Enhancing the Management of Non-Specific Neck Pain through Gamification: Design and Efficacy of a Health Application
Abstract
1. Introduction
2. Related Works
2.1. Review of Interventions for Chronic Non-Specific Neck Pain
2.2. Theoretical Models of Healthy Game Design and Application
2.2.1. Game for Health (G4H) Theory
2.2.2. Standards for Functional Design in Digital Health Applications
- The application must be driven by software.
- The therapeutic effectiveness must be supported by scientific evidence.
- The application must provide specific intervention measures for a designated disease, with the software’s functionality serving as the core mechanism.
- The application must be designed for patient use.
2.2.3. GameFlow Evaluation Model
3. Materials and Methods
3.1. Gamified Motion-Sensing Health Application Framework
- Conceptual Layer: Relying on the G4H theory, the core design elements of gamified neck exercise applications and their specific content in cervical spine disease interventions form the conceptual layer of the GMH framework. The detailed content is presented in Table 3, where each theoretical component is matched with a corresponding design developed in our research.
- Utility Layer: Integrating the functionality of digital health, digital healthcare, and digital therapies, the gamified health applications offer users a cohesive experience from basic health education to advanced therapeutic interventions. Accordingly, the functional design of each level in the utility tier is summarized in Table 4.
- Experience Layer: This study adopts the GameFlow model as the theoretical foundation for the Experience Layer in the GMH framework. To cultivate a positive feedback loop in user experience, gamified practice designs should incorporate an award system, feedback mechanisms, and the design of social interaction features. Table 5 summarizes how the eight factors are applied in the application.
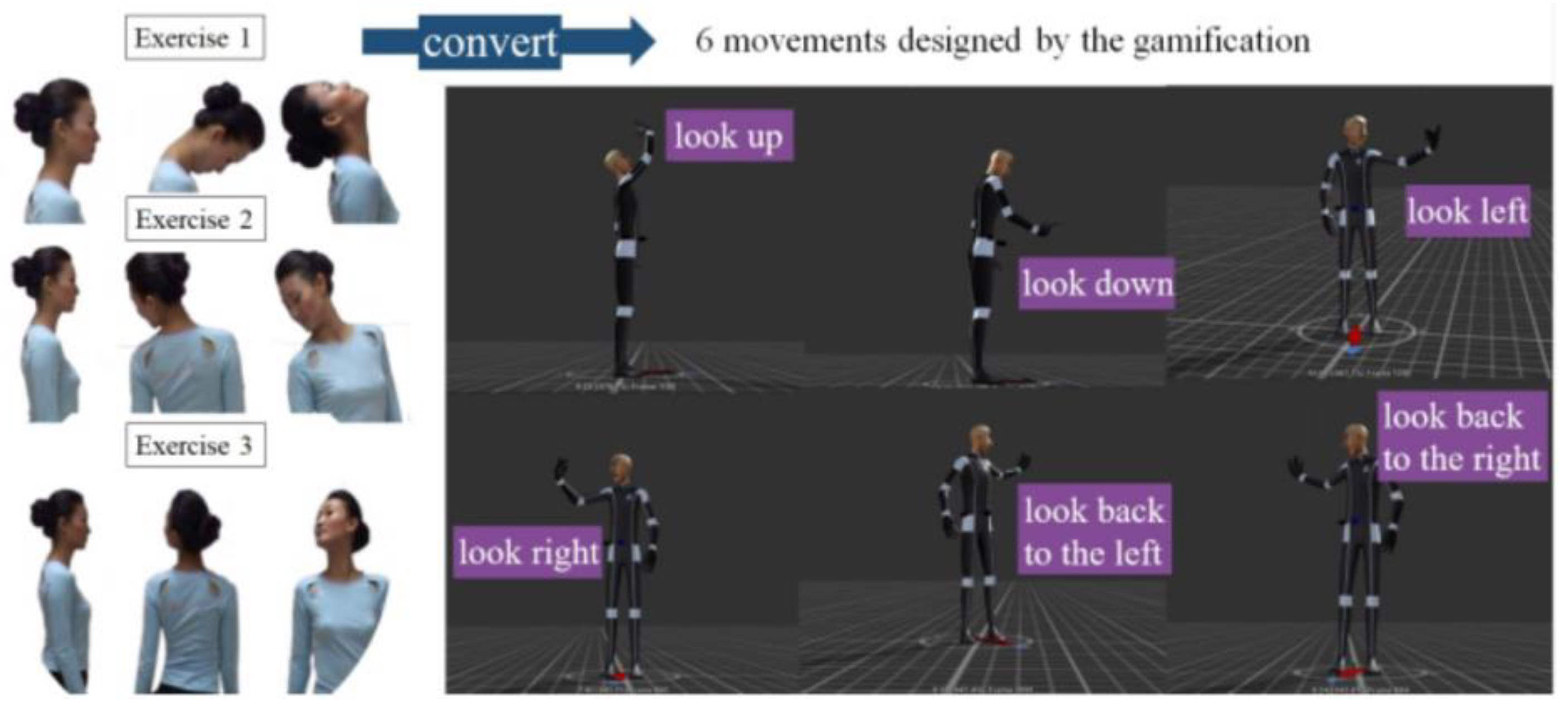
3.2. Implementation of a Gamified Somatic Health Application
3.3. Experimental Setup
3.3.1. Participants and Ethics
3.3.2. Setup of the Study
- Pre-experiment: Both control and experimental group members filled out the NDI questionnaire (refer to Appendix A, introduced in Section 3.3.3) and recorded their step data for the four days preceding the experiment. These data served as a baseline for physical activity indicators before the intervention.
