Effects of Midsole Hardness on the Mechanical Response Characteristics of the Plantar Fascia during Running
Abstract
1. Introduction
2. Methods
2.1. Subject and Shoes
2.2. Construction of the 3D FE Foot–Shoe Model
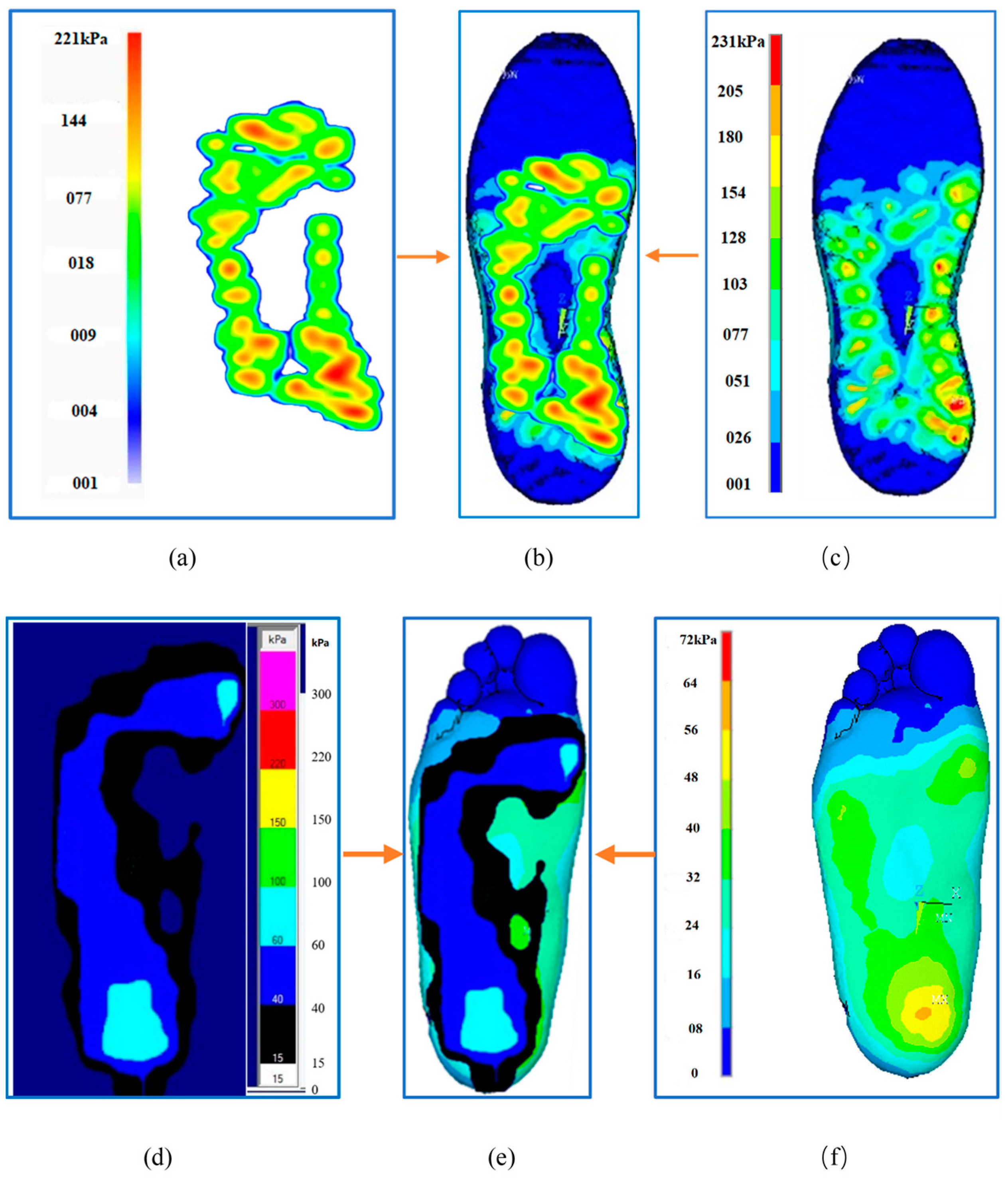
2.3. FE Model Validation
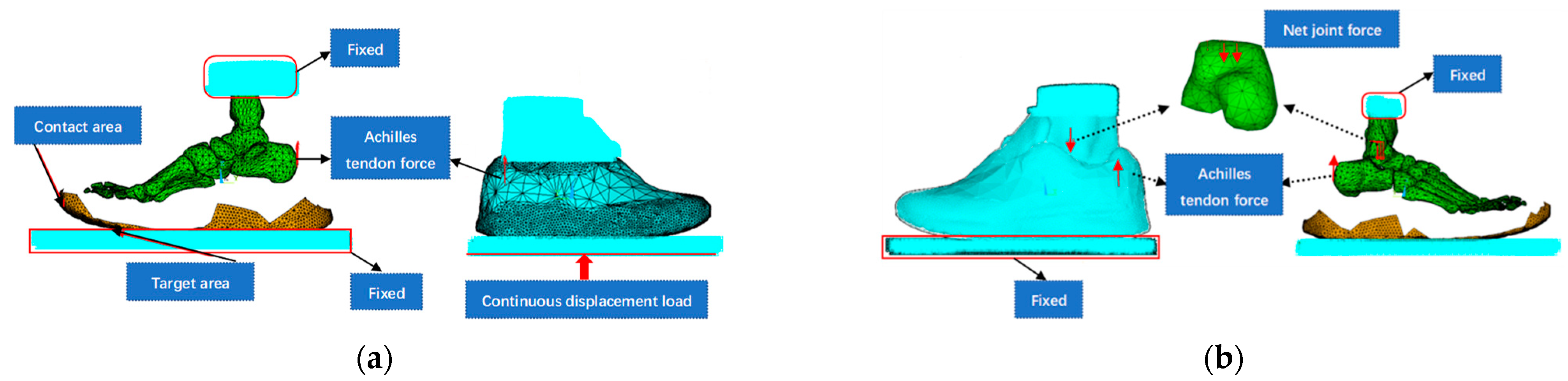
2.3.1. Finite-Element Simulation of a Balanced Standing Position
2.3.2. Foot and Sole Pressure/Distribution Data Testing
2.4. FE Simulation of the Mechanical Response of the PF to Midsole Hardness
2.4.1. Load Acquisition Simulation Experiments
2.4.2. Loading Mode and Hardness Parameter Setting
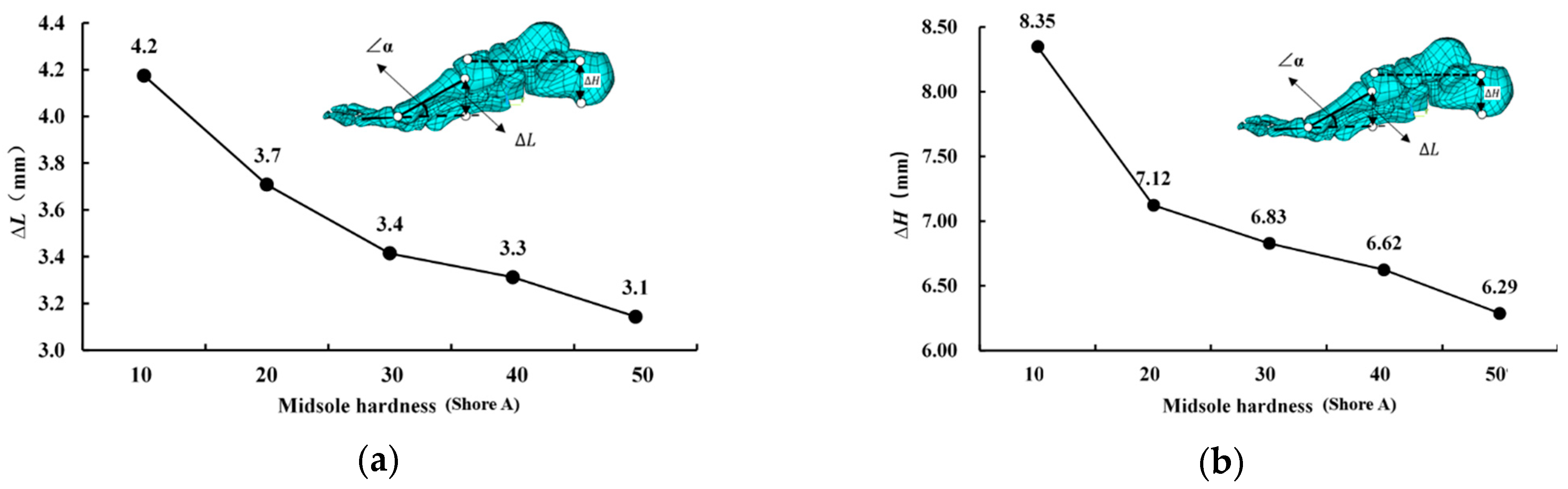
2.5. Correlation Index Definition
3. Results
3.1. Validation of the FE Foot–Shoe Model
3.2. Effects of Midsole Hardness on the PF and Its Mechanical Mechanism
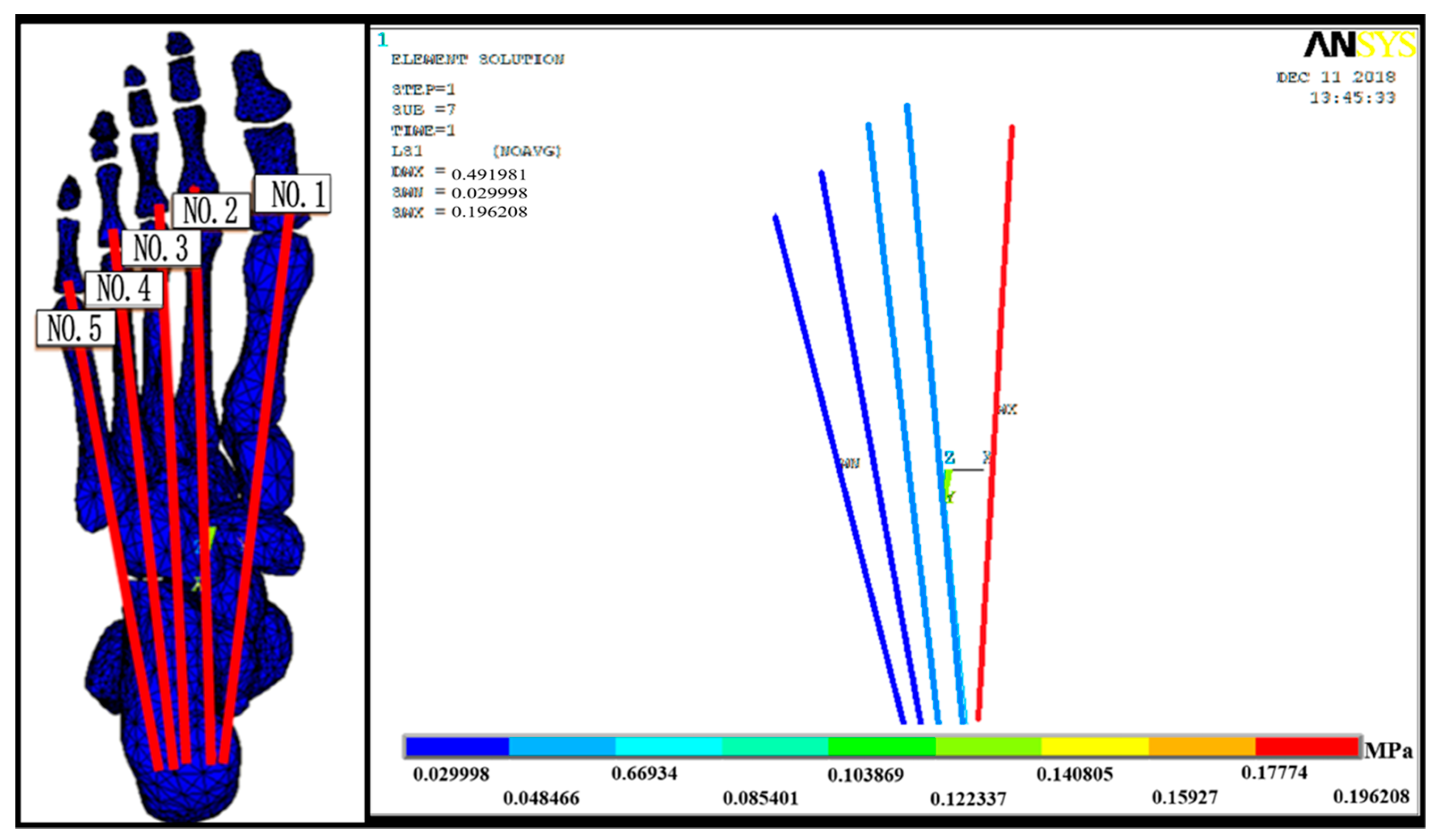
3.2.1. PF Stress–Strain Results
3.2.2. Mechanical Response Results of Risk Factors for Plantar Fasciitis
4. Discussion
4.1. Validity of 3D Finite-Element Foot–Shoe Model
4.2. Biomechanical Mechanisms of the Effects of Midsole Hardness on the PF
4.3. Limitation
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pfeffer, G.; Bacchetti, P.; Deland, J.; Lewis, A.; Anderson, R.; Davis, W.; Alvarez, R.; Brodsky, J.; Cooper, P.; Frey, C.; et al. Comparison of Custom and Prefabricated Orthoses in the Initial Treatment of Proximal Plantar Fasciitis. Foot Ankle Int. 1999, 20, 214–221. [Google Scholar]
- Ballas, M.T.; Tytko, J.; Cookson, D. Common overuse running injuries: Diagnosis and management. Am. Fam. Physician 1997, 55, 2473–2484. [Google Scholar] [PubMed]
- Roxas, M. Plantar fasciitis: Diagnosis and therapeutic considerations. Altern. Med. Rev. 2005, 10, 83–93. [Google Scholar]
- Agyekum, E.K.; Ma, K. Heel pain: A systematic review. Chin. J. Traumatol. 2015, 18, 164–169. [Google Scholar] [PubMed]
