Outcome of Application of Cryopreserved Amniotic Membrane Grafts in the Treatment of Chronic Nonhealing Wounds of Different Origins in Polymorbid Patients: A Prospective Multicenter Study
Abstract
1. Introduction
2. Materials and Methods
2.1. AM Graft Preparation
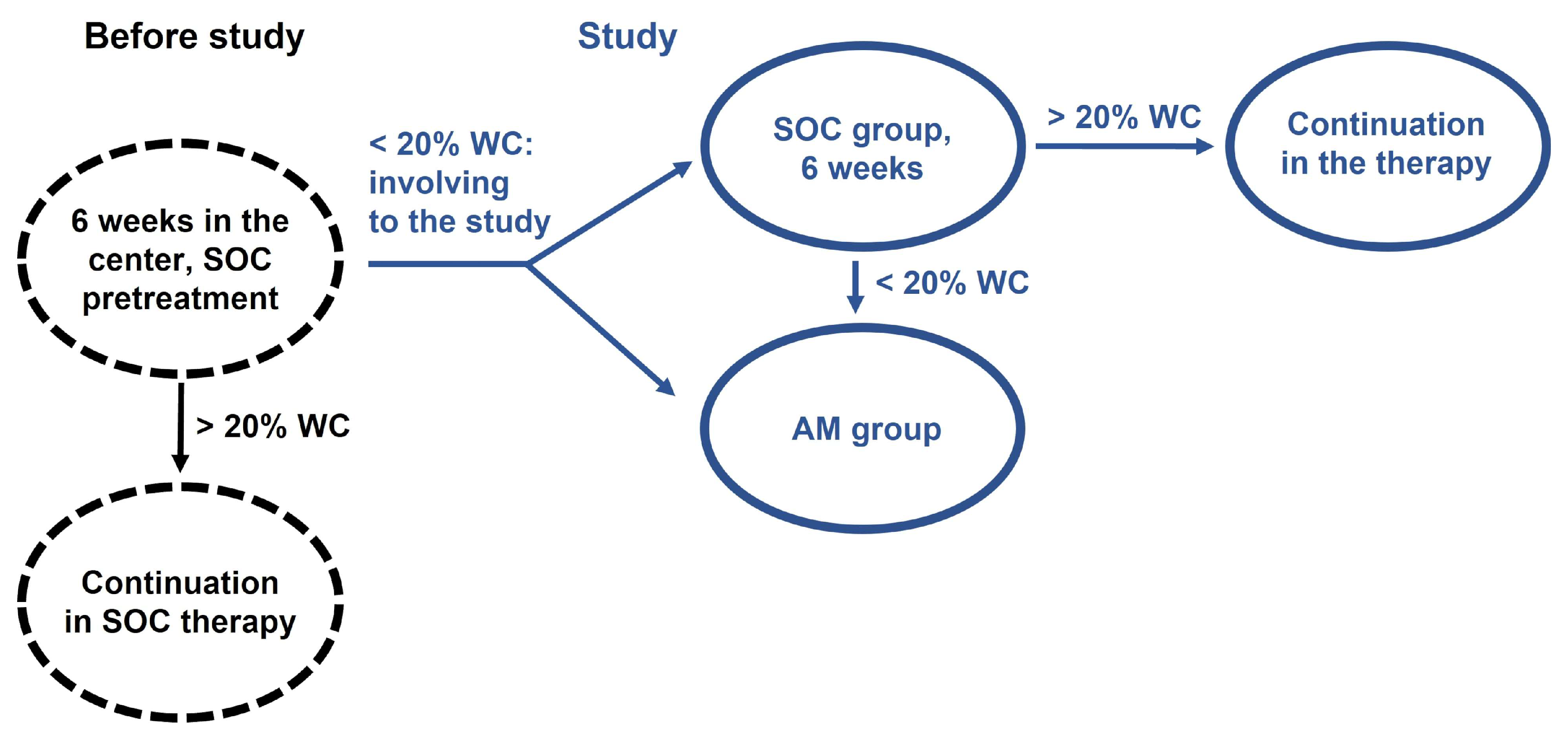
2.2. Subjects Enrolment, Study Groups
2.3. Patients
2.4. Wound Treatment Procedure, Subjective Patients’ Feelings
2.5. Healing Evaluation
2.6. Statistics
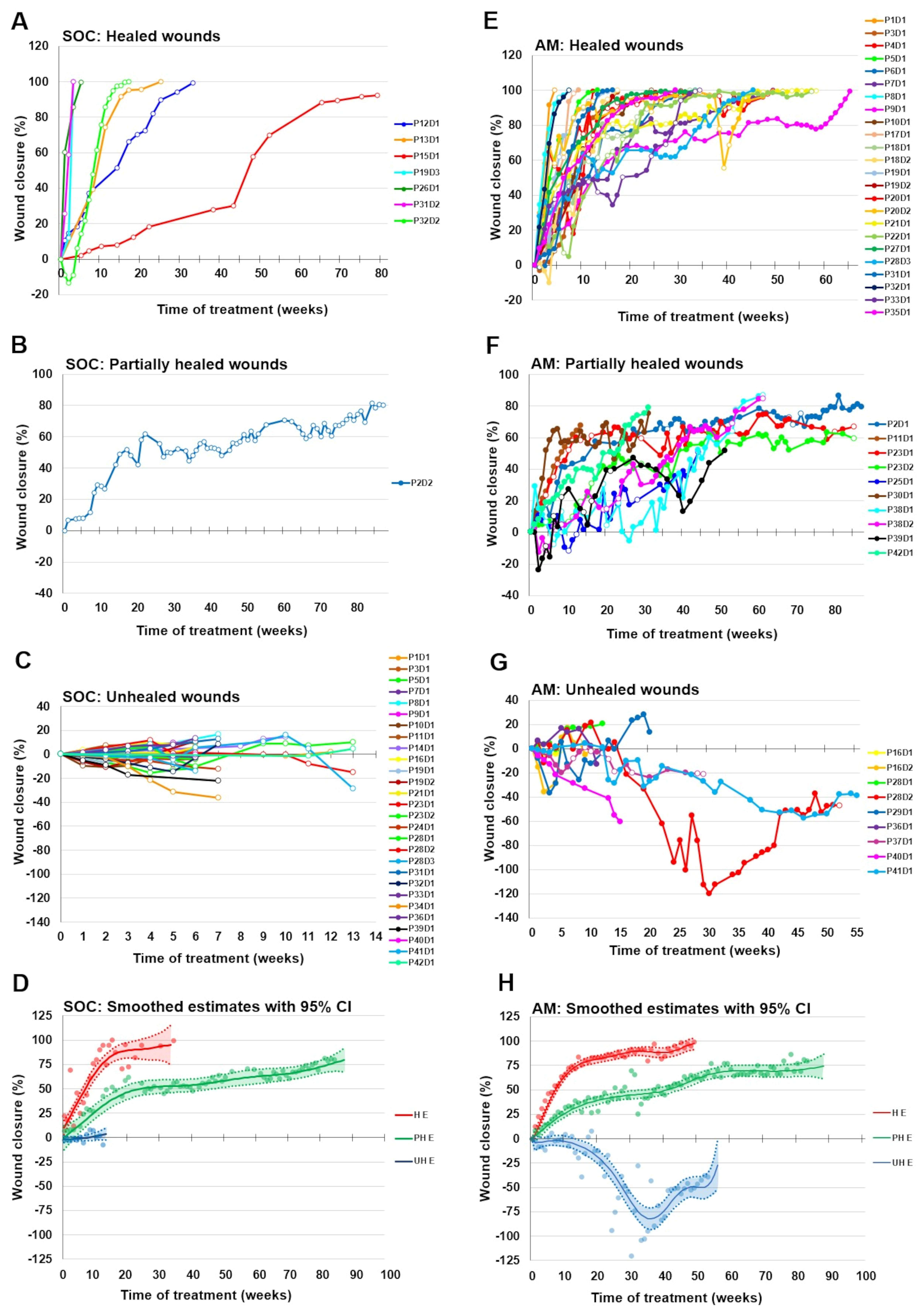
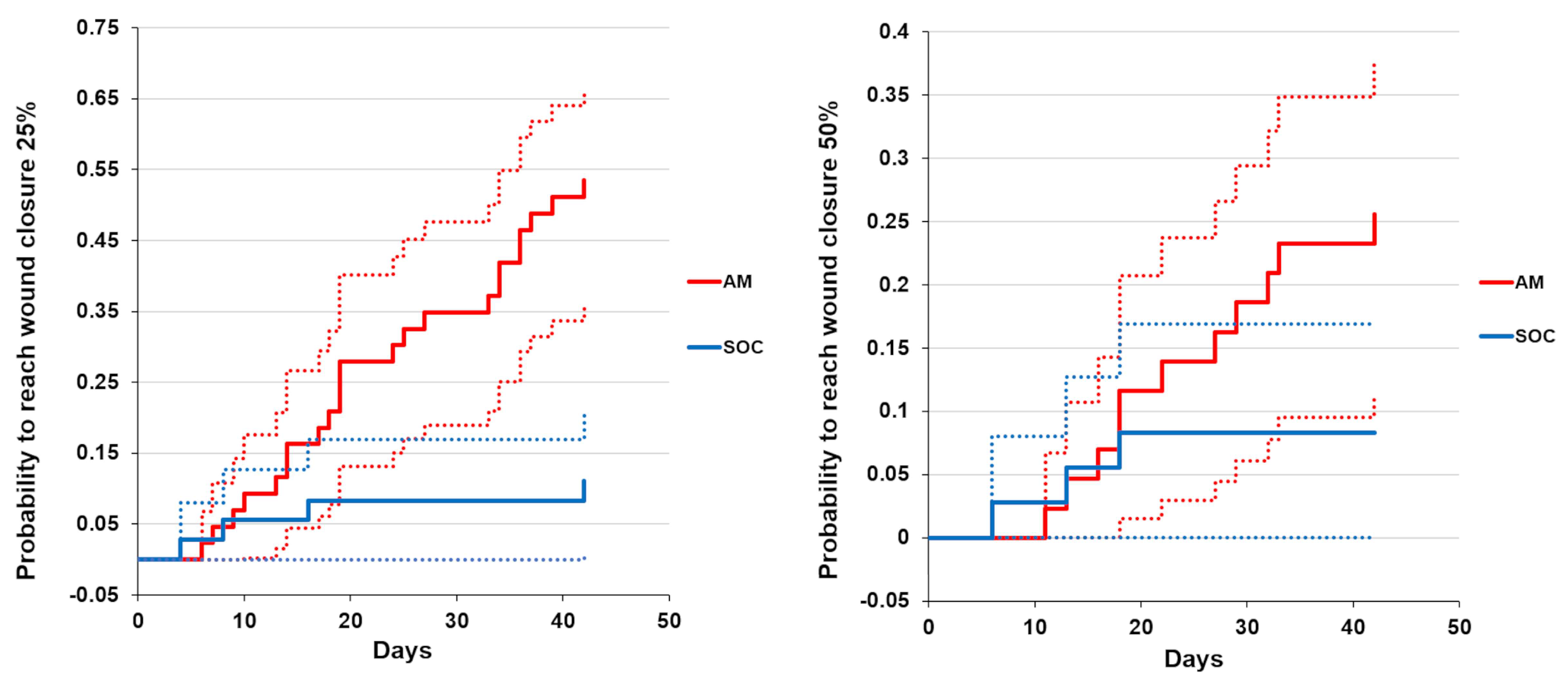
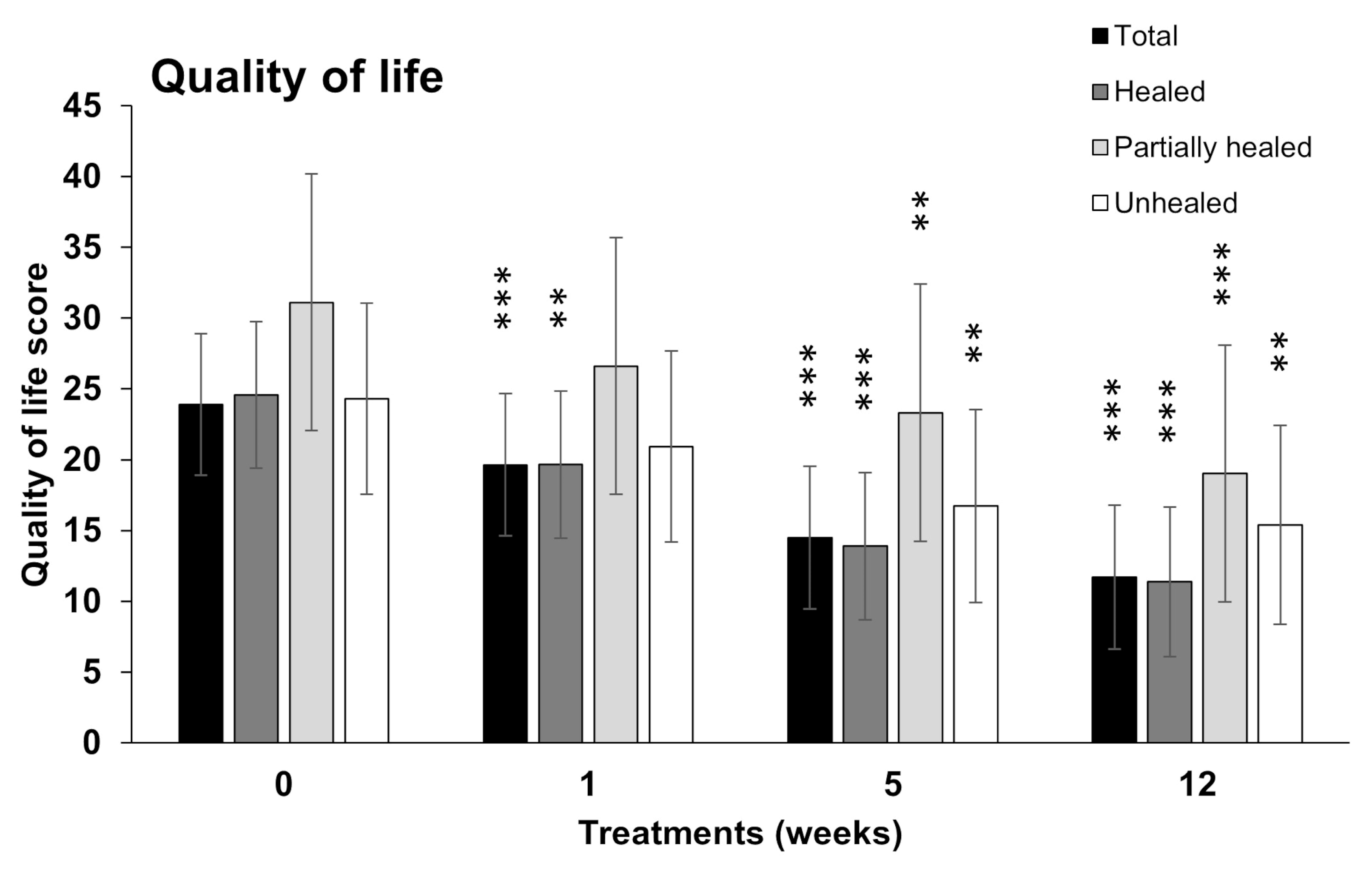
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jarbrink, K.; Ni, G.; Sonnergren, H.; Schmidtchen, A.; Pang, C.; Bajpai, R.; Car, J. The humanistic and economic burden of chronic wounds: A protocol for a systematic review. Syst. Rev. 2017, 6, 15. [Google Scholar] [CrossRef] [PubMed]
- Maita, K.C.; Avila, F.R.; Torres-Guzman, R.A.; Garcia, J.P.; Eldaly, A.S.; Palmieri, L.; Emam, O.S.; Ho, O.; Forte, A.J. Local anti-inflammatory effect and immunomodulatory activity of chitosan-based dressing in skin wound healing: A systematic review. J. Clin. Transl. Res. 2022, 8, 488–498. [Google Scholar]
- Posnett, J.; Gottrup, F.; Lundgren, H.; Saal, G. The resource impact of wounds on health-care providers in Europe. J. Wound Care 2009, 18, 154–161. [Google Scholar] [CrossRef]
- Gottrup, F.; Apelqvist, J.; Bjarnsholt, T.; Cooper, R.; Moore, Z.; Peters, E.J.; Probst, S. EWMA document: Antimicrobials and non-healing wounds. Evidence, controversies and suggestions. J. Wound Care 2013, 22, S1–S89. [Google Scholar] [CrossRef]
- Zelen, C.M.; Serena, T.E.; Denoziere, G.; Fetterolf, D.E. A prospective randomised comparative parallel study of amniotic membrane wound graft in the management of diabetic foot ulcers. Int. Wound J. 2013, 10, 502–507. [Google Scholar] [CrossRef] [PubMed]
- Mekkes, J.R.; Loots, M.A.; Van Der Wal, A.C.; Bos, J.D. Causes, investigation and treatment of leg ulceration. Br. J. Dermatol. 2003, 148, 388–401. [Google Scholar] [CrossRef]
- Mustoe, T.A.; O’Shaughnessy, K.; Kloeters, O. Chronic wound pathogenesis and current treatment strategies: A unifying hypothesis. Plast. Reconstr. Surg. 2006, 117, 35S–41S. [Google Scholar] [CrossRef]
- Frykberg, R.G.; Banks, J. Challenges in the Treatment of Chronic Wounds. Adv. Wound Care 2015, 4, 560–582. [Google Scholar] [CrossRef]
