Dossing, S.; Alkaer, T.; Magnusson, P.; Kjaer, M.; Aagaard, P. The Effects of Neuromuscular Training on Knee Joint Motor Control During Sidecutting in Female Elite Soccer and Handball Players. J. Clin. Med. 2008, 18, 329–337. [Google Scholar] [CrossRef] [PubMed]
- Zebis, M.K.; Andersen, L.L.; Brandt, M.; Myklebust, G.; Bencke, J.; Lauridsen, H.B.; Bandholm, T.; Thorborg, K.; Hölmich, P.; Aagaard, P. Effects of evidence-based prevention training on neuromuscular and biomechanical risk factors for ACL injury in adolescent female athletes: A randomized controlled trial. Br. J. Sports Med. 2016, 50, 552–557. [Google Scholar] [CrossRef]
- Gentil, P.; Souza, D.; Santana, M.; Alves, R.R.; Campos, M.H.; Pinto, R.; Bottaro, M. Multi- and Single-Joint Resistance Exercises Promote Similar Plantar Flexor Activation in Resistance Trained Men. Int. J. Environ. Res. Public Health 2020, 17, 9487. [Google Scholar] [CrossRef]
- Ali, N.; Andersen, M.S.; Rasmussen, J.; Robertson, D.G.E.; Rouhi, G. The application of musculoskeletal modeling to investigate gender bias in non-contact ACL injury rate during single-leg landings. CMBBE 2014, 17, 1602–1616. [Google Scholar] [CrossRef]
- Benke, J.; Curtis, D.; Krogshede, C.; Jensen, L.K.; Bandholm, T.; Zebis, M.K. Biomechanical evaluation of the side-cutting manoeuvre associated with ACL injury in young female handball players. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 1876–1881. [Google Scholar] [CrossRef]
- Błaszczyszyn, M.; Konieczny, M.; Pakosz, P. Analysis of ankle sEMG on both stable and unstable surfaces for elderly and young women—A pilot study. Int. J. Environ. Res. Public Health 2019, 16, 1544. [Google Scholar] [CrossRef]
- Brunner, R.; Friesenbichler, B.; Casartelli, N.C.; Bizzini, M.; Maffiuletti, N.A.; Niedermann, K. Effectiveness of multicomponent lower extremity injury prevention programmes in team-sport athletes: An umbrella review. Br. J. Sports Med. 2019, 53, 282–288. [Google Scholar] [CrossRef]
- Timmins, R.G.; Opar, D.A.; Williams, M.D.; Schache, A.G.; Dear, N.M.; Shield, A.J. Reduced biceps femoris myoelectrical activity influences eccentric knee flexor weakness after repeat sprint running. Scand. J. Med. Sci. Sports 2014, 24, e299–e305. [Google Scholar] [CrossRef]
- Bakker, R.; Tomescu, S.; Brenneman, E.; Hangalur, G.; Laing, A.; Chandrashekar, N. Effect of sagittal plane mechanics on ACL strain during jump landing. J. Orthop. 2016, 34, 1636–1644. [Google Scholar] [CrossRef]
- Ireland, M.L.; Willson, J.D.; Ballantyne, B.T.; McClay-Davis, I. Hip Strength in Females With and Without Patellofemoral Pain. J. Orthop. Sports Phys. 2003, 33, 671–676. [Google Scholar] [CrossRef]
- Baldon Rde, M.; Serrão, F.V.; Scattone Silva, R.; Piva, S.R. Effects of functional stabilization training on pain, function, and lower extremity biomechanics in women with patellofemoral pain: A randomized clinical trial. J. Orthop. Sports Phys. Ther. 2014, 44, 240–251+A1–A8. [Google Scholar] [CrossRef] [PubMed]
- Quatman, C.E.; Ford, K.R.; Myer, G.D. Maturation Leads to Gender Differences in Landing Force and Vertical Jump Performance, A Longitudinal Study. Am. J. Sports Med. 2006, 34, 806–813. [Google Scholar] [CrossRef]
- Myer, G.D.; Ford, K.R.; Khoury, J.; Succop, P.; Hewett, T.E. Development and Validation of a clinical-Based Prediction Tool to Identify Female Athletes at High Risk for Anterior Cruciate Ligament Injury. Am. J. Sports Med. 2010, 38, 2025–2033. [Google Scholar] [CrossRef] [PubMed]
- Ireland, M.L. The female ACL: Why is it more prone to injury. J. Orthop. 2016, 13, A1–A4. [Google Scholar] [CrossRef]
