The Clinical Usability Evaluation of an Attachable Video Laryngoscope in the Simulated Tracheal Intubation Scenario: A Manikin Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Scenario Simulation
2.2. Recruitment of Participants
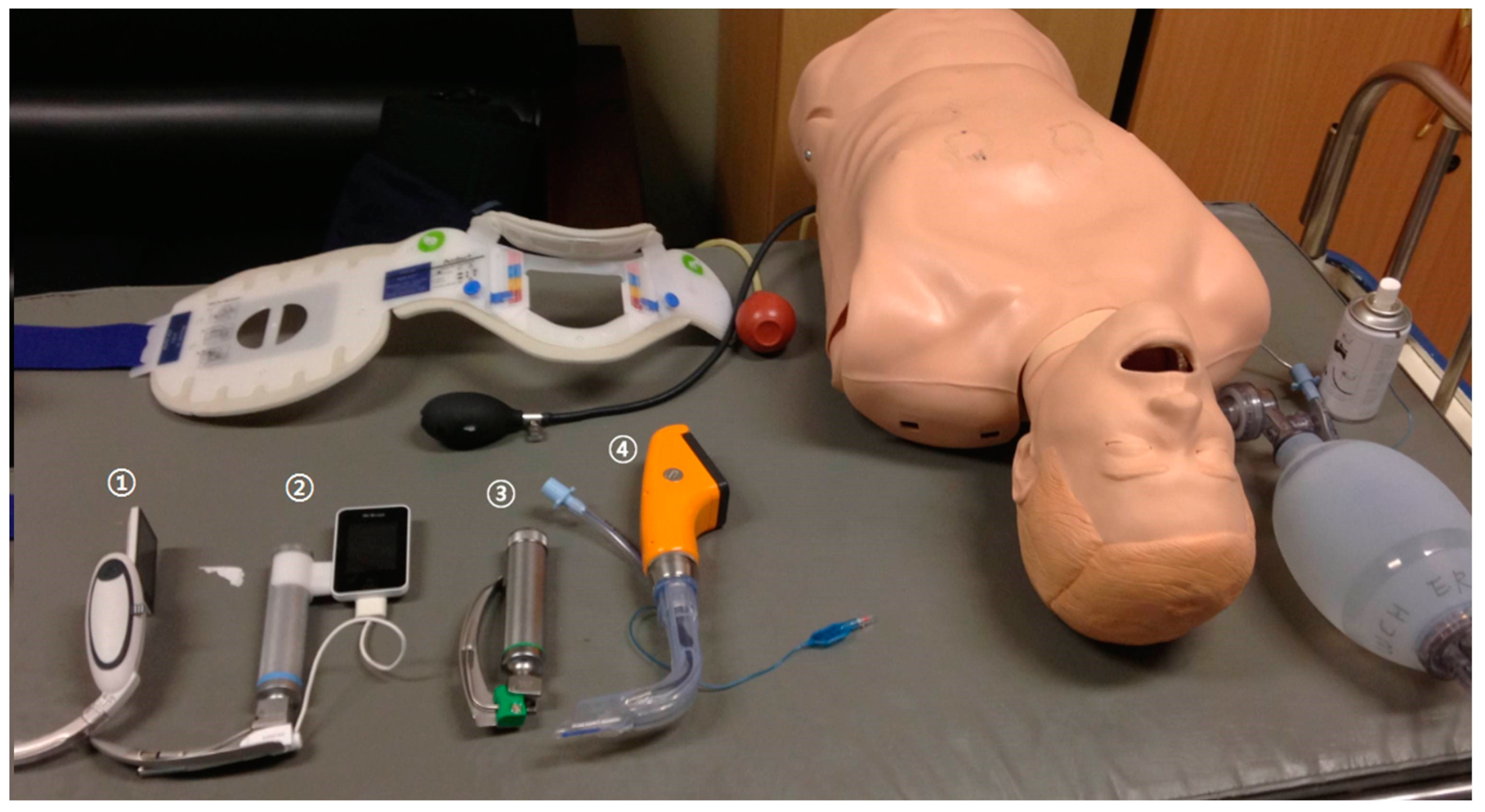
2.3. Equipment
2.4. Data Collection
2.5. Outcomes of Treatment
2.6. Statistical Analyses
3. Results
3.1. Comparative Assessment of Device in the Skilled Group
3.2. Comparative Assessment of Device in the Unskilled Group
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Griesdale, D.E.; Bosma, T.L.; Kurth, T.; Isac, G.; Chittock, D.R. Complications of endotracheal intubation in the critically ill. Intensive Care Med. 2008, 34, 1835–1842. [Google Scholar] [CrossRef]
- Jaber, S.; Amraoui, J.; Lefrant, J.-Y.; Arich, C.; Cohendy, R.; Landreau, L.; Calvet, Y.; Capdevila, X.; Mahamat, A.; Eledjam, J.-J. Clinical practice and risk factors for immediate complications of endotracheal intubation in the intensive care unit: A prospective, multiple-center study. Crit. Care Med. 2006, 34, 2355–2361. [Google Scholar] [CrossRef]
- Mort, T.C. Complications of emergency tracheal intubation: Hemodynamic alterations-part I. J. Intensive Care Med. 2007, 22, 157–165. [Google Scholar] [CrossRef]
- Martin, L.D.; Mhyre, J.M.; Shanks, A.M.; Tremper, K.K.; Kheterpal, S. 3423 emergency tracheal intubations at a university hospital: Airway outcomes and complications. J. Am. Soc. Anesthesiol. 2011, 114, 42–48. [Google Scholar] [CrossRef] [PubMed]
- Nouruzi-Sedeh, P.; Schumann, M.; Groeben, H. Laryngoscopy via Macintosh blade versus GlideScope: Success rate and time for endotracheal intubation in untrained medical personnel. J. Am. Soc. Anesthesiol. 2009, 110, 32–37. [Google Scholar] [CrossRef] [PubMed]
- Griesdale, D.E.; Liu, D.; McKinney, J.; Choi, P.T. Glidescope® video-laryngoscopy versus direct laryngoscopy for endotracheal intubation: A systematic review and meta-analysis. Can. J. Anaesth. 2012, 59, 41. [Google Scholar] [CrossRef]
- Orebaugh, S.L. Difficult airway management in the emergency department. J. Emerg. Med. 2002, 22, 31–48. [Google Scholar] [CrossRef] [PubMed]
- Pintarič, T.S. Videolaryngoscopy as a primary intubation modality in obstetrics: A narrative review of current evidence. Biomol. Biomed. 2023, 23, 949. [Google Scholar]
- Myatra, S.N.; Patwa, A.; Divatia, J.V. Videolaryngoscopy for all intubations: Is direct laryngoscopy obsolete? Indian J. Anaesth. 2022, 66, 169–173. [Google Scholar] [CrossRef]
