Association Between Neck Circumference and Uncontrolled Hyperglycemia Diabetes in Korean Adults: From the Korea National Health and Nutrition Examination Survey, 2019 to 2021
Abstract
1. Introduction
2. Materials and Methods
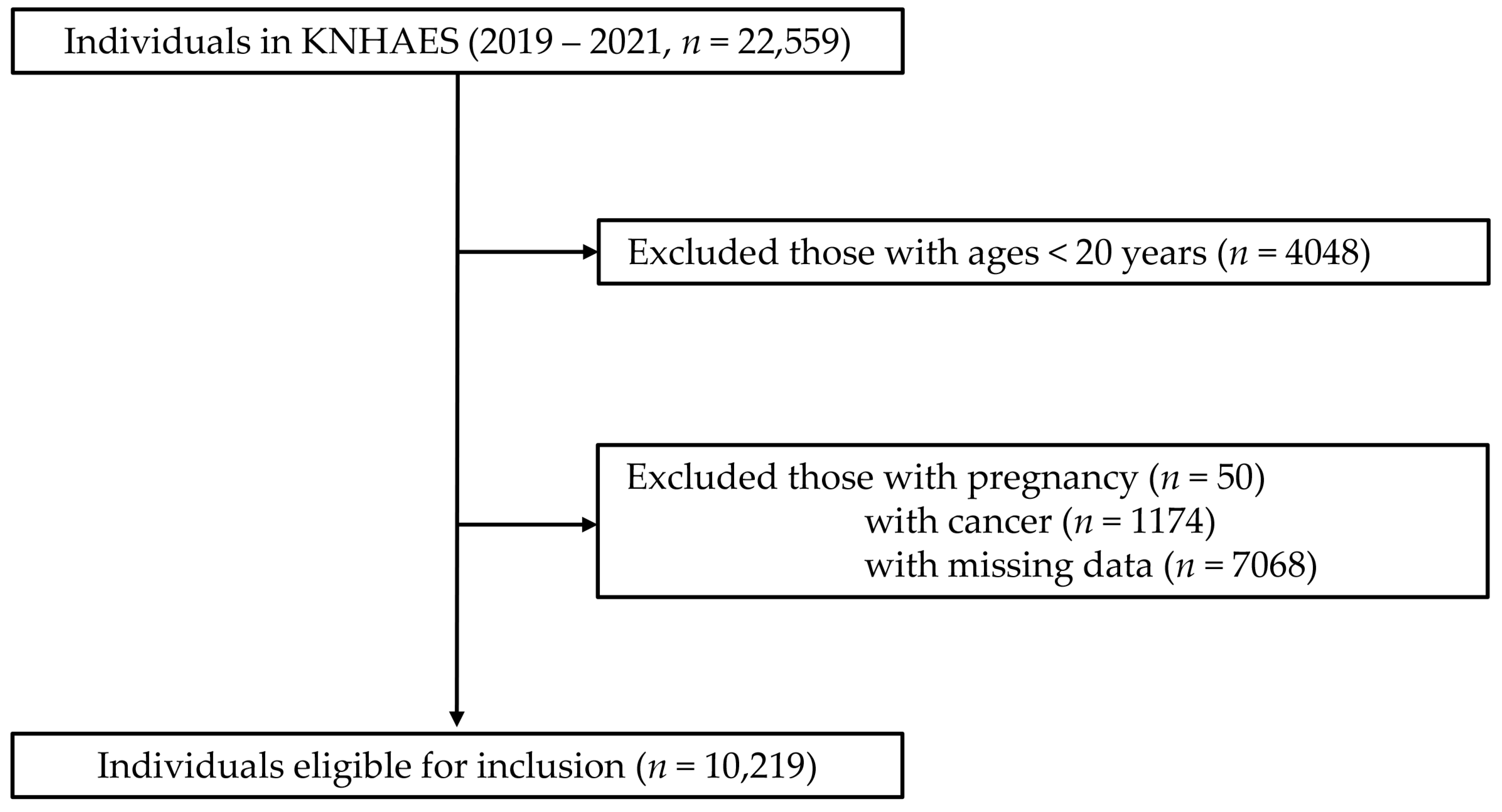
2.1. Study Population
2.2. Demographic Data and Measurements
2.3. Definition of Uncontrolled DM, Hyperglycemia of Non-DM, and MetS
2.4. Statistical Analysis
3. Results
3.1. Baseline Characteristics of the Study Participants
3.2. Associations of NC and Hyperglycemia and Uncontrolled DM
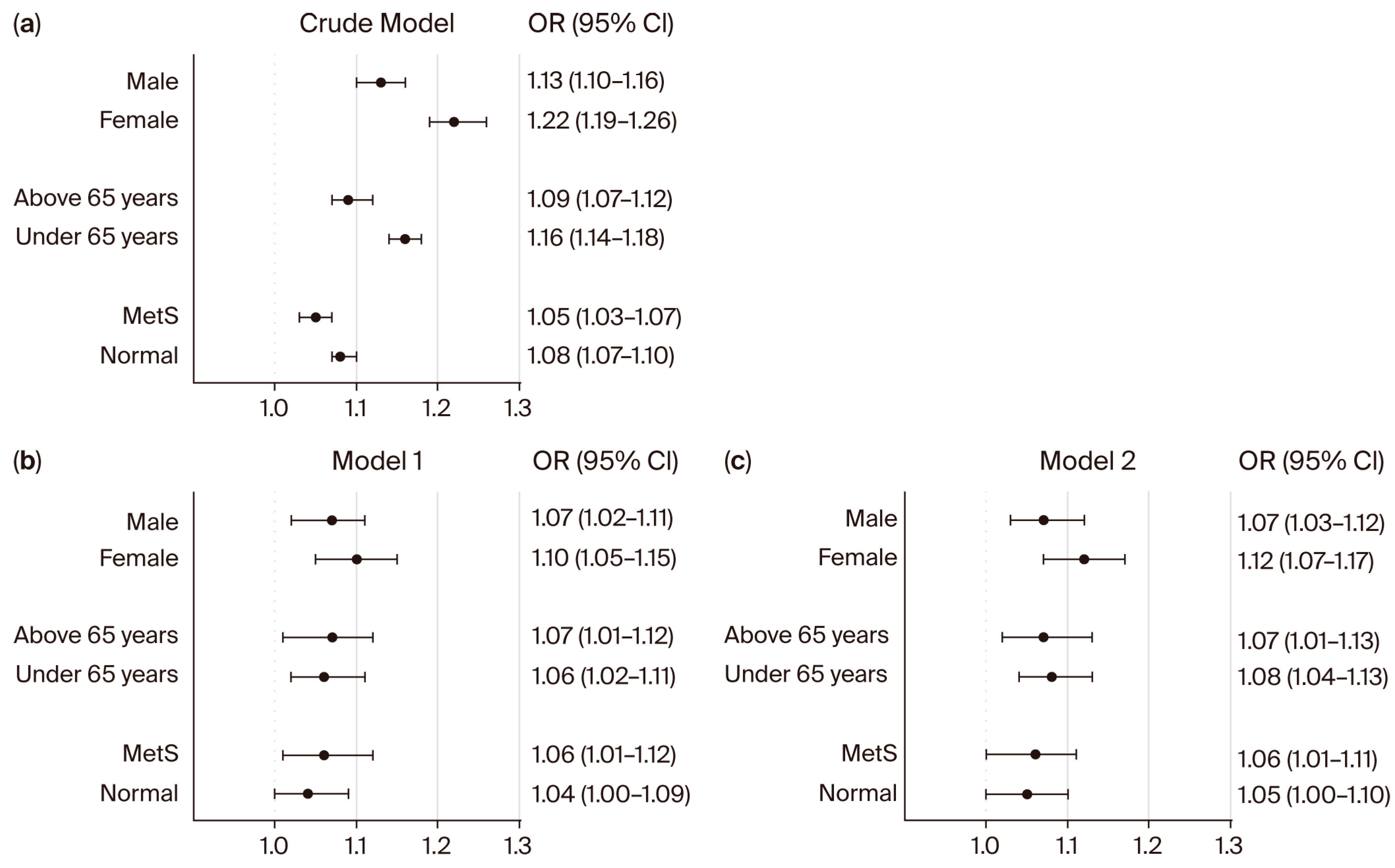
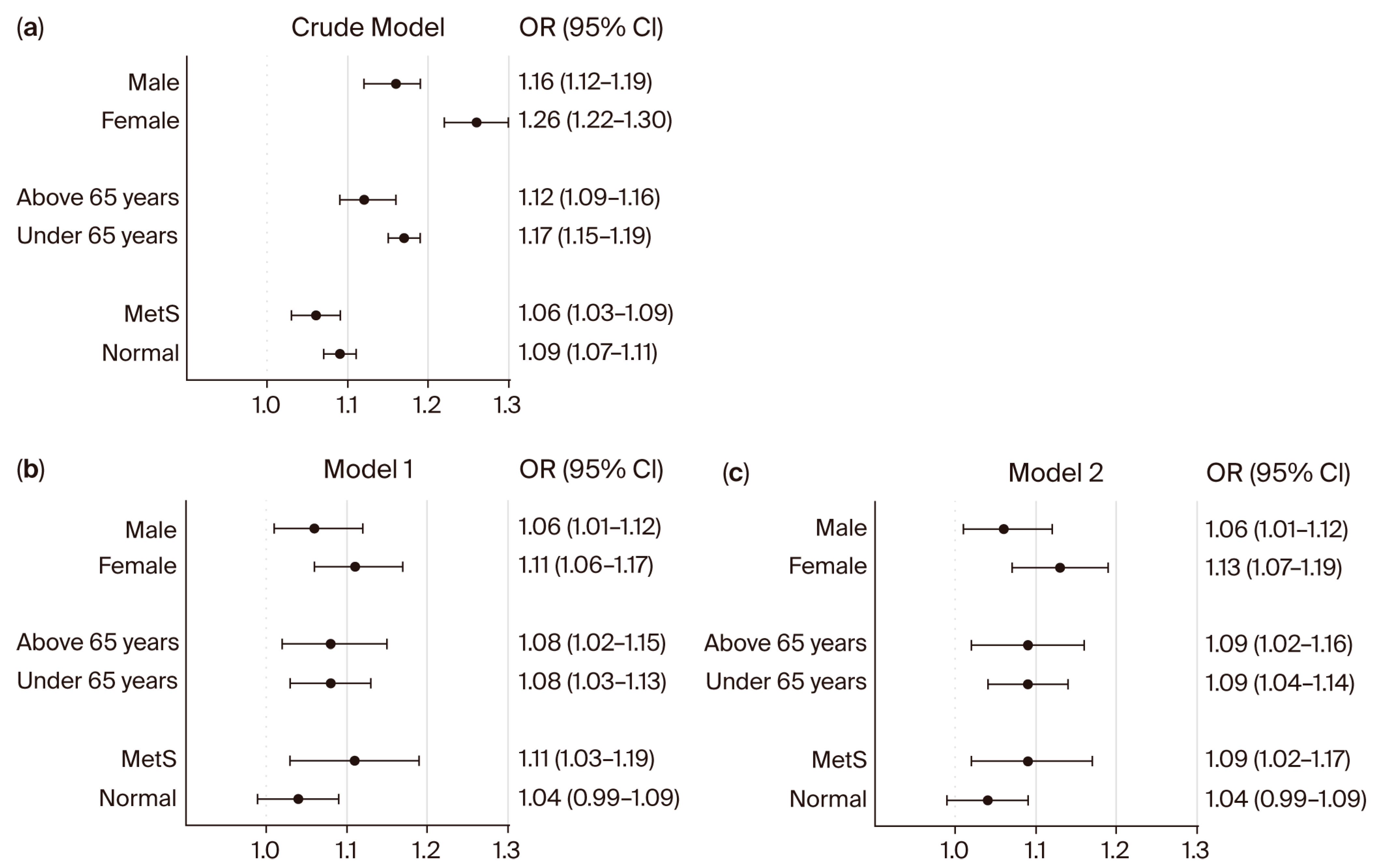
3.3. Subgroup Analysis of NC and Both Hyperglycemia and Uncontrolled DM Association
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| DM | Diabetes mellitus |
| CVD | Cardiovascular disease |
| BMI | Body mass index |
| WC | Waist circumference |
| NC | Neck circumference |
| MetS | Metabolic syndrome |
| CKD | Chronic kidney disease |
| HTN | Hypertension |
References
- Hossain, M.J.; Al-Mamun, M.; Islam, M.R. Diabetes mellitus, the fastest growing global public health concern: Early detection should be focused. Health Sci. Rep. 2024, 7, e2004. [Google Scholar] [CrossRef] [PubMed]
- Zhou, B.; Rayner, A.W.; Gregg, E.W.; Sheffer, K.E.; Carrillo-Larco, R.M.; Bennett, J.E.; Shaw, J.E.; Paciorek, C.J.; Singleton, R.K.; Pires, A.B.; et al. Worldwide trends in diabetes prevalence and treatment from 1990 to 2022: A pooled analysis of 1108 population-representative studies with 141 million participants. Lancet 2024, 404, 2077–2093. [Google Scholar] [CrossRef] [PubMed]
- Saeedi, P.; Petersohn, I.; Salpea, P.; Malanda, B.; Karuranga, S.; Unwin, N.; Colagiuri, S.; Guariguata, L.; Motala, A.A.; Ogurtsova, K. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas. Diabetes Res. Clin. Pract. 2019, 157, 107843. [Google Scholar] [CrossRef]
- Ingelfinger, J.R.; Jarcho, J.A. Increase in the incidence of diabetes and its implications. N. Engl. J. Med. 2017, 376, 1473–1474. [Google Scholar] [CrossRef]
- Lin, X.; Xu, Y.; Pan, X.; Xu, J.; Ding, Y.; Sun, X.; Song, X.; Ren, Y.; Shan, P.-F. Global, regional, and national burden and trend of diabetes in 195 countries and territories: An analysis from 1990 to 2025. Sci. Rep. 2020, 10, 14790. [Google Scholar] [CrossRef]