- During the experiment: Both groups recorded their daily step data. Control group members received text and video instructions via a WeChat group. In contrast, experimental group members engaged with a gamified health application. Participants manually clicked a “Save” button within the application to store their data in the backend database.
- Post-experiment: Both groups completed the NDI questionnaire again. Additionally, experimental group members filled out the TAM questionnaire and submitted the application data to the researchers.
3.3.3. Data Collection and Processing
- Exercise Duration
- Total Exercise Duration
- Startup Rate
- Step Count
- Neck Disability Index (NDI)
- Technology Acceptance Model (TAM)
- Likert 5-Point Scale
4. Results
4.1. Results of the Data Collected to Test H1: Gamification Method Is More Effective Than Traditional Text and Video Interventions for Neck Pain
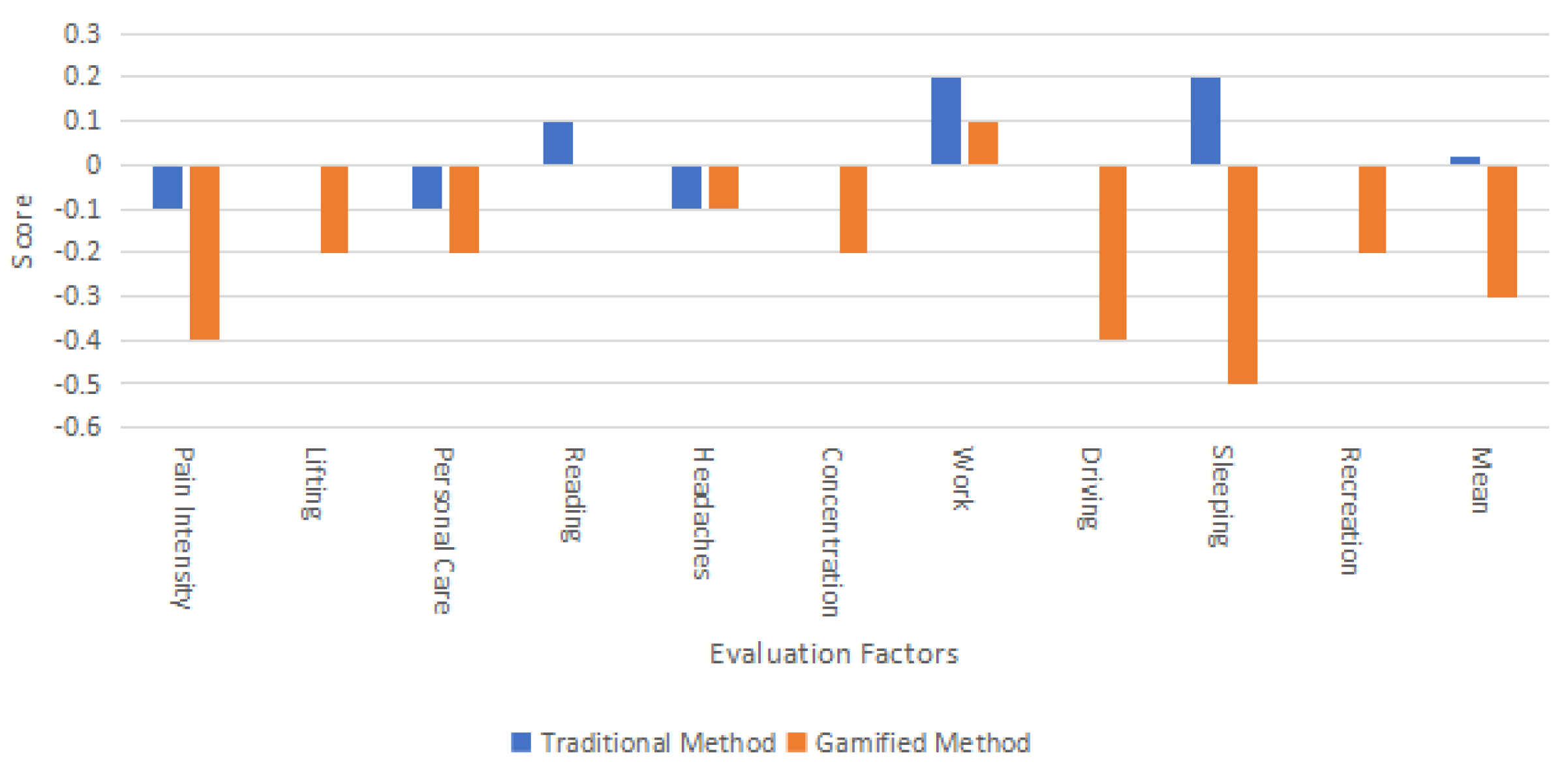
Analysis of the NDI Score
4.2. Results of the Data Collected to Test H2: The Gamification Method Can Enhance User Compliance in Neck Pain Interventions
4.2.1. Step Count Analysis
4.2.2. Exercise Duration Analysis
4.2.3. Analysis of User Technology Acceptance and Action Perception
5. Discussion
- Adaptation of Motion Capture Technology: Different rehabilitation exercises involve varying movements, necessitating appropriate motion capture and data processing technologies to record and analyze these movements accurately.