- Price, D.D.; McGrath, P.A.; Rafii, A.; Buckingham, B. The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain 1983, 17, 45–56. [Google Scholar] [CrossRef]
- Gomes, F.; Schuetz, P.; Bounoure, L.; Austin, P.; Ballesteros-Pomar, M.; Cederholm, T.; Fletcher, J.; Laviano, A.; Norman, K.; Poulia, K.A.; et al. ESPEN guidelines on nutritional support for polymorbid internal medicine patients. Clin. Nutr. 2018, 37, 336–353. [Google Scholar] [CrossRef] [PubMed]
- Forbes, J.; Fetterolf, D.E. Dehydrated amniotic membrane allografts for the treatment of chronic wounds: A case series. J. Wound Care 2012, 21, 294–296. [Google Scholar] [CrossRef]
- El Heneidy, H.; Omran, E.; Halwagy, A.; Al-Inany, H.; Al-Ansary, M.; Gad, A. Amniotic membrane can be a valid source for wound healing. Int. J. Womens Health 2016, 8, 225–231. [Google Scholar] [CrossRef]
- Sathyaraj, W.V.; Prabakaran, L.; Bhoopathy, J.; Dharmalingam, S.; Karthikeyan, R.; Atchudan, R. Therapeutic Efficacy of Polymeric Biomaterials in Treating Diabetic Wounds-An Upcoming Wound Healing Technology. Polymers 2023, 15, 1205. [Google Scholar] [CrossRef]
- Pourmoussa, A.; Gardner, D.J.; Johnson, M.B.; Wong, A.K. An update and review of cell-based wound dressings and their integration into clinical practice. Ann. Transl. Med. 2016, 4, 457. [Google Scholar] [CrossRef]
- Huerta, C.T.; Voza, F.A.; Ortiz, Y.Y.; Liu, Z.J.; Velazquez, O.C. Mesenchymal stem cell-based therapy for non-healing wounds due to chronic limb-threatening ischemia: A review of preclinical and clinical studies. Front. Cardiovasc. Med. 2023, 10, 1113982. [Google Scholar] [CrossRef] [PubMed]
- Wei, Q.; Liu, X.; Su, J.L.; Wang, Y.X.; Chu, Z.Q.; Ma, K.; Huang, Q.L.; Li, H.H.; Fu, X.B.; Zhang, C.P. Small extracellular vesicles from mesenchymal stem cells: A potential Weapon for chronic non-healing wound treatment. Front. Bioeng. Biotechnol. 2023, 10, 1083459. [Google Scholar] [CrossRef] [PubMed]
- Shaabani, E.; Sharifiaghdam, M.; Faridi-Majidi, R.; De Smedt, S.C.; Braeckmans, K.; Fraire, J.C. Gene therapy to enhance angiogenesis in chronic wounds. Mol. Ther. Nucleic Acids 2022, 29, 871–899. [Google Scholar] [CrossRef]
- Dadkhah Tehrani, F.; Firouzeh, A.; Shabani, I.; Shabani, A. A Review on Modifications of Amniotic Membrane for Biomedical Applications. Front. Bioeng. Biotechnol. 2020, 8, 606982. [Google Scholar] [CrossRef] [PubMed]