- Rome, K.; Howe, T.; Haslock, I. Risk factors associated with the development of plantar heel pain in athletes. Foot 2001, 11, 119–125. [Google Scholar] [CrossRef]
- Ribeiro, A.P.; João, S.M.A.; Dinato, R.C.; Tessutti, V.D.; Sacco, I.C.N. Dynamic Patterns of Forces and Loading Rate in Runners with Unilateral Plantar Fasciitis: A Cross-Sectional Study. PLoS ONE 2015, 10, e0136971. [Google Scholar]
- Liu, J.; Zhu, X.; Liu, H. Application of finite element method in biomechanical study of plantar fasciitis. Chin. J. Tissue Eng. Res. 2018, 22, 3900–3906. [Google Scholar]
- Wearing, S.C.; Smeathers, J.E.; Urry, S.R. The effect of plantar fasciitis on vertical foot-ground reaction force. Clin. Orthop. Relat. Res. 2003, 409, 175–185. [Google Scholar] [CrossRef] [PubMed]
- Riddle, D.L.; Pulisic, M.; Pidcoe, P.; Johnson, R.E. Risk factors for Plantar fasciitis: A matched case-control study. J. Bone Joint. Surg. Am. 2003, 85-A, 872–877. [Google Scholar] [CrossRef]
- Carlson, R.E.; Fleming, L.L.; Hutton, W.C. The biomechanical relationship between the tendoachilles, plantar fascia and metatarsophalangeal joint dorsiflexion angle. Foot Ankle Int. 2000, 21, 18–25. [Google Scholar] [PubMed]
- Wearing, S.C.; Smeathers, J.E.; Urry, S.R.; Hennig, E.M.; Hills, A.P. The pathomechanics of plantar fasciitis. Sports Med. 2006, 36, 585–611. [Google Scholar] [CrossRef]
- Lurati, A.R. Flat Feet and a Diagnosis of Plantar Fasciitis in a Marine Corps Recruit. Workplace Health Saf. 2015, 63, 136–138. [Google Scholar] [CrossRef] [PubMed]
- Baltich, J.; Maurer, C.; Nigg, B.M. Increased vertical impact forces and altered running mechanics with softer midsole shoes. PLoS ONE 2015, 10, e0125196. [Google Scholar] [CrossRef] [PubMed]
- Nigg, B.M.; Baltich, J.; Maurer, C.; Federolf, P. Shoe midsole hardness, sex and age effects on lower extremity kinematics during running. J. Biomech. 2012, 45, 1692–1697. [Google Scholar] [CrossRef] [PubMed]