- Della Villa, F.; Buckthorpe, M.; Grassi, A.; Nabiuzzi, A.; Tosarelli, F.; Zaffagnini, S.; Della Villa, S. Systematic video analysis of ACL injuries in professional male football (soccer): Injury mechanisms, situational patterns and biomechanics study on 134 consecutive cases. Br. J. Sports Med. 2020, 54, 1423–1432. [Google Scholar] [CrossRef] [PubMed]
- Hopper, A.J.; Haff, E.E.; Joyce, C.; Lloyd, R.S.; Haff, G.G. Neuromuscular Training Improves Lower Extremity Biomechanics Associated with Knee Injury during Landing in 11–13 Year Old Female Netball Athletes: A Randomized Control Study. Front. Physiol. 2017, 8, 883. [Google Scholar] [CrossRef]
- Yom, J.P.; Owens, T.; Arnett, S.; Beebe, J.; Son, V. The effects of an unanticipated side-cut on lower extremity kinematics and ground reaction forces during a drop landing. Sports Biomech. 2018, 18, 414–425. [Google Scholar] [CrossRef]
- Woo, S.L.; Hollis, J.M.; Adams, D.J.; Lyon, R.M.; Takai, S. Tensile properties of the human femur-anterior cruciate ligament-tibia complex. The effects of specimen age and orientation. Am. J. Sports Med. 1991, 19, 217–225. [Google Scholar] [CrossRef] [PubMed]
- Distefano, L.J.; Blackburn, J.T.; Marshall, S.W.; Padua, D.A. Gluteal Activation During Common Therapeutic Exercises. J. Orthop. Sports Phys. 2009, 39, 532–540. [Google Scholar] [CrossRef] [PubMed]
- Irmischer, B.S.; Harris, C.; Pfeiffer, R.P.; DeBeliso, M.A.; Adams, K.J.; Shea, K.G. Effects of a knee Ligament Injury Prevention Exercise Program on Impact Forces in Women. J. Strength Cond. Res. 2004, 18, 703–707. [Google Scholar] [CrossRef] [PubMed]
- Marinsek, M. Basic Landing Characteristics and their Application in Artistic Gymnastics. Sci. Gymnast. J. 2010, 2, 59–67. [Google Scholar] [CrossRef]



| Anatomical Site | Marker Placement (No. of Markers) |
|---|---|
| Head | Left and Right Anterior and Posterior Cranium (4) |
| Trunk (Treated as a Single Segment) | Acromion Process (2) Posterior Superior Iliac Spine—PSIS (2) Upper Thoracic Cluster (4) |
| Arm and Finger (Bilateral) | Acromion Process (1) Lateral and Medial Elbow Epicondyle (2) Lateral and Medial Aspects of the Styloid Process (2) Third Metacarpal (Distal End) (1) |
| Pelvis (a CODA Pelvis) | Anterior Superior Iliac Spine—ASIS (2) Posterior Superior Iliac Spine—PSIS (2) Sacrum |
| Thigh (Bilateral) | Greater Trochanter (1) Lateral and Medial Femoral Condyle (2) Thigh Cluster (4) |
| Shank (Bilateral) | Lateral and Medial Femoral Condyle (2) Lateral and Medial Malleolus (2) Shank Cluster (4) |
| Foot (Bilateral) | Lateral and Medial Malleolus (2) Heel (1) 1st and 5th Metatarsal (2) |
| Variables | Groups | ||
|---|---|---|---|
| CON | INT | p-Value | |
| Age (yrs) | 20.04 (1.6) | 19.9 (1.1) | 0.97 |
| Height (cm) | 165.2 (4.7) | 167.6 (5.4) | 0.40 |
| Body mass (kg) (baseline) | 62.9 (7.8) | 66.0 (6.3) | 0.68 |
| Body mass (kg) (8 weeks) | 62.7 (7.8) | 66.4 (6.4) | 0.74 |
| No. of games per week (n) | 1.5 (0.6) | 1.8 (0.4) | 0.09 |
| No. of training sessions (hockey) (n) | 1.21 (0.4) | 1.0 (0.3) | 0.92 |
| No. of training sessions per week (not hockey) (n) | 1.0 (0.6) | 1.1 (0.8) | 0.43 |
| Playing experience (years) | 9.3 (3.1) | 11.2 (2.4) | 0.03 |
| No. of injuries in intervention period (n) | 0.2 (0.4) | 0.1 (0.3) | 0.32 |
| Muscle | Time Point | Group | Normalized EMG (%) Mean (SD) | p-Value | |
|---|---|---|---|---|---|
| Baseline | Week 8 | Interaction | |||
| GasMed | 30 ms prior to IC | CON INT | 25.3 (14.9) 18.3 (11.6) | 28.4 (11.9) 23.1 (16.7) | 0.723 |
| 50 ms after IC | CON INT | 19.9 (11.7) 25.1 (11.1) | 20.2 (10.4) 28.8 (10.8) | 0.315 | |
| GasLat | 30 ms before IC | CON INT | 27.1 (15.2) 17.9 (9.9) | 25.9 (9.9) 24.0 (15.0) | 0.298 |
