Mechanical Method for Rapid Determination of Step Count Sensor Settings
Abstract
1. Introduction
2. Materials and Methods
2.1. Continuous Stepper
2.2. Activity Sensor
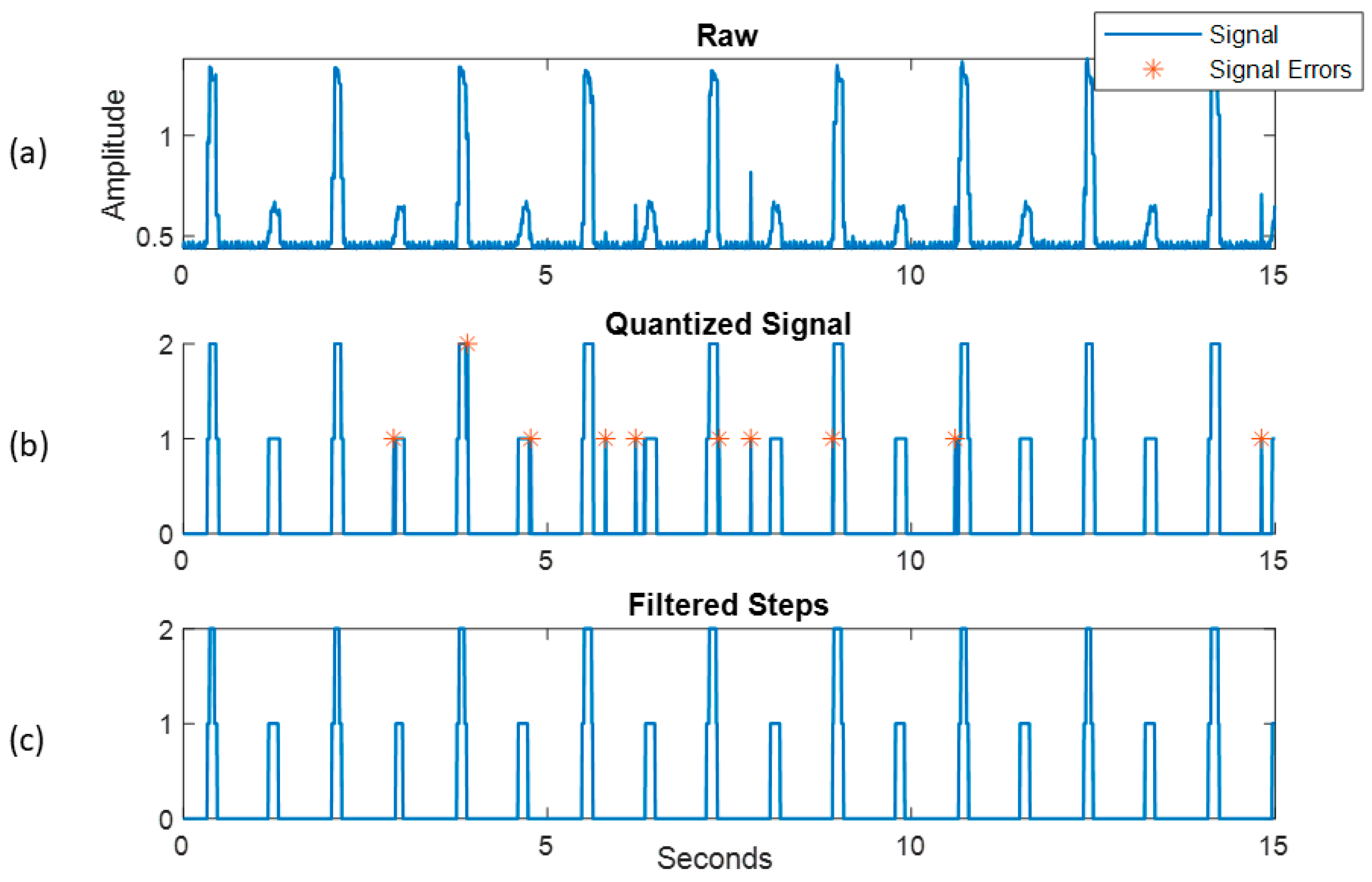
2.3. Signal Processing
2.4. Regression Model
2.5. Data Analysis
3. Results and Discussion
3.1. Model Accuracy
3.2. Model Application
3.3. Disabled and Low-Mobility Ambulator Cadences (30–60 Steps/min)
3.3.1. Threshold
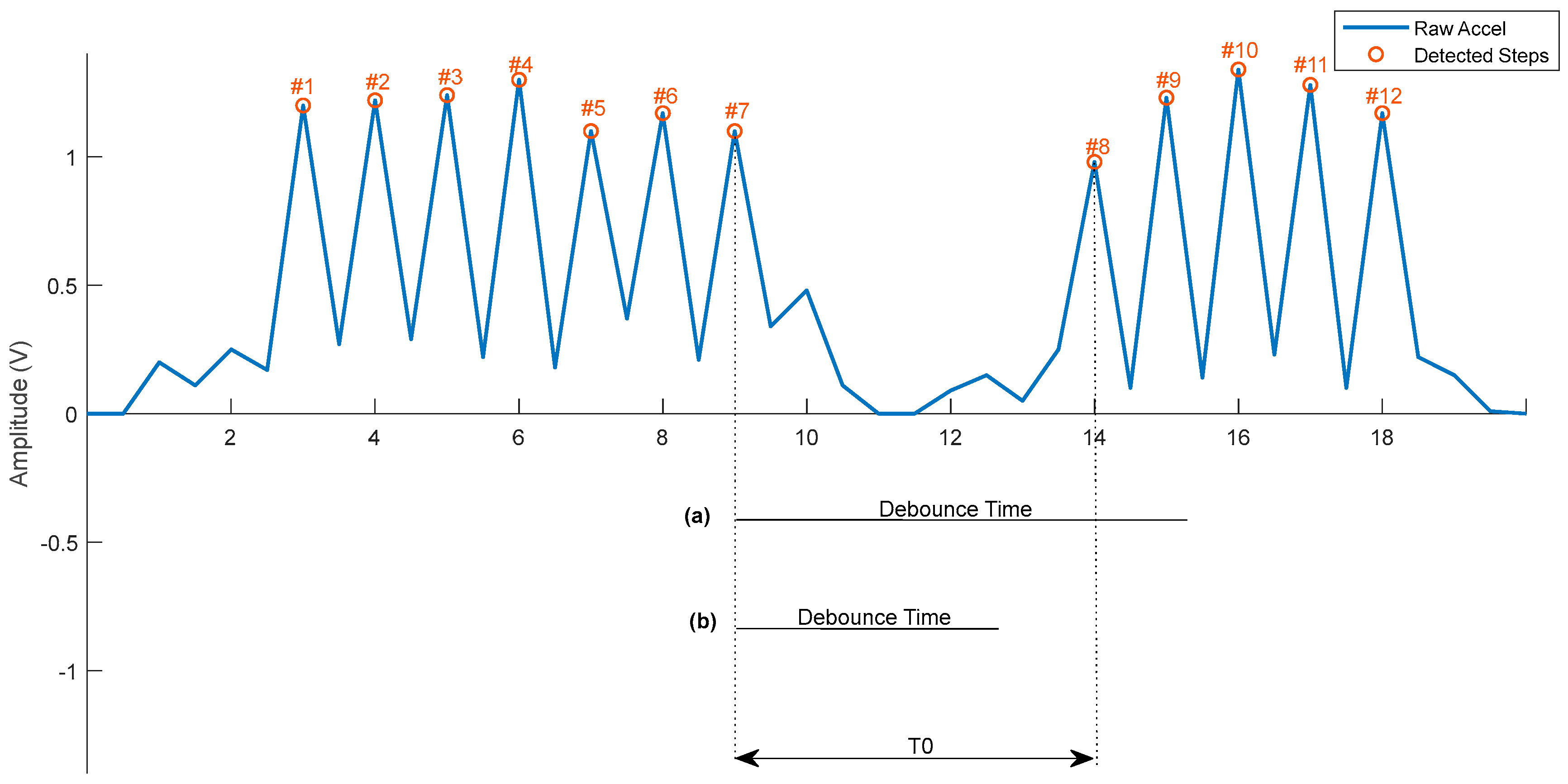
3.3.2. Debounce Time
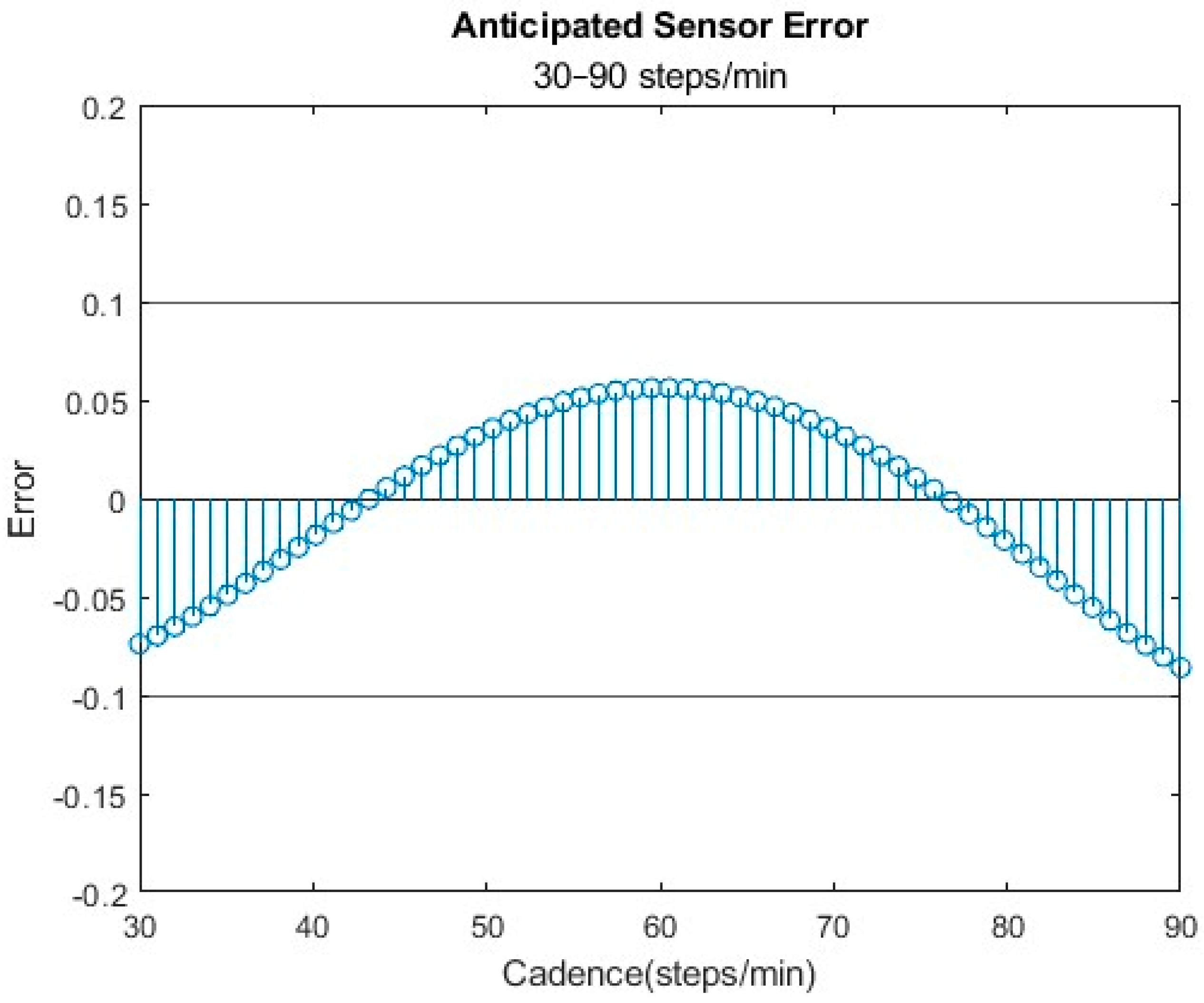
3.4. Disabled and High-Mobility Ambulator Cadences (30–90 Steps/min)
3.4.1. Threshold
3.4.2. Debounce
3.5. Healthy Ambulators (30–110 Steps/min)
3.5.1. Threshold
3.5.2. Debounce
3.6. Steps
3.7. Limitations
3.8. Implications
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dhingra, L.S.; Aminorroaya, A.; Oikonomou, E.K.; Nargesi, A.A.; Wilson, F.P.; Krumholz, H.M.; Khera, R. Use of Wearable Devices in Individuals with or at Risk for Cardiovascular Disease in the US, 2019 to 2020. JAMA Netw. Open 2023, 6, e2316634. [Google Scholar] [CrossRef] [PubMed]