- Theisen, D.; Malisoux, L.; Genin, J.; Delattre, N.; Seil, R.; Urhausen, A. Influence of midsole hardness of standard cushioned shoes on running-related injury risk. Br. J. Sports Med. 2014, 48, 371–376. [Google Scholar] [CrossRef]
- Li, M.; Liu, A.M.; Wang, F.; Richard, J.; Wang, D. The effect of lateral wedge insoles with different stiffness on knee adduction moment. Yiyong Shengwu Lixue/J. Med. Biomech. 2017, 32, 524–528. [Google Scholar]
- Shorten, M.; Mientjes, M.I. The “heel impact” force peak during running is neither “heel” nor “impact” and does not quantify shoe cushioning effects. Footwear Sci. 2011, 3, 41–58. [Google Scholar] [CrossRef]
- Sterzing, T.; Schweiger, V.; Ding, R.; Cheung, T.M.; Brauner, T. Influence of rearfoot and forefoot midsole hardness on biomechanical and perception variables during heel-toe running. Footwear Sci. 2013, 5, 71–79. [Google Scholar] [CrossRef]
- Leardini, A.; Benedetti, M.G.; Catani, F.; Simoncini, L.; Giannini, S. An anatomically based protocol for the description of foot segment kinematics during gait. Clin. Biomech. 1999, 14, 528–536. [Google Scholar] [CrossRef] [PubMed]
- Pohl, M.B.; Buckley, J. Changes in foot and shank coupling due to alterations in foot strike pattern during running. Clin. Biomech. 2008, 23, 334. [Google Scholar] [CrossRef]
- Mendes, A. An overview of plantar fasciitis. Br. J. Community Nurs. 2016, 21, 160. [Google Scholar] [CrossRef]
- Neufeld, S.K.; Cerrato, R. Plantar fasciitis: Evaluation and treatment. J. Am. Acad. Orthop. Surg. 2008, 16, 338–346. [Google Scholar] [CrossRef] [PubMed]
- Muth, C.C. Plantar Fasciitis. JAMA 2017, 318, 400. [Google Scholar] [CrossRef] [PubMed]
- Hardin, E.C.; Bogert, A.J.V.D.; Hamill, J. Kinematic adaptations during running: Effects of footwear, surface, and duration. Med. Sci. Sport. Exerc. 2004, 36, 838. [Google Scholar] [CrossRef] [PubMed]
