Validity and Reliability of a Smartphone Application for Home Measurement of Four-Meter Gait Speed in Older Adults
Abstract
1. Introduction
2. Methods
2.1. Study Design and Participants
2.2. Smartphone Application (App)
2.3. Study Procedures and 4MGS Home Test
2.4. Derivation of 4MGS from Data Collected via Smartphone App and Gold Standard Methods
2.5. Statistical Analysis
3. Results
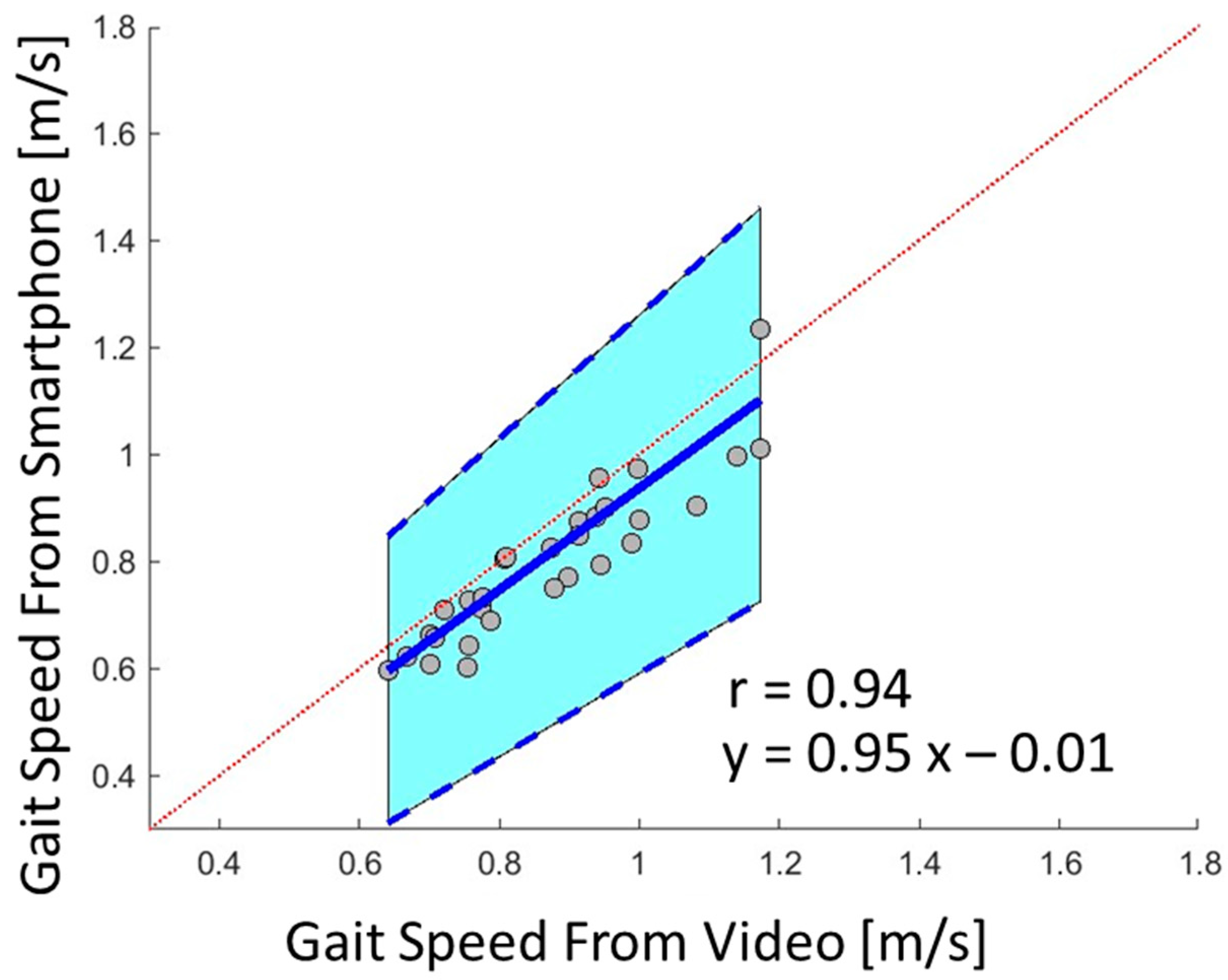
3.1. Validity of 4MGS Measured by Smartphone App
3.2. Reliability of 4MGS Measured by Smartphone App
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nakano, T.; Kimura, S.; Yamashita, T.; Yoshimi, M.; Tao, Y.; Takata, S. Correlation of 4-meter gait speed with clinical indicators of chronic obstructive pulmonary disease. Respir. Investig. 2021, 59, 505–512. [Google Scholar] [CrossRef]
- Yoshida, C.; Ichiyasu, H.; Ideguchi, H.; Hirosako, S.; Masunaga, A.; Kojima, K.; Saeki, S.; Fujii, K.; Sakagami, T.; Kohrogi, H. Four-meter gait speed predicts daily physical activity in patients with chronic respiratory diseases. Respir. Investig. 2019, 57, 368–375. [Google Scholar] [CrossRef]
- Beaudart, C.; Rolland, Y.; Cruz-Jentoft, A.J.; Bauer, J.M.; Sieber, C.; Cooper, C.; Al-Daghri, N.; Araujo de Carvalho, I.; Bautmans, I.; Bernabei, R. Assessment of muscle function and physical performance in daily clinical practice: A position paper endorsed by the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO). Calcif. Tissue Int. 2019, 105, 1–14. [Google Scholar] [CrossRef]
- Afilalo, J.; Kim, S.; O’Brien, S.; Brennan, J.M.; Edwards, F.H.; Mack, M.J.; McClurken, J.B.; Cleveland, J.C.; Smith, P.K.; Shahian, D.M. Gait speed and operative mortality in older adults following cardiac surgery. JAMA Cardiol. 2016, 1, 314–321. [Google Scholar] [CrossRef]
- Dale, W.; Klepin, H.D.; Williams, G.R.; Alibhai, S.M.; Bergerot, C.; Brintzenhofeszoc, K.; Hopkins, J.O.; Jhawer, M.P.; Katheria, V.; Loh, K.P. Practical assessment and management of vulnerabilities in older patients receiving systemic cancer therapy: ASCO guideline update. J. Clin. Oncol. 2023, 41, 4293–4312. [Google Scholar] [CrossRef]
- Maggio, M.; Ceda, G.P.; Ticinesi, A.; De Vita, F.; Gelmini, G.; Costantino, C.; Meschi, T.; Kressig, R.W.; Cesari, M.; Fabi, M. Instrumental and non-instrumental evaluation of 4-meter walking speed in older individuals. PLoS ONE 2016, 11, e0153583. [Google Scholar] [CrossRef] [PubMed]
- Rubin, D.S.; Ranjeva, S.L.; Urbanek, J.K.; Karas, M.; Madariaga, M.L.L.; Huisingh-Scheetz, M. Smartphone-Based Gait Cadence to Identify Older Adults with Decreased Functional Capacity. Digit. Biomark. 2022, 6, 61–70. [Google Scholar] [CrossRef] [PubMed]
- Dodge, H.; Mattek, N.; Austin, D.; Hayes, T.; Kaye, J. In-home walking speeds and variability trajectories associated with mild cognitive impairment. Neurology 2012, 78, 1946–1952. [Google Scholar] [CrossRef] [PubMed]
