Performance Evaluation of an Immersive Virtual Reality Application for Rehabilitation after Arthroscopic Rotator Cuff Repair
Abstract
:1. Introduction
2. Materials and Methods
2.1. Population and Equipment
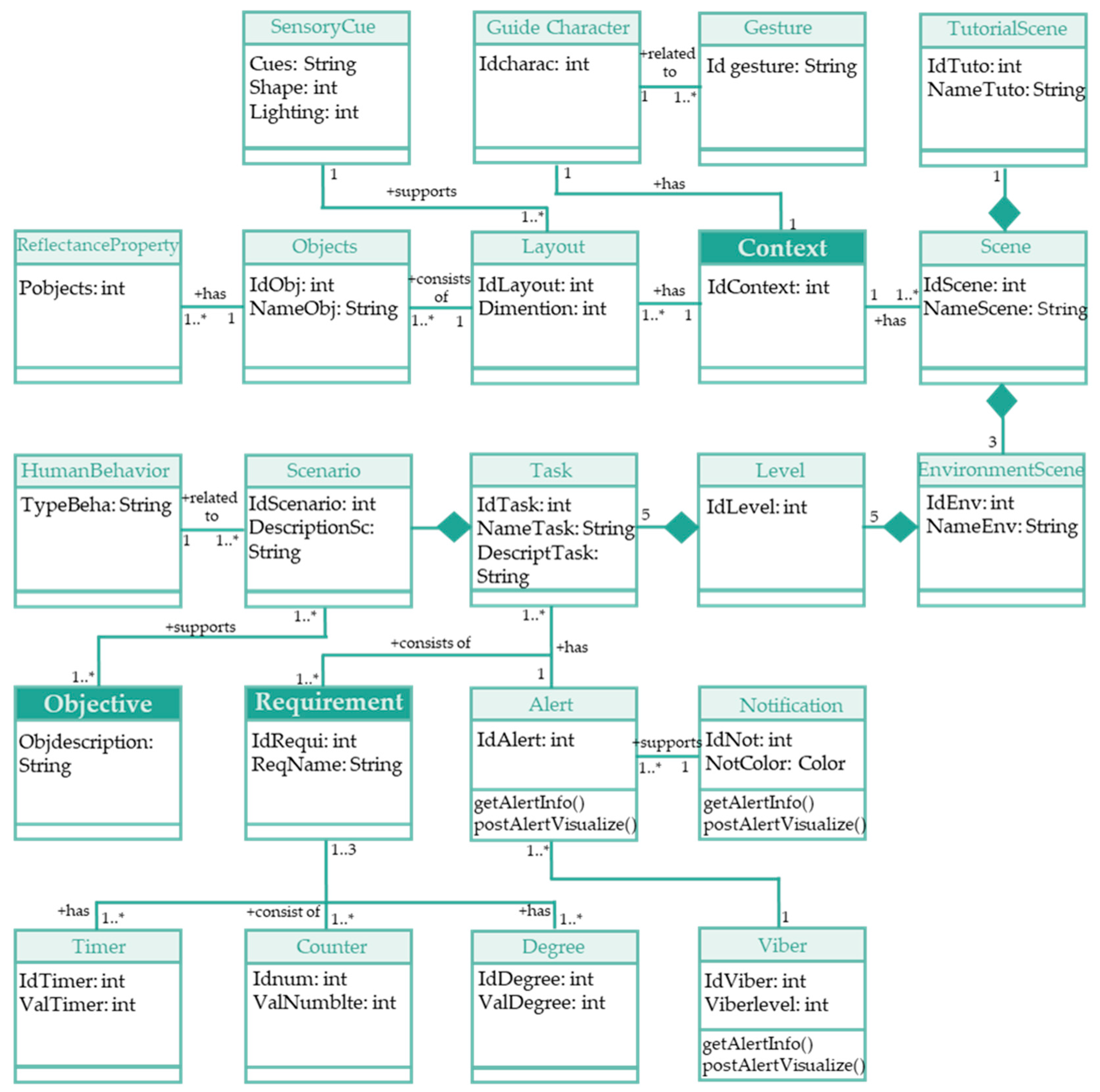
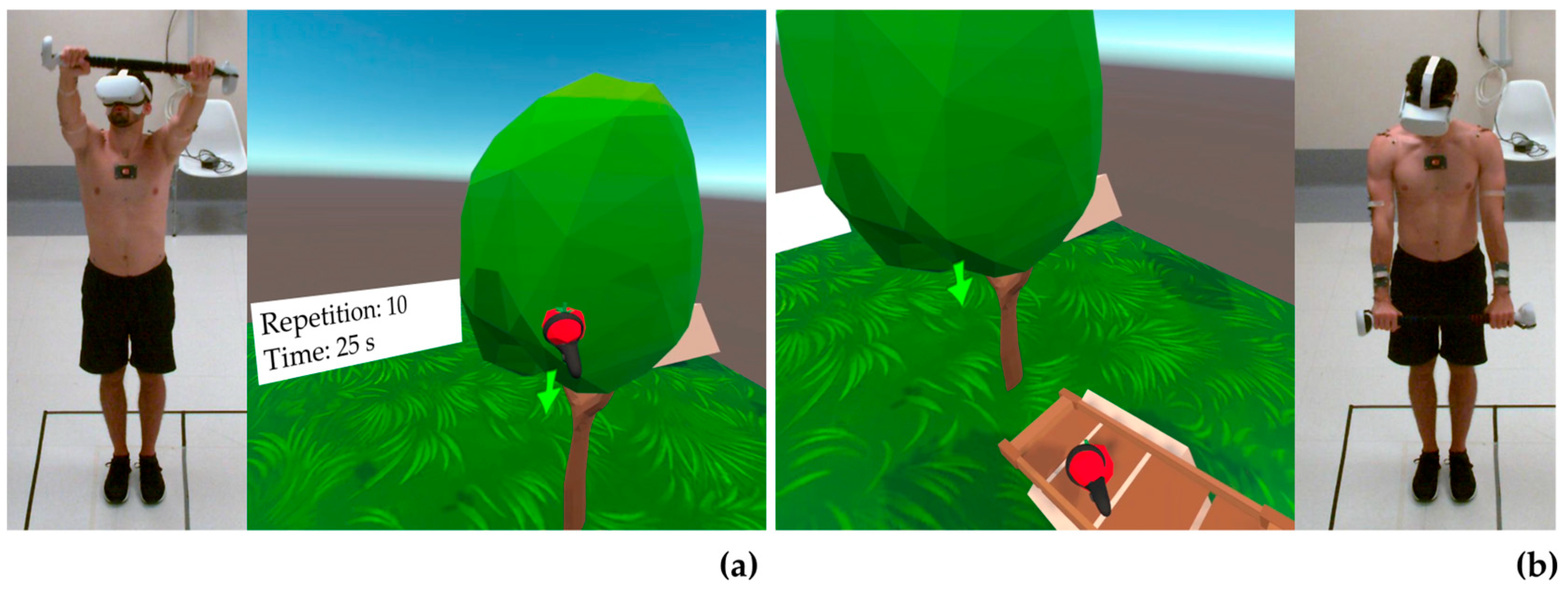
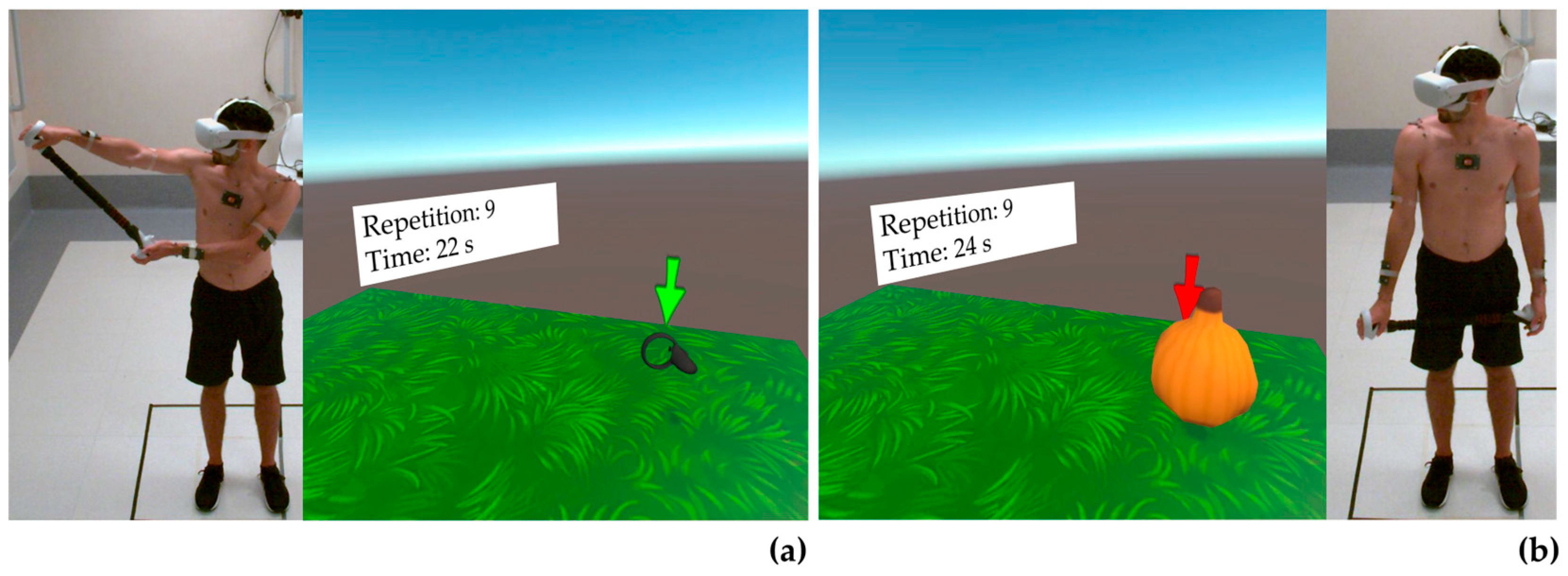
2.2. Game Design and Development
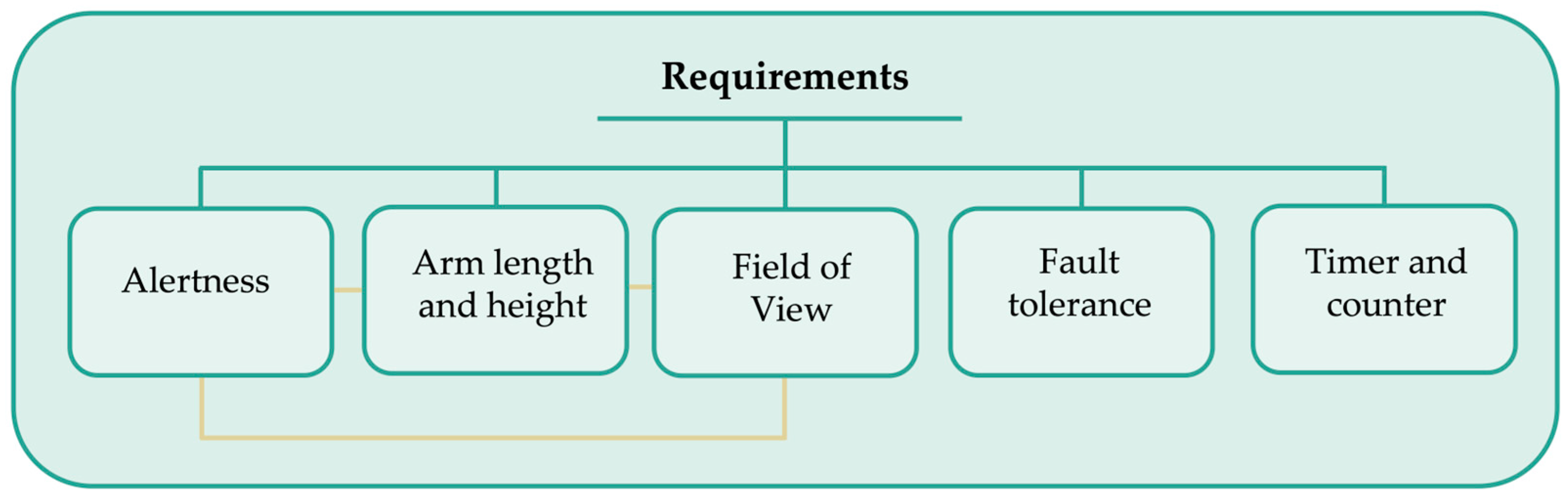
2.2.1. Specification of Requirements
2.2.2. Specification of Context
2.2.3. Specification of Objectives
2.3. Movements Protocol
2.4. Data Collection and Analysis
3. Results
3.1. Flexion
3.1.1. First Round of Flexion
3.1.2. Second Round of Flexion
3.2. Abduction
3.3. External Rotation
3.4. Internal Rotation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Berton, A.; Longo, U.G.; Candela, V.; Fioravanti, S.; Giannone, L.; Arcangeli, V.; Alciati, V.; Berton, C.; Facchinetti, G.; Marchetti, A.; et al. Virtual Reality, Augmented Reality, Gamification, and Telerehabilitation: Psychological Impact on Orthopedic Patients’ Rehabilitation. J. Clin. Med. 2020, 9, 2567. [Google Scholar] [CrossRef] [PubMed]