- Integration of Professional Knowledge: Collaboration with experts in relevant fields is required to ensure that the exercise movements and protocols within the game are scientifically sound and safe.
6. Conclusions and Future Work
- Increase the sample size to encompass a broader range of age groups, and focus on populations at high risk of significant cervical spine issues.
- Extend the experimental period to 4–6 weeks to explore the long-term effects.
- Develop complex game mechanics to enrich user interactions, thereby improving the adherence and the effectiveness of the treatment.
- Incorporate a variety of objective measurement tools, including muscle tone testers and X-ray imaging, to provide a more precise assessment of user activity levels and health status.
- Consider using advanced computer vision technology, such as learning from a single visual observation [54], to reduce reliance on motion capture devices.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Neck Disability Index (NDI) Questionnaire
Appendix B
| Technology Acceptance Model (TAM) Questionnaire | |||||||||||
| 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
| “Perceived usefulness” | |||||||||||
| Exercising with the app helps me relax my cervical spine. | |||||||||||
| Exercising with the app helps me reduce my sedentary time. | |||||||||||
| Exercising with the app helps me improve my willingness to get up and walk. | |||||||||||
| Exercising with the app helps me be more aware of my cervical spine health. | |||||||||||
| Exercising with the app is useful. | |||||||||||
| Perceived Ease of Use | |||||||||||
| The app’s operating instructions are clear. | |||||||||||
| The app is easy to interact with. | |||||||||||
| I’m satisfied with the interactive workout feature using the app. | |||||||||||
| I make very few operator errors when performing the Find the Stars workout interaction. | |||||||||||
| I think the app operation works well with my movement for virtual space exploration. | |||||||||||
| I think for the purpose of exercising the cervical spine, the star position makes sense in the app. | |||||||||||
| I rarely have unexpected problems when I use the app. | |||||||||||
| Intent to use | |||||||||||
| I like to use the “Find the Stars” interactive workout in the app. | |||||||||||
| I’m positive about the interactive exercise function of the app. | |||||||||||
| I think the app’s interactive workout design is an innovative feature. | |||||||||||
| If I’m using the app, I’ll continue to use the Somatic Interaction feature to relax my cervical spine | |||||||||||
Appendix C
References
- Ma, M.; Zhang, S.M.; Zhang, Y.D.; Li, Z.X.; Wu, G.N.; Zhang, X.J.; Jin, J.; Liu, Y.Z.; Zhang, Z.J. Preliminary analysis on X-ray in youth neck type of cervical spondylosis with upper crossed syndrome. China J. Orthop. Traumatol. 2019, 32, 225–229. [Google Scholar]
- Gómez, F.; Escribá, P.; Oliva-Pascual-Vaca, J.; Méndez-Sánchez, R.; Puente-González, A.S. Immediate and Short-term effects of upper cervical high-velocity, low-amplitude manipulation on standing postural control and cervical mobility in chronic nonspecific neck pain: A randomized controlled trial. J. Clin. Med. 2020, 9, 2580. [Google Scholar] [CrossRef] [PubMed]
- Safiri, S.; Kolahi, A.A.; Hoy, D.; Buchbinder, R.; Mansournia, M.A.; Bettampadi, D.; Ashrafi-Asgarabad, A.; Almasi-Hashiani, A.; Smith, E.; Sepidarkish, M.; et al. Global, regional, and national burden of neck pain in the general population, 1990-2017: Systematic analysis of the Global Burden of Disease Study 2017. BMJ 2020, 368, m791. [Google Scholar] [CrossRef] [PubMed]