- Scott-Brown, S.; Russell, R. Video laryngoscopes and the obstetric airway. Int. J. Obstet. Anesth. 2015, 24, 137–146. [Google Scholar] [CrossRef]
- Arulkumaran, N.; Lowe, J.; Ions, R.; Mendoza, M.; Bennett, V.; Dunser, M.W. Video laryngoscopy versus direct laryngoscopy for emergency orotracheal intubation outside the operating room: A systematic review and meta-analysis. Br. J. Anaesth. 2018, 120, 712–724. [Google Scholar] [CrossRef] [PubMed]
- Zaouter, C.; Calderon, J.; Hemmerling, T.M. Videolaryngoscopy as a new standard of care. Br. J. Anaesth. 2015, 114, 181–183. [Google Scholar] [CrossRef] [PubMed]
- Doglioni, N.; Cavallin, F.; Zanardo, V.; Trevisanuto, D. Intubation training in neonatal patients: A review of one trainee’s first 150 procedures. J. Matern. -Fetal Neonatal Med. 2012, 25, 1302–1304. [Google Scholar] [CrossRef]
- Uchinami, Y.; Fujita, N.; Ando, T.; Mizunoya, K.; Hoshino, K.; Yokota, I.; Morimoto, Y. The relationship between years of anesthesia experience and first-time intubation success rate with direct laryngoscope and video laryngoscope in infants: A retrospective observational study. J. Anesth. 2022, 36, 707–714. [Google Scholar] [CrossRef] [PubMed]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G* Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.G. Statistical power analyses using G* Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef] [PubMed]
- Cummins, R.O. ACLS: Principles and Practice; American Heart Association: Dallas, TX, USA, 2004. [Google Scholar]
- Cormack, R.S. Cormack–Lehane classification revisited. Br. J. Anaesth. 2010, 105, 867–868. [Google Scholar] [CrossRef] [PubMed]
- Si, J.W.; Lee, S.B.; Do, B.S. Comparison of the Macintosh laryngoscope and the GlideScope (R) video laryngoscope in easy and simulated difficult airway scenarios: A manikin study. J. Korean Soc. Emerg. Med. 2009, 20, 604–608. [Google Scholar]
- Tan, B.H.; Liu, E.H.C.; Lim, R.T.C.; Liow, L.M.H.; Goy, R.W.L. Ease of intubation with the GlideScope or Airway Scope by novice operators in simulated easy and difficult airways–a manikin study. Anaesthesia 2009, 64, 187–190. [Google Scholar] [CrossRef] [PubMed]
- Malik, M.A.; Hassett, P.; Carney, J.; Higgins, B.D.; Harte, B.H.; Laffey, J.G. A comparison of the Glidescope®, Pentax AWS®, and Macintosh laryngoscopes when used by novice personnel: A manikin study. Can. J. Anesth. 2009, 56, 802–811. [Google Scholar] [CrossRef]