- Carnevale, A.; Mannocchi, I.; Sassi, M.S.H.; Carli, M.; De Luca, G.; Longo, U.G.; Denaro, V.; Schena, E. Virtual Reality for Shoulder Rehabilitation: Accuracy Evaluation of Oculus Quest 2. Sensors 2022, 22, 5511. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, I.; Safran, O.; Karniel, N.; Abel, M.; Berko, A.; Seyres, M.; Tsoar, T.; Portnoy, S. Positive Effect of Manipulated Virtual Kinematic Intervention in Individuals with Traumatic Stiff Shoulder: A Pilot Study. J. Clin. Med. 2022, 11, 3919. [Google Scholar] [CrossRef] [PubMed]
- Perez-Marcos, D. Virtual reality experiences, embodiment, videogames and their dimensions in neurorehabilitation. J. Neuroeng. Rehabil. 2018, 15, 113. [Google Scholar] [CrossRef]
- Chen, J.; Or, C.K.; Chen, T. Effectiveness of Using Virtual Reality-Supported Exercise Therapy for Upper Extremity Motor Rehabilitation in Patients With Stroke: Systematic Review and Meta-analysis of Randomized Controlled Trials. J. Med. Internet Res. 2022, 24, e24111. [Google Scholar] [CrossRef]
- Lv, Z.; Guo, J. Virtual reality neurorehabilitation. Int. J. Ment. Health Promot. 2022, 24, 287–310. [Google Scholar] [CrossRef]
- Gumaa, M.; Rehan Youssef, A. Is Virtual Reality Effective in Orthopedic Rehabilitation? A Systematic Review and Meta-Analysis. Phys. Ther. 2019, 99, 1304–1325. [Google Scholar] [CrossRef]
