Mathematical Modeling of Vedolizumab Treatment’s Effect on Microbiota and Intestinal Permeability in Inflammatory Bowel Disease Patients
Abstract
1. Introduction
2. Materials and Methods
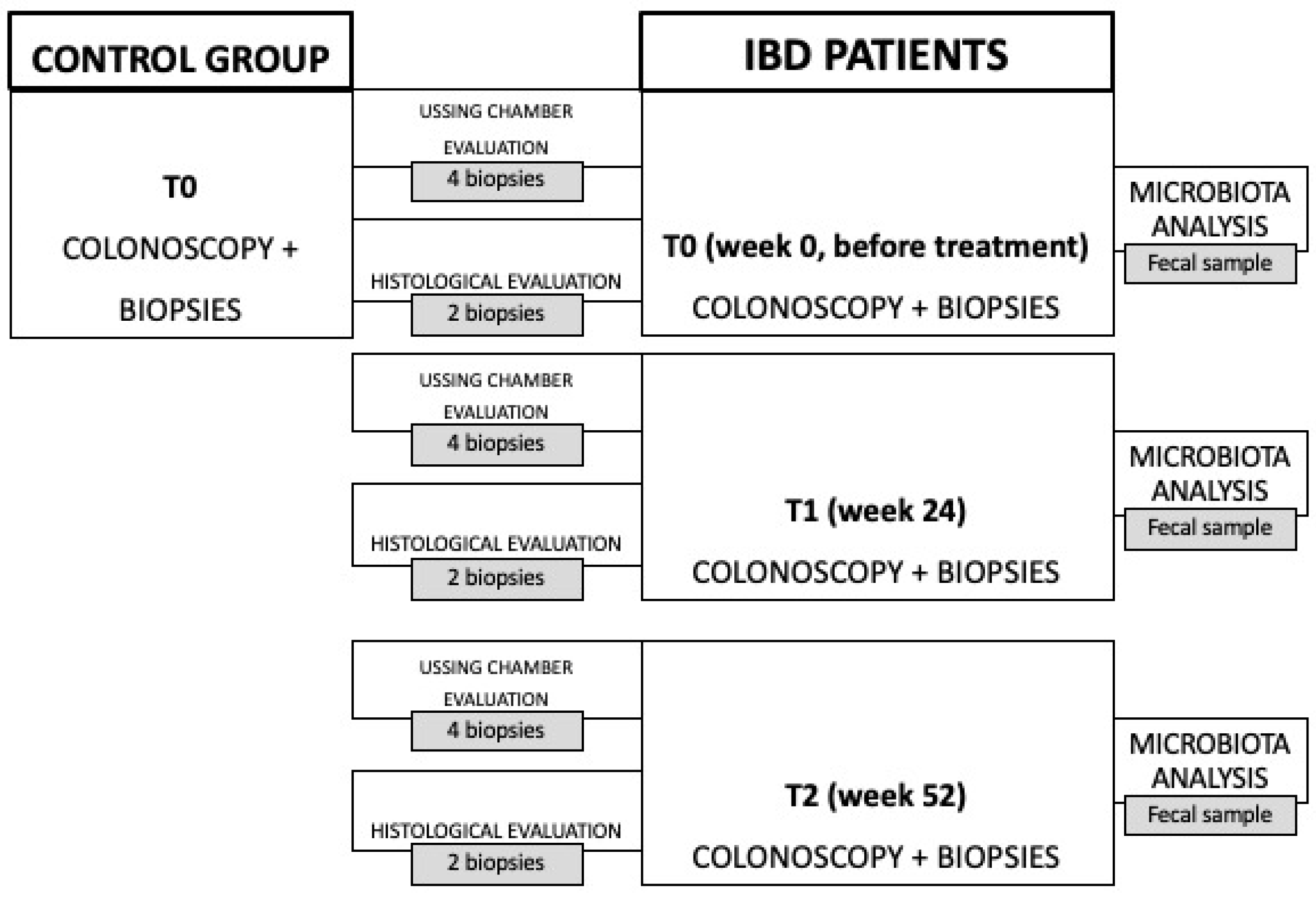
2.1. Study Design
2.2. Data Analysis
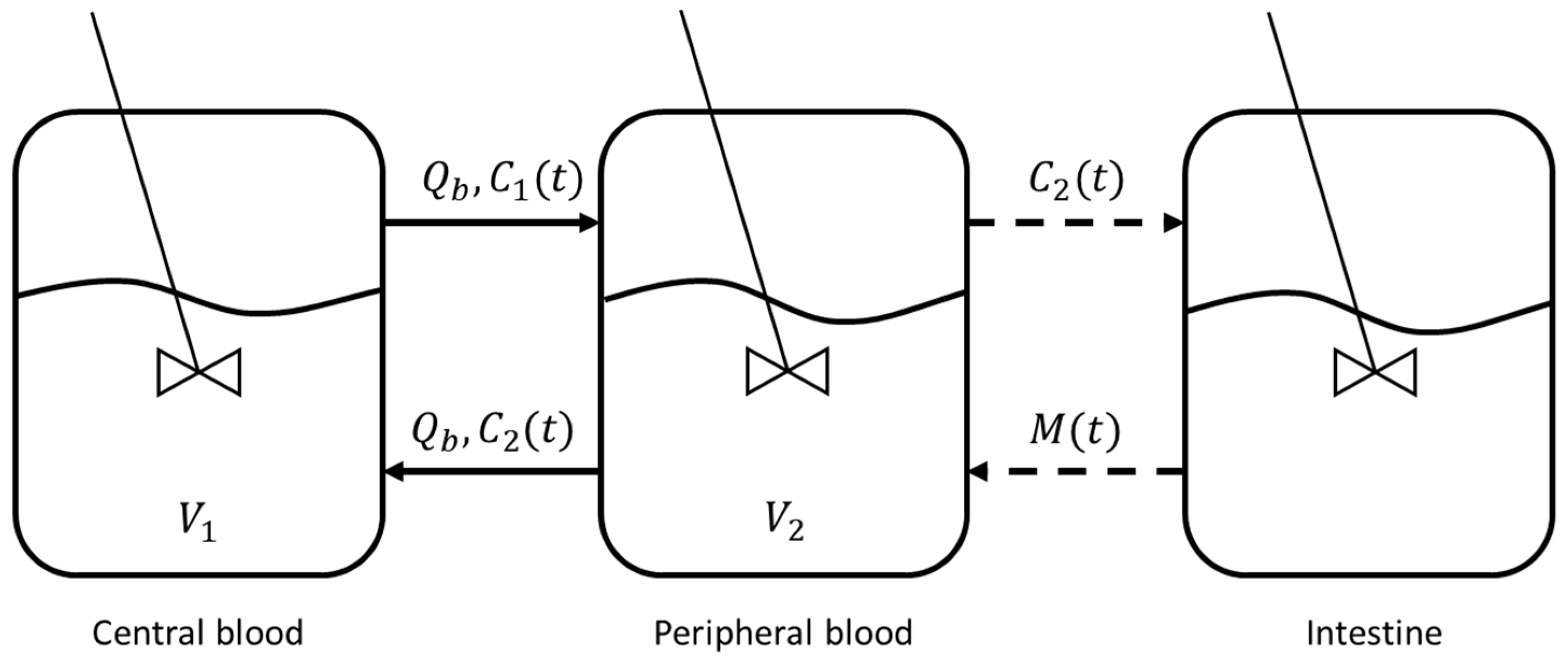
2.3. Mathematical Model
3. Results and Discussion
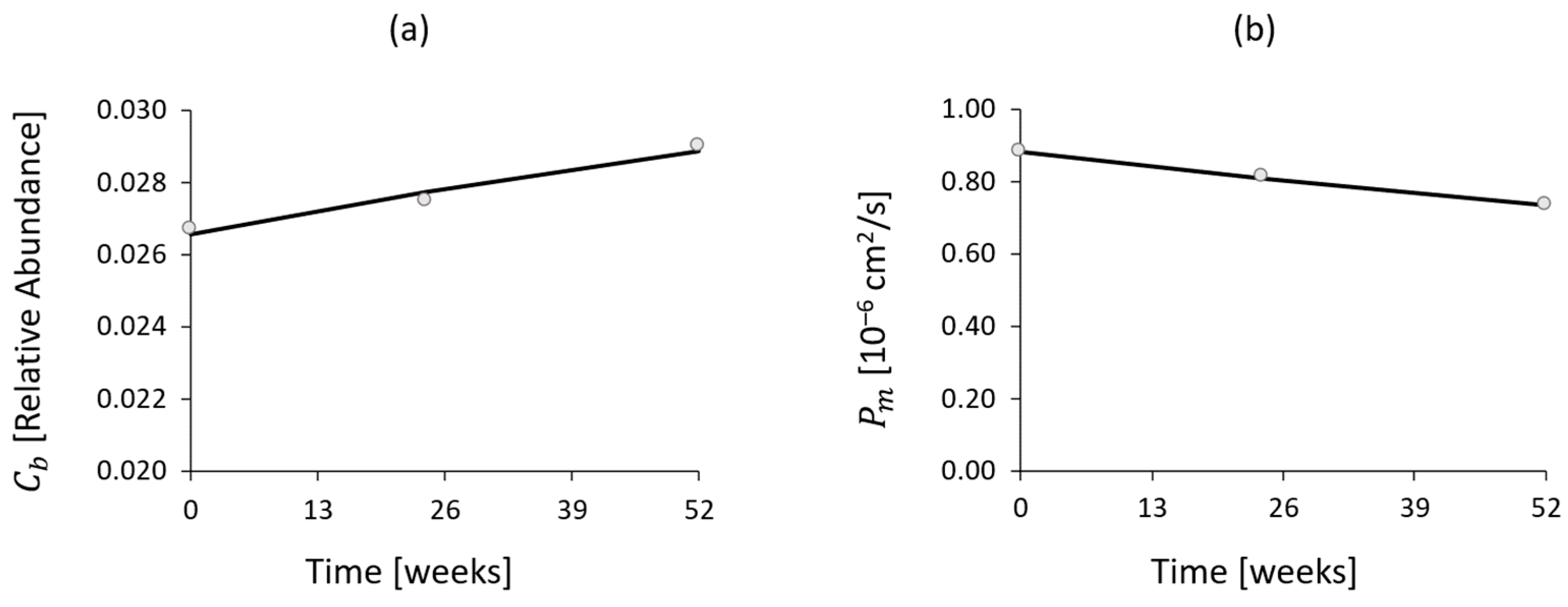
3.1. Fecal Microbiota Analysis
3.2. TEER Measurement
- In IBD patients, TEER increases from phase t0 to t2, reaching values similar to those of the control group. This trend indicates that the drug effect is restoring the function of the intestinal junctions, leading, in turn, to increased transepithelial electrical resistance to ion passage, since the paracellular resistance exerted by the TJ structure represents a major contributor to the TEER. This hypothesis was confirmed by a paired samples t-test, resulting in a significantly low p-value (less than 0.001), as shown in Figure 6.