- Bahl, N.E.; Magnavita, E.S.; Hshieh, T.; Testa, M.; Kim, D.; Manor, B.; Driver, J.A.; Abel, G.A.; DuMontier, C. Objective performance tests of cognition and physical function as part of a virtual geriatric assessment. J. Geriatr. Oncol. 2021, 12, 1256–1258. [Google Scholar] [CrossRef]
- Chen, C.; Ding, S.; Wang, J. Digital health for aging populations. Nat. Med. 2023, 29, 1623–1630. [Google Scholar] [CrossRef] [PubMed]
- Takeda, R.; Tadano, S.; Todoh, M.; Morikawa, M.; Nakayasu, M.; Yoshinari, S. Gait analysis using gravitational acceleration measured by wearable sensors. J. Biomech. 2009, 42, 223–233. [Google Scholar] [CrossRef] [PubMed]
- Nishiguchi, S.; Yamada, M.; Nagai, K.; Mori, S.; Kajiwara, Y.; Sonoda, T.; Yoshimura, K.; Yoshitomi, H.; Ito, H.; Okamoto, K. Reliability and validity of gait analysis by android-based smartphone. Telemed. E-Health 2012, 18, 292–296. [Google Scholar] [CrossRef] [PubMed]
- Aminian, K.; Najafi, B.; Büla, C.; Leyvraz, P.-F.; Robert, P. Spatio-temporal parameters of gait measured by an ambulatory system using miniature gyroscopes. J. Biomech. 2002, 35, 689–699. [Google Scholar] [CrossRef] [PubMed]
- Manor, B.; Yu, W.; Zhu, H.; Harrison, R.; Lo, O.-Y.; Lipsitz, L.; Travison, T.; Pascual-Leone, A.; Zhou, J. Smartphone app–based assessment of gait during normal and dual-task walking: Demonstration of validity and reliability. JMIR Mhealth Uhealth 2018, 6, e8815. [Google Scholar] [CrossRef] [PubMed]
- Lee, P.-A.; Dumontier, C.; Yu, W.; Ho, K.T.; Groblewski, N.; Zhou, J.; Travison, T.; Testa, M.; Hshieh, T.; Kim, D. Validity, Reliability, and Feasibility of Smartphone Application Intended for Home Measurement of Gait Speed and Other Gait Dynamics in Older Adults with Blood Cancers. Blood 2023, 142, 2354. [Google Scholar] [CrossRef]
- Manor, B.; Yu, W.; Lo, O.-Y.; Zhu, H.; Travison, T.G.; Lipsitz, L.; Zhou, J. Validity and reliability of remote, smartphone-based assessment of dual-task standing and walking in older adults. Innov. Aging 2019, 3, S10. [Google Scholar] [CrossRef]
- Manor, B.; Zhou, J.; Lo, O.; Zhu, H.; Zafonte, R.; Travison, T.; Lipsitz, L.; Pascual-Leone, A. Remote smartphone assessment of dual task walking, self-reported head trauma and health in retired nfl players. Innov. Aging 2018, 2, 512. [Google Scholar] [CrossRef]
- Yu, W.; Zhu, H.; Lo, O.; Zhou, J.; Harrison, R.; Lipsitz, L.; Pascual-Leone, A.; Manor, B. Remote, smartphone app-based assessment of normal and dual task walking in healthy younger and older adults. Innov. Aging 2018, 2, 731. [Google Scholar] [CrossRef]
- Zhou, J.; Cattaneo, G.; Yu, W.; Tormos, J.; Lipsitz, L.; Bartres-Faz, D.; Pascual-Leone, A.; Manor, B. Effects of Age on Dual Task Walking Performance as Measured Using a Smartphone Application in Middle-Aged Adults. Innov. Aging 2021, 5, 166–167. [Google Scholar] [CrossRef]
