Verification of the Effectiveness of a Token Economy Method Through Digital Intervention Content for Children with Attention-Deficit/Hyperactivity Disorder
Abstract
1. Introduction
2. Materials and Methods
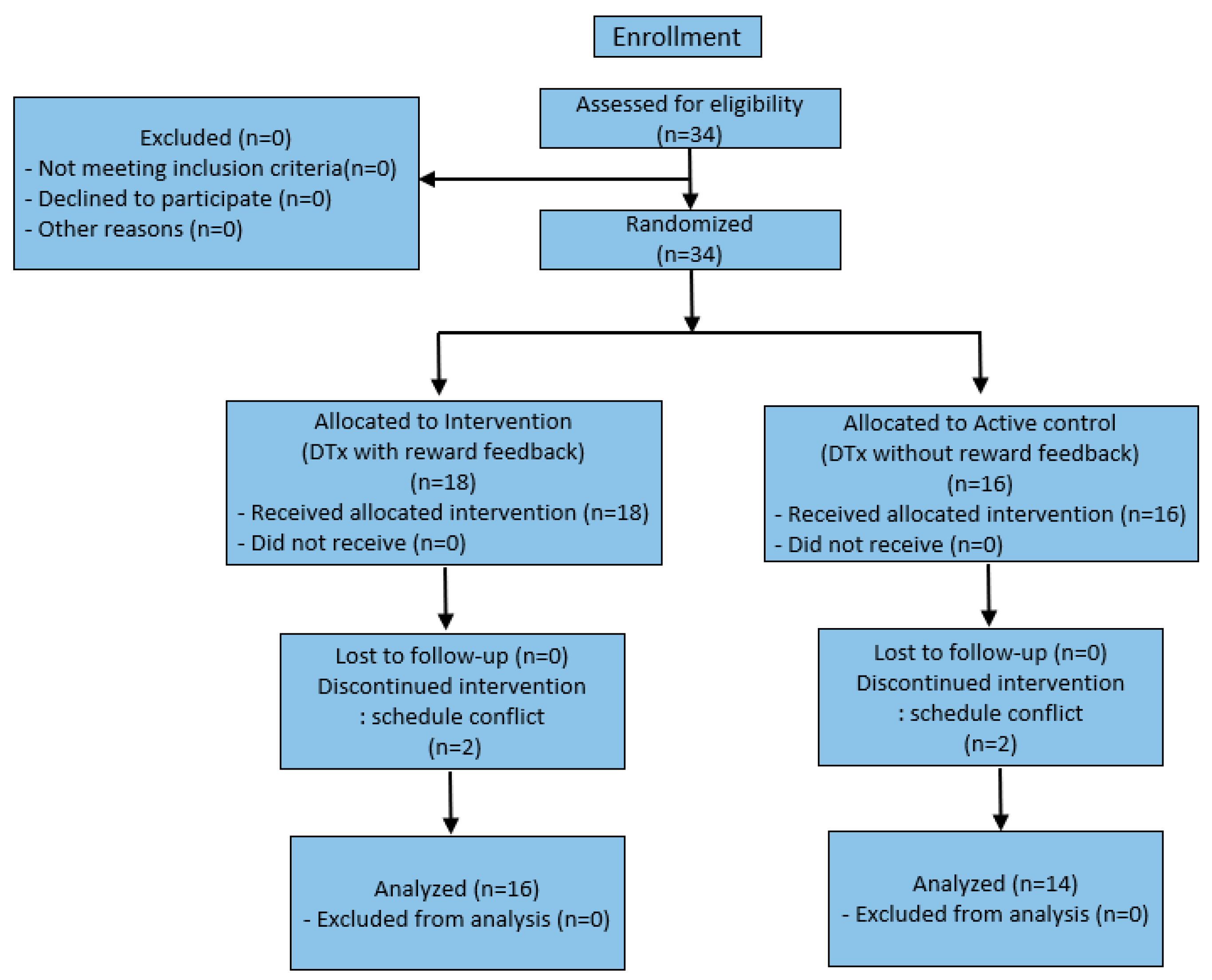
2.1. Study Participants
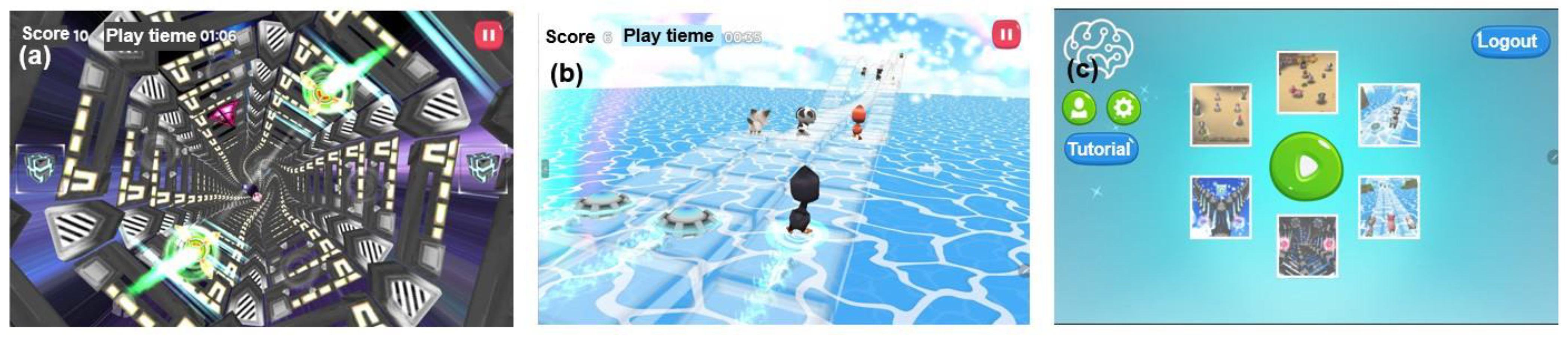
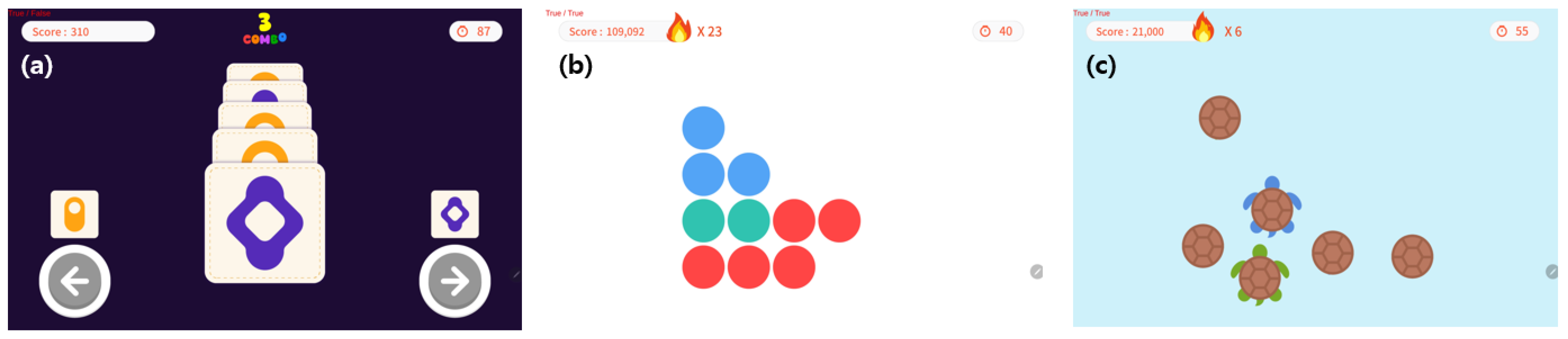
2.2. Implementation of Reward Feedback Content
2.3. Experimental Methods
2.4. Evaluation Tool
2.4.1. Korean Version of the Child Behavior Checklist (K-CBCL)
2.4.2. Comprehension Attention Test (CAT)