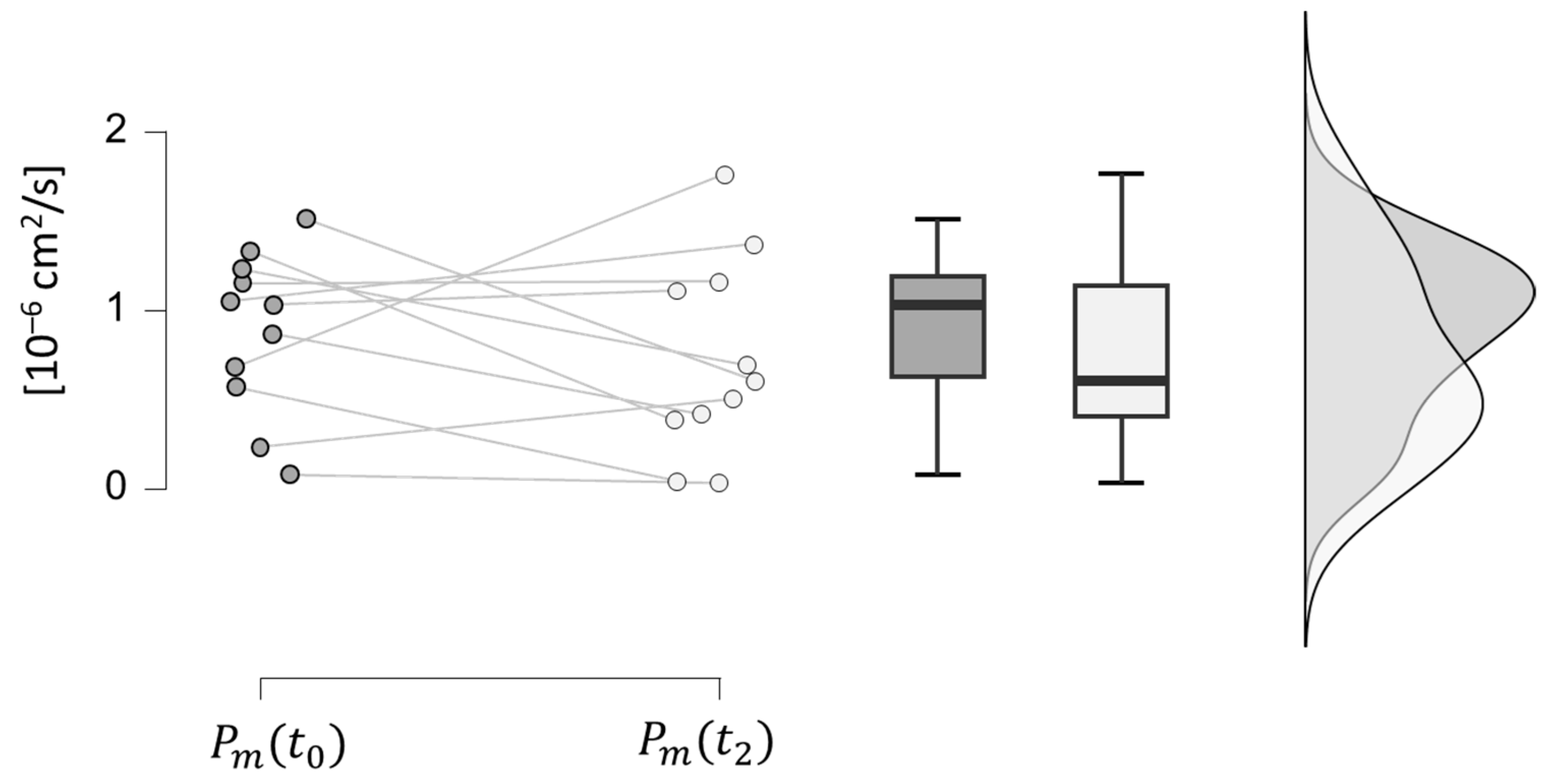
3.3. Intestinal Permeability to Paracellular Passage Evaluation
3.4. Histological Analysis
3.5. Mathematical Modeling Results
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Viggiano, D.; Ianiro, G.; Vanella, G.; Bibbò, S.; Bruno, G.; Simeone, G.; Mele, G. Gut Barrier in Health and Disease: Focus on Childhood. Eur. Rev. Med. Pharmacol. Sci. 2015, 19, 1077–1085. [Google Scholar] [PubMed]
- Busillo, V. Il Lume Intestinale e La Sclerosi Multipla. Sclerosi Mult. Inf. Lett. Evidenze 2020, 3, 70–76. [Google Scholar]
- Farré, R.; Fiorani, M.; Abdu Rahiman, S.; Matteoli, G. Intestinal Permeability, Inflammation and the Role of Nutrients. Nutrients 2020, 12, 1185. [Google Scholar] [CrossRef] [PubMed]
- Ulluwishewa, D.; Anderson, R.C.; McNabb, W.C.; Moughan, P.J.; Wells, J.M.; Roy, N.C. Regulation of Tight Junction Permeability by Intestinal Bacteria and Dietary Components1,2. J. Nutr. 2011, 141, 769–776. [Google Scholar] [CrossRef] [PubMed]
- Guo, X.; Rao, J.N.; Liu, L.; Zou, T.-T.; Turner, D.J.; Bass, B.L.; Wang, J.-Y. Regulation of Adherens Junctions and Epithelial Paracellular Permeability: A Novel Function for Polyamines. Am. J. Physiol. Cell Physiol. 2003, 285, C1174–C1187. [Google Scholar] [CrossRef] [PubMed]
- Gori, M.; Altomare, A.; Cocca, S.; Solida, E.; Ribolsi, M.; Carotti, S.; Rainer, A.; Francesconi, M.; Morini, S.; Cicala, M.; et al. Palmitic Acid Affects Intestinal Epithelial Barrier Integrity and Permeability In Vitro. Antioxidants 2020, 9, 417. [Google Scholar] [CrossRef] [PubMed]
- Landman, C.; Quévrain, E. Le Microbiote Intestinal: Description, Rôle et Implication Physiopathologique. Rev. Med. Interne 2016, 37, 418–423. [Google Scholar] [CrossRef] [PubMed]
- Gomaa, E.Z. Human Gut Microbiota/Microbiome in Health and Diseases: A Review. Antonie Leeuwenhoek 2020, 113, 2019–2040. [Google Scholar] [CrossRef] [PubMed]
- Thursby, E.; Juge, N. Introduction to the Human Gut Microbiota. Biochem. J. 2017, 474, 1823–1836. [Google Scholar] [CrossRef]
- Jandhyala, S.M. Role of the Normal Gut Microbiota. World J. Gastroenterol. 2015, 21, 8787. [Google Scholar] [CrossRef]
- Swidsinski, A. Spatial Organization of Bacterial Flora in Normal and Inflamed Intestine: A Fluorescence in Situ Hybridization Study in Mice. World J. Gastroenterol. 2005, 11, 1131. [Google Scholar] [CrossRef]
- Karl, J.P.; Margolis, L.M.; Madslien, E.H.; Murphy, N.E.; Castellani, J.W.; Gundersen, Y.; Hoke, A.V.; Levangie, M.W.; Kumar, R.; Chakraborty, N.; et al. Changes in Intestinal Microbiota Composition and Metabolism Coincide with Increased Intestinal Permeability in Young Adults under Prolonged Physiological Stress. Am. J. Physiol. Gastrointest. Liver Physiol. 2017, 312, G559–G571. [Google Scholar] [CrossRef] [PubMed]
- Marteau, P.; Seksik, P. Microbiota Intestinale, Pre-e Probiotici. EMC-AKOS-Trattato Med. 2020, 22, 1–6. [Google Scholar] [CrossRef]
- Jairath, V.; Feagan, B.G. Global Burden of Inflammatory Bowel Disease. Lancet Gastroenterol. Hepatol. 2020, 5, 2–3. [Google Scholar] [CrossRef]