- Cannon, A.; Handelsman, Y.; Heile, M.; Shannon, M. Burden of illness in type 2 diabetes mellitus. J. Manag. Care Spec. Pharm. 2018, 24, S5–S13. [Google Scholar] [CrossRef] [PubMed]
- Tripathi, B.K.; Srivastava, A.K. Diabetes mellitus: Complications and therapeutics. Med. Sci. Monit. 2006, 12, 130–147. [Google Scholar]
- Harding, J.L.; Pavkov, M.E.; Magliano, D.J.; Shaw, J.E.; Gregg, E.W. Global trends in diabetes complications: A review of current evidence. Diabetologia 2019, 62, 3–16. [Google Scholar] [CrossRef]
- Rao Kondapally Seshasai, S.; Kaptoge, S.; Thompson, A.; Di Angelantonio, E.; Gao, P.; Sarwar, N.; Whincup, P.H.; Mukamal, K.J.; Gillum, R.F.; Holme, I.; et al. Diabetes mellitus, fasting glucose, and risk of cause-specific death. N. Engl. J. Med. 2011, 364, 829–841. [Google Scholar]
- Stratton, I.M.; Adler, A.I.; Neil, H.A.W.; Matthews, D.R.; Manley, S.E.; Cull, C.A.; Hadden, D.; Turner, R.C.; Holman, R.R. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): Prospective observational study. BMJ 2000, 321, 405–412. [Google Scholar] [CrossRef]
- American Diabetes Association. 6. Glycemic targets: Standards of medical care in diabetes—2019. Diabetes Care 2019, 42, S61–S70. [Google Scholar] [CrossRef] [PubMed]
- Luc, K.; Schramm-Luc, A.; Guzik, T.; Mikolajczyk, T. Oxidative stress and inflammatory markers in prediabetes and diabetes. J. Physiol. Pharmacol. 2019, 70. [Google Scholar] [CrossRef]
- Evans, J.L.; Maddux, B.A.; Goldfine, I.D. The molecular basis for oxidative stress-induced insulin resistance. Antioxid. Redox Signal. 2005, 7, 1040–1052. [Google Scholar] [CrossRef]
- Głuszek, S.; Ciesla, E.; Głuszek-Osuch, M.; Kozieł, D.; Kiebzak, W.; Wypchło, Ł.; Suliga, E. Anthropometric indices and cut-off points in the diagnosis of metabolic disorders. PLoS ONE 2020, 15, e0235121. [Google Scholar] [CrossRef]
- Li, Y.; Zheng, R.; Li, S.; Cai, R.; Ni, F.; Zheng, H.; Hu, R.; Sun, T. Association between four anthropometric indexes and metabolic syndrome in US adults. Front. Endocrinol. 2022, 13, 889785. [Google Scholar] [CrossRef]
