Bone Bruises and Concomitant Meniscus and Cartilage Damage in Anterior Cruciate Ligament Injuries: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Acquisition and Literature Review
2.2. Selection of Studies
2.3. Data Extraction
2.4. Quality Assessment
2.5. Statistical Analyses
3. Results
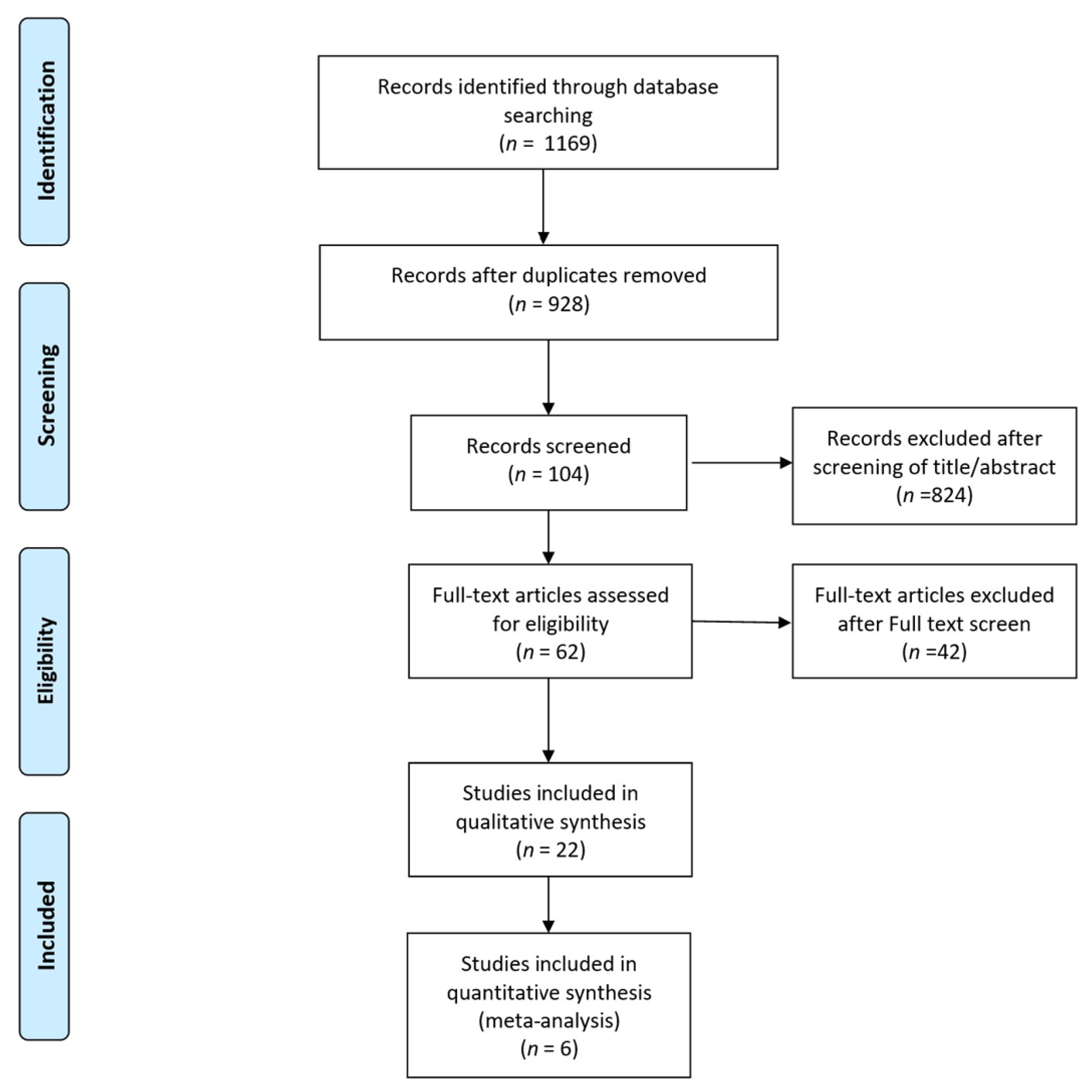
3.1. Literature Selection
3.2. Study Characteristics
3.3. Presence and Distribution of Bone Bruises across Anatomical Locations
3.4. Characteristics of Bone Bruises and Associated Injuries
3.5. Bone Bruises and MM Injuries
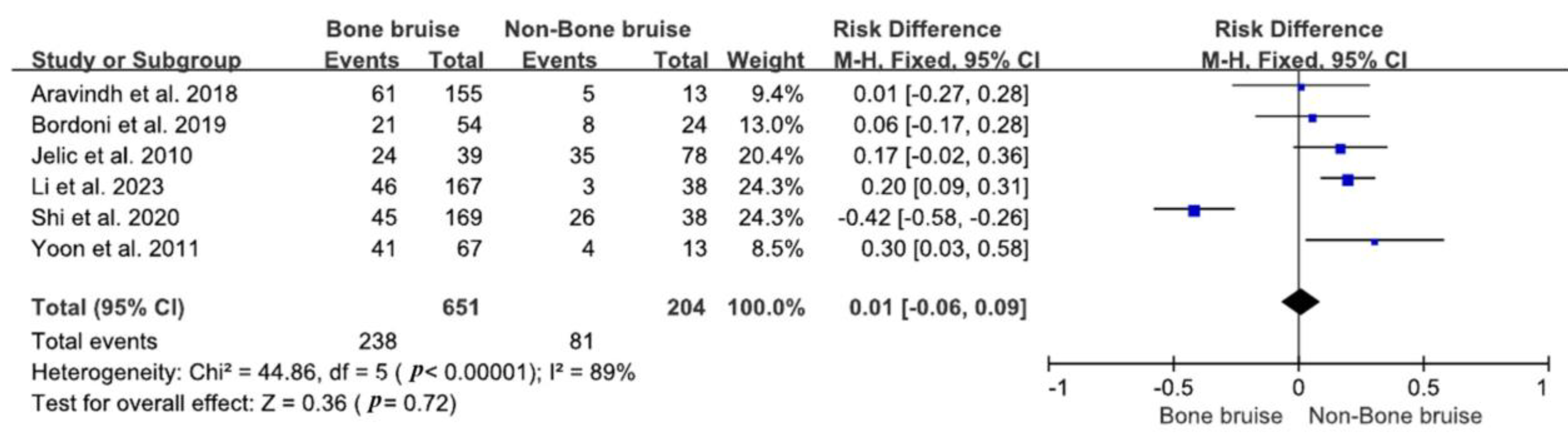
3.6. Bone Bruises and LM Injuries
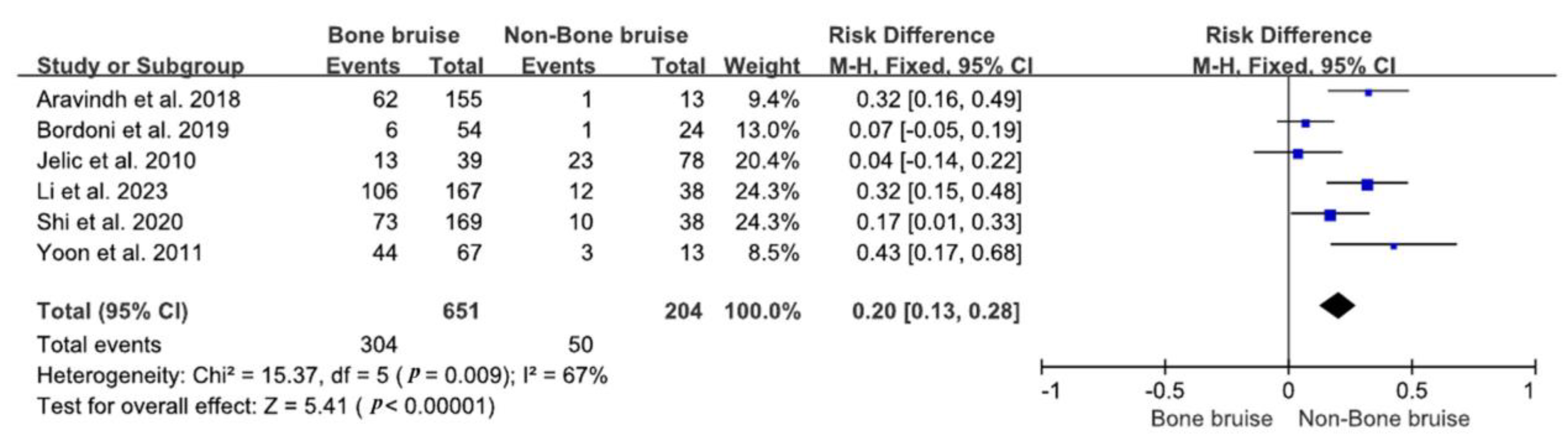
3.7. Bone Bruises and Cartilage Injuries
3.8. The Severity of Bone Bruises and Associated Injuries
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bae, B.S.; Yoo, S.; Lee, S.H. Ramp lesion in anterior cruciate ligament injury: A review of the anatomy, biomechanics, epidemiology, and diagnosis. Knee Surg. Relat. Res. 2023, 35, 23. [Google Scholar] [CrossRef] [PubMed]
- Chung, K.S.; Kim, J.H.; Kong, D.H.; Park, I.; Kim, J.G.; Ha, J.K. An Increasing Trend in the Number of Anterior Cruciate Ligament Reconstruction in Korea: A Nationwide Epidemiologic Study. Clin. Orthop. Surg. 2022, 14, 220–226. [Google Scholar] [CrossRef]
- Granan, L.P.; Forssblad, M.; Lind, M.; Engebretsen, L. The Scandinavian ACL registries 2004–2007: Baseline epidemiology. Acta Orthop. 2009, 80, 563–567. [Google Scholar] [CrossRef]
- Helito, C.P.; da Silva, A.G.M.; Guimarães, T.M.; Sobrado, M.F.; Pécora, J.R.; Camanho, G.L. Functional results of multiple revision anterior cruciate ligament with anterolateral tibial tunnel associated with anterolateral ligament reconstruction. Knee Surg. Relat. Res. 2022, 34, 24. [Google Scholar] [CrossRef]
- Johnston, J.T.; Mandelbaum, B.R.; Schub, D.; Rodeo, S.A.; Matava, M.J.; Silvers-Granelli, H.J.; Cole, B.J.; ElAttrache, N.S.; McAdams, T.R.; Brophy, R.H. Video Analysis of Anterior Cruciate Ligament Tears in Professional American Football Athletes. Am. J. Sports Med. 2018, 46, 862–868. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.G.; Lee, D.W.; Bae, K.C.; Choi, B.C.; Yang, S.J.; Cho, S.I.; Kim, D.H. Correlation of Y Balance with Clinical Scores and Functional Tests after Anterior Cruciate Ligament Reconstruction in Young and Middle-Aged Patients. Clin. Orthop. Surg. 2023, 15, 50–58. [Google Scholar] [CrossRef] [PubMed]
- Moon, H.S.; Choi, C.H.; Jung, M.; Yoo, J.H.; Kwon, H.J.; Hong, Y.T.; Kim, S.H. Small Intercondylar Notch Size Is Not Associated with Poor Surgical Outcomes of Anatomical Single-Bundle Anterior Cruciate Ligament Reconstructions. Clin. Orthop. Surg. 2024, 16, 73–85. [Google Scholar] [CrossRef]
- Moran, J.; Katz, L.D.; Schneble, C.A.; Li, D.T.; Kahan, J.B.; Wang, A.; Porrino, J.; Fosam, A.; Cheng, R.; Jokl, P.; et al. A Novel MRI Mapping Technique for Evaluating Bone Bruising Patterns Associated with Noncontact ACL Ruptures. Orthop. J. Sports Med. 2022, 10, 1–8. [Google Scholar] [CrossRef]
- Nordenvall, R.; Bahmanyar, S.; Adami, J.; Stenros, C.; Wredmark, T.; Felländer-Tsai, L. A population-based nationwide study of cruciate ligament injury in Sweden, 2001–2009: Incidence, treatment, and sex differences. Am. J. Sports Med. 2012, 40, 1808–1813. [Google Scholar] [CrossRef]
- Sundararajan, S.R.; Ramakanth, R.; Jha, A.K.; Rajasekaran, S. Outside-in technique versus inside-out semitendinosus graft harvest technique in ACLR: A randomised control trial. Knee Surg. Relat. Res. 2022, 34, 16. [Google Scholar] [CrossRef]