- Kaplan, G.G.; Ng, S.C. Understanding and Preventing the Global Increase of Inflammatory Bowel Disease. Gastroenterology 2017, 152, 313–321.e2. [Google Scholar] [CrossRef]
- Magro, F.; Gionchetti, P.; Eliakim, R.; Ardizzone, S.; Armuzzi, A.; Barreiro-de Acosta, M.; Burisch, J.; Gecse, K.B.; Hart, A.L.; Hindryckx, P.; et al. Third European Evidence-Based Consensus on Diagnosis and Management of Ulcerative Colitis. Part 1: Definitions, Diagnosis, Extra-Intestinal Manifestations, Pregnancy, Cancer Surveillance, Surgery, and Ileo-Anal Pouch Disorders. J. Crohns Colitis 2017, 11, 649–670. [Google Scholar] [CrossRef]
- Torres, J.; Mehandru, S.; Colombel, J.-F.; Peyrin-Biroulet, L. Crohn’s Disease. Lancet 2017, 389, 1741–1755. [Google Scholar] [CrossRef] [PubMed]
- Thompson-Chagoyán, O.C.; Maldonado, J.; Gil, A. Aetiology of Inflammatory Bowel Disease (IBD): Role of Intestinal Microbiota and Gut-Associated Lymphoid Tissue Immune Response. Clin. Nutr. 2005, 24, 339–352. [Google Scholar] [CrossRef]
- Dotan, I.; Allez, M.; Danese, S.; Keir, M.; Tole, S.; McBride, J. The Role of Integrins in the Pathogenesis of Inflammatory Bowel Disease: Approved and Investigational Anti-integrin Therapies. Med. Res. Rev. 2020, 40, 245–262. [Google Scholar] [CrossRef]
- Park, S.C.; Jeen, Y.T. Anti-Integrin Therapy for Inflammatory Bowel Disease. World J. Gastroenterol. 2018, 24, 1868–1880. [Google Scholar] [CrossRef]
- DeBerg, H.A.; Konecny, A.J.; Shows, D.M.; Lord, J.D. MAdCAM-1 Costimulates T Cells through Integrin A4β7 to Cause Gene Expression Events Resembling Costimulation through CD28. Immunohorizons 2022, 6, 211–223. [Google Scholar] [CrossRef] [PubMed]
- Ben-Horin, S.; Chowers, Y. Review Article: Loss of Response to Anti-TNF Treatments in Crohn’s Disease. Aliment. Pharmacol. Ther. 2011, 33, 987–995. [Google Scholar] [CrossRef] [PubMed]
- Adegbola, S.O.; Sahnan, K.; Warusavitarne, J.; Hart, A.; Tozer, P. Anti-TNF Therapy in Crohn’s Disease. Int. J. Mol. Sci. 2018, 19, 2244. [Google Scholar] [CrossRef] [PubMed]
- Wyant, T.; Fedyk, E.; Abhyankar, B. An Overview of the Mechanism of Action of the Monoclonal Antibody Vedolizumab. J. Crohns Colitis 2016, 10, 1437–1444. [Google Scholar] [CrossRef] [PubMed]
- Petrovic, A.; Alpdogan, O.; Willis, L.M.; Eng, J.M.; Greenberg, A.S.; Kappel, B.J.; Liu, C.; Murphy, G.J.; Heller, G.; van den Brink, M.R.M. LPAM (A4β7 Integrin) Is an Important Homing Integrin on Alloreactive T Cells in the Development of Intestinal Graft-versus-Host Disease. Blood 2004, 103, 1542–1547. [Google Scholar] [CrossRef] [PubMed]
- Ward, M.G.; Sparrow, M.P.; Roblin, X. Therapeutic Drug Monitoring of Vedolizumab in Inflammatory Bowel Disease: Current Data and Future Directions. Therap Adv. Gastroenterol. 2018, 11, 175628481877278. [Google Scholar] [CrossRef] [PubMed]
- Rosario, M.; Dirks, N.L.; Milch, C.; Parikh, A.; Bargfrede, M.; Wyant, T.; Fedyk, E.; Fox, I. A Review of the Clinical Pharmacokinetics, Pharmacodynamics, and Immunogenicity of Vedolizumab. Clin. Pharmacokinet. 2017, 56, 1287–1301. [Google Scholar] [CrossRef]