- Ramesh, N.; Kumar, P.; Sweta, S.; Prasad, A.; Tiwari, L.K. Correlation of anthropometric measurements with body mass index and estimation of the proportion of metabolic syndrome among overweight and obese children: A hospital-based cross-sectional study. BMJ Paediatr. Open 2024, 8, e002354. [Google Scholar] [CrossRef]
- Ross, R.; Neeland, I.J.; Yamashita, S.; Shai, I.; Seidell, J.; Magni, P.; Santos, R.D.; Arsenault, B.; Cuevas, A.; Hu, F.B. Waist circumference as a vital sign in clinical practice: A Consensus Statement from the IAS and ICCR Working Group on Visceral Obesity. Nat. Rev. Endocrinol. 2020, 16, 177–189. [Google Scholar] [CrossRef]
- Namazi, N.; Larijani, B.; Surkan, P.; Azadbakht, L. The association of neck circumference with risk of metabolic syndrome and its components in adults: A systematic review and meta-analysis. Nutr. Metab. Cardiovasc. Dis. 2018, 28, 657–674. [Google Scholar] [CrossRef]
- Onat, A.; Hergenç, G.; Yüksel, H.; Can, G.; Ayhan, E.; Kaya, Z.; Dursunoğlu, D. Neck circumference as a measure of central obesity: Associations with metabolic syndrome and obstructive sleep apnea syndrome beyond waist circumference. Clin. Nutr. 2009, 28, 46–51. [Google Scholar] [CrossRef]
- Yang, G.-R.; Yuan, S.-Y.; Fu, H.-J.; Wan, G.; Zhu, L.-X.; Bu, X.-L.; Zhang, J.-D.; Du, X.-P.; Li, Y.-L.; Ji, Y. Neck circumference positively related with central obesity, overweight, and metabolic syndrome in Chinese subjects with type 2 diabetes: Beijing Community Diabetes Study 4. Diabetes Care 2010, 33, 2465–2467. [Google Scholar] [CrossRef] [PubMed]
- Saneei, P.; Shahdadian, F.; Moradi, S.; Ghavami, A.; Mohammadi, H.; Rouhani, M.H. Neck circumference in relation to glycemic parameters: A systematic review and meta-analysis of observational studies. Diabetol. Metab. Syndr. 2019, 11, 1–16. [Google Scholar] [CrossRef]
- Cho, N.H.; Oh, T.J.; Kim, K.M.; Choi, S.H.; Lee, J.H.; Park, K.S.; Jang, H.C.; Kim, J.Y.; Lee, H.K.; Lim, S. Neck circumference and incidence of diabetes mellitus over 10 years in the Korean Genome and Epidemiology Study (KoGES). Sci. Rep. 2015, 5, 18565. [Google Scholar] [CrossRef]