- Chi, B.; Chau, B.; Yeo, E.; Ta, P. Virtual reality for spinal cord injury-associated neuropathic pain: Systematic review. Ann. Phys. Rehabil. Med. 2019, 62, 49–57. [Google Scholar] [CrossRef]
- D’Antoni, F.; Russo, F.; Ambrosio, L.; Vollero, L.; Vadalà, G.; Merone, M.; Papalia, R.; Denaro, V. Artificial Intelligence and Computer Vision in Low Back Pain: A Systematic Review. Int. J. Environ. Res. Public. Health 2021, 18, 10909. [Google Scholar] [CrossRef]
- Hauschild, J.; Rivera, J.C.; Johnson, A.E.; Burns, T.C.; Roach, C.J. Shoulder Arthroscopy Simulator Training Improves Surgical Procedure Performance: A Controlled Laboratory Study. Orthop. J. Sports Med. 2021, 9, 23259671211003873. [Google Scholar] [CrossRef]
- Aïm, F.; Lonjon, G.; Hannouche, D.; Nizard, R. Effectiveness of Virtual Reality Training in Orthopaedic Surgery. Arthroscopy 2016, 32, 224–232. [Google Scholar] [CrossRef] [PubMed]
- Goh, G.S.; Lohre, R.; Parvizi, J.; Goel, D.P. Virtual and augmented reality for surgical training and simulation in knee arthroplasty. Arch. Orthop. Trauma. Surg. 2021, 141, 2303–2312. [Google Scholar] [CrossRef] [PubMed]
- Elaraby, A.E.R.; Shahien, M.; Jahan, A.M.; Etoom, M.; Bekhet, A.H. The Efficacy of Virtual Reality Training in the Rehabilitation of Orthopedic Ankle Injuries: A Systematic Review and Meta-analysis. Adv. Rehabil. Sci. Pract. 2023, 12, 11795727231151636. [Google Scholar] [CrossRef] [PubMed]