- Henriksen, A.; Haugen Mikalsen, M.; Woldaregay, A.Z.; Muzny, M.; Hartvigsen, G.; Hopstock, L.A.; Grimsgaard, S. Using Fitness Trackers and Smartwatches to Measure Physical Activity in Research: Analysis of Consumer Wrist-Worn Wearables. J. Med. Internet Res. 2018, 20, e110. [Google Scholar] [CrossRef] [PubMed]
- Pieper, N.L.; Lewek, M.D.; Franz, J.R. Can shank acceleration provide a clinically feasible surrogate for individual limb propulsion during walking? J. Biomech. 2020, 98, 109449. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, L.J.H.; Caspi, A.; Ambler, A.; Broadbent, J.M.; Cohen, H.J.; d’Arbeloff, T.; Elliott, M.; Hancox, R.J.; Harrington, H.; Hogan, S.; et al. Association of Neurocognitive and Physical Function with Gait Speed in Midlife. JAMA Netw. Open 2019, 2, e1913123. [Google Scholar] [CrossRef] [PubMed]
- Studenski, S. Gait Speed Reveals Clues to Lifelong Health. JAMA Netw. Open 2019, 2, e1913112. [Google Scholar] [CrossRef] [PubMed]
- Storm, F.A.; Heller, B.W.; Mazzà, C. Step Detection and Activity Recognition Accuracy of Seven Physical Activity Monitors. PLoS ONE 2015, 10, e0118723. [Google Scholar] [CrossRef] [PubMed]
- Beauchet, O.; Annweiler, C.; Lecordroch, Y.; Allali, G.; Dubost, V.; Herrmann, F.R.; Kressig, R.W. Walking speed-related changes in stride time variability: Effects of decreased speed. J. Neuroeng. Rehabil. 2009, 6, 32. [Google Scholar] [CrossRef] [PubMed]
- Nilsson, J.; Thorstensson, A. Ground reaction forces at different speeds of human walking and running. Acta Physiol. Scand. 1989, 136, 217–227. [Google Scholar] [CrossRef] [PubMed]
- Cosoli, G.; Antognoli, L.; Scalise, L. Methods for the metrological characterization of wearable devices for the measurement of physiological signals: State of the art and future challenges. MethodsX 2023, 10, 102038. [Google Scholar] [CrossRef] [PubMed]
- Husted, H.M.; Llewellyn, T.L. The Accuracy of Pedometers in Measuring Walking Steps on a Treadmill in College Students. Int. J. Exerc. Sci. 2017, 10, 146–153. [Google Scholar] [PubMed]