2.5. Analysis Methods
3. Results
3.1. Characteristics of the Study Participants
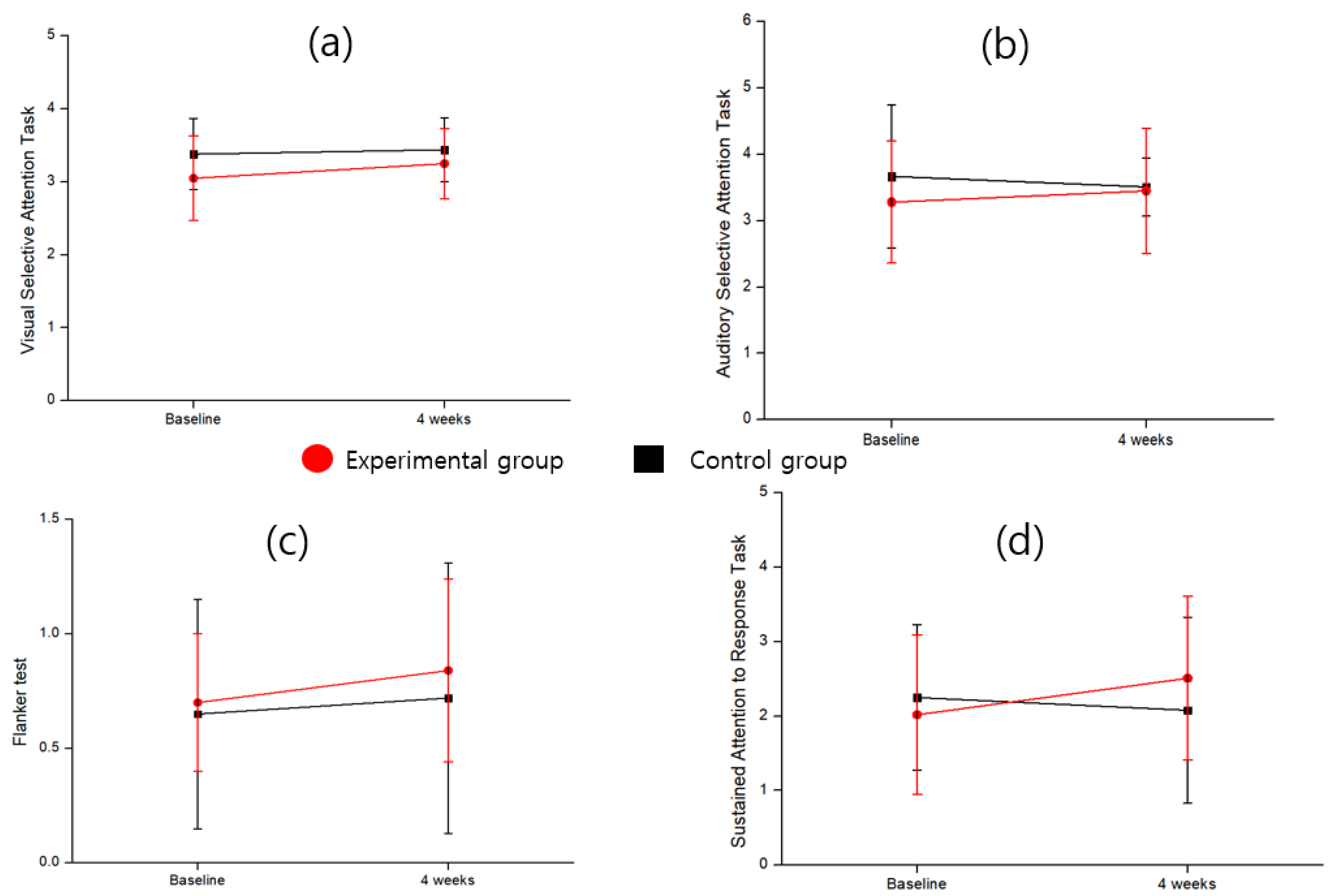
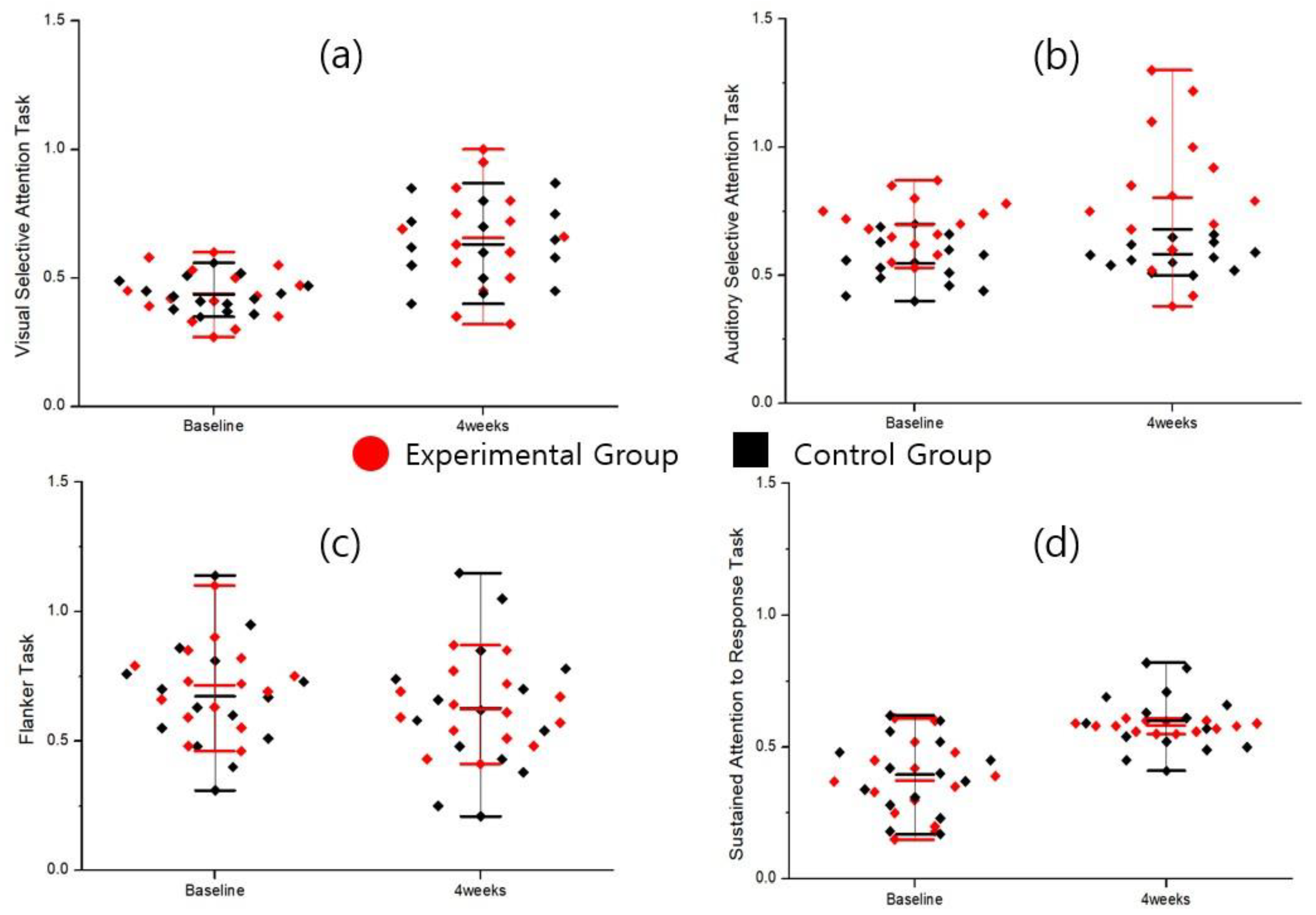
3.2. Results of the CAT Analysis
3.3. Results of the K-CBCL Analysis
4. Discussion
5. Conclusions
- In the CAT sensitivity factor, the flanker task showed that after controlling for baseline scores, the experimental group (0.84 ± 0.40) scored significantly higher than the control group (0.72 ± 0.59), with a large effect size (F = 4.76, p = 0.038, partial η2 = 0.150). In the sustained attention to response task, after controlling for baseline scores, the experimental group (2.51 ± 1.10) also demonstrated significantly higher sensitivity indices than the control group (2.08 ± 1.25) (F = 6.01, p = 0.021, partial η2 = 0.182). Additionally, analysis of the rate of change indicated that the experimental group (24.26 ± 48.06) showed significantly greater improvement than the control group (–7.56 ± 45.61), with statistical significance (t = 2.13, p = 0.028) and a large effect size (Cohen’s d = 0.848).