- Lohre, R.; Warner, J.J.P.; Athwal, G.S.; Goel, D.P. The evolution of virtual reality in shoulder and elbow surgery. JSES Int. 2020, 4, 215–223. [Google Scholar] [CrossRef]
- Park, M.; Cho, Y.; Na, G.; Kim, J. Application of Virtual Avatar using Motion Capture in Immersive Virtual Environment. Int. J. Hum.-Comput. Interact. 2023, 1–15. [Google Scholar] [CrossRef]
- Hao, J.; He, Z.; Yu, X.; Remis, A. Comparison of immersive and non-immersive virtual reality for upper extremity functional recovery in patients with stroke: A systematic review and network meta-analysis. Neurol. Sci. 2023, 44, 2679–2697. [Google Scholar] [CrossRef]
- Salatino, A.; Zavattaro, C.; Gammeri, R.; Cirillo, E.; Piatti, M.L.; Pyasik, M.; Serra, H.; Pia, L.; Geminiani, G.; Ricci, R. Virtual reality rehabilitation for unilateral spatial neglect: A systematic review of immersive, semi-immersive and non-immersive techniques. Neurosci. Biobehav. Rev. 2023, 152, 105248. [Google Scholar] [CrossRef]
- Liu, P.R.; Lu, L.; Zhang, J.Y.; Huo, T.T.; Liu, S.X.; Ye, Z.W. Application of Artificial Intelligence in Medicine: An Overview. Curr. Med. Sci. 2021, 41, 1105–1115. [Google Scholar] [CrossRef]