| 50 ms after IC | CON INT | 18.7 (10.1) 24.1 (12.4) | 20.8 (10.5) 28.3 (8.1) | 0.183 | |
| ST | 30 ms before IC | CON INT | 35.9 (11.5) 35.7 (15.1) | 31.1 (9.9) 34.2 (18.6) | 0.291 |
| IC to 50 ms | CON INT | 37.2 (11.6) 37.8 (11.5) | 31.1 (8.2) 34.5 (9.8) | 0.030 | |
| BF | 30 ms before IC | CON INT | 36.3 (13.7) 33.7 (15.2) | 37.1 (15.2) 34.4 (11.4) | 0.800 |
| IC to 50 ms | CON INT | 35.6 (11.1) 35.5 (12.2) | 33.4 (9.9) 35.6 (9.6) | 0.567 | |
| GMed | 30 ms before IC | CON INT | 27.9 (11.7) 24.7 (7.1) | 21.9 (6.1) 22.1 (8.4) | 0.013 |
| IC to 50 ms | CON INT | 29.2 (10.8) 23.2 (8.2) | 24.5 (6.1) 23.9 (4.7) | 0.035 | |
| GMax | 30 ms before IC | CON INT | 29.2 (12.6) 28.9 (9.8) | 24.4 (9.6) 24.9 (12.0) | 0.067 |
| IC to 50 ms | CON INT | 19.9 (11.7) 27.2 (11.9) | 20.5 (10.1) 29.0 (10.6) | 0.542 | |
| Joint | Time Point | Variable | Group | Value | ||
|---|---|---|---|---|---|---|
| Before | Week 8 | Interaction | ||||
| Hip | IC | Flexion | CON INT | 38.86 (8.6) 41.99 (9.8) | 37.85 (8.7) 35.77 (8.7) | 0.853 |
| IC | Lateral flexion | CON INT | 12.74 (5.4) 10.87 (6.4) | 10.87 (6.4) 9.72 (5.4) | 0.291 | |
| Knee | IC | Flexion | CON INT | 20.70 (6.7) 19.28 (10.1) | 18.64 (8.4) 17.96 (8.2) | 0.193 |
| Knee | IC | Abduction | CON INT | 0.27 (4.5) 1.01 (4.3) | 0.77 (4.9) 1.9 (3.1) | 0.732 |
| Joint | Time Point | Variable | Group | Value | ||
|---|---|---|---|---|---|---|
| Before | Week 8 | Interaction | ||||
| Hip | MKF | Flexion | CON INT | 45.7 (11.7) 45.2 (11.1) | 46.1 (11.0) 38.8 (8.0) | 0.073 |
| MKF | Lateral flexion | CON INT | 13.02 (7.3) 11.4 (6.6) | 12.4 (7.2) 10.4 (6.2) | 0.370 | |
| Knee | MKF | Flexion | CON INT | 61.8 (7.2) 62.0 (11.5) | 63.6 (6.9) 63.6 (6.8) | 0.680 |
| MKF | Abduction | CON INT | −1.09 (6.7) −3.81 (7.6) | −3.65(7.1) −5.68 (6.6) | 0.055 | |
| Variable | Group | Value Mean (SD) | p-Value | |||
|---|---|---|---|---|---|---|
| Before | Week 8 | Interaction | Within | Between | ||
| Peak vGRF | CON | 1185.2 (212.6) | 1226.3 (211.2) | 0.838 | 0.170 | 0.910 |
| (N) | INT | 1226.7 (208.6) | 1171.5 (180.5) | |||
| Norm vGRF | CON | 1.97 (0.3) | 1.98 (0.3) | 0.527 | 0.360 | 0.100 |
| (N/BW) | INT | 1.90 (0.3) | 1.82 (0.2) | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Johnston, T.; Valentin, S.; Brown, S.J.; Kaliarntas, K. The Effects of Neuromuscular Training on Electromyography, Lower Extremity Kinematics, and Ground Reaction Force During an Unanticipated Side-Cut on Recreational Female Hockey Players. Bioengineering 2025, 12, 1101. https://doi.org/10.3390/bioengineering12101101
Johnston T, Valentin S, Brown SJ, Kaliarntas K. The Effects of Neuromuscular Training on Electromyography, Lower Extremity Kinematics, and Ground Reaction Force During an Unanticipated Side-Cut on Recreational Female Hockey Players. Bioengineering. 2025; 12(10):1101. https://doi.org/10.3390/bioengineering12101101
Chicago/Turabian StyleJohnston, Tom, Stephanie Valentin, Susan J. Brown, and Konstantinos Kaliarntas. 2025. "The Effects of Neuromuscular Training on Electromyography, Lower Extremity Kinematics, and Ground Reaction Force During an Unanticipated Side-Cut on Recreational Female Hockey Players" Bioengineering 12, no. 10: 1101. https://doi.org/10.3390/bioengineering12101101
APA StyleJohnston, T., Valentin, S., Brown, S. J., & Kaliarntas, K. (2025). The Effects of Neuromuscular Training on Electromyography, Lower Extremity Kinematics, and Ground Reaction Force During an Unanticipated Side-Cut on Recreational Female Hockey Players. Bioengineering, 12(10), 1101. https://doi.org/10.3390/bioengineering12101101