- Duan, Z.; Jiang, Y.; Huang, Q.; Yuan, Z.; Zhao, Q.; Wang, S.; Zhang, Y.; Tai, H. A do-it-yourself approach to achieving a flexible pressure sensor using daily use materials. J. Mater. Chem. C 2021, 9, 13659–13667. [Google Scholar] [CrossRef]
- Blades, S.; Marriott, H.; Hundza, S.; Honert, E.C.; Stellingwerff, T.; Klimstra, M. Evaluation of Different Pressure-Based Foot Contact Event Detection Algorithms across Different Slopes and Speeds. Sensors 2023, 23, 2736. [Google Scholar] [CrossRef]
- Kim, S.; Cho, J.; Choi, J.; Ryu, S.; Jeong, W. Coupled foot-shoe-ground interaction model to assess landing impact transfer characteristics to ground condition. Interact. Multiscale Mech. 2012, 5, 75–90. [Google Scholar] [CrossRef]
- Li, S.; Zhang, Y.; Gu, Y.; Ren, J. Stress distribution of metatarsals during forefoot strike versus rearfoot strike: A finite element study. Comput. Biol. Med. 2017, 91, 38–46. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.N.; Chang, C.W.; Li, C.T.; Chang, C.H.; Lin, C.F. Finite element analysis of plantar fascia during walking: A quasi-static simulation. Foot Ankle Int. 2015, 36, 90–97. [Google Scholar] [CrossRef] [PubMed]
- Shu-dong, L.I.; Yao-dong, G.U. A Finite Element Study of the Stress on Metatarsals during Forefoot Strike at Different Angles. China Sport Sci. 2018, 38, 67–72. [Google Scholar]
- Tao, K.; Wang, D.; Wang, C.; Wang, X. Effects of ligaments and plantar fascia on the foot finite element analysis. J. Biomed. Eng. 2008, 25, 336. [Google Scholar]
- Zhu, X.; Wang, H.; Liu, J.; Zhao, J.; Shen, Y. The difference of foot and ankle stress distribution based on finite element model with different ice-pushing angles. J. Med. Biomech. 2022, 37, 1138–1144. [Google Scholar]
- Nakamura, S.; Crowninshield, R.D.; Cooper, R.R. An analysis of soft tissue loading in the foot—A preliminary report. Bull Prosthet. Res. 1981, 10–35, 27–34. [Google Scholar]