- Wan, H.; Wang, Y.; Xiang, Q.; Fang, S.; Chen, Y.; Chen, C.; Zhang, W.; Zhang, H.; Xia, F.; Wang, N. Associations between abdominal obesity indices and diabetic complications: Chinese visceral adiposity index and neck circumference. Cardiovasc. Diabetol. 2020, 19, 1–12. [Google Scholar] [CrossRef]
- American Diabetes Association Professional Practice Committee. 6. Glycemic targets: Standards of medical care in diabetes—2022. Diabetes Care 2022, 45, S83–S96. [Google Scholar]
- American Diabetes Association Professional Practice Committee. 2. Diagnosis and Classification of Diabetes: Standards of Care in Diabetes—2025. Diabetes Care 2025, 48, S27–S49. [Google Scholar] [CrossRef] [PubMed]
- Deng, W.; Zhao, L.; Chen, C.; Ren, Z.; Jing, Y.; Qiu, J.; Liu, D. National burden and risk factors of diabetes mellitus in China from 1990 to 2021: Results from the Global Burden of Disease study 2021. J. Diabetes 2024, 16, e70012. [Google Scholar] [CrossRef]
- He, K.-J.; Wang, H.; Xu, J.; Gong, G.; Liu, X.; Guan, H. Global burden of type 2 diabetes mellitus from 1990 to 2021, with projections of prevalence to 2044: A systematic analysis across SDI levels for the global burden of disease study 2021. Front. Endocrinol. 2024, 15, 1501690. [Google Scholar] [CrossRef]
- Zheng, Y.; Ley, S.H.; Hu, F.B. Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat. Rev. Endocrinol. 2018, 14, 88–98. [Google Scholar] [CrossRef]
- Animaw, W.; Seyoum, Y. Increasing prevalence of diabetes mellitus in a developing country and its related factors. PLoS ONE 2017, 12, e0187670. [Google Scholar] [CrossRef]
- Nordwall, M.; Arnqvist, H.J.; Bojestig, M.; Ludvigsson, J. Good glycemic control remains crucial in prevention of late diabetic complications–the Linköping Diabetes Complications Study. Pediatr. Diabetes 2009, 10, 168–176. [Google Scholar] [CrossRef] [PubMed]
- Kanter, J.E.; Bornfeldt, K.E. Impact of diabetes mellitus. Arter. Thromb. Vasc. Biol. 2016, 36, 1049–1053. [Google Scholar] [CrossRef]
- Dal Canto, E.; Ceriello, A.; Rydén, L.; Ferrini, M.; Hansen, T.B.; Schnell, O.; Standl, E.; Beulens, J.W. Diabetes as a cardiovascular risk factor: An overview of global trends of macro and micro vascular complications. Eur. J. Prev. Cardiol. 2019, 26, 25–32. [Google Scholar] [CrossRef]