- Zhou, J.; Jiang, X.; Yu, W.; Zhu, H.; Lo, O.-Y.; Gouskova, N.A.; Travison, T.; Lipsitz, L.A.; Pascual-Leone, A.; Manor, B. A smartphone app-based application enabling remote assessments of standing balance during the COVID-19 pandemic and beyond. IEEE Internet Things J. 2021, 8, 15818–15828. [Google Scholar] [CrossRef]
- Zhou, J.; Yu, W.; Zhu, H.; Lo, O.-Y.; Gouskova, N.; Travison, T.; Lipsitz, L.A.; Pascual-Leone, A.; Manor, B. A novel smartphone App-based assessment of standing postural control: Demonstration of reliability and sensitivity to aging and task constraints. In Proceedings of the 2020 IEEE International Conference on E-health Networking, Application & Services (HEALTHCOM), Shenzhen, China, 1–2 March 2021; pp. 1–6. [Google Scholar]
- Zhou, J.; Yu, W.; Zhu, H.; Lo, O.-Y.; Travison, T.; Lipsitz, L.; Manor, B. Novel remote assessment of the standing postural control in younger and older adults using smartphone application. Innov. Aging 2019, 3, S334–S335. [Google Scholar] [CrossRef]
- Parker, S.J.; Jessel, S.; Richardson, J.E.; Reid, M.C. Older adults are mobile too! Identifying the barriers and facilitators to older adults’ use of mHealth for pain management. BMC Geriatr. 2013, 13, 43. [Google Scholar] [CrossRef]
- Wang, J.; Du, Y.; Coleman, D.; Peck, M.; Myneni, S.; Kang, H.; Gong, Y. Mobile and connected health technology needs for older adults aging in place: Cross-sectional survey study. JMIR Aging 2019, 2, e13864. [Google Scholar] [CrossRef]
- Lee, J.-A.; Nguyen, A.L.; Berg, J.; Amin, A.; Bachman, M.; Guo, Y.; Evangelista, L. Attitudes and preferences on the use of mobile health technology and health games for self-management: Interviews with older adults on anticoagulation therapy. JMIR Mhealth Uhealth 2014, 2, e3196. [Google Scholar] [CrossRef] [PubMed]
- Clancy, D.D.; Revette, A.C.; Bahl, N.E.; Ho, K.T.; Manor, B.; Testa, M.A.; Dieli-Conwright, C.M.; Hshieh, T.; Driver, J.A.; Abel, G.A. Benefits and Barriers of Technology for Home Function and Mobility Assessment: Perspectives of Older Patients with Blood Cancers, Caregivers, and Clinicians. JCO Clin. Cancer Inform. 2023, 7, e2200171. [Google Scholar] [CrossRef] [PubMed]
- Mukaka, M.M. A guide to appropriate use of correlation coefficient in medical research. Malawi Med. J. 2012, 24, 69–71. [Google Scholar] [PubMed]
- Silsupadol, P.; Teja, K.; Lugade, V. Reliability and validity of a smartphone-based assessment of gait parameters across walking speed and smartphone locations: Body, bag, belt, hand, and pocket. Gait Posture 2017, 58, 516–522. [Google Scholar] [CrossRef]
- Auepanwiriyakul, C.; Waibel, S.; Songa, J.; Bentley, P.; Faisal, A.A. Accuracy and acceptability of wearable motion tracking for inpatient monitoring using smartwatches. Sensors 2020, 20, 7313. [Google Scholar] [CrossRef]