- Siegler, S.; Block, J.; Schneck, C.D. The mechanical characteristics of the collateral ligaments of the human ankle joint. Foot Ankle 1988, 8, 234. [Google Scholar] [CrossRef] [PubMed]
- Athanasiou, K.A.; Liu, G.T.; Lavery, L.A.; Lanctot, D.R.; Schenck, R.C., Jr. Biomechanical topography of human articular cartilage in the first metatarsophalangeal joint. Clin. Orthop. Relat. Res. 1998, 348, 269–281. [Google Scholar] [CrossRef]
- Qiu, T.X.; Teo, E.C.; Yan, Y.B.; Lei, W. Finite element modeling of a 3D coupled foot-boot model. Med. Eng. Phys. 2011, 33, 1228–1233. [Google Scholar] [CrossRef] [PubMed]
- Cheung, J.T.-M.; Zhang, M. Parametric design of pressure-relieving foot orthosis using statistics-based finite element method. Med. Eng. Phys. 2008, 30, 269–277. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Yuan, Q.; Zhang, Z.; He, Y.; Huang, S. Parameter identification of constitutive models of rubber materials based on hyperstatic equations. J. Chongqing Univ. 2017, 40, 1–9. [Google Scholar]
- Franciosa, P.; Gerbino, S.; Lanzotti, A.; Silvestri, L. Improving comfort of shoe sole through experiments based on CAD-FEM modeling. Med. Eng. Phys. 2013, 35, 36–46. [Google Scholar] [CrossRef] [PubMed]
- Sun, D.; Fekete, G.; Baker, J.S.; Mei, Q.; István, B.; Zhang, Y.; Gu, Y. A Pilot Study of Musculoskeletal Abnormalities in Patients in Recovery from a Unilateral Rupture-Repaired Achilles Tendon. Int. J. Environ. Res. Public Health 2020, 17, 4642. [Google Scholar] [CrossRef]
- Cheung, J.T.; Zhang, M.; Leung, A.K.; Fan, Y.B. Three-dimensional finite element analysis of the foot during standing--a material sensitivity study. J. Biomech. 2005, 38, 1045–1054. [Google Scholar] [CrossRef]
- Lu, C.; Yu, B.; Chen, H.Q.; Lin, Q.R. Establishment of a three-dimensional finite element model and stress analysis of the talus during normal gait. Nan Fang Yi Ke Da Xue Xue Bao 2010, 30, 2273–2276. [Google Scholar] [PubMed]