- Xie, R.; Zhao, N.; Jia, B.; Zhao, X.; Cui, Y.; Okamoto, H.; Yang, L.; Prokopienko, A. Pharmacokinetics and Safety of Vedolizumab Following Administration of a Single Intravenous Dose in Healthy Chinese Subjects. Eur. J. Drug Metab. Pharmacokinet. 2023, 48, 35–40. [Google Scholar] [CrossRef]
- Parikh, A.; Leach, T.; Wyant, T.; Scholz, C.; Sankoh, S.; Mould, D.R.; Ponich, T.; Fox, I.; Feagan, B.G. Vedolizumab for the Treatment of Active Ulcerative Colitis: A Randomized Controlled Phase 2 Dose-Ranging Study. Inflamm. Bowel Dis. 2012, 18, 1470–1479. [Google Scholar] [CrossRef]
- Rosario, M.; Wyant, T.; Leach, T.; Sankoh, S.; Scholz, C.; Parikh, A.; Fox, I.; Feagan, B.G. Vedolizumab Pharmacokinetics, Pharmacodynamics, Safety, and Tolerability Following Administration of a Single, Ascending, Intravenous Dose to Healthy Volunteers. Clin. Drug Investig. 2016, 36, 913–923. [Google Scholar] [CrossRef]
- Boden, E.K.; Shows, D.M.; Chiorean, M.V.; Lord, J.D. Identification of Candidate Biomarkers Associated with Response to Vedolizumab in Inflammatory Bowel Disease. Dig. Dis. Sci. 2018, 63, 2419–2429. [Google Scholar] [CrossRef]
- Binder, M.-T.; Becker, E.; Wiendl, M.; Schleier, L.; Fuchs, F.; Leppkes, M.; Atreya, R.; Neufert, C.; Atreya, I.; Neurath, M.F.; et al. Similar Inhibition of Dynamic Adhesion of Lymphocytes From IBD Patients to MAdCAM-1 by Vedolizumab and Etrolizumab-s. Inflamm. Bowel Dis. 2018, 24, 1237–1250. [Google Scholar] [CrossRef]
- Gerlowski, L.E.; Jain, R.K. Physiologically Based Pharmacokinetic Modeling: Principles and Applications. J. Pharm. Sci. 1983, 72, 1103–1127. [Google Scholar] [CrossRef]
- Upton, R.N.; Foster, D.J.R.; Abuhelwa, A.Y. An Introduction to Physiologically-Based Pharmacokinetic Models. Pediatr. Anesth. 2016, 26, 1036–1046. [Google Scholar] [CrossRef]
- Himmelstein, K.J.; Lutz, R.J. A Review of the Applications of Physiologically Based Pharmacokinetic Modeling. J. Pharmacokinet. Biopharm. 1979, 7, 127–145. [Google Scholar] [CrossRef] [PubMed]
- Jones, H.M.; Rowland-Yeo, K. Basic Concepts in Physiologically Based Pharmacokinetic Modeling in Drug Discovery and Development. CPT Pharmacomet. Syst. Pharmacol. 2013, 2, 1–12. [Google Scholar] [CrossRef]
- Theil, F.P.; Guentert, T.W.; Haddad, S.; Poulin, P. Utility of Physiologically Based Pharmacokinetic Models to Drug Development and Rational Drug Discovery Candidate Selection. Toxicol. Lett. 2003, 138, 29–49. [Google Scholar] [CrossRef] [PubMed]
- Emoto, C.; McPhail, B.T.; Fukuda, T. Clinical Applications of Physiologically Based Pharmacokinetic Modeling: Perspectives on the Advantages and Challenges. Ther. Drug Monit. 2020, 42, 157–158. [Google Scholar] [CrossRef]
- Loisios-Konstantinidis, I.; Dressman, J. Physiologically Based Pharmacokinetic/Pharmacodynamic Modeling to Support Waivers of In Vivo Clinical Studies: Current Status, Challenges, and Opportunities. Mol. Pharm. 2020, 18, 1–17. [Google Scholar] [CrossRef]