- In the response style index, the auditory selective attention task revealed that after controlling for baseline scores, the experimental group scored significantly higher than the control group after 4 weeks (F = 4.26, p = 0.044, partial η2 = 0.136). The rate of change was also greater in the experimental group (17.39%) than in the control group (9.09%), with a medium-to-large effect size (Cohen’s d = 0.780). In the flanker task, the experimental group showed significantly lower scores than the control group (F = 4.66, p = 0.040, partial η2 = 0.147), indicating reduced bias between impulsive and overly cautious responses. Moreover, the proportion of symptom improvement was significantly higher in the experimental group than in the control group (χ2 = 6.6, p = 0.037), indicating overall clinical improvement.
- In the K-CBCL, the analysis of externalizing scores showed a significant difference between the groups at 4 weeks after controlling for baseline scores (F = 4.56, p = 0.042). This difference explained approximately 14.4% of the variance in externalizing scores, indicating a clinically large effect size (partial η2 = 0.144). Furthermore, the rate of change analysis revealed a significant difference between the groups (t = 2.35, p = 0.026, Cohen’s d = 0.860), demonstrating that the experimental group achieved greater improvement in externalizing symptoms than the control group.
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ADHD | Attention-Deficit/Hyperactivity Disorder |
| CAT | Comprehensive Attention Test |
| K-CBCL | Korean version of the Child Behavior Checklist |
| DTx | Digital Therapeutics |
| K-WISC-V | Korean Wechsler Intelligence Scale for Children–Fifth Edition |
| ANCOVA | Analysis of Covariance |
| IRB | Institutional Review Board |
| CRIS | Clinical Research Information Service |
References
- Schippers, L.M.; Greven, C.U.; Hoogman, M. Associations between ADHD traits and self-reported strengths in the general population. Compr. Psychiatry 2024, 130, 152461. [Google Scholar] [CrossRef]
- Berchiatti, M.; Ferrer, A.; Badenes-Ribera, L.; Longobardi, C. School adjustments in children with attention deficit hyperactivity disorder (ADHD): Peer relationships, the quality of the student-teacher relationship, and children’s academic and behavioral competencies. J. Appl. Sch. Psychol. 2022, 38, 241–261. [Google Scholar] [CrossRef]
- Choi, W.S.; Wang, S.M.; Woo, Y.S.; Bahk, W.M. Therapeutic Efficacy and Safety of Memantine for Children and Adults with ADHD with a Focus on Glutamate-Dopamine Regulation: A Systematic Review. J. Clin. Psychiatry 2024, 86, 58158. [Google Scholar] [CrossRef]
- Johnson, M.; Johnels, J.Å.; Östlund, S.; Cedergren, K.; Omanovic, Z.; Hjalmarsson, K.; Jakobsson, K.; Högstedt, J.; Bilstedt, E. Long-term medication for ADHD and development of cognitive functions in children and adolescents. J. Psychiatr. Res. 2021, 142, 204–209. [Google Scholar] [CrossRef]
- Ning, K.; Wang, T.Z. Multimodal interventions are more effective in improving core symptoms in children with ADHD. Front. Psychiatry 2021, 12, 759315. [Google Scholar] [CrossRef]
- Ojinna, B.T.; Parisapogu, A.; Sherpa, M.L.; Choday, S.; Ravi, N.; Giva, S.; Kumar, V.S.; Shrestha, N.; Tran, H.H.V.; Penumetcha, S.S. Efficacy of Cognitive Behavioral Therapy and Methylphenidate in the Treatment of Attention Deficit Hyperactivity Disorder in Children and Adolescents: A Systematic Review. Cureus 2022, 14, e32647. [Google Scholar] [CrossRef] [PubMed]
- Thorell, L.B.; Buren, J.; Ström Wiman, J.; Sandberg, D.; Nutley, S.B. Longitudinal associations between digital media use and ADHD symptoms in children and adolescents: A systematic literature review. Eur. Child Adolesc. Psychiatry 2024, 33, 2503–2526. [Google Scholar] [CrossRef] [PubMed]
- Lutz, J.; Offidani, E.; Taraboanta, L.; Lakhan, S.E.; Campellone, T.R. Appropriate controls for digital therapeutic clinical trials: A narrative review of control conditions in clinical trials of digital therapeutics (DTx) deploying psychosocial, cognitive, or behavioral content. Front. Digit. Health 2022, 4, 823977. [Google Scholar] [CrossRef] [PubMed]
- Huang, S.; Zhang, T.; Lu, Q.; Xiong, X.; Liu, Z.; Sun, D. Clinical study on the intervention effect of digital therapy on children with attention deficit hyperactivity disorder (ADHD). Sci. Rep. 2024, 14, 23733. [Google Scholar] [CrossRef]