- Zeng, X.Y.; Qi, J.L.; Yin, P.; Wang, L.J.; Liu, Y.N.; Liu, J.M. Report on the Burden of Disease in China and Provincial Administrative Regions, 1990~2016. Chin. Circ. J. 2018, 33, 1147–1158. [Google Scholar]
- Wu, A.-M.; Cross, M.; Elliott, J.M.; Culbreth, G.T.; Haile, L.M.; Steinmetz, J.D.; Hagins, H.; Kopec, J.A.; Brooks, P.M.; Woolf, A.D.; et al. Global, regional, and national burden of neck pain, 1990–2020, and projections to 2050: A systematic analysis of the Global Burden of Disease Study 2021. Lancet Rheumatol. 2024, 6, e142–e155. [Google Scholar] [CrossRef] [PubMed]
- Breivik, H.; Collett, B.; Ventafridda, V.; Cohen, R.; Gallacher, D. Survey of chronic pain in Europe: Prevalence, impact on daily life, and treatment. Eur. J. Pain 2006, 10, 287–333. [Google Scholar] [CrossRef] [PubMed]
- Stirratt, M.J.; Dunbar-Jacob, J.; Crane, H.M.; Simoni, J.M.; Czajkowski, S.; Hilliard, M.E.; Aikens, J.E.; Hunter, C.M.; Velligan, D.I.; Huntley, K.; et al. Self-report measures of medication adherence behavior: Recommendations on optimal use. Transl. Behav. Med. 2015, 5, 470–482. [Google Scholar] [CrossRef] [PubMed]
- Deponti, D.; Maggiorini, D.; Palazzi, C.E. Smartphone’s physiatric serious game. In Proceedings of the 2011 IEEE 1st International Conference on Serious Games and Applications for Health (SeGAH), Braga, Portugal, 16–18 November 2011; IEEE: Piscataway, NJ, USA, 2011. [Google Scholar]
- Sucar, L.E.; Orihuela-Espina, F.; Velazquez, R.L.; Reinkensmeyer, D.J.; Leder, R.; Hernandez-Franco, J. Gesture therapy: An upper limb virtual reality-based motor rehabilitation platform. IEEE Trans. Neural Syst. Rehabil. Eng. 2013, 22, 634–643. [Google Scholar] [CrossRef] [PubMed]
- Gaggi, O.; Ciman, M. The use of games to help children eyes testing. Multimed. Tools Appl. 2016, 75, 3453–3478. [Google Scholar] [CrossRef]
- Sera, L.; Wheeler, E. Game on: The gamification of the pharmacy classroom. Curr. Pharm. Teach. Learn. 2017, 9, 155–159. [Google Scholar] [CrossRef] [PubMed]
- Schonauer, C.; Pintaric, T.; Kaufmann, H.; Kosterink, S.J.; Vollenbroek-Hutten, M. Chronic pain rehabilitation with a serious game using multimodal input. In Proceedings of the 2011 International Conference on Virtual Rehabilitation, Zurich, Switzerland, 27–29 June 2011; IEEE: Piscataway, NJ, USA, 2011. [Google Scholar]
- France, C.R.; Thomas, J.S. Virtual immersive gaming to optimize recovery (VIGOR) in low back pain: A phase II randomized controlled trial. Contemp. Clin. Trials 2018, 69, 83–91. [Google Scholar] [CrossRef] [PubMed]
- Althoff, T.; White, R.W.; Horvitz, E. Influence of Pokémon Go on physical activity: Study and implications. J. Med. Internet Res. 2016, 18, e315. [Google Scholar] [CrossRef] [PubMed]
- Vernon, H.; Mior, S. The Neck Disability Index: A study of reliability and validity. J. Manip. Physiol. Ther. 1991, 14, 409–415. [Google Scholar]
- Venkatesh, V.; Davis, F.D. A theoretical extension of the technology acceptance model: Four longitudinal field studies. Manag. Sci. 2000, 46, 186–204. [Google Scholar] [CrossRef]
- Benzel, E.C.; Connolly, P.J. The Cervical Spine. Available online: https://books.google.com.hk/books?hl=zh-CN&lr=&id=uIYL14Qs8qoC&oi=fnd&pg=PR1&dq=The+Cervical+Spine&ots=itYrozN3YF&sig=-zpNqSniR4qK1hn6aWt2F5_s6Us&redir_esc=y#v=onepage&q=The%20Cervical%20Spine&f=false. (accessed on 20 May 2024).
