Effects of Backward Walking on External Knee Adduction Moment and Knee Adduction Angular Impulse in Individuals with Medial Knee Osteoarthritis
Abstract
1. Introduction
2. Methods
2.1. Participants
2.2. Ethics Statement
2.3. Data Collection
2.4. Data Processing
2.5. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sharma, L. Osteoarthritis of the Knee. N. Engl. J. Med. 2021, 384, 51–59. [Google Scholar] [CrossRef]
- Li, D.; Li, S.; Chen, Q.; Xie, X. The Prevalence of Symptomatic Knee Osteoarthritis in Relation to Age, Sex, Area, Region, and Body Mass Index in China: A Systematic Review and Meta-Analysis. Front. Med. 2020, 7, 304. [Google Scholar] [CrossRef]
- Schuring, N.; Aoki, H.; Gray, J.; Kerkhoffs, G.M.M.J.; Lambert, M.; Gouttebarge, V. Osteoarthritis Is Associated with Symptoms of Common Mental Disorders among Former Elite Athletes. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 3179–3185. [Google Scholar] [CrossRef]
- Robbins, S.M.; Birmingham, T.B.; Callaghan, J.P.; Jones, G.R.; Chesworth, B.M.; Maly, M.R. Association of Pain with Frequency and Magnitude of Knee Loading in Knee Osteoarthritis. Arthritis Care Res. 2011, 63, 991–997. [Google Scholar] [CrossRef]
- Hall, M.; Bennell, K.L.; Wrigley, T.V.; Metcalf, B.R.; Campbell, P.K.; Kasza, J.; Paterson, K.L.; Hunter, D.J.; Hinman, R.S. The Knee Adduction Moment and Knee Osteoarthritis Symptoms: Relationships According to Radiographic Disease Severity. Osteoarthr. Cartil. 2017, 25, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Trepczynski, A.; Kutzner, I.; Bergmann, G.; Taylor, W.R.; Heller, M.O. Modulation of the Relationship between External Knee Adduction Moments and Medial Joint Contact Forces across Subjects and Activities. Arthritis Rheumatol. 2014, 66, 1218–1227. [Google Scholar] [CrossRef] [PubMed]
- Brisson, N.M.; Gatti, A.A.; Damm, P.; Duda, G.N.; Maly, M.R. Association of Machine Learning-Based Predictions of Medial Knee Contact Force with Cartilage Loss over 2.5 Years in Knee Osteoarthritis. Arthritis Rheumatol. 2021, 73, 1638–1645. [Google Scholar] [CrossRef]
- Kutzner, I.; Trepczynski, A.; Heller, M.O.; Bergmann, G. Knee Adduction Moment and Medial Contact Force—Facts about Their Correlation during Gait. PLoS ONE 2013, 8, e81036. [Google Scholar] [CrossRef] [PubMed]
- Manal, K.; Gardinier, E.; Buchanan, T.S.; Snyder-Mackler, L. A More Informed Evaluation of Medial Compartment Loading: The Combined Use of the Knee Adduction and Flexor Moments. Osteoarthr. Cartil. 2015, 23, 1107–1111. [Google Scholar] [CrossRef]