- Leal-Marin, S.; Thomas, K.; Nicola, H.; Olena, P.; Carsten, F.; Martin, B.; Constanca, F.; Birgit, G.; Oleksandr, G. Human Amniotic Membrane: A review on tissue engineering, application, and storage. J. Biomed. Mater. Res. B Appl. Biomater. 2020, 109, 1198–1215. [Google Scholar] [CrossRef]
- Koizumi, N.J.; Inatomi, T.J.; Sotozono, C.J.; Fullwood, N.J.; Quantock, A.J.; Kinoshita, S. Growth factor mRNA and protein in preserved human amniotic membrane. Curr. Eye Res. 2000, 20, 173–177. [Google Scholar] [CrossRef]
- Malhotra, C.; Jain, A.K. Human amniotic membrane transplantation: Different modalities of its use in ophthalmology. World J. Transplant. 2014, 4, 111–121. [Google Scholar] [CrossRef] [PubMed]
- Litwiniuk, M.; Krejner, A.; Speyrer, M.S.; Gauto, A.R.; Grzela, T. Hyaluronic Acid in Inflammation and Tissue Regeneration. Wounds 2016, 28, 78–88. [Google Scholar]
- Litwiniuk, M.; Radowicka, M.; Krejner, A.; Grzela, T. The influence of amniotic membrane extracts on cell growth depends on the part of membrane and childbirth mode selected: A proof-of-concept study. J. Wound Care 2017, 26, 498–503. [Google Scholar] [CrossRef]
- Nejad, A.R.; Hamidieh, A.A.; Amirkhani, M.A.; Sisakht, M.M. Update review on five top clinical applications of human amniotic membrane in regenerative medicine. Placenta 2021, 103, 104–119. [Google Scholar] [CrossRef] [PubMed]
- Svobodova, A.; Vrkoslav, V.; Smeringaiova, I.; Jirsova, K. Distribution of an analgesic palmitoylethanolamide and other N-acylethanolamines in human placental membranes. PLoS ONE 2023, 18, e0279863. [Google Scholar] [CrossRef]
- Farivar, B.S.; Toursavadkohi, S.; Monahan, T.S.; Sharma, J.; Ucuzian, A.A.; Kundi, R.; Sarkar, R.; Lal, B.K. Prospective study of cryopreserved placental tissue wound matrix in the management of chronic venous leg ulcers. J. Vasc. Surg. Venous Lymphat. Disord. 2019, 7, 228–233. [Google Scholar] [CrossRef] [PubMed]
- Serena, T.E.; Orgill, D.P.; Armstrong, D.G.; Galiano, R.D.; Glat, P.M.; Carter, M.J.; Kaufman, J.P.; Li, W.W.; Zelen, C.M. A Multicenter, Randomized, Controlled, Clinical Trial Evaluating Dehydrated Human Amniotic Membrane in the Treatment of Venous Leg Ulcers. Plast. Reconstr. Surg. 2022, 150, 1128–1136. [Google Scholar] [CrossRef]
- Ananian, C.E.; Dhillon, Y.S.; Van Gils, C.C.; Lindsey, D.C.; Otto, R.J.; Dove, C.R.; Pierce, J.T.; Saunders, M.C. A multicenter, randomized, single-blind trial comparing the efficacy of viable cryopreserved placental membrane to human fibroblast-derived dermal substitute for the treatment of chronic diabetic foot ulcers. Wound Repair. Regen. 2018, 26, 274–283. [Google Scholar] [CrossRef]