- Décary, S.; Ouellet, P.; Vendittoli, P.A.; Roy, J.S.; Desmeules, F. Diagnostic validity of physical examination tests for common knee disorders: An overview of systematic reviews and meta-analysis. Phys. Ther. Sport 2017, 23, 143–155. [Google Scholar] [CrossRef]
- Ali, A.A.; Abdelwahab, M.B. Short-Term Outcome of Multi-Ligament Knee Injury among Sudanese Patients. Open Access Maced. J. Med. Sci. 2019, 7, 1486–1493. [Google Scholar] [CrossRef] [PubMed]
- Everhart, J.S.; DiBartola, A.C.; Swank, K.; Pettit, R.; Hughes, L.; Lewis, C.; Flanigan, D.C. Cartilage damage at the time of anterior cruciate ligament reconstruction is associated with weaker quadriceps function and lower risk of future ACL injury. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 576–583. [Google Scholar] [CrossRef]
- Gentili, A.; Seeger, L.L.; Yao, L.; Do, H.M. Anterior cruciate ligament tear: Indirect signs at MR imaging. Radiology 1994, 193, 835–840. [Google Scholar] [CrossRef]
- Walczak, B.E.; Lukes, C.; Amendola, N.; Dunn, W.R. Limited evidence that the presence of a bone bruise alone affects the clinical outcome of surgically reconstructed anterior cruciate ligaments: A systematic review. J. Isakos 2017, 2, 186–190. [Google Scholar] [CrossRef]
- Li, X.; Ma, B.C.; Bolbos, R.I.; Stahl, R.; Lozano, J.; Zuo, J.; Lin, K.; Link, T.M.; Safran, M.; Majumdar, S. Quantitative assessment of bone marrow edema-like lesion and overlying cartilage in knees with osteoarthritis and anterior cruciate ligament tear using MR imaging and spectroscopic imaging at 3 Tesla. J. Magn. Reson. Imaging 2008, 28, 453–461. [Google Scholar] [CrossRef]
- McCauley, T.R.; Moses, M.; Kier, R.; Lynch, J.K.; Barton, J.W.; Jokl, P. MR diagnosis of tears of anterior cruciate ligament of the knee: Importance of ancillary findings. AJR Am. J. Roentgenol. 1994, 162, 115–119. [Google Scholar] [CrossRef]
- Jelić, D.; Masulović, D. Bone bruise of the knee associated with the lesions of anterior cruciate ligament and menisci on magnetic resonance imaging. Vojnosanit. Pregl. 2011, 68, 762–766. [Google Scholar] [CrossRef]
- Nishimori, M.; Deie, M.; Adachi, N.; Kanaya, A.; Nakamae, A.; Motoyama, M.; Ochi, M. Articular cartilage injury of the posterior lateral tibial plateau associated with acute anterior cruciate ligament injury. Knee Surg. Sports Traumatol. Arthrosc. 2008, 16, 270–274. [Google Scholar] [CrossRef]
- Theologis, A.A.; Kuo, D.; Cheng, J.; Bolbos, R.I.; Carballido-Gamio, J.; Ma, C.B.; Li, X. Evaluation of bone bruises and associated cartilage in anterior cruciate ligament-injured and -reconstructed knees using quantitative t(1ρ) magnetic resonance imaging: 1-year cohort study. Arthroscopy 2011, 27, 65–76. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef] [PubMed]
- Slim, K.; Nini, E.; Forestier, D.; Kwiatkowski, F.; Panis, Y.; Chipponi, J. Methodological index for non-randomized studies (minors): Development and validation of a new instrument. ANZ J. Surg. 2003, 73, 712–716. [Google Scholar] [CrossRef]