- Oh, S.; Choi, J.; Han, D.H.; Kim, E. Effects of game-based digital therapeutics on attention deficit hyperactivity disorder in children and adolescents as assessed by parents or teachers: A systematic review and meta-analysis. Eur. Child Adolesc. Psychiatry 2024, 33, 481–493. [Google Scholar] [CrossRef]
- Jiang, H.; Natarajan, R.; Shuy, Y.K.; Rong, L.; Zhang, M.W.; Vallabhajosyula, R. The use of mobile games in the management of patients with attention deficit hyperactive disorder: A scoping review. Front. Psychiatry 2022, 13, 792402. [Google Scholar] [CrossRef]
- Lee, H.J.; Jeong, Y.J.; Kim, J.S.; Kim, S.J.; Jo, U.; Jun, S.J.; Lim, J.; Park, Y.J.; Lee, M.; Kim, D.; et al. Current Status and Future Directions in the Development of Digital Therapeutic Interventions for Neurodevelopmental Disorders. Clin. Pharmacol. Ther. 2025, 117, 1632–1636. [Google Scholar] [CrossRef] [PubMed]
- Rodrigo-Yanguas, M.; Martín-Moratinos, M.; González-Tardón, C.; Sanchez-Sanchez, F.; Royuela, A.; Bella-Fernández, M.; Blasco-Fontecilla, H. Effectiveness of a personalized, chess-based training serious video game in the treatment of adolescents and young adults with attention-deficit/hyperactivity disorder: Randomized controlled trial. JMIR Serious Games 2023, 11, e39874. [Google Scholar] [CrossRef]
- Choi, E.; Yoon, E.H.; Park, M.H. Game-based digital therapeutics for children and adolescents: Their therapeutic effects on mental health problems, the sustainability of the therapeutic effects and the transfer of cognitive functions. Front. Psychiatry 2022, 13, 986687. [Google Scholar] [CrossRef]
- Visser, L.; Röschinger, J.; Barck, K.; Büttner, G.; Hasselhorn, M. Learning Difficulties in Children with Symptoms of DCD and/or ADHD: Analyses from a Categorical and a Continuous Approach. Int. J. Disability. Dev. Educ. 2022, 69, 1505–1521. [Google Scholar] [CrossRef]
- Norkhalisah, N.; Mirnawati, M.; Adhim, F. Efektivitas Teknik Token Ekonomi untuk Meningkatkan Konsentrasi Belajar Anak ADHD. J. Disabil. Stud. Educ. Sport 2024, 1, 10–18. [Google Scholar]
- Fang, H.; Fang, C.; Che, Y.; Peng, X.; Zhang, X.; Lin, D. Reward Feedback Mechanism in Virtual Reality Serious Games in Interventions for Children With Attention Deficits: Pre-and Posttest Experimental Control Group Study. JMIR Serious Games 2025, 13, e67338. Available online: https://games.jmir.org/2025/1/e67338 (accessed on 27 June 2025). [CrossRef]
- Azizah, R.N.; Anjarwati, E.; Prabowo, K.M.; Hamidah, H. Buddy sebagai Digital Psychological Intervention berbasis token ekonomi bagi individu dengan ADHD. Prod. J. Desain Prod. (Pengetah. Dan Peranc. Prod.) 2024, 7, 21–28. [Google Scholar] [CrossRef]
- Sari, N. Token Economy Intervention for Early Childhood Children with Attention Deficit and Hyperactivity Disorder. Educ. Psychol. J. 2024, 13, 12–18. Available online: http://journal.unnes.ac.id/sju/index.php/epj (accessed on 13 June 2025). [CrossRef]
- Irianjani, N.D.; Rohmah, F.A. Applying token economy to improve attention of child with ADHD. J. Early Child. Care Educ. 2020, 3, 1–13. [Google Scholar] [CrossRef]
- Abramowitz, A.J.; O’Leary, S.G. Behavioral interventions for the classroom: Implications for students with ADHD. Sch. Psychol. Rev. 1991, 20, 220–234. [Google Scholar] [CrossRef]
- Darwish, A.H.; Elgohary, T.M.; Nosair, N.A. Serum interleukin-6 level in children with attention-deficit hyperactivity disorder (ADHD). J. Child Neurol. 2019, 34, 61–67. [Google Scholar] [CrossRef]
- Kim, S.H.; Choi, H.S.; Koo, C.M.; Joo, B.R.; Park, B.J.; Lee, H.K.; Lee, J.S.; Kim, D.H.; Kang, H.C. Effects of cannabidiol on adaptive behavior and quality of life in pediatric patients with treatment-resistant epilepsy. J. Clin. Neurol. 2022, 18, 547. [Google Scholar] [CrossRef] [PubMed]
- Kang, H. Sample size determination and power analysis using the G* Power software. J. Educ. Eval. Health Prof. 2021, 18, 17. [Google Scholar] [CrossRef] [PubMed]
- Ingvaldsen, S.H.; Tronvik, E.; Brenner, E.; Winnberg, I.; Olsen, A.; Gravdahl, G.B.; Stubberud, A. A biofeedback app for migraine: Development and usability study. JMIR Form. Res. 2021, 5, e23229. [Google Scholar] [CrossRef]