- Miyazaki, T.; Wada, M.; Kawahara, H.; Sato, M.; Baba, H.; Shimada, S. Dynamic Load at Baseline Can Predict Radiographic Disease Progression in Medial Compartment Knee Osteoarthritis. Ann. Rheum. Dis. 2002, 61, 617–622. [Google Scholar] [CrossRef]
- Sharma, L.; Hurwitz, D.E.; Thonar, E.J.; Sum, J.A.; Lenz, M.E.; Dunlop, D.D.; Schnitzer, T.J.; Kirwan-Mellis, G.; Andriacchi, T.P. Knee Adduction Moment, Serum Hyaluronan Level, and Disease Severity in Medial Tibiofemoral Osteoarthritis. Arthritis Rheum. 1998, 41, 1233–1240. [Google Scholar] [CrossRef]
- Ferreira, V.; Simões, R.; Gonçalves, R.S.; Machado, L.; Roriz, P. The Optimal Degree of Lateral Wedge Insoles for Reducing Knee Joint Load: A Systematic Review and Meta-Analysis. Arch. Physiother. 2019, 9, 18. [Google Scholar] [CrossRef]
- Silva, M.D.C.; Perriman, D.M.; Fearon, A.M.; Tait, D.; Spencer, T.J.; Walton-Sonda, D.; Simic, M.; Hinman, R.S.; Bennell, K.L.; Scarvell, J.M. Effects of Neuromuscular Gait Modification Strategies on Indicators of Knee Joint Load in People with Medial Knee Osteoarthritis: A Systematic Review and Meta-Analysis. PLoS ONE 2022, 17, e0274874. [Google Scholar] [CrossRef]
- Walter, J.P.; D’Lima, D.D.; Colwell, C.W., Jr.; Fregly, B.J. Decreased Knee Adduction Moment Does Not Guarantee Decreased Medial Contact Force during Gait. J. Orthop. Res. 2010, 28, 1348–1354. [Google Scholar] [CrossRef] [PubMed]
- Thorp, L.E.; Sumner, D.R.; Block, J.A.; Moisio, K.C.; Shott, S.; Wimmer, M.A. Knee Joint Loading Differs in Individuals with Mild Compared with Moderate Medial Knee Osteoarthritis. Arthritis Rheum. 2006, 54, 3842–3849. [Google Scholar] [CrossRef] [PubMed]
- Kito, N.; Shinkoda, K.; Yamasaki, T.; Kanemura, N.; Anan, M.; Okanishi, N.; Ozawa, J.; Moriyama, H. Contribution of Knee Adduction Moment Impulse to Pain and Disability in Japanese Women with Medial Knee Osteoarthritis. Clin. Biomech. 2010, 25, 914–919. [Google Scholar] [CrossRef]
- Alghadir, A.H.; Anwer, S.; Sarkar, B.; Paul, A.K.; Anwar, D. Effect of 6-Week Retro or Forward Walking Program on Pain, Functional Disability, Quadriceps Muscle Strength, and Performance in Individuals with Knee Osteoarthritis: A Randomized Controlled Trial (Retro-Walking Trial). BMC Musculoskelet. Disord. 2019, 20, 159. [Google Scholar] [CrossRef]
- Castro, R.Q.; Oliveira, J.V.V.; Veras, P.M.; Correa, C.P.S.; Peixoto, J.G.; Fonseca, D.S. Effect of Gait Retraining Strategies on Clinical and Biomechanical Outcomes in Subjects with Knee Osteoarthritis: A Systematic Review with Meta-Analysis and GRADE Recommendations. Disabil. Rehabil. 2025; online ahead of print. [Google Scholar] [CrossRef]