- Schreve, M.A.; Vos, C.G.; Vahl, A.C.; de Vries, J.P.; Kum, S.; de Borst, G.J.; Ünlü, Ç. Venous Arterialisation for Salvage of Critically Ischaemic Limbs: A Systematic Review and Meta-Analysis. Eur. J. Vasc. Endovasc. Surg. 2017, 53, 387–402. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.D.; Zhang, J.; Li, Y.; Li, Z.; Yan, W.; Ao, Y. Classification of Bone Bruises in Pediatric Patients with Anterior Cruciate Ligament Injuries. Orthop. J. Sports Med. 2023, 11, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Vermeijden, H.D.; Yang, X.A.; Mintz, D.N.; Rademakers, M.V.; van der List, J.P.; Kerkhoffs, G.; DiFelice, G.S. Age and Bone Bruise Patterns Predict Tear Location in the Anterior Cruciate Ligament. Arthrosc. Sports Med. Rehabil. 2023, 5, e41–e50. [Google Scholar] [CrossRef] [PubMed]
- Orringer, M.; Lau, J.; Feeley, B.; Pandya, N. Bone Bruise Patterns Associated with Pediatric and Adult Anterior Cruciate Ligament Tears Are Different. Arthrosc. Sports Med. Rehabil. 2023, 5, e151–e157. [Google Scholar] [CrossRef] [PubMed]
- Moran, J.; Lee, M.S.; Kunze, K.N.; Green, J.S.; Katz, L.D.; Wang, A.; McLaughlin, W.M.; Gillinov, S.M.; Jimenez, A.E.; Hewett, T.E.; et al. Examining the Distribution of Bone Bruise Patterns in Contact and Noncontact Acute Anterior Cruciate Ligament Injuries. Am. J. Sports Med. 2023, 51, 1155–1161. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Mao, Y.; Wang, D.; Fu, W.; Li, Q.; Tang, X.; Chen, G.; Chen, X.; Yao, L.; You, M.; et al. Correlation between the Location and Distance of Kissing Contusions and Knee Laxity in Acute Noncontact ACL Injury. Am. J. Sports Med. 2023, 51, 3179–3189. [Google Scholar] [CrossRef]
- Galloway, C.; Ward, H.; Higbie, S.; Kleihege, J.; Kumaravel, M.; Lowe, W.R.; Bailey, L. Relationship between Bone Bruise Volume and Patient Outcomes After ACL Reconstruction. Orthop. J. Sports Med. 2023, 11, 1–6. [Google Scholar] [CrossRef]
- D’Hooghe, P.; Grassi, A.; Villa, F.D.; Alkhelaifi, K.; Papakostas, E.; Rekik, R.; Marin, T.; Tosarelli, F.; Zaffagnini, S. The injury mechanism correlation between MRI and video-analysis in professional football players with an acute ACL knee injury reveals consistent bone bruise patterns. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 121–132. [Google Scholar] [CrossRef]
- Brophy, R.H.; Baker, J.C.; Crain, J.M.; Herzog, M.M.; Stollberg, B.; Wojtys, E.M.; Mack, C.D. MRI Findings Associated with Anterior Cruciate Ligament Tears in National Football League Athletes. Orthop. J. Sports Med. 2023, 11, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Kubota, M.; Sato, T.; Inui, T.; Ohno, R.; Ishijima, M. A bone bruise at the lateral and medial tibial plateau with an anterior cruciate ligament injury is associated with a meniscus tear. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 2298–2306. [Google Scholar] [CrossRef]
- Agostinone, P.; Di Paolo, S.; Lucidi, G.A.; Dal Fabbro, G.; Grassi, A.; Zaffagnini, S. Severe bicompartmental bone bruise is associated with rotatory instability in anterior cruciate ligament injury. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 1725–1732. [Google Scholar] [CrossRef] [PubMed]
- Shi, H.; Ding, L.; Ren, S.; Jiang, Y.; Zhang, H.; Hu, X.; Huang, H.; Ao, Y. Prediction of Knee Kinematics at the Time of Noncontact Anterior Cruciate Ligament Injuries Based on the Bone Bruises. Ann. Biomed. Eng. 2021, 49, 162–170. [Google Scholar] [CrossRef] [PubMed]
- Shi, H.; Ding, L.; Jiang, Y.; Zhang, H.; Ren, S.; Hu, X.; Liu, Z.; Huang, H.; Ao, Y. Bone Bruise Distribution Patterns After Acute Anterior Cruciate Ligament Ruptures: Implications for the Injury Mechanism. Orthop. J. Sports Med. 2020, 8, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Bordoni, V.; di Laura Frattura, G.; Previtali, D.; Tamborini, S.; Candrian, C.; Cristallo Lacalamita, M.; Del Grande, F.; Filardo, G. Bone Bruise and Anterior Cruciate Ligament Tears: Presence, Distribution Pattern, and Associated Lesions in the Pediatric Population. Am. J. Sports Med. 2019, 47, 3181–3186. [Google Scholar] [CrossRef] [PubMed]