- Cheung, J.T.-M.; Zhang, M. A 3-dimensional finite element model of the human foot and ankle for insole design. Arch. Phys. Med. Rehabil. 2005, 86, 353–358. [Google Scholar] [CrossRef] [PubMed]
- Sun, P.C.; Shih, S.L.; Chen, Y.L.; Hsu, Y.C.; Yang, R.C.; Chen, C.S. Biomechanical analysis of foot with different foot arch heights: A finite element analysis. Comput. Methods Biomech. Biomed. Eng. 2012, 15, 563–569. [Google Scholar] [CrossRef] [PubMed]
- Cheung, J.T.-M.; Zhang, M.; An, K.-N. Effect of Achilles tendon loading on plantar fascia tension in the standing foot. Clin. Biomech. 2006, 21, 194–203. [Google Scholar] [CrossRef]
- Guo, J.; Liu, X.; Ding, X.; Wang, L.; Fan, Y. Biomechanical and mechanical behavior of the plantar fascia in macro and micro structures. J. Biomech. 2018, 76, 160–166. [Google Scholar] [CrossRef] [PubMed]
- Kitaoka, H.B.; Luo, Z.P.; Growney, E.S.; Berglund, L.J.; An, K.N. Material properties of the plantar aponeurosis. Foot Ankle Int. 1994, 15, 557–560. [Google Scholar] [CrossRef]
- Lin, S.C.; Chen, C.P.C.; Tang, S.F.T.; Chen, C.W.; Wang, J.J.; Hsu, C.C.; Hsieh, J.H.; Chen, W.P. Stress distribution within the planter aponeurosis during during walking—A dynamic finite element analysis. J. Mech. Med. Biol. 2014, 14, 1450053. [Google Scholar] [CrossRef]
- Gefen, A.; Megido-Ravid, M.; Itzchak, Y.; Arcan, M. Biomechanical analysis of the three-dimensional foot structure during gait: A basic tool for clinical applications. J. Biomech. Eng. 2000, 122, 630–639. [Google Scholar] [CrossRef] [PubMed]
- De Wit, B.; De Clercq, D.; Lenoir, M. The Effect of Varying Midsole Hardness on impact Forces and Foot Motion during Foot Contact in Running. J. Appl. Biomech. 1995, 11, 395–406. [Google Scholar] [CrossRef]
- Cheng, H.-Y.K.; Lin, C.-L.; Chou, S.-W.; Wang, H.-W. Nonlinear finite element analysis of the plantar fascia due to the windlass mechanism. Foot Ankle Int. 2008, 29, 845–851. [Google Scholar] [CrossRef] [PubMed]