- Perry, C.; Davis, G.; Conner, T.M.; Zhang, T. Utilization of Physiologically Based Pharmacokinetic Modeling in Clinical Pharmacology and Therapeutics: An Overview. Curr. Pharmacol. Rep. 2020, 6, 71–84. [Google Scholar] [CrossRef]
- Rosario, M.; Dirks, N.L.; Gastonguay, M.R.; Fasanmade, A.A.; Wyant, T.; Parikh, A.; Sandborn, W.J.; Feagan, B.G.; Reinisch, W.; Fox, I. Population Pharmacokinetics-Pharmacodynamics of Vedolizumab in Patients with Ulcerative Colitis and Crohn’s Disease. Aliment. Pharmacol. Ther. 2015, 42, 188–202. [Google Scholar] [CrossRef] [PubMed]
- Cicala, M.; Gori, M.; Balestrieri, P.; Altomare, A.; Tullio, A.; Cola, S.D.; Dejongh, S.; Graziani, M.G.; Pagnini, C.; Carotti, S.; et al. Colonic Epithelial Permeability to Ions Is Restored after Vedolizumab Treatment and May Predict Clinical Response in Inflammatory Bowel Disease Patients. Int. J. Mol. Sci. 2024, 25, 5817. [Google Scholar] [CrossRef] [PubMed]
- Best, W.R. Predicting the Crohn’s Disease Activity Index from the Harvey-Bradshaw Index. Inflamm. Bowel Dis. 2006, 12, 304–310. [Google Scholar] [CrossRef] [PubMed]
- Lewis, J.D.; Chuai, S.; Nessel, L.; Lichtenstein, G.R.; Aberra, F.N.; Ellenberg, J.H. Use of the Noninvasive Components of the Mayo Score to Assess Clinical Response in Ulcerative Colitis. Inflamm. Bowel Dis. 2008, 14, 1660–1666. [Google Scholar] [CrossRef] [PubMed]
- Bolyen, E.; Rideout, J.R.; Dillon, M.R.; Bokulich, N.A.; Abnet, C.C.; Al-Ghalith, G.A.; Alexander, H.; Alm, E.J.; Arumugam, M.; Asnicar, F.; et al. Reproducible, Interactive, Scalable and Extensible Microbiome Data Science Using QIIME 2. Nat. Biotechnol. 2019, 37, 852–857. [Google Scholar] [CrossRef] [PubMed]
- Callahan, B.J.; McMurdie, P.J.; Rosen, M.J.; Han, A.W.; Johnson, A.J.A.; Holmes, S.P. DADA2: High-Resolution Sample Inference from Illumina Amplicon Data. Nat. Methods 2016, 13, 581–583. [Google Scholar] [CrossRef] [PubMed]
- DeSantis, T.Z.; Hugenholtz, P.; Larsen, N.; Rojas, M.; Brodie, E.L.; Keller, K.; Huber, T.; Dalevi, D.; Hu, P.; Andersen, G.L. Greengenes, a Chimera-Checked 16S RRNA Gene Database and Workbench Compatible with ARB. Appl. Environ. Microbiol. 2006, 72, 5069–5072. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Sheppard, D.N.; Hug, M.J. Transepithelial Electrical Measurements with the Ussing Chamber. J. Cyst. Fibros. 2004, 3, 123–126. [Google Scholar] [CrossRef] [PubMed]
- Altomare, A.; Gori, M.; Cocca, S.; Carotti, S.; Francesconi, M.; Ribolsi, M.; Emerenziani, S.; Perrone, G.; Morini, S.; Cicala, M.; et al. Impaired Colonic Contractility and Intestinal Permeability in Symptomatic Uncomplicated Diverticular Disease. J. Neurogastroenterol. Motil. 2021, 27, 292–301. [Google Scholar] [CrossRef]
- Vllasaliu, D.; Exposito-Harris, R.; Heras, A.; Casettari, L.; Garnett, M.; Illum, L.; Stolnik, S. Tight Junction Modulation by Chitosan Nanoparticles: Comparison with Chitosan Solution. Int. J. Pharm. 2010, 400, 183–193. [Google Scholar] [CrossRef]
- Vespa, E.; D’Amico, F.; Sollai, M.; Allocca, M.; Furfaro, F.; Zilli, A.; Dal Buono, A.; Gabbiadini, R.; Danese, S.; Fiorino, G. Histological Scores in Patients with Inflammatory Bowel Diseases: The State of the Art. J. Clin. Med. 2022, 11, 939. [Google Scholar] [CrossRef] [PubMed]