- Passing, H.; Bablok, W. A new biometrical procedure for testing the equality of measurements from two different analytical methods. Application of linear regression procedures for method comparison studies in clinical chemistry, Part I. J. Clin. Chem. Clin. Biochem. 1983, 21, 709–720. [Google Scholar] [CrossRef]
- Bland, J.M.; Altman, D.G. Measuring agreement in method comparison studies. Stat. Methods Med. Res. 1999, 8, 135–160. [Google Scholar] [CrossRef]
- Cicchetti, D.V. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol. Assess. 1994, 6, 284. [Google Scholar] [CrossRef]
- Soangra, R.; Lockhart, T.E. Agreement in gait speed from smartphone and stopwatch for five meter walk in laboratory and clinical environments. Biomed. Sci. Instrum. 2014, 50, 254. [Google Scholar]
- Kim, A.; Kim, J.; Rietdyk, S.; Ziaie, B. A wearable smartphone-enabled camera-based system for gait assessment. Gait Posture 2015, 42, 138–144. [Google Scholar] [CrossRef]
- Lipsmeier, F.; Taylor, K.I.; Kilchenmann, T.; Wolf, D.; Scotland, A.; Schjodt-Eriksen, J.; Cheng, W.Y.; Fernandez-Garcia, I.; Siebourg-Polster, J.; Jin, L. Evaluation of smartphone-based testing to generate exploratory outcome measures in a phase 1 Parkinson’s disease clinical trial. Mov. Disord. 2018, 33, 1287–1297. [Google Scholar] [CrossRef]
- Silsupadol, P.; Prupetkaew, P.; Kamnardsiri, T.; Lugade, V. Smartphone-based assessment of gait during straight walking, turning, and walking speed modulation in laboratory and free-living environments. IEEE J. Biomed. Health Inform. 2019, 24, 1188–1195. [Google Scholar] [CrossRef] [PubMed]
- Rashid, U.; Barbado, D.; Olsen, S.; Alder, G.; Elvira, J.L.; Lord, S.; Niazi, I.K.; Taylor, D. Validity and reliability of a smartphone app for gait and balance assessment. Sensors 2021, 22, 124. [Google Scholar] [CrossRef]
- Christensen, J.C.; Stanley, E.C.; Oro, E.G.; Carlson, H.B.; Naveh, Y.Y.; Shalita, R.; Teitz, L.S. The validity and reliability of the OneStep smartphone application under various gait conditions in healthy adults with feasibility in clinical practice. J. Orthop. Surg. Res. 2022, 17, 417. [Google Scholar] [CrossRef] [PubMed]
- DuMontier, C.; Jaung, T.; Bahl, N.E.; Manor, B.; Testa, M.; Dieli-Conwright, C.M.; Kim, D.; Hshieh, T.; Driver, J.A.; Abel, G.A. Virtual frailty assessment for older adults with hematologic malignancies. Blood Adv. 2022, 6, 5360–5363. [Google Scholar] [CrossRef]
- McCambridge, J.; Witton, J.; Elbourne, D.R. Systematic review of the Hawthorne effect: New concepts are needed to study research participation effects. J. Clin. Epidemiol. 2014, 67, 267–277. [Google Scholar] [CrossRef] [PubMed]
- Perera, S.; Mody, S.H.; Woodman, R.C.; Studenski, S.A. Meaningful change and responsiveness in common physical performance measures in older adults. J. Am. Geriatr. Soc. 2006, 54, 743–749. [Google Scholar] [CrossRef]