- Lavery, L.; Fulmer, J.; Shebetka, K.A.; Regulski, M.; Vayser, D.; Fried, D.; Kashefsky, H.; Owings, T.M.; Nadarajah, J.; Hesp, Z. Open-label Extension Phase of a Chronic Diabetic Foot Ulcer Multicenter, Controlled, Randomized Clinical Trial Using Cryopreserved Placental Membrane. Wounds 2018, 30, 283–289. [Google Scholar]
- Eskandarlou, M.; Azimi, M.; Rabiee, S.; Seif Rabiee, M.A. The Healing Effect of Amniotic Membrane in Burn Patients. World J. Plast. Surg. 2016, 5, 39–44. [Google Scholar]
- Loeffelbein, D.J.; Rohleder, N.H.; Eddicks, M.; Baumann, C.M.; Stoeckelhuber, M.; Wolff, K.D.; Drecoll, E.; Steinstraesser, L.; Hennerbichler, S.; Kesting, M.R. Evaluation of human amniotic membrane as a wound dressing for split-thickness skin-graft donor sites. Biomed. Res. Int. 2014, 2014, 572183. [Google Scholar] [CrossRef][Green Version]
- Tettelbach, W.; Cazzell, S.; Reyzelman, A.M.; Sigal, F.; Caporusso, J.M.; Agnew, P.S. A confirmatory study on the efficacy of dehydrated human amnion/chorion membrane dHACM allograft in the management of diabetic foot ulcers: A prospective, multicentre, randomised, controlled study of 110 patients from 14 wound clinics. Int. Wound J. 2019, 16, 19–29. [Google Scholar] [CrossRef]
- Svobodova, A.; Horvath, V.; Smeringaiova, I.; Cabral, J.V.; Zemlickova, M.; Fiala, R.; Burkert, J.; Nemetova, D.; Stadler, P.; Lindner, J.; et al. The healing dynamics of non-healing wounds using cryo-preserved amniotic membrane. Int. Wound J. 2022, 19, 1243–1252. [Google Scholar] [CrossRef] [PubMed]
- Horvath, V.; Svobodova, A.; Cabral, J.V.; Fiala, R.; Burkert, J.; Stadler, P.; Lindner, J.; Bednar, J.; Zemlickova, M.; Jirsova, K. Inter-placental variability is not a major factor affecting the healing efficiency of amniotic membrane when used for treating chronic non-healing wounds. Cell Tissue Bank. 2023. [Google Scholar] [CrossRef] [PubMed]
- Blome, C.; Baade, K.; Price, P.; Debus, E.S.; Augustin, M. The ‘Wound-QoL’: A Short Questionnaire Measuring Quality of Life in Patients with Chronic Wounds. Wound Repair. Regen. 2014, 22, 504–514. [Google Scholar] [CrossRef]
- Snyder, D.; Sullivan, N.; Margolis, D.; Schoelles, K. Skin Substitutes for Treating Chronic Wounds; Technology Assessment Program—Technical Brief; Project ID: WNDT0818; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2020. [Google Scholar]