- Bernal-Utrera, C.; Gonzalez-Gerez, J.J.; Anarte-Lazo, E.; Rodriguez-Blanco, C. Manual therapy versus therapeutic exercise in non-specific chronic neck pain: A randomized controlled trial. Trials 2020, 21, 682. [Google Scholar] [CrossRef] [PubMed]
- Seo, B.-K.; Lee, J.-H.; Kim, P.-K.; Baek, Y.-H.; Jo, D.-J.; Lee, S. Bee venom acupuncture, NSAIDs or combined treatment for chronic neck pain: Study protocol for a randomized, assessor-blind trial. Trials 2014, 15, 132. [Google Scholar] [CrossRef] [PubMed]
- Bakar, Y.; Sertel, M.; Öztürk, A.; Yümin, E.T.; Tatarli, N.; Ankarali, H. Short term effects of classic massage compared to connective tissue massage on pressure pain threshold and muscle relaxation response in women with chronic neck pain: A preliminary study. J. Manip. Physiol. Ther. 2014, 37, 415–421. [Google Scholar] [CrossRef] [PubMed]
- Witt, C.M.; Jena, S.; Brinkhaus, B.; Liecker, B.; Wegscheider, K.; Willich, S.N. Acupuncture for patients with chronic neck pain. Pain 2006, 125, 98–106. [Google Scholar] [CrossRef] [PubMed]
- De Zoete, R.M.; Armfield, N.R.; McAuley, J.H.; Chen, K.; Sterling, M. Comparative effectiveness of physical exercise interventions for chronic non-specific neck pain: A systematic review with network meta-analysis of 40 randomised controlled trials. Br. J. Sports Med. 2021, 55, 730–742. [Google Scholar] [CrossRef] [PubMed]
- Vincent, K.; Maigne, J.-Y.; Fischhoff, C.; Lanlo, O.; Dagenais, S. Systematic review of manual therapies for nonspecific neck pain. Jt. Bone Spine 2013, 80, 508–515. [Google Scholar] [CrossRef] [PubMed]
- Franke, H.; Franke, J.-D.; Fryer, G. Osteopathic manipulative treatment for chronic nonspecific neck pain: A systematic review and meta-analysis. Int. J. Osteopath. Med. 2015, 18, 255–267. [Google Scholar] [CrossRef]
- Lauche, R.; Langhorst, J.; Dobos, G.J.; Cramer, H. Clinically meaningful differences in pain, disability and quality of life for chronic nonspecific neck pain–a reanalysis of 4 randomized controlled trials of cupping therapy. Complement. Ther. Med. 2013, 21, 342–347. [Google Scholar] [CrossRef] [PubMed]
- Haslam, K.; Doucette, H.; Hachey, S.; MacCallum, T.; Zwicker, D.; Smith-Brilliant, M.; Gilbert, R. YouTube videos as health decision aids for the public: An integrative review. Can. J. Dent. Hyg. 2019, 53, 53. [Google Scholar] [PubMed]
- Price, J.; Rushton, A.; Tyros, I.; Tyros, V.; Heneghan, N.R. Effectiveness and optimal dosage of exercise training for chronic non-specific neck pain: A systematic review with a narrative synthesis. PLoS ONE 2020, 15, e0234511. [Google Scholar] [CrossRef] [PubMed]
- Bobos, P.; Billis, E.; Papanikolaou, D.-T.; Koutsojannis, C.; MacDermid, J.C. Does deep cervical flexor muscle training affect pain pressure thresholds of myofascial trigger points in patients with chronic neck pain? A prospective randomized controlled trial. Rehabil. Res. Pract. 2016, 2016, 6480826. [Google Scholar] [CrossRef] [PubMed]
- Rudolfsson, T.; Djupsjöbacka, M.; Häger, C.; Björklund, M. Effects of neck coordination exercise on sensorimotor function in chronic neck pain: A randomized controlled trial. J. Rehabil. Med. 2014, 46, 908–914. [Google Scholar] [CrossRef] [PubMed]
- Yildiz, T.I.; Turgut, E.; Duzgun, I. Neck and Scapula-Focused Exercise Training on Patients With Nonspecific Neck Pain: A Randomized Controlled Trial. J. Sport Rehabil. 2018, 27, 403–412. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Lin, C.; Liu, C.; Ke, S.; Wan, Q.; Luo, H.; Huang, Z.; Xin, W.; Ma, C.; Wu, S. Comparison of the effectiveness of resistance training in women with chronic computer-related neck pain: A randomized controlled study. Int. Arch. Occup. Environ. Health 2017, 90, 673–683. [Google Scholar] [CrossRef] [PubMed]
- Suvarnnato, T.; Puntumetakul, R.; Uthaikhup, S.; Boucaut, R. Effect of specific deep cervical muscle exercises on functional disability, pain intensity, craniovertebral angle, and neck-muscle strength in chronic mechanical neck pain: A randomized controlled trial. J. Pain Res. 2019, 12, 915–925. [Google Scholar] [CrossRef] [PubMed]