- Novaretti, J.V.; Shin, J.J.; Albers, M.; Chambers, M.C.; Cohen, M.; Musahl, V.; Fu, F.H. Bone Bruise Patterns in Skeletally Immature Patients with Anterior Cruciate Ligament Injury: Shock-Absorbing Function of the Physis. Am. J. Sports Med. 2018, 46, 2128–2132. [Google Scholar] [CrossRef] [PubMed]
- Aravindh, P.; Wu, T.; Chan, C.X.; Wong, K.L.; Krishna, L. Association of Compartmental Bone Bruise Distribution with Concomitant Intra-articular and Extra-articular Injuries in Acute Anterior Cruciate Ligament Tears After Noncontact Sports Trauma. Orthop. J. Sports Med. 2018, 6, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Lattermann, C.; Jacobs, C.A.; Reinke, E.K.; Scaramuzza, E.A.; Huston, L.J.; Dunn, W.R.; Spindler, K.P. Are Bone Bruise Characteristics and Articular Cartilage Pathology Associated with Inferior Outcomes 2 and 6 Years After Anterior Cruciate Ligament Reconstruction? Cartilage 2017, 8, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Song, G.Y.; Zhang, H.; Wang, Q.Q.; Zhang, J.; Li, Y.; Feng, H. Bone Contusions After Acute Noncontact Anterior Cruciate Ligament Injury Are Associated with Knee Joint Laxity, Concomitant Meniscal Lesions, and Anterolateral Ligament Abnormality. Arthroscopy 2016, 32, 2331–2341. [Google Scholar] [CrossRef]
- Filardo, G.; Kon, E.; Tentoni, F.; Andriolo, L.; Di Martino, A.; Busacca, M.; Di Matteo, B.; Marcacci, M. Anterior cruciate ligament injury: Post-traumatic bone marrow oedema correlates with long-term prognosis. Int. Orthop. 2016, 40, 183–190. [Google Scholar] [CrossRef] [PubMed]
- Wittstein, J.; Vinson, E.; Garrett, W. Comparison between Sexes of Bone Contusions and Meniscal Tear Patterns in Noncontact Anterior Cruciate Ligament Injuries. Am. J. Sports Med. 2014, 42, 1401–1407. [Google Scholar] [CrossRef] [PubMed]
- Bisson, L.J.; Kluczynski, M.A.; Hagstrom, L.S.; Marzo, J.M. A prospective study of the association between bone contusion and intra-articular injuries associated with acute anterior cruciate ligament tear. Am. J. Sports Med. 2013, 41, 1801–1807. [Google Scholar] [CrossRef] [PubMed]
- Yoon, K.H.; Yoo, J.H.; Kim, K.I. Bone contusion and associated meniscal and medial collateral ligament injury in patients with anterior cruciate ligament rupture. J. Bone Jt. Surg. Am. 2011, 93, 1510–1518. [Google Scholar] [CrossRef] [PubMed]
- Kia, C.; Cavanaugh, Z.; Gillis, E.; Dwyer, C.; Chadayammuri, V.; Muench, L.N.; Berthold, D.P.; Murphy, M.; Pacheco, R.; Arciero, R.A. Size of Initial Bone Bruise Predicts Future Lateral Chondral Degeneration in ACL Injuries: A Radiographic Analysis. Orthop. J. Sports Med. 2020, 8, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Zeiss, J.; Paley, K.; Murray, K.; Saddemi, S.R. Comparison of bone contusion seen by MRI in partial and complete tears of the anterior cruciate ligament. J. Comput. Assist. Tomogr. 1995, 19, 773–776. [Google Scholar] [CrossRef] [PubMed]