- Mishra, B.K.; Raghav, A.; Jeong, G.-B.; Jain, M.; Shukla, P.; Sharma, S. Estimation of HbA1c and Impact of Continuous Glucose Monitoring in Hypoglycemic States. Glucose Insul. Homeost. 2024, 63. [Google Scholar] [CrossRef]
- Jovanovic, L.; Peterson, C.M. The clinical utility of glycosylated hemoglobin. Am. J. Med. 1981, 70, 331–338. [Google Scholar] [CrossRef] [PubMed]
- Radin, M.S. Pitfalls in hemoglobin A1c measurement: When results may be misleading. J. Gen. Intern. Med. 2014, 29, 388–394. [Google Scholar] [CrossRef]
- Inoue, K.; Goto, A.; Kishimoto, M.; Tsujimoto, T.; Yamamoto-Honda, R.; Noto, H.; Kajio, H.; Terauchi, Y.; Noda, M. Possible discrepancy of HbA1c values and its assessment among patients with chronic renal failure, hemodialysis and other diseases. Clin. Exp. Nephrol. 2015, 19, 1179–1183. [Google Scholar] [CrossRef]
- Gram-Hansen, P.; Eriksen, J.; Mourits-Andersen, T.; Olesen, L. Glycosylated haemoglobin (HbA1c) in iron-and vitamin B12 deficiency. J. Intern. Med. 1990, 227, 133–136. [Google Scholar] [CrossRef]
- Alzahrani, B.A.; Salamatullah, H.K.; Alsharm, F.S.; Baljoon, J.M.; Abukhodair, A.O.; Ahmed, M.E.; Malaikah, H.; Radi, S. The effect of different types of anemia on HbA1c levels in non-diabetics. BMC Endocr. Disord. 2023, 23, 24. [Google Scholar] [CrossRef]
- Yoon, Y.; Kim, Y.-m.; Lee, S.; Shin, B.-C.; Kim, H.-L.; Chung, J.-H.; Son, M. Association between Neck Circumference and Chronic Kidney Disease in Korean Adults in the 2019–2021 Korea National Health and Nutrition Examination Survey. Nutrients 2023, 15, 5039. [Google Scholar] [CrossRef] [PubMed]
- Aswathappa, J.; Garg, S.; Kutty, K.; Shankar, V. Neck circumference as an anthropometric measure of obesity in diabetics. N. Am. J. Med. Sci. 2013, 5, 28. [Google Scholar] [CrossRef] [PubMed]
- Díaz, D.A.; Lera, L.; Márquez, C.; Valenzuela, A.; Saguez, R.; Weisstaub, G.; Albala, C. Neck Circumference Cut-Off Points for Identifying Adiposity: Association with Chronic Metabolic Diseases in Older People. J. Pers. Med. 2024, 14, 710. [Google Scholar] [CrossRef]