- Fitzmaurice, G.M.; Laird, N.M.; Ware, J.H. Applied Longitudinal Analysis, 2nd ed.; John Wiley & Sons: Hoboken, NJ, USA, 2004. [Google Scholar]
- Laird, N.M.; Ware, J.H. Random-effects models for longitudinal data. Biometrics 1982, 38, 963–974. [Google Scholar]
- Dmitrienko, A.; Tamhane, A.C.; Bretz, F. Multiple Testing Problems in Pharmaceutical Statistics, 1st ed.; CRC Press: New York, NY, USA, 2009. [Google Scholar]
- Kaplan, E.L.; Meier, P. Nonparametric Estimation from Incomplete Observations. J. Amer. Statist. Assoc. 1958, 53, 457–481. [Google Scholar] [CrossRef]
- Aalen, O.O.; Borgan, Ø.; Gjessing, H.K. Survival and Event History Analysis: A Process Point of View; Springer: Berlin/Heidelberg, Germany, 2008; pp. 90–104. [Google Scholar]
- Wood, S.N. Generalized Additive Models: An Introduction with R, 2nd ed.; Chapman and Hall/CRC: Boca Raton, FL, USA, 2017. [Google Scholar]
- Wood, S.N.; Pya, N.; Säfken, B. Smoothing Parameter and Model Selection for General Smooth Models. J. Am. Stat. Assoc. 2017, 111, 1548–1563. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2020; Available online: http://www.r-project.org/index.html (accessed on 15 January 2023).
- Beyene, R.T.; Derryberry, S.L., Jr.; Barbul, A. The Effect of Comorbidities on Wound Healing. Surg. Clin. N. Am. 2020, 100, 695–705. [Google Scholar] [CrossRef] [PubMed]
- Raspovic, K.M.; Wukich, D.K.; Naiman, D.Q.; Lavery, L.A.; Kirsner, R.S.; Kim, P.J.; Steinberg, J.S.; Attinger, C.E.; Danilkovitch, A. Effectiveness of viable cryopreserved placental membranes for management of diabetic foot ulcers in a real world setting. Wound Repair. Regen. 2018, 26, 213–220. [Google Scholar] [CrossRef] [PubMed]
- Ananian, C.E.; Davis, R.D.; Johnson, E.L.; Regulski, M.J.; Reyzelman, A.M.; Saunders, M.C.; Danilkovitch, A. Wound Closure Outcomes Suggest Clinical Equivalency between Lyopreserved and Cryopreserved Placental Membranes Containing Viable Cells. Adv. Wound Care 2019, 8, 546–554. [Google Scholar] [CrossRef] [PubMed]
- Lavery, L.A.; Fulmer, J.; Shebetka, K.A.; Regulski, M.; Vayser, D.; Fried, D.; Kashefsky, H.; Owings, T.M.; Nadarajah, J.; Grafix Diabetic Foot Ulcer Study, G. The efficacy and safety of Grafix((R)) for the treatment of chronic diabetic foot ulcers: Results of a multi-centre, controlled, randomised, blinded, clinical trial. Int. Wound J. 2014, 11, 554–560. [Google Scholar] [CrossRef] [PubMed]