- Simkin, A. Structural Analysis of the Human Foot in Standing Posture; Tel-Aviv University: Tel Aviv-Yafo, Israel, 1982. [Google Scholar]
- Wei, L.; Fei, L.; Haiyang, H.; Teraili, A.; Xue, W.; Wahapu, P.; Chengwei, W. Biomechanical application of finite elements in the orthopedics of stiff clubfoot. BMC Musculoskelet. Disord. 2022, 23, 1112. [Google Scholar]
- Simonsen, E.B.; Svendsen, M.B.; Nørreslet, A.; Baldvinsson, H.K.; Heilskov-Hansen, T.; Larsen, P.K.; Alkjær, T.; Henriksen, M. Walking on high heels changes muscle activity and the dynamics of human walking significantly. J. Appl. Biomech. 2012, 28, 20–28. [Google Scholar] [CrossRef] [PubMed]
- Cronin, N.J.; Barrett, R.; Carty, C.P. Long-term use of high-heeled shoes alters the neuromechanics of human walking. J. Appl. Physiol. 2012, 112, 1054–1058. [Google Scholar] [CrossRef] [PubMed]

| Component | Young’s Modulus E (MPa) | Poisson’s Ratio V | Density (kg·m−3) | Cross-Sectional Area (mm−2) |
|---|---|---|---|---|
| Bony Structure | 7300 | 0.3 | 1500 | — |
| Soft Tissue | 1.15 | 0.49 | 937 | — |
| Ligaments | 260 | — | 937 | 18.4 |
| Cartilage | 1 | 0.4 | — | — |
| Plantar Fascia | 350 | — | 937 | 290.7 |
| Upper Part | 11.76 | 0.35 | 9400 | — |
| Midsole (10) | Third-order Yeoh hyperelastic model (C10 = 0.052; C20 = −0.074; C30 = 0.072) | |||
| Midsole (20) | Third-order Yeoh hyperelastic model (C10 = 0.127; C20 = −0.149; C30 = 0.153) | |||
| Midsole (30) | Third-order Yeoh hyperelastic model (C10 = 0.273; C20 = −0.256; C30 = 0.185) | |||
| Midsole (40) | Third-order Yeoh hyperelastic model (C10 = 0.372; C20 = −0.327; C30 = 0.227) | |||
| Midsole (50) | Third-order Yeoh hyperelastic model (C10 = 0.655; C20 = −0.725; C30 = 0.634) | |||
| Outsole | 8 | 0.47 | 2300 | — |
| Ground Support | 17,000 | 0.1 | 5000 | — |
| Vertical Axis Joint Net Force (N) | Ankle Plantar Flexion Moment (Nm) | Achilles Tendon Arm (mm) | Achilles Tendon Force (N) |