- Wang, P.K.; Huang, C.C.; Lee, Y.; Chen, T.Y.; Lai, H.Y. Comparison of 3 video laryngoscopes with the Macintosh in a manikin with easy and difficult simulated airways. Am. J. Emerg. Med. 2013, 31, 330–338. [Google Scholar] [CrossRef] [PubMed]
- Phillips, S.; Celenza, A. Comparison of the Pentax AWS videolaryngoscope with the Macintosh laryngoscope in simulated difficult airway intubations by emergency physicians. Am. J. Emerg. Med. 2011, 29, 863–867. [Google Scholar] [CrossRef] [PubMed]
- Brown, C.A., III; Bair, A.E.; Pallin, D.J.; Walls, R.M.; Near III Investigators. Techniques, success, and adverse events of emergency department adult intubations. Ann. Emerg. Med. 2015, 65, 363–370. [Google Scholar] [CrossRef]
- Prekker, M.E.; Driver, B.E.; Trent, S.A.; Resnick-Ault, D.; Seitz, K.P.; Russell, D.W.; Gaillard, J.P.; Latimer, A.J.; Ghamande, S.A.; Gibbs, K.W.; et al. Video versus direct laryngoscopy for tracheal intubation of critically ill adults. N. Engl. J. Med. 2023, 389, 418–429. [Google Scholar] [CrossRef] [PubMed]
- Collins, S.R. Direct and Indirect Laryngoscopy: Equipment and Techniques Discussion. Respir. Care 2014, 59, 850–864. [Google Scholar] [CrossRef] [PubMed]
- Szarpak, L.; Kurowski, A.; Czyzewski, L.; Rodríguez-Núñez, A. Video rigid flexing laryngoscope (RIFL) vs Miller laryngoscope for tracheal intubation during pediatric resuscitation by paramedics: A simulation study. Am. J. Emerg. Med. 2015, 33, 1019–1024. [Google Scholar] [CrossRef]
- Ayyan, S.M.; Ali, Z. New assembled video laryngoscope: A study on efficacy and cost-effectiveness. Crit. Care 2015, 19 (Suppl. S1), P202. [Google Scholar] [CrossRef]
- Donald, E.; Griesdale, G.; Chau, A.; Isac, G.; Ayas, N.; Foster, D.; Choi, P. Video-laryngoscopy versus direct laryngoscopy in critically ill patients: A pilot randomized trial. Can. J. Anesth. 2012, 59, 1032. [Google Scholar]
- Yong, S.A.; Chaou, C.H.; Yu, S.R.; Kuan, J.T.; Lin, C.C.; Liu, H.P.; Chiu, T.F. Video assisted laryngoscope facilitates intubation skill learning in the emergency department. J. Acute Med. 2020, 10, 60. [Google Scholar]
- Aziz, M.F.; Dillman, D.; Fu, R.; Brambrink, A.M. Comparative effectiveness of the C-MAC video laryngoscope versus direct laryngoscopy in the setting of the predicted difficult airway. J. Am. Soc. Anesthesiol. 2012, 116, 629–636. [Google Scholar] [CrossRef]