- Guerrini Usubini, A.; Marazzi, N.; Abbruzzese, L.; Tringali, G.; De Micheli, R.; Castelnuovo, G.; Sartorio, A. Emotional and behavioural adjustment in children and adolescents with short stature vs. Their normal-statured peers. J. Clin. Med. 2025, 14, 538. [Google Scholar] [CrossRef] [PubMed]
- Park, E.Y.; Seo, H.; Blair, K.S.C.; Kang, M.C. Rasch analysis of the Korean-Child Behavior Checklist (K-CBCL) to assess emotional and behavioral problems in children with autism spectrum disorder. Sage Open 2021, 11, 21582440211040790. [Google Scholar] [CrossRef]
- Jung, M.; Park, J. Effects of a Virtual Reality-Based Aggression Control Program on Children with Autism Spectrum Disorder: A Case Study. Children 2025, 12, 173. [Google Scholar] [CrossRef]
- Eun-Bin, S.; Hyun-Joo, H. Clinical utility of the MMPI-A-RF’s internalization and externalization higher-order scales: Comparison with the K-CBCL’s internalization and externalization scales. Korean J. Psychosom. Med. 2022, 30, 119–126. [Google Scholar] [CrossRef]
- Lee, K.; Cho, I.H.; Park, J.; Choi, H.; Cheon, K.A. Response inhibition as a critical executive function in differentiating attention-deficit/hyperactivity disorder from autism spectrum disorder: A comprehensive attention test study. Front. Psychiatry 2024, 15, 1426376. [Google Scholar] [CrossRef]
- Lee, H.; Huh, H.; Kim, W.Y.; Lee, E.K.; Choi, B.S.; Kim, B.; Yoo, H. Diagnostic validity of the comprehensive attention test in patients with attention-deficit/hyperactivity disorder. J. Korean Acad. Child Adolesc. Psychiatry 2024, 35, 243. [Google Scholar] [CrossRef] [PubMed]
- Yoo, K.H.; Lee, J.; Kang, S.H.; Park, E.H.; Jung, J.S.; Kim, B.N.; Son, J.W.; Park, T.W.; Kim, B.S.; Lee, Y.S. Standardization of the comprehensive attention test for the Korean children and adolescents. J. Korean Acad. Child Adolesc. Psychiatry 2009, 20, 68–75. [Google Scholar]
- Mishra, P.; Singh, U.; Pandey, C.M.; Mishra, P.; Pandey, G. Application of student’s t-test, analysis of variance, and covariance. Ann. Card. Anaesth. 2019, 22, 407–411. [Google Scholar] [CrossRef]
- Leppink, J. Analysis of Covariance (ANCOVA) vs. Moderated Regression (MODREG): Why the Interaction Matters. Health Prof. Educ. 2018, 4, 225–232. [Google Scholar] [CrossRef]
- Kim, H.Y. Statistical notes for clinical researchers: Chi-squared test and Fisher’s exact test. Restor. Dent. Endod. 2017, 42, 152. [Google Scholar] [CrossRef]
- Ludbrook, J. Should we use one-sided or two-sided P values in tests of significance? Clin. Exp. Pharmacol. Physiol. 2013, 40, 357–361. [Google Scholar] [CrossRef]
- Lakens, D. Calculating and reporting effect sizes to facilitate cumulative science: A practical primer for t-tests and ANOVAs. Front. Psychol. 2013, 4, 863. [Google Scholar] [CrossRef]
- Lovic, D.; Stojanov, V.; Jakovljevic, B.; Krotin, M.; Jurisic, V.; Djordjevic, D.; Paunovic, K.; Zdravkovic, M.; Simonovic, D.; Bastac, D.; et al. Prevalence of arterial hypertension in Serbia: PAHIS study. J. Hypertens. 2013, 31, 2151–2157. [Google Scholar] [CrossRef]
- Malek, M.S.; Askary, R. A Comparative Study of Participation in Extracurricular Activities between Children with and without Attention-Deficit/Hyperactivity Disorder. Iran. J. Child Neurol. 2025, 19, 35–43. [Google Scholar]
- Ghiaccio, R.; Passaro, A.; Stasolla, F.; Martini, E.; De Fortuna, A.M.; De Luca Picione, R. Exploring the Association Between Problematic Internet Use, Internet Gaming Disorder in Adolescents with ADHD: A Scoping Review. Int. J. Environ. Res. Public Health 2025, 22, 496. [Google Scholar] [CrossRef]
- Lin, J.; Chang, W.R. Effectiveness of Serious Games as Digital Therapeutics for Enhancing the Abilities of Children With Attention-Deficit/Hyperactivity Disorder (ADHD): Systematic Literature Review. JMIR Serious Games 2025, 13, e60937. [Google Scholar] [CrossRef] [PubMed]
- De Luca, V.; Schena, A.; Covino, A.; Di Bitonto, P.; Potenza, A.; Barba, M.C.; D’Errico, G. Serious games for the treatment of children with ADHD: The BRAVO project. Inf. Syst. Frontiers. 2025, 27, 841–863. [Google Scholar] [CrossRef]
- Hupp, S.D.; Reitman, D.; Northup, J.; O’Callaghan, P.; LeBlanc, M. The effects of delayed rewards, tokens, and stimulant medication on sportsmanlike behavior with ADHD-diagnosed children. Behav. Modif. 2002, 26, 148–162. [Google Scholar] [CrossRef] [PubMed]