- Zelen, C.M.; Serena, T.E.; Gould, L.; Le, L.; Carter, M.J.; Keller, J.; Li, W.W. Treatment of chronic diabetic lower extremity ulcers with advanced therapies: A prospective, randomised, controlled, multi-centre comparative study examining clinical efficacy and cost. Int. Wound J. 2015, 13, 272–282. [Google Scholar] [CrossRef] [PubMed]
- Valiente, M.R.; Nicolas, F.J.; Garcia-Hernandez, A.M.; Fuente Mora, C.; Blanquer, M.; Alcaraz, P.J.; Almansa, S.; Merino, G.R.; Lucas, M.D.L.; Alguero, M.C.; et al. Cryopreserved amniotic membrane in the treatment of diabetic foot ulcers: A case series. J. Wound Care 2018, 27, 806–815. [Google Scholar] [CrossRef]
- Zidan, S.M.; Eleowa, S.A.; Nasef, M.A.; Abd-Almoktader, M.A.; Elbatawy, A.M.; Borhamy, A.G.; Aboliela, M.A.; Ali, A.M.; Algamal, M.R. Maximizing the safety of glycerol preserved human amniotic membrane as a biological dressing. Burns 2015, 41, 1498–1503. [Google Scholar] [CrossRef]
- Kadkhoda, Z.; Tavakoli, A.; Chokami Rafiei, S.; Zolfaghari, F.; Akbari, S. Effect of Amniotic Membrane Dressing on Pain and Healing of Palatal Donor Site: A Randomized Controlled Trial. Int. J. Organ. Transplant. Med. 2020, 11, 55–62. [Google Scholar]
- Vaheb, M.; Kohestani, B.M.; Karrabi, M.; Khosrojerdi, M.; Khajeh, M.; Shahrestanaki, E.; Sahebkar, M. Evaluation of Dried Amniotic Membrane on Wound Healing at Split-Thickness Skin Graft Donor Sites: A Randomized, Placebo-Controlled, Double-blind Trial. Adv. Skin. Wound Care 2020, 33, 636–641. [Google Scholar] [CrossRef]
- Tseng, S.C. HC-HA/PTX3 Purified from Amniotic Membrane as Novel Regenerative Matrix: Insight into Relationship between Inflammation and Regeneration. Investig. Ophthalmol. Vis. Sci. 2016, 57, ORSFh1–ORSFh8. [Google Scholar] [CrossRef]
- Vrkoslav, V.; Smeringaiova, I.; Smorodinova, N.; Svobodova, A.; Strnad, S.; Jackson, C.J.; Burkert, J.; Jirsova, K. Quantification of Analgesic and Anti-Inflammatory Lipid Mediators in Long-Term Cryopreserved and Freeze-Dried Preserved Human Amniotic Membrane. Bioengineering 2023, 10, 740. [Google Scholar] [CrossRef]

| Patients | All Patients | SOC Patients | AM Patients |
|---|---|---|---|
| Number of Patients | 42 (100%) | 29 (100%) | 35 (100%) |
| Age, in years (mean ± SD) | 65 ± 14 | 65 ± 16 | 67 ± 12 |
| Age ≥ 65 years: N, (%) | 28 (67) | 21 (72) | 25 (71) |
| Male (N, %) | 27 (64) | 19 (66) | 23 (66) |
| Smoker (N, %) | 7 (17) | 5 (17) | 6 (17) |
| BMI (mean ± SD) | 29 ± 5 | 29 ± 5 | 29 ± 5 |
| Obese BMI ≥ 30 (N, %) | 13 (31) | 8 (28) | 10 (29) |