- Fortune, E.; Lugade, V.; Morrow, M.; Kaufman, K. Validity of using tri-axial accelerometers to measure human movement—Part II: Step counts at a wide range of gait velocities. Med. Eng. Phys. 2014, 36, 659–669. [Google Scholar] [CrossRef] [PubMed]
- Fortune, E.; Lugade, V.; Amin, S.; Kaufman, K.R. Step detection using multi- versus single tri-axial accelerometer-based systems. Physiol. Meas. 2015, 36, 2519–2535. [Google Scholar] [CrossRef] [PubMed]
- Mixter, S.; Mathiassen, S.E.; Bjärntoft, S.; Lindfors, P.; Lyskov, E.; Hallman, D.M. Fatigue, Stress, and Performance during Alternating Physical and Cognitive Tasks—Effects of the Temporal Pattern of Alternations. Ann. Work. Expo. Health 2021, 65, 1107–1122. [Google Scholar] [CrossRef] [PubMed]
- iNEMO Inertial Module: Always-on 3D Accelerometer and 3D Gyroscope. ST Life. Augmented, September 2017. Available online: https://www.st.com/en/mems-and-sensors/lsm6dsop.html (accessed on 1 January 2024).
- Cecen, A. MultiPolyregression. Multivariate Polynomial Regression. Github. 2020. Available online: https://github.com/ahmetcecen/MultiPolyRegress-MatlabCentral (accessed on 28 February 2024).