|---|---|---|---|
| −1454 | 156 | 54.2 | 2878 |
| PF | Stress (MPa) | Strain (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Bundles (Shore A) | 10 | 20 | 30 | 40 | 50 | 10 | 20 | 30 | 40 | 50 |
| Firs bundle | 2.231 | 2.224 | 2.213 | 2.208 | 2.194 | 0.637 | 0.635 | 0.632 | 0.631 | 0.627 |
| Second bundle | 1.504 | 1.499 | 1.492 | 1.489 | 1.48 | 0.430 | 0.428 | 0.426 | 0.425 | 0.423 |
| Third bundle | 1.348 | 1.344 | 1.337 | 1.334 | 1.326 | 0.385 | 0.384 | 0.382 | 0.381 | 0.379 |
| Fourth bundle | 1.044 | 1.041 | 1.036 | 1.033 | 1.028 | 0.298 | 0.297 | 0.296 | 0.295 | 0.294 |
| Fifth bundle | 0.754 | 0.751 | 0.747 | 0.745 | 0.741 | 0.215 | 0.215 | 0.213 | 0.213 | 0.212 |
| Sum | 6.881 | 6.859 | 6.825 | 6.810 | 6.769 | 1.966 | 1.960 | 1.950 | 1.954 | 1.934 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhu, X.; Liu, J.; Liu, H.; Liu, J.; Yang, Y.; Wang, H. Effects of Midsole Hardness on the Mechanical Response Characteristics of the Plantar Fascia during Running. Bioengineering 2023, 10, 533. https://doi.org/10.3390/bioengineering10050533
Zhu X, Liu J, Liu H, Liu J, Yang Y, Wang H. Effects of Midsole Hardness on the Mechanical Response Characteristics of the Plantar Fascia during Running. Bioengineering. 2023; 10(5):533. https://doi.org/10.3390/bioengineering10050533
Chicago/Turabian StyleZhu, Xiaolan, Jiaojiao Liu, Hui Liu, Jingxi Liu, Yufeng Yang, and Haichun Wang. 2023. "Effects of Midsole Hardness on the Mechanical Response Characteristics of the Plantar Fascia during Running" Bioengineering 10, no. 5: 533. https://doi.org/10.3390/bioengineering10050533
APA StyleZhu, X., Liu, J., Liu, H., Liu, J., Yang, Y., & Wang, H. (2023). Effects of Midsole Hardness on the Mechanical Response Characteristics of the Plantar Fascia during Running. Bioengineering, 10(5), 533. https://doi.org/10.3390/bioengineering10050533