| Diabetes mellitus II (N, %) | 11 (26) | 9 (31) | 10 (29) |
| HbA1c (mean % ± SD) | 6.1 ± 1.1 | 6.2 ± 1.2 | 6.1 ± 1.1 |
| Albumin (g/L) (mean ± SD) | 40 ± 5 | 40 ± 5 | 40 ± 5 |
| Albumin ≤ 35 g/L (N, %) | 8 (19) | 5 (17) | 7 (20) |
| Total protein (g/L) (mean ± SD) | 72 ± 6 | 72 ± 5 | 72 ± 6 |
| ABI 0.6–0.9 (N, %) | 12 (29) | 7 (24) | 11 (31) |
| ABI > 0.9 (N, %) | 15 (36) | 11 (38) | 11 (31) |
| Comorbidities | |||
| Two and more chronic diseases (N, %) | 32 (76) | 22 (76) | 28 (80) |
| Three and more chronic diseases (N, %) | 23 (55) | 16 (55) | 20 (58) |
| Five and more chronic diseases (N, %) | 9 (21) | 6 (21) | 8 (23) |
| Wounds | All Defects | SOC Defects | AM Defects |
| Number of Wounds | 54 (100%) | 36 (100%) | 43 (100%) |
| Start size (mean ± SD, cm2) | 20 ± 23 | 22 ± 23 | 16 ± 19 |
| Time from onset (weeks, mean ± SD) | 124 ± 219 | 144 ± 257 | 167 ± 290 |
| Time from onset >1 year (weeks) | 21 (39) | 16 (44) | 18 (42) |
| Type | |||
| Venous (N, %) | 37 (68) | 23 (63) | 32 (74) |
| Arterial (N, %) | 6 (11) | 5 (14) | 2 (5) |
| Traumatic (N, %) | 6 (11) | 5 (14) | 5 (12) |
| Postoperative (N, %) | 3 (6) | 1 (3) | 2 (5) |
| Pressure (N, %) | 1 (2) | 1 (3) | 1 (2) |
| Diabetic (N, %) | 1 (2) | 1 (3) | 1 (2) |
| Location | |||
| Calf/Midfoot (N, %) | 29 (54) | 20 (55) | 22 (51) |
| Forefoot (N, %) | 5 (9) | 5 (14) | 3 (7) |
| Hindfoot/ankle (N, %) | 17 (31) | 9 (25) | 16 (38) |
| Toe (N, %) | 1 (2) | 1 (3) | 1 (2) |
| Other (N, %) | 2 (4) | 1 (3) | 1 (2) |
| Wound Treatment | SOC | SOC-H | SOC-PH | SOC-UH | AM | AM-H | AM-PH | AM-UH |
|---|---|---|---|---|---|---|---|---|
| No of wounds: N (%) | 36 (100) | 7 (19.4) | 1 (2.8) | 28 (77.8) | 43 (100) | 24 (55.8) | 10 (23.3) | 9 (20.9) |
| Start size (mean ± SD, cm2) | 22 ± 23 | 23 ± 30 | 87 ± NA | 20 ± 18 | 16 ± 19 | 15 ± 15 | 20 ± 29 | 15 ± 15 |
| Start size median | 12.2 | 10 | 87 | 12.2 | 11.2 | 8 | 10.3 | 8.6 |
| End size (mean ± SD, cm2) | 16 ± 18 | 0 ± 0 | 17.4 | 20 ± 18 | 5 ± 11 | 0 ± 0 | 6 ± 7 | 17 ± 17 |
| End size median | 9.2 | 0 | 17.4 | 11.7 | 10.7 | 0 | 3.4 | 9.7 |
| Wound closure area (%) | 21 | 100 | 80.1 | −0.8 | 68.5 | 100 | 70.3 | −16.6 |
| Treatment duration (mean ± SD, weeks) | 14 ± 24 | 30 ± 44 | 87 | 8 ± 3 | 34 ± 23 | 30 ± 18 | 55 ± 26 | 23 ± 18 |
| Treatment duration (median, weeks) | 7 | 17 | 87 | 7 | 31 | 30 | 56 | 15 |
| Mean N of AM applications (from-to) | NA | NA | NA | NA | 24 (4–68) | 20 (4–43) | 38 (14–68) | 18 (4–45) |