- Bassett, D.R.; Toth, L.P.; LaMunion, S.R.; Crouter, S.E. Step Counting: A Review of Measurement Considerations and Health-Related Applications. Sports Med. 2017, 47, 1303–1315. [Google Scholar] [CrossRef] [PubMed]
- Beisheim, E.H.; Arch, E.S.; Horne, J.R.; Sions, J.M. Performance-based outcome measures are associated with cadence variability during community ambulation among individuals with a transtibial amputation. Prosthet. Orthot. Int. 2020, 44, 215–224. [Google Scholar] [CrossRef] [PubMed]
- McAvoy, C.R.; Miller, T.A.; Aguiar, E.J.; Ducharme, S.W.; Moore, C.C.; Schuna, J.M.; Barreira, T.V.; Chase, C.J.; Gould, Z.R.; Amalbert-Birriel, M.A.; et al. Cadence (steps/min) and relative intensity in 61 to 85-year-olds: The CADENCE-Adults study. Int. J. Behav. Nutr. Phys. Act. 2023, 20, 141. [Google Scholar] [CrossRef] [PubMed]
- Fukuchi, C.A.; Fukuchi, R.K.; Duarte, M. Effects of walking speed on gait biomechanics in healthy participants: A systematic review and meta-analysis. Syst. Rev. 2019, 8, 153. [Google Scholar] [CrossRef]
- Abouhossein, A.; Awad, M.I.; Maqbool, H.F.; Crisp, C.; Stewart, T.D.; Messenger, N.; Richardson, R.C.; Dehghani-Sanij, A.A.; Bradley, D. Foot trajectories and loading rates in a transfemoral amputee for six different commercial prosthetic knees: An indication of adaptability. Med. Eng. Phys. 2019, 68, 46–56. [Google Scholar] [CrossRef] [PubMed]
- Orendurff, M.S. How humans walk: Bout duration, steps per bout, and rest duration. J. Rehabil. Res. Dev. 2008, 45, 1077–1090. [Google Scholar] [CrossRef] [PubMed]
- Carcreff, L.; Gerber, C.N.; Paraschiv-Ionescu, A.; De Coulon, G.; Aminian, K.; Newman, C.J.; Armand, S. Walking Speed of Children and Adolescents with Cerebral Palsy: Laboratory Versus Daily Life. Front. Bioeng. Biotechnol. 2020, 8, 812. [Google Scholar] [CrossRef]
- Takayanagi, N.; Sudo, M.; Yamashiro, Y.; Lee, S.; Kobayashi, Y.; Niki, Y.; Shimada, H. Relationship between Daily and In-laboratory Gait Speed among Healthy Community-dwelling Older Adults. Sci. Rep. 2019, 9, 3496. [Google Scholar] [CrossRef]



| 1st Order | 2nd Order | 3rd Order | 4th Order | 5th Order | |
|---|---|---|---|---|---|
| R-Squared | 0.271 | 0.524 | 0.722 | 0.800 | 0.847 |
| RMSE | 0.086 | 0.0813 | 0.075 | 0.044 | 0.185 |
| CVMAE | 5.085 | 5.295 | 3.383 | 3.589 1 | 4.171 |
| Fit | −0.062 | −0.012 | 0.019 | 0.003 | 0.154 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lundell, S.; Kaufman, K.R. Mechanical Method for Rapid Determination of Step Count Sensor Settings. Bioengineering 2024, 11, 547. https://doi.org/10.3390/bioengineering11060547
Lundell S, Kaufman KR. Mechanical Method for Rapid Determination of Step Count Sensor Settings. Bioengineering. 2024; 11(6):547. https://doi.org/10.3390/bioengineering11060547
Chicago/Turabian StyleLundell, Sydney, and Kenton R. Kaufman. 2024. "Mechanical Method for Rapid Determination of Step Count Sensor Settings" Bioengineering 11, no. 6: 547. https://doi.org/10.3390/bioengineering11060547
APA StyleLundell, S., & Kaufman, K. R. (2024). Mechanical Method for Rapid Determination of Step Count Sensor Settings. Bioengineering, 11(6), 547. https://doi.org/10.3390/bioengineering11060547