- Laurindo, L.F.; Cruz Camargo, F.; Perfeito, A.; Benedito Ciano, B.; Tainá Coelho, C.; Assis Apolinário, G.; do Nascimento Vicentin, I.; Cambui Andreasi, J.; Leme Boaro, B.; José Tofano, R. Exploring the Associations of Neck Circumference, Blood Pressure, CRP, and Insulin Resistance on the Visceral Adiposity Index: Insights from a Cross-Sectional Study. Endocrines 2024, 5, 538–546. [Google Scholar] [CrossRef]
- Kim, K.-Y.; Moon, H.-R.; Yun, J.-M. Neck circumference as a predictor of metabolic syndrome in koreans: A cross-sectional study. Nutrients 2021, 13, 3029. [Google Scholar] [CrossRef]
- Son, D.-H.; Han, J.H.; Lee, J.-H. Neck Circumference as a Predictor of Insulin Resistance in People with Non-alcoholic Fatty Liver Disease. J. Obes. Metab. Syndr. 2023, 32, 214. [Google Scholar] [CrossRef]
- Jensen, M.D. Role of body fat distribution and the metabolic complications of obesity. J. Clin. Endocrinol. Metab. 2008, 93, s57–s63. [Google Scholar] [CrossRef]
- Goodpaster, B.H.; Krishnaswami, S.; Harris, T.B.; Katsiaras, A.; Kritchevsky, S.B.; Simonsick, E.M.; Nevitt, M.; Holvoet, P.; Newman, A.B. Obesity, regional body fat distribution, and the metabolic syndrome in older men and women. Arch. Intern. Med. 2005, 165, 777–783. [Google Scholar] [CrossRef] [PubMed]
- Grundy, S.M.; Williams, C.; Vega, G.L. Upper body fat predicts metabolic syndrome similarly in men and women. Eur. J. Clin. Investig. 2018, 48, e12941. [Google Scholar] [CrossRef] [PubMed]
- Ahbab, S.; Ataoğlu, H.E.; Tuna, M.; Karasulu, L.; Çetin, F.; Temiz, L.Ü.; Yenigün, M. Neck circumference, metabolic syndrome and obstructive sleep apnea syndrome; evaluation of possible linkage. Med. Sci. Monit. 2013, 19, 111. [Google Scholar] [PubMed]
- Kim, S.E.; Park, B.S.; Park, S.H.; Shin, K.J.; Ha, S.Y.; Park, J.; Park, K.M. Predictors for presence and severity of obstructive sleep apnea in snoring patients: Significance of neck circumference. Sleep Med. 2015, 12, 34–38. [Google Scholar] [CrossRef]
| Variables | Non-DM (n = 8203) | DM (n = 2016) | ||||
|---|---|---|---|---|---|---|
| Study Population (n = 10,219) | Normal (n = 5181) | Hyperglycemic (n = 3022) | p-Value | Controlled (n = 1156) | Uncontrolled (n = 860) | p-Value |
| Sex (%) | ||||||