- Lambert, J.D. Numerical Methods for Ordinary Differential Systems; Wiley: New York, NY, USA, 1991; Volume 146. [Google Scholar]
- Battat, R.; Dulai, P.S.; Vande Casteele, N.; Evans, E.; Hester, K.D.; Webster, E.; Jain, A.; Proudfoot, J.A.; Mairalles, A.; Neill, J.; et al. Biomarkers Are Associated With Clinical and Endoscopic Outcomes With Vedolizumab Treatment in Ulcerative Colitis. Inflamm. Bowel Dis. 2019, 25, 410–420. [Google Scholar] [CrossRef] [PubMed]
- Matsuoka, K.; Kanai, T. The Gut Microbiota and Inflammatory Bowel Disease. Semin. Immunopathol. 2015, 37, 47–55. [Google Scholar] [CrossRef] [PubMed]
- Shen, Z.; Zhu, C.; Quan, Y.; Yang, J.; Yuan, W.; Yang, Z.; Wu, S.; Luo, W.; Tan, B.; Wang, X. Insights into Roseburia Intestinalis Which Alleviates Experimental Colitis Pathology by Inducing Anti-inflammatory Responses. J. Gastroenterol. Hepatol. 2018, 33, 1751–1760. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, K.; Nishida, A.; Fujimoto, T.; Fujii, M.; Shioya, M.; Imaeda, H.; Inatomi, O.; Bamba, S.; Andoh, A.; Sugimoto, M. Reduced Abundance of Butyrate-Producing Bacteria Species in the Fecal Microbial Community in Crohn’s Disease. Digestion 2016, 93, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Poritz, L.S.; Garver, K.I.; Green, C.; Fitzpatrick, L.; Ruggiero, F.; Koltun, W.A. Loss of the Tight Junction Protein ZO-1 in Dextran Sulfate Sodium Induced Colitis. J. Surg. Res. 2007, 140, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Lechuga, S.; Ivanov, A.I. Disruption of the Epithelial Barrier during Intestinal Inflammation: Quest for New Molecules and Mechanisms. Biochim. Biophys. Acta (BBA)-Mol. Cell Res. 2017, 1864, 1183–1194. [Google Scholar] [CrossRef] [PubMed]
- Vicario, M.; Alonso, C.; Santos, J. Impaired Intestinal Molecular Tightness in the Mucosa of Irritable Bowel Syndrome: What Are the Mediators? Gut 2009, 58, 161–162. [Google Scholar] [CrossRef]
- Schmitz, H.; Barmeyer, C.; Fromm, M.; Runkel, N.; Foss, H.D.; Bentzel, C.J.; Riecken, E.O.; Schulzke, J.D. Altered Tight Junction Structure Contributes to the Impaired Epithelial Barrier Function in Ulcerative Colitis. Gastroenterology 1999, 116, 301–309. [Google Scholar] [CrossRef]










| Vedolizumab Dose [mg/kg] | ||||
|---|---|---|---|---|
| Healthy Volunteers | UC Patients | |||
| Parameter | 2.0 () | 10.0 () | 2.0 () | 10.0 () |
| [μg/mL] | 58.4 | 243 | 60.4 | 291.9 |
| AUC [μg·day/mL] | 955 | 4840 | 848 | 4373 |
| 14.1 | 14.8 | 15.1 | 20.6 | |
| [L/day] | 0.164 | 0.139 | - | - |
| [L] | 3.28 | 2.73 | - | - |
| Patient Number | IBD | Therapy | HBI () | PMS () |
|---|---|---|---|---|
| 1 | UC | Naïve | 8-4-4 | |
| 2 | UC | Naïve | 8-2-2 | |
| 3 | CD | Naïve | 6-6-4 | |
| 4 | UC | Anti-TNF | 6-3-4 | |
| 5 | CD | Naïve | 7-5-1 | |
| 6 | CD | Anti-TNF | 5-4-3 | |
| 7 | UC | Anti-TNF | 11-1-2 | |
| 8 | CD | Naïve | 10-1-0 | |
| 9 | UC | Anti-TNF | 9-3-2 | |
| 10 | UC | Naïve | 7-3-2 | |
| 11 | UC | Anti-TNF | 6-6-4 |