- Mendonca, C.; Mesbah, A.; Velayudhan, A.; Danha, R. A randomised clinical trial comparing the flexible fibrescope and the Pentax Airway Scope (AWS)® for awake oral tracheal intubation. Anaesthesia 2016, 71, 908–914. [Google Scholar] [CrossRef] [PubMed]
- Thong, S.Y.; Lim, Y. Video and optic laryngoscopy assisted tracheal intubation–the new era. Anaesth. Intensive Care 2009, 37, 219–233. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.J.; Kang, H.G.; Lim, T.H.; Chung, H.S.; Cho, J.; Oh, Y.M.; Kim, Y.M. Endotracheal intubation using a GlideScope video laryngoscope by emergency physicians: A multicentre analysis of 345 attempts in adult patients. Emerg. Med. J. 2010, 27, 380–382. [Google Scholar] [CrossRef] [PubMed]
- Pirlich, N.; Piepho, T.; Gervais, H.; Noppens, R.R. Indirekte Laryngoskopie/Videolaryngoskopie. Übersicht über in Deutschland verwendete Instrumente in der Notfall- und Intensivmedizin [Indirect laryngoscopy/video laryngoscopy. A review of devices used in emergency and intensive care medicine in Germany. Med. Klin. Intensivmed. Notfallmedizin 2012, 107, 521–530. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Chung, S.P.; Park, I.C.; Cho, J.; Lee, H.S.; Park, Y.S. Comparison of the GlideScope video laryngoscope and Macintosh laryngoscope in simulated tracheal intubation scenarios. Emerg. Med. J. 2008, 25, 279–282. [Google Scholar] [CrossRef] [PubMed]
- Narang, A.T.; Oldeg, P.F.; Medzon, R.; Mahmood, A.R.; Spector, J.A.; Robinett, D.A. Comparison of intubation success of video laryngoscopy versus direct laryngoscopy in the difficult airway using high-fidelity simulation. Simul. Healthc. 2009, 4, 160–165. [Google Scholar] [CrossRef]
- Kariya, T.; Inagawa, G.; Nakamura, K.; Fujimoto, J.; Aoi, Y.; Morita, S.; Goto, T. Evaluation of the Pentax-AWS® and the Macintosh laryngoscope in difficult intubation: A manikin study. Acta Anaesthesiol. Scand. 2011, 55, 223–227. [Google Scholar] [CrossRef]


| AVL | CML | AWS | MAC | p-Value | |
|---|---|---|---|---|---|
| Normal Airway | |||||
| Success Rate, n(%) | 9(90) | 10(100) | 10(100) | 10(100) | 0.38 |
| Tracheal Intubation Time, sec [M ± S.D *, IQR] | 13.4 ± 5.5 * | 15.0 [10.5–16.7] | 11.6 [9.2–15.3] | 16.1 ± 10.5 * | 0.68 |
| Grade of Glottic View, n(%) | <0.001 | ||||
| I | 10(100) | 3(30) | 10(100) | 8(80) | |
| II | 0 | 7(70) | 0 | 2(20) | |
| III | 0 | 0 | 0 | 0 | |
| IV | 0 | 0 | 0 | 0 | |
| Tongue Edema | |||||
| Success Rate, n(%) | 6(60) | 1(10) | 10(100) | 6(60) | 0.001 |
| Tracheal Intubation Time, sec [M ± S.D *, IQR] | 19.2 [14.4–23.4] | 9.3 [9.3–9.3] | 10.2 [9.8–11.7] | 20.4 [16.6–23.9] | 0.007 |