- Price, J.; Rushton, A.; Tyros, I.; Heneghan, N.R. Effectiveness and optimal dosage of resistance training for chronic non-specific neck pain: A protocol for a systematic review with a qualitative synthesis and meta-analysis. BMJ Open 2019, 9, e025158. [Google Scholar] [CrossRef] [PubMed]
- Shiravi, S.; Letafatkar, A.; Bertozzi, L.; Pillastrini, P.; Tazji, M.K. Efficacy of Abdominal Control Feedback and Scapula Stabilization Exercises in Participants With Forward Head, Round Shoulder Postures and Neck Movement Impairment. Sports Health 2019, 11, 272–279. [Google Scholar] [CrossRef] [PubMed]
- Borisut, S.; Vongsirinavarat, M.; Vachalathiti, R.; Sakulsriprasert, P. Effects of strength and endurance training of superficial and deep neck muscles on muscle activities and pain levels of females with chronic neck pain. J. Phys. Ther. Sci. 2013, 25, 1157–1162. [Google Scholar] [CrossRef] [PubMed]
- Falla, D.; Lindstrøm, R.; Rechter, L.; Boudreau, S.; Petzke, F. Effectiveness of an 8-week exercise programme on pain and specificity of neck muscle activity in patients with chronic neck pain: A randomized controlled study. Eur. J. Pain 2013, 17, 1517–1528. [Google Scholar] [CrossRef] [PubMed]
- Gupta, B.D.; Aggarwal, S.; Gupta, B.; Gupta, M.; Gupta, N. Effect of deep cervical flexor training vs. conventional isometric training on forward head posture, pain, neck disability index in dentists suffering from chronic neck pain. J. Clin. Diagn. Res. JCDR 2013, 7, 2261. [Google Scholar] [CrossRef] [PubMed]
- Gallego Izquierdo, T.; Pecos-Martin, D.; Lluch Girbés, E.; Plaza-Manzano, G.; Rodriguez Caldentey, R.; Mayor Melus, R.; Blanco Mariscal, D.; Falla, D. Comparison of cranio-cervical flexion training versus cervical proprioception training in patients with chronic neck pain: A randomized controlled clinical trial. J. Rehabil. Med. 2016, 48, 48–55. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.Y.; Kwag, K.I. Clinical effects of deep cervical flexor muscle activation in patients with chronic neck pain. J. Phys. Ther. Sci. 2016, 28, 269–273. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.-W.; Kim, W.-H. Effect of thoracic manipulation and deep craniocervical flexor training on pain, mobility, strength, and disability of the neck of patients with chronic nonspecific neck pain: A randomized clinical trial. J. Phys. Ther. Sci. 2016, 28, 175–180. [Google Scholar] [CrossRef] [PubMed]
- Randløv, A.; Østergaard, M.; Manniche, C.; Kryger, P.; Jordan, A.; Heegaardand, S.; Holm, B. Intensive dynamic training for females with chronic neck/shoulder pain. A randomized controlled trial. Clin. Rehabil. 1998, 12, 200–210. [Google Scholar] [CrossRef] [PubMed]
- Uluğ, N.; Kara, M.; Özçakar, L. Effects of Pilates and yoga in patients with chronic neck pain: A sonographic study. J. Rehabil. Med. 2018, 50, 80–85. [Google Scholar] [CrossRef]
- Chung, S.; Jeong, Y.-G. Effects of the craniocervical flexion and isometric neck exercise compared in patients with chronic neck pain: A randomized controlled trial. Physiother. Theory Pract. 2018, 34, 916–925. [Google Scholar] [CrossRef] [PubMed]
- Baranowski, T.; Blumberg, F.; Buday, R.; DeSmet, A.; Fiellin, L.E.; Green, C.S.; Kato, P.M.; Lu, A.S.; Maloney, A.E.; Mellecker, R. Games for Health for Children-Current Status and Needed Research. Games Health J. 2016, 5, 1–12. [Google Scholar] [PubMed]
- Jandoo, T. WHO guidance for digital health: What it means for researchers. Digit. Health 2020, 6, 2055207619898984. [Google Scholar] [CrossRef] [PubMed]
- Seo, Y.-C.; Yong, S.Y.; Choi, W.W.; Kim, S.H. Meta-Analysis of Studies on the Effects of Digital Therapeutics. J. Pers. Med. 2024, 14, 157. [Google Scholar] [CrossRef] [PubMed]
- Sweetser, P.; Wyeth, P. GameFlow: A model for evaluating player enjoyment in games. Comput. Entertain. (CIE) 2005, 3, 3. [Google Scholar] [CrossRef]
- Chen, J. Flow in games (and everything else). Commun. ACM 2007, 50, 31–34. [Google Scholar] [CrossRef]
- Schulz, K.F.; Grimes, D.A. The Lancet Handbook of Essential Concepts In Clinical Research; Elsevier: Amsterdam, The Netherlands, 2006. [Google Scholar]
- Norman, G. Likert scales, levels of measurement and the “laws” of statistics. Adv. Health Sci. Educ. Theory Pract. 2010, 15, 625–632. [Google Scholar] [CrossRef] [PubMed]