| Parameter | Notation | Value | Reference |
|---|---|---|---|
| Blood flow rate [L/g] | 0.12 | [41] | |
| Vedolizumab kinetic constant [g−1] | 0.0368 | [This Work] | |
| Central blood compartment volume [L] | 3.12 | [41] | |
| Peripheral blood compartment volume [L] | 1.65 | [41] | |
| MAdCAM-1 initial concentration [mg/L] | 2.23 × 10−2 | [53] | |
| 0.956 | [41] | ||
| 0.3512 | [This Work] | ||
| Vedolizumab concentration at half-maximum effect [mg/L] | 0.093 | [41] |
| Parameter [Ω·cm2] | IBD Patients () | IBD Patients () | IBD Patients () | Control Group |
|---|---|---|---|---|
| Mean | 12.27 | 18.12 | 18.36 | 21.15 |
| Median | 12.80 | 16.80 | 18.30 | 18.50 |
| Std | 3.15 | 7.23 | 4.86 | 9.14 |
| Minimum | 7.50 | 10.00 | 13.25 | 10.00 |
| Maximum | 17.40 | 34.50 | 28.00 | 39.32 |
| Parameter [10−6·cm2/s] | IBD Patients () | IBD Patients () | IBD Patients () | Control Group |
|---|---|---|---|---|
| Mean | 0.883 | 0.814 | 0.735 | 0.686 |
| Median | 1.030 | 0.974 | 0.605 | 0.528 |
| Std | 0.451 | 0.446 | 0.552 | 0.365 |
| Minimum | 0.080 | 0.054 | 0.032 | 0.249 |
| Maximum | 1.510 | 1.450 | 1.760 | 1.270 |
| Patient Number | RHI (t0) | RHI (t1) | RHI (t2) |
|---|---|---|---|
| 1 | 17 | 8 | 8 |
| 2 | 12 | 6 | 6 |
| 3 | 6 | 6 | 6 |
| 4 | 14 | 1 | 1 |
| 5 | 12 | 1 | 1 |
| 6 | 6 | 6 | 6 |
| 7 | 23 | 6 | 6 |
| 8 | 17 | 6 | 7 |
| 9 | 23 | 11 | 6 |
| 10 | 23 | 16 | 9 |
| 11 | 19 | 6 | 6 |
| Mean | 16 | 7 | 6 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
D’Ambrosio, A.; Altomare, A.; Boscarino, T.; Gori, M.; Balestrieri, P.; Putignani, L.; Del Chierico, F.; Carotti, S.; Cicala, M.; Guarino, M.P.L.; et al. Mathematical Modeling of Vedolizumab Treatment’s Effect on Microbiota and Intestinal Permeability in Inflammatory Bowel Disease Patients. Bioengineering 2024, 11, 710. https://doi.org/10.3390/bioengineering11070710
D’Ambrosio A, Altomare A, Boscarino T, Gori M, Balestrieri P, Putignani L, Del Chierico F, Carotti S, Cicala M, Guarino MPL, et al. Mathematical Modeling of Vedolizumab Treatment’s Effect on Microbiota and Intestinal Permeability in Inflammatory Bowel Disease Patients. Bioengineering. 2024; 11(7):710. https://doi.org/10.3390/bioengineering11070710
Chicago/Turabian StyleD’Ambrosio, Antonio, Annamaria Altomare, Tamara Boscarino, Manuele Gori, Paola Balestrieri, Lorenza Putignani, Federica Del Chierico, Simone Carotti, Michele Cicala, Michele Pier Luca Guarino, and et al. 2024. "Mathematical Modeling of Vedolizumab Treatment’s Effect on Microbiota and Intestinal Permeability in Inflammatory Bowel Disease Patients" Bioengineering 11, no. 7: 710. https://doi.org/10.3390/bioengineering11070710
APA StyleD’Ambrosio, A., Altomare, A., Boscarino, T., Gori, M., Balestrieri, P., Putignani, L., Del Chierico, F., Carotti, S., Cicala, M., Guarino, M. P. L., & Piemonte, V. (2024). Mathematical Modeling of Vedolizumab Treatment’s Effect on Microbiota and Intestinal Permeability in Inflammatory Bowel Disease Patients. Bioengineering, 11(7), 710. https://doi.org/10.3390/bioengineering11070710