- Sanders, T.G.; Medynski, M.A.; Feller, J.F.; Lawhorn, K.W. Bone contusion patterns of the knee at MR imaging: Footprint of the mechanism of injury. Radiographics 2000, 20, S135–S151. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.P., 3rd; Barrett, G.R. Medial and lateral meniscal tear patterns in anterior cruciate ligament-deficient knees. A prospective analysis of 575 tears. Am. J. Sports Med. 2001, 29, 415–419. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.A.; Hageman, J.; Quatman, C.E.; Wordeman, S.C.; Hewett, T.E. Prevalence and location of bone bruises associated with anterior cruciate ligament injury and implications for mechanism of injury: A systematic review. Sports Med. 2014, 44, 281–293. [Google Scholar] [CrossRef]
- Pringle, L.; Wissman, R.D. Imaging of Noncontact Anterior Cruciate Ligament Injuries and Associated Bone Marrow Contusion Patterns. J. Knee Surg. 2022, 35, 475–481. [Google Scholar] [CrossRef]
- Zhang, L.; Hacke, J.D.; Garrett, W.E.; Liu, H.; Yu, B. Bone Bruises Associated with Anterior Cruciate Ligament Injury as Indicators of Injury Mechanism: A Systematic Review. Sports Med. 2019, 49, 453–462. [Google Scholar] [CrossRef]
- Kaplan, P.A.; Walker, C.W.; Kilcoyne, R.F.; Brown, D.E.; Tusek, D.; Dussault, R.G. Occult fracture patterns of the knee associated with anterior cruciate ligament tears: Assessment with MR imaging. Radiology 1992, 183, 835–838. [Google Scholar] [CrossRef]
- Illingworth, K.D.; Hensler, D.; Casagranda, B.; Borrero, C.; van Eck, C.F.; Fu, F.H. Relationship between bone bruise volume and the presence of meniscal tears in acute anterior cruciate ligament rupture. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 2181–2186. [Google Scholar] [CrossRef]
- Viskontas, D.G.; Giuffre, B.M.; Duggal, N.; Graham, D.; Parker, D.; Coolican, M. Bone bruises associated with ACL rupture: Correlation with injury mechanism. Am. J. Sports Med. 2008, 36, 927–933. [Google Scholar] [CrossRef]
- Cerabona, F.; Sherman, M.F.; Bonamo, J.R.; Sklar, J. Patterns of meniscal injury with acute anterior cruciate ligament tears. Am. J. Sports Med. 1988, 16, 603–609. [Google Scholar] [CrossRef]
- Duncan, J.B.; Hunter, R.; Purnell, M.; Freeman, J. Meniscal injuries associated with acute anterior cruciate ligament tears in alpine skiers. Am. J. Sports Med. 1995, 23, 170–172. [Google Scholar] [CrossRef]
- Hagino, T.; Ochiai, S.; Senga, S.; Yamashita, T.; Wako, M.; Ando, T.; Haro, H. Meniscal tears associated with anterior cruciate ligament injury. Arch. Orthop. Trauma. Surg. 2015, 135, 1701–1706. [Google Scholar] [CrossRef]
- Keene, G.C.; Bickerstaff, D.; Rae, P.J.; Paterson, R.S. The natural history of meniscal tears in anterior cruciate ligament insufficiency. Am. J. Sports Med. 1993, 21, 672–679. [Google Scholar] [CrossRef]
- Spindler, K.P.; Schils, J.P.; Bergfeld, J.A.; Andrish, J.T.; Weiker, G.G.; Anderson, T.E.; Piraino, D.W.; Richmond, B.J.; Medendorp, S.V. Prospective study of osseous, articular, and meniscal lesions in recent anterior cruciate ligament tears by magnetic resonance imaging and arthroscopy. Am. J. Sports Med. 1993, 21, 551–557. [Google Scholar] [CrossRef]
- Bastos, R.; Andrade, R.; Vasta, S.; Pereira, R.; Papalia, R.; van der Merwe, W.; Rodeo, S.; Espregueira-Mendes, J. Tibiofemoral bone bruise volume is not associated with meniscal injury and knee laxity in patients with anterior cruciate ligament rupture. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 3318–3326. [Google Scholar] [CrossRef]
- Calvo-Gurry, M.; Hurley, E.T.; Withers, D.; Vioreanu, M.; Moran, R. Posterior tibial bone bruising associated with posterior-medial meniscal tear in patients with acute anterior cruciate ligament injury. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 3633–3637. [Google Scholar] [CrossRef]