- Gondhalekar, G.A.; Deo, M.V. Retrowalking as an Adjunct to Conventional Treatment versus Conventional Treatment Alone on Pain and Disability in Patients with Acute Exacerbation of Chronic Knee Osteoarthritis: A Randomized Clinical Trial. N. Am. J. Med. Sci. 2013, 5, 108–112. [Google Scholar] [CrossRef] [PubMed]
- Goonasegaran, A.R.; Suhaimi, A.; Mokhtar, A.H. A Randomized Control Trial on Retro-Walking Improves Symptoms, Pain, and Function in Primary Knee Osteoarthritis. J. Sports Med. Phys. Fitness. 2022, 62, 229–237. [Google Scholar] [CrossRef]
- Zhang, M.; Pang, J.; Lu, J.; Kang, M.; Chen, B.; Jones, R.K.; Liu, A. The Immediate Effect of Backward Walking on External Knee Adduction Moment in Healthy Individuals. J. Healthc. Eng. 2022, 2022, 4232990. [Google Scholar] [CrossRef]
- Amin, S.; Luepongsak, N.; McGibbon, C.A.; LaValley, M.P.; Krebs, D.E.; Felson, D.T. Knee Adduction Moment and Development of Chronic Knee Pain in Elders. Arthritis Rheum. 2004, 51, 371–376. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.; Kim, J.; Son, J.; Kim, Y. Kinematic and Kinetic Analysis during Forward and Backward Walking. Gait Posture 2013, 38, 674–678. [Google Scholar] [CrossRef] [PubMed]
- Gerbrands, T.A.; Pisters, M.F.; Theeven, P.J.R.; Verschueren, S.; Vanwanseele, B. Lateral Trunk Lean and Medializing the Knee as Gait Strategies for Knee Osteoarthritis. Gait Posture 2017, 51, 247–253. [Google Scholar] [CrossRef]
- Kellgren, J.H.; Lawrence, J.S. Radiological Assessment of Osteo-Arthrosis. Ann. Rheum. Dis. 1957, 16, 494–502. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef]
- Cappozzo, A.; Catani, F.; Croce, U.D.; Leardini, A. Position and Orientation in Space of Bones during Movement: Anatomical Frame Definition and Determination. Clin. Biomech. 1995, 10, 171–178. [Google Scholar] [CrossRef]
- Jones, R.K.; Zhang, M.; Laxton, P.; Findlow, A.H.; Liu, A. The Biomechanical Effects of a New Design of Lateral Wedge Insole on the Knee and Ankle during Walking. Hum. Mov. Sci. 2013, 32, 596–604. [Google Scholar] [CrossRef]
- Sawada, T.; Tanimoto, K.; Tokuda, K.; Iwamoto, Y.; Ogata, Y.; Anan, M.; Takahashi, M.; Kito, N.; Shinkoda, K. Rear Foot Kinematics When Wearing Lateral Wedge Insoles and Foot Alignment Influence the Effect of Knee Adduction Moment for Medial Knee Osteoarthritis. Gait Posture 2017, 57, 177–181. [Google Scholar] [CrossRef]
- Shull, P.B.; Shultz, R.; Silder, A.; Dragoo, J.L.; Besier, T.F.; Cutkosky, M.R.; Delp, S.L. Toe-In Gait Reduces the First Peak Knee Adduction Moment in Patients with Medial Compartment Knee Osteoarthritis. J. Biomech. 2013, 46, 122–128. [Google Scholar] [CrossRef]