- Liu, F.; Zhou, F.; Zhao, M.; Fang, T.; Chen, M.; Yan, X. Acupotomy Therapy for Chronic Nonspecific Neck Pain: A Systematic Review and Meta-Analysis. Evid. -Based Complement. Altern. Med. 2017, 2017, 6197308. [Google Scholar] [CrossRef] [PubMed]
- Kloster, M.; Babic, A. Mobile VR-Application for Neck Exercises; IOS Press: Amsterdam, The Netherlands, 2019. [Google Scholar]
- Chattha, U.A.; Janjua, U.I.; Anwar, F.; Madni, T.M.; Cheema, M.F.; Janjua, S.I. Motion sickness in virtual reality: An empirical evaluation. IEEE Access 2020, 8, 130486–130499. [Google Scholar] [CrossRef]
- Zhou, P.; Qi, J.; Duan, A.; Huo, S.; Wu, Z.; Navarro-Alarcon, D. Imitating tool-based garment folding from a single visual observation using hand-object graph dynamics. IEEE Trans. Ind. Inform. 2024, 20, 6245–6256. [Google Scholar] [CrossRef]


| Treatment Type | Description |
|---|---|
| Drugs [19] | Medication such as non-steroidal anti-inflammatory drugs (NSAIDs) |
| Cervical Massage [20] | Uses manipulation or instruments (such as a massage hammer, massage pad, and massage chair) to stimulate specific parts of the human body |
| Acupuncture [21] | A traditional Chinese practice involves the insertion of fine needles into specific points on the body to balance the flow of energy. |
| Physical Exercise [22] | Exercise that includes neck stretching and training |
| Manual Therapy [23] | Delivered by specially trained physicians, using muscle techniques to relax tight muscles |
| Osteopathic manipulative treatment [24] | A variety of techniques applied by osteopathic physicians to manipulate the body’s musculoskeletal system |
| Cupping Therapy [25] | Alternative medicine technique involving suction cups placed on the skin; promotes blood flow and muscle relaxation |
| Researcher | Description of the Intervention Method | Number of Participants |
|---|---|---|
| Bobos et al., 2016 [28] | Move the head backward in a sitting position; Move the head forward in a sitting position; Move the head to the left in a sitting position; Move the head to the right in a sitting position. | 67 |
| Chung et al., 2018 [43] | Isometric neck flexion/extension/rotation/lateral flexion in a seated position using hands as counter resistance; 3 workouts per week; perform 10–15 repetitions of each workout with 10 s of holding and 15 s of rest. | 41 |
| Yildiz et al., 2017 [30] | Cervical spine extension (anterior and posterior recession exercises using a towel/elastic band as a resistance hold). | 30 |
| Shiravi et al., 2019 [34] | Press the top of your head (hold your hand on your forehead); retraction and outward rotation. | 135 |
| Components | Corresponding Design |
|---|---|
| Gamified interaction methods | Using the gyroscope on the phone helps users to conduct gamified motion-sensing interaction. |
| Behavioral determinants | Transform the habit of using smartphones into a motion-sensing interaction for gamified exercise. |
| Behavioral intervention | Help users reduce sedentary behavior through gamified interactive content. |
| Identification of Antecedents of health Problems | Help users reduce their resistance and fear in learning neck exercises. These exercises can be completed using only one mobile phone, dispelling concerns about space and equipment restrictions. |
| Achievement of health goals | Enhancing users’ awareness of cervical spine care, imparting exercise skills, preventing cervical spondylosis, and reducing sedentary behavior. |
| Factor | Major Functions and Design |
|---|---|
| Digital health | Provide information on cervical spine healthcare teaching content |
| Digital healthcare | Infer the user’s cervical spine health status based on the user’s cervical spine movement angle information |
| Digital therapeutics | Provide cervical spine health exercise program with clinical evidence to improve users’ cervical spine health condition |
| Factor | Corresponding Design |
|---|---|
| Attention | “Find the Stars” interactive content design |
| Challenge | Learn how to perform neck exercises and the timings of the exercises |
| Player skill | High-precision digital model demonstration animation, gamified interactive guidelines |
| Control | Full-angle motion-sensing exploration in virtual space |