- Park, S.Y.; Choi, D.H. Influence of Education in Environment on Maladjusted Behavior Changes among Children with ADHD. Environ. Educ. 2010, 23, 113–128. [Google Scholar]
- Widihapsari, I.A.G.K.; Yoenanto, N.H. Aplikasi Teknik Shaping dan Token Ekonomi untuk Meningkatkan Durasi Perilaku On-Task pada Anak dengan ADHD: The Application of Shaping Technique and Token Economy to Increase On-Task Behavior in a Child with ADHD. J. Psikol. Teor. Dan Terap. 2021, 12, 64–80. [Google Scholar]
- Isorna Folgar, M.; Faílde Garrido, J.M.; Dapía Conde, M.D.; Braña Rey, F. Evaluation of problematic video game use in adolescents with ADHD and without ADHD: New evidence and recommendations. Behav. Sci. 2024, 14, 524. [Google Scholar] [CrossRef] [PubMed]
- Obiokoye, E.E.; Onukwufor, J.N. Effects of Token Economy on The Management of Attention Deficit Hyperactivity Disorder Among Children In Schools in Rivers State. Int. J. Innov. Educ. Res. 2025, 13, 343–354. [Google Scholar] [CrossRef]
- Choi, J.Y.; Kang, J.H. Longitudinal Relationship Between Smartphone Dependence and Externalizing Behavior Problems: An Autoregressive Cross-Lagged Model. Psychiatry Investig. 2025, 22, 287. [Google Scholar] [CrossRef]
- Gizatdinova, Y.; Remizova, V.; Sand, A.; Sharma, S.; Rantanen, K.; Helminen, T.; Kylliäinen, A. PigScape: An embodied video game for cognitive peer-training of impulse and behavior control in children with ADHD. In Proceedings of the 24th International ACM SIGACCESS Conference on Computers and Accessibility (ASSETS 2022), Athens, Greece, 23–26 October 2022; ACM: New York, NY, USA, 2022; pp. 1–4. [Google Scholar] [CrossRef]
- Thawalampola, O.; Jayasuriya, D.; Kariyawasam, S.; Makawita, M.; Wijendra, D.; Joseph, J. Adaptive Learning Tool to Enhance Educational Outcomes for Students with Inattentive Attention Deficit Hyperactivity Disorder (ADHD). In Proceedings of the 2024 6th International Conference on Advancements in Computing (ICAC), Colombo, Sri Lanka, 27–29 March 2024; IEEE: Piscataway, NJ, USA, 2024; pp. 462–467. [Google Scholar] [CrossRef]
- Vidal, A.F.P.; Cervantes, J.A.; Rumbo-Morales, J.Y.; Sorcia-Vázquez, F.D.; Ortiz-Torres, G.; Moncada, C.A.C.; Arias, I.D.L.T. Development of RelaxQuest: A Serious EEG-Controlled Game Designed to Promote Relaxation and Self-Regulation with a Potential Focus on ADHD Intervention. Appl. Sci. 2024, 14, 11173. [Google Scholar] [CrossRef]
- Babu, A.; Joseph, A.P. Integrating virtual reality into ADHD therapy: Advancing clinical evidence and implementation strategies. Front. Psychiatry 2025, 16, 1591504. [Google Scholar] [CrossRef]



| Experimental Group (N = 16) | Control Group (N = 14) | Accompanying Symptoms | p-Value | ||||
|---|---|---|---|---|---|---|---|
| N | % | N | % | 0.67 * | |||
| Sex | Male | 13 | 81.3 | 12 | 85.7 | None | |
| Female | 3 | 18.7 | 2 | 14.3 | None | ||
| Age | Mean | SD | Mean | SD | 0.61 ** | ||
| 9.27 | 1.62 | 8.93 | 1.91 | ||||
| Experimental Group (N = 16) | Control Group (N = 14) | Adjusted Mean Difference (95% CI) | p-Value | Effect Size (95% CI) | |||||
|---|---|---|---|---|---|---|---|---|---|
| Mean or % | SD or % | Mean or % | SD or % | ||||||
| Attention Task_ Sensitivity Factor | Visual Selective Attention Task | Baseline | 3.05 | 0.58 | 3.38 | 0.49 | 0.482 * | ||
| 4 weeks | 3.25 | 0.48 | 3.44 | 0.54 | 0.752 * | ||||
| p-value | 0.057 ** | 0.287 ** | −0.19 (−0.43, 0.05) | 0.104 *** | 0.095 ## (0.00, 0.23) | ||||
| Rate of change | 6.56 | 26.07 | 1.78 | 22.86 | 0.118 * | 0.194 # | |||
| Auditory Selective Attention Task | Baseline | 3.28 | 0.92 | 3.67 | 1.08 | 0.048 * | |||
| 4 weeks | 3.45 | 0.94 | 3.51 | 0.44 | 0.487 * | ||||
| p-value | 0.148 ** | 0.251 ** | −0.12 (−0.32, 0.03) | 0.103 *** | 0.095 ## (0.00, 0.26) | ||||
| Rate of change | 5.18 | 41.13 | −4.36 | 30.59 | 0.048 * | 0.261 # | |||
| Flanker Task | Baseline | 0.70 | 0.30 | 0.65 | 0.50 | 0.540 * | |||
| 4 weeks | 0.84 | 0.40 | 0.72 | 0.59 | 0.697 * | ||||
| p-value | 0.045 ** | 0.087 ** | 0.12 (0.01, 0.23) | 0.038 *** | 0.150 ## (0.01, 0.32) | ||||
| Rate of change | 20.00 | 25.00 | 10.77 | 20.00 | 0.548 * | 0.405 # | |||
| Sustained Attention to Response Task | Baseline | 2.02 | 1.07 | 2.25 | 0.98 | 0.085 * | |||
| 4 weeks | 2.51 | 1.10 | 2.08 | 1.25 | 0.105 * | ||||