- Robbins, S.M.; Maly, M.R. The Effect of Gait Speed on the Knee Adduction Moment Depends on Waveform Summary Measures. Gait Posture 2009, 30, 543–546. [Google Scholar] [CrossRef] [PubMed]
- Fukuchi, C.A.; Fukuchi, R.K.; Duarte, M. Effects of Walking Speed on Gait Biomechanics in Healthy Participants: A Systematic Review and Meta-Analysis. Syst. Rev. 2019, 8, 153. [Google Scholar] [CrossRef]
- Tang, S.F.; Chen, C.P.; Chen, M.J.; Pei, Y.C.; Lau, Y.C.; Leong, C.P. Changes in Sagittal Ground Reaction Forces after Intra-Articular Hyaluronate Injections for Knee Osteoarthritis. Arch. Phys. Med. Rehabil. 2004, 85, 951–955. [Google Scholar] [CrossRef]
- Goh, J.C.; Bose, K.; Khoo, B.C. Gait Analysis Study on Patients with Varus Osteoarthrosis of the Knee. Clin. Orthop. Relat. Res. 1993, 294, 223–231. [Google Scholar]
- Mundermann, A.; Dyrby, C.O.; Hurwitz, D.E.; Sharma, L.; Andriacchi, T.P. Potential Strategies to Reduce Medial Compartment Loading in Patients with Knee Osteoarthritis of Varying Severity: Reduced Walking Speed. Arthritis Rheum. 2004, 50, 1172–1178. [Google Scholar] [CrossRef]
- Donno, L.; Monoli, C.; Frigo, C.A.; Galli, M. Forward and Backward Walking: Multifactorial Characterization of Gait Parameters. Sensors 2023, 23, 4671. [Google Scholar] [CrossRef] [PubMed]
- Kawaji, H.; Kojima, S. Effect of Altered Sagittal-Plane Knee Kinematics on Loading during the Early Stance Phase of Gait. Gait Posture 2019, 74, 108–113. [Google Scholar] [CrossRef]
- Wang, S.; Chan, P.P.K.; Lam, B.M.F.; Chan, Z.Y.S.; Zhang, J.H.W.; Wang, C.; Lam, W.K.; Ho, K.K.W.; Chan, R.H.M.; Cheung, R.T.H. Sensor-Based Gait Retraining Lowers Knee Adduction Moment and Improves Symptoms in Patients with Knee Osteoarthritis: A Randomized Controlled Trial. Sensors 2021, 21, 5596. [Google Scholar] [CrossRef] [PubMed]
- Chehab, E.F.; Favre, J.; Erhart-Hledik, J.C.; Andriacchi, T.P. Baseline Knee Adduction and Flexion Moments during Walking Are Both Associated with 5-Year Cartilage Changes in Patients with Medial Knee Osteoarthritis. Osteoarthr. Cartil. 2014, 22, 1833–1839. [Google Scholar] [CrossRef] [PubMed]
- Chang, A.H.; Moisio, K.C.; Chmiel, J.S.; Eckstein, F.; Guermazi, A.; Prasad, P.V.; Zhang, Y.; Almagor, O.; Belisle, L.; Hayes, K.; et al. External Knee Adduction and Flexion Moments during Gait and Medial Tibiofemoral Disease Progression in Knee Osteoarthritis. Osteoarthr. Cartil. 2015, 23, 1099–1106. [Google Scholar] [CrossRef]