| Number of visits | 9 | 11 | 74 | 6 | 29 | 26 | 44 | 19 |
| Wound Type | SOC | SOC-H | SOC-PH | SOC-UH | AM | AM-H | AM-PH | AM-UH |
|---|---|---|---|---|---|---|---|---|
| Venous (N, %) | 23 (100) | 2 (9) | 1 (4) | 20 (87) | 32 (100) | 16 (50) | 8 (25) | 8 (25) |
| Arterial (N, %) | 5 (100) | 3 (60) | 0 (0) | 2 (40) | 2 (100) | 2 (100) | 0 (0) | 0 (0) |
| Traumatic (N, %) | 5 (100) | 1 (20) | 0 (0) | 4 (80) | 5 (100) | 4 (80) | 0 (0) | 1 (20) |
| Postoperative (N, %) | 1 (100) | 1 (100) | 0 (0) | 0 (0) | 2 (100) | 1 (50) | 1 (50) | 0 (0) |
| Pressure (N, %) | 1 (100) | 0 (0) | 0 (0) | 1 (100) | 1 (100) | 0 (0) | 1 (100) | 0 (0) |
| Diabetic (N, %) | 1 (100) | 0 (0) | 0 (0) | 1 (100) | 1 (100) | 1 (100) | 0 (0) | 0 (0) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Svobodova, A.; Horvath, V.; Balogh, L.; Zemlickova, M.; Fiala, R.; Burkert, J.; Brabec, M.; Stadler, P.; Lindner, J.; Bednar, J.; et al. Outcome of Application of Cryopreserved Amniotic Membrane Grafts in the Treatment of Chronic Nonhealing Wounds of Different Origins in Polymorbid Patients: A Prospective Multicenter Study. Bioengineering 2023, 10, 900. https://doi.org/10.3390/bioengineering10080900
Svobodova A, Horvath V, Balogh L, Zemlickova M, Fiala R, Burkert J, Brabec M, Stadler P, Lindner J, Bednar J, et al. Outcome of Application of Cryopreserved Amniotic Membrane Grafts in the Treatment of Chronic Nonhealing Wounds of Different Origins in Polymorbid Patients: A Prospective Multicenter Study. Bioengineering. 2023; 10(8):900. https://doi.org/10.3390/bioengineering10080900
Chicago/Turabian StyleSvobodova, Alzbeta, Vojtech Horvath, Lukas Balogh, Martina Zemlickova, Radovan Fiala, Jan Burkert, Marek Brabec, Petr Stadler, Jaroslav Lindner, Jan Bednar, and et al. 2023. "Outcome of Application of Cryopreserved Amniotic Membrane Grafts in the Treatment of Chronic Nonhealing Wounds of Different Origins in Polymorbid Patients: A Prospective Multicenter Study" Bioengineering 10, no. 8: 900. https://doi.org/10.3390/bioengineering10080900
APA StyleSvobodova, A., Horvath, V., Balogh, L., Zemlickova, M., Fiala, R., Burkert, J., Brabec, M., Stadler, P., Lindner, J., Bednar, J., & Jirsova, K. (2023). Outcome of Application of Cryopreserved Amniotic Membrane Grafts in the Treatment of Chronic Nonhealing Wounds of Different Origins in Polymorbid Patients: A Prospective Multicenter Study. Bioengineering, 10(8), 900. https://doi.org/10.3390/bioengineering10080900