| p-value | 0.068 ** | 0.425 ** | 0.18 (0.03, 0.33) | 0.021 *** | 0.182 ## (0.02, 0.35) | ||||
| Rate of change | 24.26 | 48.06 | −7.56 | 45.61 | 0.028 * | 0.848 # | |||
| Attention Task_ Response Style Index | Visual Selective Attention Task | Baseline | 0.42 | 0.20 | 0.43 | 0.11 | 0.340 * | ||
| 4 weeks | 0.64 | 0.48 | 0.65 | 0.33 | 0.245 * | ||||
| p-value | 0.146 ** | 0.320 ** | 0.05 (−0.10, 0.20) | 0.518 *** | 0.016 ## (0.00, 0.10) | ||||
| Exacerbation | 5 | 33.3 | 3 | 20 | 0.157 **** | ||||
| No Change | 1 | 6.7 | 2 | 13.3 | |||||
| Improvement | 9 | 60 | 10 | 66.7 | |||||
| Rate of change | 52.38 | 74.38 | 51.16 | 54.87 | 0.265 * | 0.416 # | |||
| Auditory Selective Attention Task | Baseline | 0.69 | 0.25 | 0.55 | 0.17 | 0.420 * | |||
| 4 weeks | 0.81 | 0.67 | 0.60 | 0.11 | 0.058 * | ||||
| p-value | 0.120 ** | 0.420 ** | 0.15 (0.01, 0.29) | 0.044 *** | 0.136 ## (0.01, 0.30) | ||||
| Exacerbation | 2 | 13.3 | 4 | 26.7 | 0.157 **** | ||||
| No Change | 3 | 20 | 3 | 20 | |||||
| Improvement | 10 | 66.7 | 8 | 53.3 | |||||
| Rate of change | 17.39 | 66.40 | 9.09 | 15.58 | 0.042 * | 0.780 # | |||
| Flanker Task | Baseline | 0.72 | 0.38 | 0.70 | 0.44 | 0.470 * | |||
| 4 weeks | 0.64 | 0.28 | 0.68 | 0.57 | 0.184 * | ||||
| p-value | 0.650 ** | 0.497 ** | 0.16 (0.01, 0.31) | 0.040 *** | 0.147 ## (0.01, 0.31) | ||||
| Exacerbation | 3 | 20 | 5 | 33.3 | 0.037 **** | ||||
| No Change | 2 | 20 | 2 | 13.3 | |||||
| Improvement | 10 | 20 | 8 | 53.3 | |||||
| Rate of change | −11.11 | 42.84 | −2.86 | 66.63 | 0.620 * | 0.183 # | |||
| Sustained Attention to Response Task | Baseline | 0.37 | 0.29 | 0.40 | 0.28 | 0.879 * | |||
| 4 weeks | 0.58 | 0.04 | 0.62 | 0.24 | 0.316 * | ||||
| p-value | 0.514 ** | 0.084 ** | 0.12 (−0.01, 0.25) | 0.064 *** | 0.121 ## (0.00, 0.27) | ||||
| Exacerbation | 6 | 40 | 10 | 66.7 | 0.078 **** | ||||
| No Change | 2 | 13.3 | 0 | 0.0 | |||||
| Improvement | 7 | 46.7 | 5 | 33.3 | |||||
| Rate of change | 56.76 | 45.55 | 55.00 | 39.94 | 0.229 * | 0.041 # | |||
| Experimental Group (N = 16) | Control Group (N = 14) | Adjusted Mean Difference (95% CI) | p-Value | Effect Size (95% CI) | |||||
|---|---|---|---|---|---|---|---|---|---|
| Mean or % | SD | Mean or % | SD | ||||||
| Behavior Problems And Social Competence | K-CBCL_ Total Behavior Problems | Baseline | 63.26 | 3.85 | 65.13 | 4.20 | 0.502 * | ||
| 4 weeks | 60.04 | 3.20 | 62.84 | 3.25 | 0.305 * | ||||
| p-value | 0.161 ** | 0.074 ** | 0.10 (−0.03, 0.23) | 0.130 *** | 0.080 ## (0.00, 0.020) | ||||
| Rate of change | −5.09 | 5.07 | −3.52 | 5.28 | 0.053 * | 0.739 # | |||
| K-CBCL_ Internalizing Disorders | Baseline | 63.40 | 5.20 | 61.05 | 3.28 | 0.072 * | |||
| 4 weeks | 56.35 | 5.01 | 59.45 | 3.37 | 0.033 * | ||||
| p-value | 0.095 ** | 0.134 ** | 0.14 (0.00, 0.28) | 0.051 *** | 0.134 ## (0.00, 0.29) | ||||
| Rate of change | −11.12 | 8.20 | −2.62 | 5.37 | 0.206 * | 0.474 # | |||
| K-CBCL_ Externalizing Disorders | Baseline | 60.54 | 8.20 | −2.62 | 5.37 | 0.201 * | |||
| 4 weeks | 54.04 | 1.54 | 57.00 | 3.50 | 0.034 * | ||||
| p-value | 0.046 ** | 0.085 ** | −5.2 (−10.10, −0.32) | 0.042 *** | 0.144 ## (0.01, 0.31) | ||||
| Rate of change | −10.74 | 2.05 | −8.12 | 4.51 | 0.026 * | 0.860 # | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.-C. Verification of the Effectiveness of a Token Economy Method Through Digital Intervention Content for Children with Attention-Deficit/Hyperactivity Disorder. Bioengineering 2025, 12, 1035. https://doi.org/10.3390/bioengineering12101035
Kim S-C. Verification of the Effectiveness of a Token Economy Method Through Digital Intervention Content for Children with Attention-Deficit/Hyperactivity Disorder. Bioengineering. 2025; 12(10):1035. https://doi.org/10.3390/bioengineering12101035
Chicago/Turabian StyleKim, Seon-Chil. 2025. "Verification of the Effectiveness of a Token Economy Method Through Digital Intervention Content for Children with Attention-Deficit/Hyperactivity Disorder" Bioengineering 12, no. 10: 1035. https://doi.org/10.3390/bioengineering12101035
APA StyleKim, S.-C. (2025). Verification of the Effectiveness of a Token Economy Method Through Digital Intervention Content for Children with Attention-Deficit/Hyperactivity Disorder. Bioengineering, 12(10), 1035. https://doi.org/10.3390/bioengineering12101035