- DelMastro, H.M.; Ruiz, J.A.; Simaitis, L.B.; Gromisch, E.S.; Neto, L.O.; Cohen, E.T.; Wong, E.; Krug, R.J.; Lo, A.C. Effect of Backward and Forward Walking on Lower Limb Strength, Balance, and Gait in Multiple Sclerosis: A Randomized Feasibility Trial. Int. J. MS Care 2023, 25, 45–50. [Google Scholar] [CrossRef]
- Al-Khlaifat, L.; Herrington, L.C.; Hammond, A.; Tyson, S.F.; Jones, R.K. The Effectiveness of an Exercise Programme on Knee Loading, Muscle Co-Contraction, and Pain in Patients with Medial Knee Osteoarthritis: A Pilot Study. Knee 2016, 23, 63–69. [Google Scholar] [CrossRef] [PubMed]
- Hodges, P.W.; van den Hoorn, W.; Wrigley, T.V.; Hinman, R.S.; Bowles, K.A.; Cicuttini, F.; Wang, Y.; Bennell, K. Increased Duration of Co-Contraction of Medial Knee Muscles Is Associated with Greater Progression of Knee Osteoarthritis. Man. Ther. 2016, 21, 151–158. [Google Scholar] [CrossRef] [PubMed]
- Sims, E.L.; Carland, J.M.; Keefe, F.J.; Kraus, V.B.; Guilak, F.; Schmitt, D. Sex differences in biomechanics associated with knee osteoarthritis. J. Women Aging 2009, 21, 159–170. [Google Scholar] [CrossRef] [PubMed]
- Kobsar, D.; Barden, J.M.; Clermont, C.; Wilson, J.L.A.; Ferber, R. Sex differences in the regularity and symmetry of gait in older adults with and without knee osteoarthritis. Gait Posture 2022, 95, 192–197. [Google Scholar] [CrossRef]
| Variable | Definition |
|---|---|
| 1st EKAM (Nm/kg) | The peak of EKAM in the 1st half of the stance (from 1 to 33%). |
| 2nd EKAM (Nm/kg) | The peak of EKAM in the 2nd half of the stance (from 68 to 100%). |
| 1st EKAM arm (m) | The perpendicular distance between the GRF and knee joint center in the laboratory frontal plane, calculated at the time of 1st peak of EKAM. |
| 2nd EKAM arm (m) | The perpendicular distance between the GRF and knee joint center in the laboratory frontal plane, calculated at the time of 2nd peak of EKAM. |
| KAAI (Nm/kg) · s | The positive area under the EKAM–time graph. |
| 1st EKFM (Nm/kg) | The peak of EKFM in the 1st half of the stance (from 0 to 50%). |
| 1st GRFz (body weight) | The peak of vertical GRF in the 1st half of the stance (from 0 to 50%). |
| 2nd GRFz (body weight) | The peak of vertical GRF in the 2nd half of the stance (from 51 to 100%). |
| ESGRFx (body weight) | The peak of medial GRF in the 1st half of the stance (from 0 to 50%). |
| LSGRFx (body weight) | The peak of medial GRF in the 2nd half of the stance (from 51 to 100%). |
| Variable | |
|---|---|
| Gender (male/female) | 3/29 |
| Age (years) | 60.56 ± 4.93 |
| Height (m) | 1.59 ± 0.06 |
| Body mass (kg) | 58.20 ± 5.73 |