| Male | 1922 (37.1) | 1546 (51.2) | <0.01 | 601 (52.0) | 454 (52.8) | 0.72 |
| Female | 3259 (62.9) | 1476 (48.8) | 555 (48.0) | 406 (47.2) | ||
| Age (years) | 57.5 ± 11.7 | 60.0 ± 11.3 | <0.01 | 65.3 ± 10.4 | 63.5 ± 10.6 | <0.01 |
| Blood analysis | ||||||
| Hemoglobin (g/dL) | 13.6 ± 1.5 | 14.1 ± 1.5 | <0.01 | 13.8 ± 1.6 | 14.0 ± 1.6 | <0.01 |
| Glucose (mg/dL) | 91.8 ± 5.3 | 108.1 ± 14.0 | <0.01 | 119.9 ± 18.1 | 154.1 ± 44.1 | <0.01 |
| Hemoglobin A1c (%) | 5.6 ± 0.3 | 5.8 ± 0.4 | <0.01 | 6.4 ± 0.4 | 8.1 ± 1.3 | <0.01 |
| Total cholesterol (mg/dL) | 196.7 ± 37.3 | 196.6 ± 36.5 | 0.44 | 172.4 ± 41.6 | 171.6 ± 45.2 | 0.69 |
| HDL cholesterol (mg/dL) | 53.8 ± 13.1 | 50.4 ± 12.1 | <0.01 | 47.9 ± 11.5 | 46.0 ± 11.0 | <0.01 |
| Triglyceride (mg/dL) | 119.6 ± 86.2 | 151.6 ± 125.5 | <0.01 | 141.1 ± 98.9 | 173.0 ± 153.1 | <0.01 |
| eGFR | 89.3 ± 18.2 | 87.7 ± 17.8 | <0.01 | 83.6 ± 20.1 | 86.8 ± 22.0 | <0.01 |
| Blood pressure | ||||||
| Systolic blood pressure (SBP; mmHg) | 119.8 ± 16.9 | 125.2 ± 15.7 | <0.01 | 127.0 ± 16.4 | 126.9 ± 15.7 | 0.86 |
| Diastolic blood pressure (DBP; mmHg) | 75.5 ± 9.7 | 77.8 ± 9.8 | <0.01 | 74.6 ± 9.6 | 75.6 ± 10.3 | 0.03 |
| Body measurements | ||||||
| Body mass index (BMI; kg/m2) | 23.5 ± 3.1 | 24.8 ± 3.2 | <0.01 | 25.3 ± 3.5 | 25.6 ± 3.8 | 0.06 |
| Waist circumference (WC; cm) | 82.6 ± 9.3 | 87.3 ± 9.0 | <0.01 | 89.8 ± 9.3 | 91.1 ± 9.6 | <0.01 |
| Neck circumference (NC; cm) | 34.3 ± 3.1 | 35.7 ± 3.3 | <0.01 | 36.2 ± 3.3 | 36.6 ± 3.4 | <0.01 |
| Health interview (%) | ||||||
| Current smoker | 629 (12.1) | 441 (14.6) | <0.01 | 165 (14.3) | 175 (20.3) | <0.01 |
| Alcohol consumption | 1862 (35.9) | 1386 (45.9) | <0.01 | 420 (36.3) | 319 (37.1) | 0.72 |
| Regular exercise | 2079 (40.1) | 1152 (38.1) | 0.07 | 407 (35.2) | 310 (36.0) | 0.70 |
| Underlying diseases (%) | ||||||
| Hypertension (HTN) | 1637 (31.6) | 1431 (47.4) | <0.01 | 763 (66.0) | 498 (57.9) | <0.01 |
| Dyslipidemia | 2167 (41.8) | 1664 (55.1) | <0.01 | 801 (69.3) | 640 (74.4) | 0.02 |
| Chronic kidney disease (CKD) | 168 (3.2) | 152 (5.0) | <0.01 | 120 (10.4) | 77 (9.0) | 0.29 |
| Metabolic syndrome (MetS) | 622 (12.0) | 1537 (50.9) | <0.01 | 618 (53.5) | 574 (66.7) | <0.01 |