- Frobell, R.B. Change in cartilage thickness, posttraumatic bone marrow lesions, and joint fluid volumes after acute ACL disruption: A two-year prospective MRI study of sixty-one subjects. J. Bone Jt. Surg. Am. 2011, 93, 1096–1103. [Google Scholar] [CrossRef] [PubMed]
- Quatman, C.E.; Kiapour, A.; Myer, G.D.; Ford, K.R.; Demetropoulos, C.K.; Goel, V.K.; Hewett, T.E. Cartilage pressure distributions provide a footprint to define female anterior cruciate ligament injury mechanisms. Am. J. Sports Med. 2011, 39, 1706–1713. [Google Scholar] [CrossRef]
- Lee, K.; Siegel, M.J.; Lau, D.M.; Hildebolt, C.F.; Matava, M.J. Anterior cruciate ligament tears: MR imaging-based diagnosis in a pediatric population. Radiology 1999, 213, 697–704. [Google Scholar] [CrossRef] [PubMed]
- Jones, G.; Ding, C.; Glisson, M.; Hynes, K.; Ma, D.; Cicuttini, F. Knee articular cartilage development in children: A longitudinal study of the effect of sex, growth, body composition, and physical activity. Pediatr. Res. 2003, 54, 230–236. [Google Scholar] [CrossRef]
- Myer, G.D.; Ford, K.R.; Paterno, M.V.; Nick, T.G.; Hewett, T.E. The effects of generalized joint laxity on risk of anterior cruciate ligament injury in young female athletes. Am. J. Sports Med. 2008, 36, 1073–1080. [Google Scholar] [CrossRef] [PubMed]
- Yoon, J.P.; Chang, C.B.; Yoo, J.H.; Kim, S.J.; Choi, J.Y.; Choi, J.A.; Seong, S.C.; Kim, T.K. Correlation of magnetic resonance imaging findings with the chronicity of an anterior cruciate ligament tear. J. Bone Jt. Surg. Am. 2010, 92, 353–360. [Google Scholar] [CrossRef]
- Deangelis, J.P.; Spindler, K.P. Traumatic Bone Bruises in the Athlete’s Knee. Sports Health 2010, 2, 398–402. [Google Scholar] [CrossRef]
- Pezeshki, S.; Vogl, T.J.; Pezeshki, M.Z.; Daghighi, M.H.; Pourisa, M. Association of the type of trauma, occurrence of bone bruise, fracture and joint effusion with the injury to the menisci and ligaments in MRI of knee trauma. Muscles Ligaments Tendons J. 2016, 6, 161–166. [Google Scholar] [CrossRef]
- Ward, P.; Chang, P.; Radtke, L.; Brophy, R.H. Clinical Implications of Bone Bruise Patterns Accompanying Anterior Cruciate Ligament Tears. Sports Health 2022, 14, 585–591. [Google Scholar] [CrossRef]
- Yi, Z.; Jiang, J.; Liu, Z.; Wang, H.; Yi, Q.; Zhan, H.; Liang, X.; Niu, Y.; Xiang, D.; Geng, B.; et al. The Association between Bone Bruises and Concomitant Ligaments Injuries in Anterior Cruciate Ligament Injuries: A Systematic Review and Meta-analysis. Indian. J. Orthop. 2023, 57, 20–32. [Google Scholar] [CrossRef]

| Author | Year | Nation | Period | Study Design | MRI Timing | MRI Intensity | Sample Size | Bone Bruise | Age, Years | Gender (M) |
|---|---|---|---|---|---|---|---|---|---|---|
| Wang et al. [24] | 2023 | China | 2011–2020 | Retrospective | 4 wks | 1.5 T | 188 | 153 | 15.2 | 55 |
| Vermeijden et al. [25] | 2023 | Netherland | 2019 | Retrospective | 31 days | 1.5 or 3 T | 254 | 251 | 34 | 114 |
| Orringer et al. [26] | 2023 | USA | 2015–2021 | Retrospective | 8 wks | 26 | 20 | 11.8 | 17 | |
| 26 | 20 | 34.3 | 17 | |||||||
| Moran et al. [27] | 2023 | USA | Retrospective | 30 days | 3 T | 78 | 75 | 23.1 | 54 | |
| 142 | 138 | 25.6 | 77 | |||||||
| Li et al. [28] | 2023 | China | 2021–2022 | Retrospective | 3 wks | 1.5 T | 205 | 167 | 27.05 | 118 |
| Galloway et al. [29] | 2023 | USA | 2014–2019 | Retrospective | 2 months | 60 | 57 | 23.4 | 31 | |