| Clear goal | Science-based star position setting and interaction sequence arrangement in virtual space |
| Feedback | Gamified visual feedback and sound feedback |
| Immersion | Realistic physical settings and scenarios |
| Social interaction | Reasonable virtual asset rewards |
| Question | Pre-Intervention | Post-Intervention | Change |
|---|---|---|---|
| Pain Intensity | 2.2 | 2.1 | −0.1 |
| Lifting | 1.9 | 1.9 | / |
| Personal Care | 0.5 | 0.4 | −0.1 |
| Reading | 1.2 | 1.3 | +0.1 |
| Headaches | 1.6 | 1.5 | −0.1 |
| Concentration | 1.8 | 1.8 | / |
| Work | 2.0 | 2.2 | +0.2 |
| Driving | 1.4 | 1.4 | / |
| Sleeping | 1.5 | 1.7 | +0.2 |
| Recreation | 0.7 | 0.7 | / |
| Mean | 1.48 | 1.50 | +0.02 |
| Question | Pre-Intervention | Post-Intervention | Change |
|---|---|---|---|
| Pain Intensity | 2.1 | 1.7 | −0.4 |
| Lifting | 2.0 | 1.8 | −0.2 |
| Personal Care | 0.6 | 0.4 | −0.2 |
| Reading | 1.3 | 1.3 | / |
| Headaches | 1.5 | 1.4 | −0.1 |
| Concentration | 2.0 | 1.8 | −0.2 |
| Work | 1.9 | 1.9 | +0.1 |
| Driving | 1.6 | 1.2 | −0.4 |
| Sleeping | 1.8 | 1.3 | −0.5 |
| Recreation | 0.6 | 0.4 | −0.2 |
| Mean | 1.54 | 1.24 | −0.3 |
| Question | Min | Max | Mean | SD | p Value |
|---|---|---|---|---|---|
| What is your level of cervical stretching sensation when you are doing a head-up maneuver? | 3.000 | 5.000 | 4.100 | 0.738 | p < 0.001 |
| What is your level of cervical stretching sensation when you are doing a head-down maneuver? | 2.000 | 5.000 | 3.400 | 0.843 | p < 0.001 |
| What is your level of cervical stretching sensation when you look to the left? | 4.000 | 5.000 | 4.300 | 0.483 | p < 0.001 |
| What is your level of cervical stretching sensation when you look to the right? | 4.000 | 5.000 | 4.300 | 0.483 | p < 0.001 |
| What is your level of cervical stretching sensation when you do the left backward-looking maneuver? | 3.000 | 5.000 | 4.400 | 0.843 | p < 0.001 |
| What is your level of cervical stretching sensation when you do the right backward-looking maneuver? | 3.000 | 5.000 | 4.500 | 0.707 | p < 0.001 |
| Question | Min | Max | Mean | SD | p Value |
|---|---|---|---|---|---|
| Exercising with the app helps me relax my cervical spine. | 6.000 | 11.000 | 9.200 | 1.398 | p < 0.001 |
| Exercising with the app helps me reduce my sedentary time. | 4.000 | 11.000 | 8.500 | 2.068 | p < 0.001 |
| Exercising with the app improves my willingness to get up and walk. | 4.000 | 11.000 | 8.600 | 1.955 | p < 0.001 |
| Exercising with the app helps me be more aware of my cervical spine health. | 6.000 | 11.000 | 8.900 | 1.663 | p < 0.001 |
| Exercising with the app is useful. | 6.000 | 11.000 | 9.100 | 1.595 | p < 0.001 |
| Question | Min | Max | Mean | SD | p Value |
|---|---|---|---|---|---|
| I like to use the “Find the Stars” interactive workout in the app. | 8.000 | 11.000 | 9.400 | 0.843 | p < 0.001 |
| I’m positive about the interactive exercise function of the app. | 8.000 | 11.000 | 9.500 | 0.850 | p < 0.001 |
| I think the app’s interactive workout design is an innovative feature. | 8.000 | 11.000 | 9.700 | 0.949 | p < 0.001 |
| If I’m using the app, I’ll continue to use the Somatic Interaction feature to relax my cervical spine | 5.000 | 11.000 | 9.200 | 1.687 | p < 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sun, Y.; Xian, Y.; Lin, H.; Sun, X. Enhancing the Management of Non-Specific Neck Pain through Gamification: Design and Efficacy of a Health Application. Bioengineering 2024, 11, 640. https://doi.org/10.3390/bioengineering11070640
Sun Y, Xian Y, Lin H, Sun X. Enhancing the Management of Non-Specific Neck Pain through Gamification: Design and Efficacy of a Health Application. Bioengineering. 2024; 11(7):640. https://doi.org/10.3390/bioengineering11070640
Chicago/Turabian StyleSun, Yiran, Yanjie Xian, Hongbo Lin, and Xing Sun. 2024. "Enhancing the Management of Non-Specific Neck Pain through Gamification: Design and Efficacy of a Health Application" Bioengineering 11, no. 7: 640. https://doi.org/10.3390/bioengineering11070640
APA StyleSun, Y., Xian, Y., Lin, H., & Sun, X. (2024). Enhancing the Management of Non-Specific Neck Pain through Gamification: Design and Efficacy of a Health Application. Bioengineering, 11(7), 640. https://doi.org/10.3390/bioengineering11070640