| Demographic Characteristic Parameters | ||||||
|---|---|---|---|---|---|---|
| Sex | 15 women | |||||
| Age (years) | 77.67 ± 6.41 [88.00–67.00] | |||||
| Height (m) | 1.62 ± 0.06 [1.69–1.47] | |||||
| Body weight (kg) | 70.00 ± 15.26 [92.00–43.50] | |||||
| Body mass index (BMI) | 26.78 ± 5.96 [37.36–17.21] | |||||
| Ethnicity | 13 white or Caucasian, 1 black or African American, and 1 other group | |||||
| MoCA | 25.93 ± 2.58 [29.00–20.00] | |||||
| SPPB | 9.67 ± 2.38 [12.00–5.00] | |||||
| Four-Meter Gait Speed (4MGS) | ||||||
| With Supervision | ||||||
| Smartphone App | Video | Stopwatch | ||||
| Day 1 | Day 2 | Day 1 | Day 2 | Day 1 | Day 2 | |
| Gait Speed (m/s) | 0.81 ± 0.17 [1.23–0.60] | 0.79 ± 0.13 [1.01–0.60] | 0.88 ± 0.15 [1.17–0.70] | 0.87 ± 0.15 [1.17–0.64] | 0.94 ± 0.26 [1.55–0.68] | 0.84 ± 0.14 [1.17–0.61] |
| Without Supervision | ||||||
| Smartphone App | ||||||
| Day 3 | Day 4 | Day 5 | ||||
| Gait Speed (m/s) | 0.82 ± 0.15 [1.20–0.61] | 0.79 ± 0.21 [1.14–0.30] | 0.80 ± 0.16 [1.16–0.61] | |||
| ICC | p-Value | 95% CI | |
|---|---|---|---|
| Home assessment with supervision between two visits | |||
| Smartphone App | 0.85 | <0.001 | 0.62–0.95 |
| Video | 0.85 | <0.001 | 0.62–0.95 |
| Stopwatch | 0.68 | <0.001 | 0.27–0.88 |
| Home assessment without supervision among three visits | |||
| Smartphone App | 0.75 | <0.001 | 0.49–0.91 |
| Home assessment with and without supervision | |||
| Smartphone App | 0.93 | <0.001 | 0.77–0.98 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, P.-A.; DuMontier, C.; Yu, W.; Ask, L.; Zhou, J.; Testa, M.A.; Kim, D.; Abel, G.; Travison, T.; Manor, B.; et al. Validity and Reliability of a Smartphone Application for Home Measurement of Four-Meter Gait Speed in Older Adults. Bioengineering 2024, 11, 257. https://doi.org/10.3390/bioengineering11030257
Lee P-A, DuMontier C, Yu W, Ask L, Zhou J, Testa MA, Kim D, Abel G, Travison T, Manor B, et al. Validity and Reliability of a Smartphone Application for Home Measurement of Four-Meter Gait Speed in Older Adults. Bioengineering. 2024; 11(3):257. https://doi.org/10.3390/bioengineering11030257
Chicago/Turabian StyleLee, Pei-An, Clark DuMontier, Wanting Yu, Levi Ask, Junhong Zhou, Marcia A. Testa, Dae Kim, Gregory Abel, Tom Travison, Brad Manor, and et al. 2024. "Validity and Reliability of a Smartphone Application for Home Measurement of Four-Meter Gait Speed in Older Adults" Bioengineering 11, no. 3: 257. https://doi.org/10.3390/bioengineering11030257
APA StyleLee, P.-A., DuMontier, C., Yu, W., Ask, L., Zhou, J., Testa, M. A., Kim, D., Abel, G., Travison, T., Manor, B., & Lo, O.-Y. (2024). Validity and Reliability of a Smartphone Application for Home Measurement of Four-Meter Gait Speed in Older Adults. Bioengineering, 11(3), 257. https://doi.org/10.3390/bioengineering11030257