| D’Hooghe et al. [30] | 2023 | Italy | 2014–2018 | Retrospective | 19 | 19 | 19.5 | 19 | ||
| Brophy et al. [31] | 2023 | USA | 2015–2019 | Retrospective | 3 weeks | 191 | 181 | |||
| Kim et al. [32] | 2022 | Japan | 2013–2021 | Retrospective | 2 T | 176 | 141 | 26.8 | 98 | |
| Agostinone et al. [33] | 2022 | Italy | Retrospective | 3 months | 1.5 T | 29 | 24 | 29.1 | 24 | |
| Shi et al. [34] | 2021 | China | 2016–2018 | Retrospective | 4 wks | 1.5 T | 56 | 43 | 30.3 | 2 |
| 82 | 66 | 26.7 | 6 | |||||||
| Shi et al. [35] | 2020 | China | 2016–2018 | Retrospective | 4 wks | 1.5 T | 207 | 169 | 28.7 | |
| Bordoni et al. [36] | 2019 | Swiss | 2010–2018 | Retrospective | 90 days | 78 | 54 | 14.3 | 41 | |
| Novaretti et al. [37] | 2018 | USA | 2012–2016 | Retrospective | 6 wks | 53 | 51 | 13.3 | 26 | |
| Aravindh et al. [38] | 2018 | Singapore | 2013–2016 | Retrospective | 6 wks | 168 | 155 | 126 | ||
| Lattermann et al. [39] | 2017 | USA | Retrospective | 81 | 81 | |||||
| Song et al. [40] | 2016 | China | 2011–2013 | Retrospective | 6 wks | 1.5 T | 193 | 32.3 | 141 | |
| Filardo et al. [41] | 2015 | Italy | 2004–2008 | Retrospective | 1 month | 134 | 74 | 31.9 | 98 | |
| Witstein et al. [42] | 2014 | USA | 2005–2010 | Retrospective | 6 wks | 1.5 T | 73 | 70 | 28 | |
| Bisson et al. [43] | 2013 | USA | 2005–2011 | Retrospective | 6 wks | 1.5 T | 171 | 154 | 25.2 | 89 |
| Yoon et al. [44] | 2011 | Korea | 2006–2008 | Retrospective | 6 wks | 81 | 68 | 29 | 22 | |
| Jelic et al. [18] | 2010 | Serbia | Retrospective | 1 month | 0.3 T | 120 | 39 | 31 | 88 | |
| Author | Clearly Stated Aim | Inclusion of Consecutive Patients | Prospective Collection of Data | Endpoints Appropriate for Aim | Unbiased Assessment of Endpoints | Appropriate Follow-Up Period | Lost to Follow-Up< 5% | Prospective Calculation of Study Size | Item 9–12 Only for Comparative Studies | Adequate Control Group | Contemporary Groups | Baseline Equivalence of Groups | Adequate Statistical Analysis | Total Score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wang et al. [24] | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 0 | 12 | |||||
| Vermeijden et al. [25] | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 21 | |
| Orringer et al. [26] | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 20 | |
| Moran et al. [27] | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 20 | |
| Li et al. [28] | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 21 | |
| Galloway et al. [29] | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 1 | 13 | |||||
| D’Hooghe et al. [30] | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 0 | 12 | |||||
| Brophy et al. [31] | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 20 | |
| Kim et al. [32] | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 1 | 1 | 1 | 2 | 2 | 19 | |
| Agostinone et al. [33] | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 21 | |
| Shi et al. [34] | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 20 | |
| Shi et al. [35] | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 20 | |
| Bordoni et al. [36] | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 0 | 12 | |||||
| Novaretti et al. [37] | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 20 | |
| Aravindh et al. [38] | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 20 | |
| Lattermann et al. [39] | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 20 | |
| Song et al. [40] | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 21 | |