| Body mass index (kg/m2) | 23.17 ± 2.41 |
| Kellgren & Lawrence grade of knee OA | grade 1 = 12, grade 2 = 15, grade 3 = 5 |
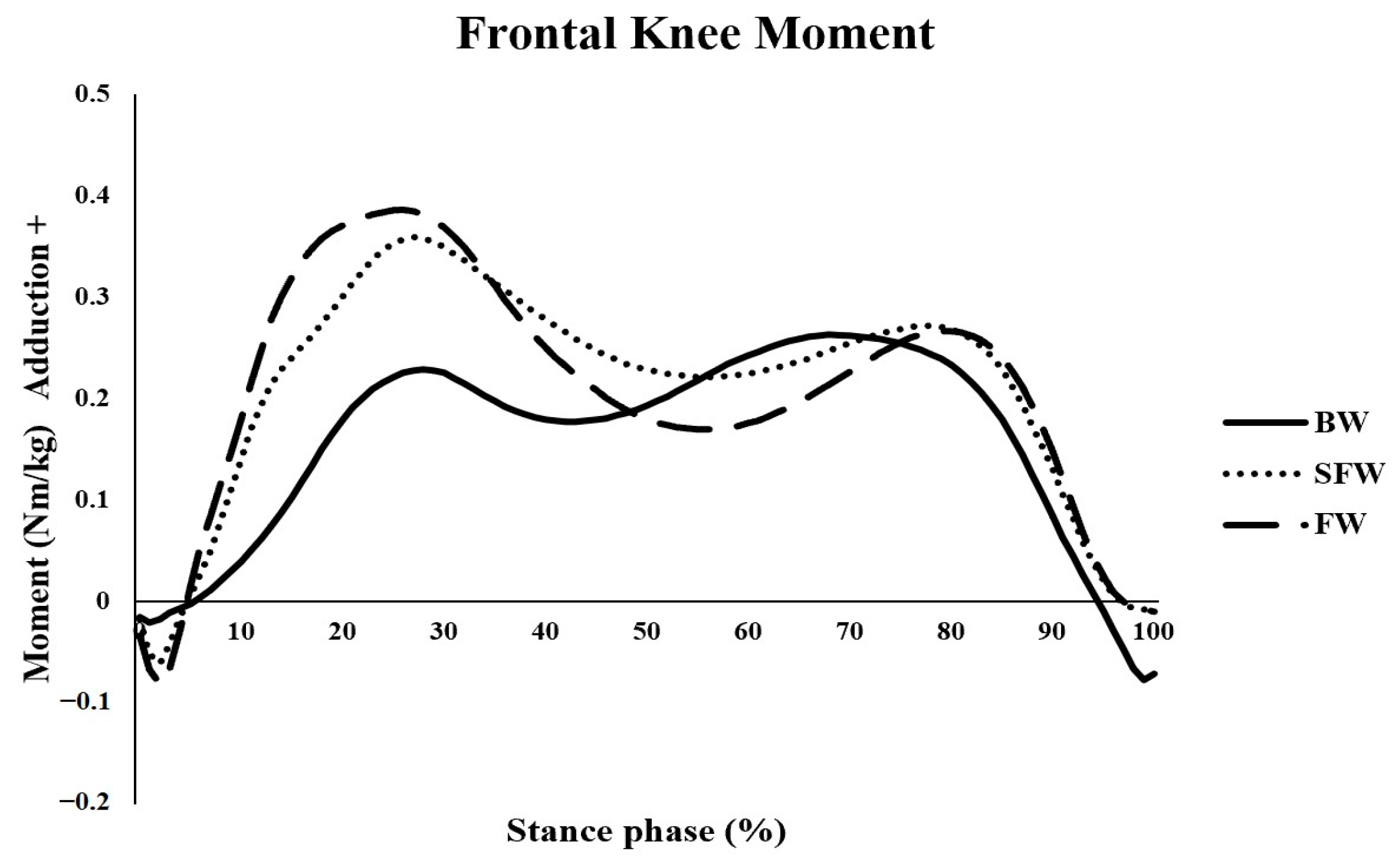
| Variable | BW | FW | SCFW | p Value | ||
|---|---|---|---|---|---|---|
| Main Effect | BW vs. FW | BW vs. SCFW | ||||
| Walking speed (m/s) | 0.87 ± 0.12 | 1.12 ± 0.12 | 0.86 ± 0.11 | <0.001 | <0.001 | 1.000 |
| 1st EKAM (Nm/kg) | 0.26 ± 0.12 | 0.39 ± 0.09 | 0.36 ± 0.09 | <0.001 | <0.001 | <0.001 |
| 2nd EKAM (Nm/kg) | 0.28 ± 0.09 | 0.27 ± 0.10 | 0.28 ± 0.11 | 0.785 | 0.700 | 1.000 |
| 1st EKAM arm (m) | 0.04 ± 0.02 | 0.07 ± 0.02 | 0.06 ± 0.02 | <0.001 | <0.001 | <0.001 |
| 2nd EKAM arm (m) | 0.05 ± 0.02 | 0.05 ± 0.02 | 0.05 ± 0.02 | 0.446 | 0.179 | 0.166 |
| KAAI (Nm/kg) · s | 0.12 ± 0.05 | 0.13 ± 0.05 | 0.16 ± 0.05 | <0.001 | <0.001 | <0.001 |
| 1st EKFM (Nm/kg) | 0.31 ± 0.17 | 0.38 ± 0.18 | 0.18 ± 0.15 | <0.001 | <0.001 | <0.001 |
| 1st GRFz (body weight) | 1.13 ± 0.10 | 1.06 ± 0.09 | 1.00 ± 0.06 | <0.001 | <0.001 | <0.001 |
| 2nd GRFz (body weight) | 0.98 ± 0.08 | 1.09 ± 0.07 | 1.08 ± 0.06 | <0.001 | <0.001 | <0.001 |
| ESGRFx (body weight) | −0.08 ± 0.02 | 0.06 ± 0.01 | 0.05 ± 0.01 | <0.001 | <0.001 | <0.001 |
| LSGRFx (body weight) | −0.06 ± 0.01 | 0.05 ± 0.02 | 0.05 ± 0.02 | <0.001 | <0.001 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, M.; Wang, S.; Lu, J.; Pang, J.; Wang, P.; Chen, B.; Zhan, H. Effects of Backward Walking on External Knee Adduction Moment and Knee Adduction Angular Impulse in Individuals with Medial Knee Osteoarthritis. Bioengineering 2025, 12, 1057. https://doi.org/10.3390/bioengineering12101057
Zhang M, Wang S, Lu J, Pang J, Wang P, Chen B, Zhan H. Effects of Backward Walking on External Knee Adduction Moment and Knee Adduction Angular Impulse in Individuals with Medial Knee Osteoarthritis. Bioengineering. 2025; 12(10):1057. https://doi.org/10.3390/bioengineering12101057
Chicago/Turabian StyleZhang, Min, Sizhong Wang, Jiehang Lu, Jian Pang, Peige Wang, Bo Chen, and Hongsheng Zhan. 2025. "Effects of Backward Walking on External Knee Adduction Moment and Knee Adduction Angular Impulse in Individuals with Medial Knee Osteoarthritis" Bioengineering 12, no. 10: 1057. https://doi.org/10.3390/bioengineering12101057
APA StyleZhang, M., Wang, S., Lu, J., Pang, J., Wang, P., Chen, B., & Zhan, H. (2025). Effects of Backward Walking on External Knee Adduction Moment and Knee Adduction Angular Impulse in Individuals with Medial Knee Osteoarthritis. Bioengineering, 12(10), 1057. https://doi.org/10.3390/bioengineering12101057