| Neck Circumference | Crude Model | Adjusted Model | ||||
|---|---|---|---|---|---|---|
| Model 1 a | Model 2 b | |||||
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | OR (95% CI) | p-Value | |
| Non-diabetic patients | 1.15 | <0.01 | 1.09 | <0.01 | 1.09 | <0.01 |
| (1.14–1.17) | (1.05–1.13) | (1.05–1.13) | ||||
| DM patients | 1.04 | <0.01 | 1.10 | <0.01 | 1.11 | <0.01 |
| (1.02–1.07) | (1.03–1.17) | (1.04–1.18) | ||||
| Neck Circumference | Crude Model | Adjusted Model | ||||
|---|---|---|---|---|---|---|
| Model 1 a | Model 2 b | |||||
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | OR (95% CI) | p-Value | |
| All subjects | 1.15 | <0.01 | 1.19 | <0.01 | 1.23 | <0.01 |
| (1.13–1.17) | (1.15–1.24) | (1.18–1.28) | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seo, H.; Yoon, W.; Kim, J.H.; Shin, B.C.; Kim, H.L.; Son, M.; Yoon, Y. Association Between Neck Circumference and Uncontrolled Hyperglycemia Diabetes in Korean Adults: From the Korea National Health and Nutrition Examination Survey, 2019 to 2021. Bioengineering 2025, 12, 1099. https://doi.org/10.3390/bioengineering12101099
Seo H, Yoon W, Kim JH, Shin BC, Kim HL, Son M, Yoon Y. Association Between Neck Circumference and Uncontrolled Hyperglycemia Diabetes in Korean Adults: From the Korea National Health and Nutrition Examination Survey, 2019 to 2021. Bioengineering. 2025; 12(10):1099. https://doi.org/10.3390/bioengineering12101099
Chicago/Turabian StyleSeo, Hyeonah, Wonju Yoon, Jae Ho Kim, Byung Chul Shin, Hyun Lee Kim, Minkook Son, and Youngmin Yoon. 2025. "Association Between Neck Circumference and Uncontrolled Hyperglycemia Diabetes in Korean Adults: From the Korea National Health and Nutrition Examination Survey, 2019 to 2021" Bioengineering 12, no. 10: 1099. https://doi.org/10.3390/bioengineering12101099
APA StyleSeo, H., Yoon, W., Kim, J. H., Shin, B. C., Kim, H. L., Son, M., & Yoon, Y. (2025). Association Between Neck Circumference and Uncontrolled Hyperglycemia Diabetes in Korean Adults: From the Korea National Health and Nutrition Examination Survey, 2019 to 2021. Bioengineering, 12(10), 1099. https://doi.org/10.3390/bioengineering12101099