| Grade of Glottic View, n(%) | <0.001 | ||||
| I | 8(80) | 0 | 9(90) | 7(70) | |
| II | 2(20) | 2(20) | 0 | 1(10) | |
| III | 0 | 3(30) | 1(10) | 1(10) | |
| IV | 0 | 5(50) | 0 | 1(10) | |
| Degree of Difficulty of Use [M ± S.D *, IQR] | 2.8 [2.1–4.3] | 7.8 [5.5–8.1] | 1.5 [0.4–2.6] | 5.3 [3.9–5.8] | <0.001 |
| AVL | CML | AWS | MAC | p-Value | |
|---|---|---|---|---|---|
| Normal Airway | |||||
| Success Rate, n(%) | 6(60) | 5(50) | 8(80) | 9(90) | 0.19 |
| Tracheal Intubation Time, sec [M ± S.D *, IQR] | 18.8 [11.4–21.8] | 15.7 [12.5–24.5] | 19.6 ± 7.7 * | 13.4 [10.9–17.9] | 0.90 |
| Grade of Glottic View, n(%) | <0.001 | ||||
| I | 10(100) | 3(30) | 10(100) | 9(90) | |
| II | 0 | 7(70) | 0 | 1(10) | |
| III | 0 | 0 | 0 | 0 | |
| IV | 0 | 0 | 0 | 0 | |
| Tongue Edema | |||||
| Success Rate, n(%) | 4(40) | 1(10) | 8(80) | 6(60) | 0.12 |
| Tracheal Intubation Time, sec [M ± S.D *, IQR] | 23.3 [18.8–27.3] | 26.7 [26.7–26.7] | 17.2 ± 11.9 * | 27.2 ± 22.7 * | 0.13 |
| Grade of Glottic View, n(%) | <0.001 | ||||
| I | 10(100) | 0 | 9(90) | 8(80) | |
| II | 0 | 2(20) | 0 | 2(20) | |
| III | 0 | 4(40) | 1(10) | 0 | |
| IV | 0 | 4(40) | 0 | 0 | |
| Degree of Difficulty of Use [M ± S.D *, IQR] | 3.3 [3.1–4.9] | 8.8 [6.9–9.1] | 0.7 [0.1–1.8] | 2.4 [2.0–3.3] | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, W.-J.; Lee, H.-Y.; Kim, S.-J.; Lee, K.-H. The Clinical Usability Evaluation of an Attachable Video Laryngoscope in the Simulated Tracheal Intubation Scenario: A Manikin Study. Bioengineering 2024, 11, 570. https://doi.org/10.3390/bioengineering11060570
Lee W-J, Lee H-Y, Kim S-J, Lee K-H. The Clinical Usability Evaluation of an Attachable Video Laryngoscope in the Simulated Tracheal Intubation Scenario: A Manikin Study. Bioengineering. 2024; 11(6):570. https://doi.org/10.3390/bioengineering11060570
Chicago/Turabian StyleLee, Won-Jun, Hee-Young Lee, Sun-Ju Kim, and Kang-Hyun Lee. 2024. "The Clinical Usability Evaluation of an Attachable Video Laryngoscope in the Simulated Tracheal Intubation Scenario: A Manikin Study" Bioengineering 11, no. 6: 570. https://doi.org/10.3390/bioengineering11060570
APA StyleLee, W.-J., Lee, H.-Y., Kim, S.-J., & Lee, K.-H. (2024). The Clinical Usability Evaluation of an Attachable Video Laryngoscope in the Simulated Tracheal Intubation Scenario: A Manikin Study. Bioengineering, 11(6), 570. https://doi.org/10.3390/bioengineering11060570