| Filardo et al. [41] | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 20 | |
| Witstein et al. [42] | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 20 | |
| Bisson et al. [43] | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 20 | |
| Yoon et al. [44] | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 0 | 1 | 1 | 2 | 2 | 18 | |
| Jelic et al. [18] | 2 | 1 | 0 | 1 | 2 | 2 | 2 | 0 | 2 | 1 | 2 | 2 | 17 |
| Author | ACL Sample | Bone Bruise Sample | LTP | MTP | LFC | MFC | MM | LM | Cartilage |
|---|---|---|---|---|---|---|---|---|---|
| Wang et al. [24] | 188 | 153 | 139 | 48 | 136 | 40 | 59 | 58 | 22 |
| Vermeijden et al. [25] | 254 | 251 | 240 | 32 | 163 | 138 | 79 | 72 | |
| Orringer et al. [26] | 26 | 20 | 18 | 1 | 19 | 4 | 11 | 10 | |
| 26 | 20 | 16 | 9 | 10 | 12 | 16 | 11 | ||
| Moran et al. [27] | 78 | 75 | 70 | 47 | 65 | 49 | 28 | 27 | |
| 142 | 138 | 77 | 102 | 119 | 120 | 31 | 59 | ||
| Li et al. [28] | 205 | 137 | 167 | 90 | 135 | 62 | 46 | 106 | 55 |
| Galloway et al. [29] | 60 | 57 | 53 | 16 | 46 | 13 | 28 | 30 | 8 |
| D’Hooghe et al. [30] | 19 | 19 | 18 | 3 | 12 | 0 | 9 | 6 | 2 |
| Brophy et al. [31] | 191 | 181 | 154 | 93 | 140 | 44 | 78 | 113 | |
| Kim et al. [32] | 176 | 141 | 82 | 47 | 116 | 29 | 56 | 42 | 7 |
| Agostinone et al. [33] | 29 | 24 | 24 | 16 | 21 | 5 | 12 | 8 | 4 |
| Shi et al. [34] | 56 | 43 | 40 | 32 | 38 | 12 | 12 | 17 | |
| 82 | 66 | 62 | 31 | 42 | 20 | 23 | 27 | ||
| Shi et al. [35] | 207 | 169 | 169 | 80 | 156 | 91 | 45 | 73 | |
| Bordoni et al. [36] | 78 | 54 | 44 | 11 | 57 | 34 | 21 | 6 | 2 |
| Novaretti et al. [37] | 53 | 51 | 51 | 37 | 51 | 20 | 10 | 19 | |
| Aravindh et al. [38] | 168 | 155 | 141 | 95 | 132 | 50 | 61 | 62 | 18 |
| Lattermann et al. [39] | 81 | 81 | 76 | 46 | 66 | 20 | 42 | 42 | 17 |
| Song et al. [40] | 193 | 141 | 141 | 41 | 117 | 12 | 84 | 94 | 20 |
| Filardo et al. [41] | 134 | 74 | 35 | 11 | 23 | 5 | 34 | 11 | |
| Witstein et al. [42] | 73 | 70 | 67 | 45 | 70 | 31 | 34 | 29 | |
| Bisson et al. [43] | 171 | 154 | 145 | 44 | 132 | 11 | 59 | 65 | 26 |
| Yoon et al. [44] | 81 | 68 | 59 | 21 | 55 | 19 | 41 | 44 | |
| Jelic et al. [18] | 120 | 39 | 20 | 12 | 24 | 6 | 24 | 13 | |
| Total | 2891 | 2381 | 2108 | 1010 | 1945 | 847 | 943 | 1044 | 181 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sohn, S.; AlShammari, S.M.; Lee, J.H.; Kim, M.S. Bone Bruises and Concomitant Meniscus and Cartilage Damage in Anterior Cruciate Ligament Injuries: A Systematic Review and Meta-Analysis. Bioengineering 2024, 11, 515. https://doi.org/10.3390/bioengineering11050515
Sohn S, AlShammari SM, Lee JH, Kim MS. Bone Bruises and Concomitant Meniscus and Cartilage Damage in Anterior Cruciate Ligament Injuries: A Systematic Review and Meta-Analysis. Bioengineering. 2024; 11(5):515. https://doi.org/10.3390/bioengineering11050515
Chicago/Turabian StyleSohn, Sueen, Saad Mohammed AlShammari, Jeong Han Lee, and Man Soo Kim. 2024. "Bone Bruises and Concomitant Meniscus and Cartilage Damage in Anterior Cruciate Ligament Injuries: A Systematic Review and Meta-Analysis" Bioengineering 11, no. 5: 515. https://doi.org/10.3390/bioengineering11050515
APA StyleSohn, S., AlShammari, S. M., Lee, J. H., & Kim, M. S. (2024). Bone Bruises and Concomitant Meniscus and Cartilage Damage in Anterior Cruciate Ligament Injuries: A Systematic Review and Meta-Analysis. Bioengineering, 11(5), 515. https://doi.org/10.3390/bioengineering11050515