- Beyaz, S. A brief history of artificial intelligence and robotic surgery in orthopedics & traumatology and future expectations. Jt. Dis. Relat. Surg. 2020, 31, 653–655. [Google Scholar] [CrossRef]
- Economopoulos, K.J.; Brockmeier, S.F. Rotator cuff tears in overhead athletes. Clin. Sports Med. 2012, 31, 675–692. [Google Scholar] [CrossRef]
- Plancher, K.D.; Shanmugam, J.; Briggs, K.; Petterson, S.C. Diagnosis and Management of Partial Thickness Rotator Cuff Tears: A Comprehensive Review. J. Am. Acad. Orthop. Surg. 2021, 29, 1031–1043. [Google Scholar] [CrossRef] [PubMed]
- Lazarides, A.L.; Alentorn-Geli, E.; Choi, J.H.; Stuart, J.J.; Lo, I.K.; Garrigues, G.E.; Taylor, D.C. Rotator cuff tears in young patients: A different disease than rotator cuff tears in elderly patients. J. Shoulder Elb. Surg. 2015, 24, 1834–1843. [Google Scholar] [CrossRef] [PubMed]
- Longo, U.G.; Risi Ambrogioni, L.; Candela, V.; Berton, A.; Carnevale, A.; Schena, E.; Denaro, V. Conservative versus surgical management for patients with rotator cuff tears: A systematic review and META-analysis. BMC Musculoskelet. Disord. 2021, 22, 50. [Google Scholar] [CrossRef]
- Maffulli, N.; Longo, U.G.; Berton, A.; Loppini, M.; Denaro, V. Biological factors in the pathogenesis of rotator cuff tears. Sports Med. Arthrosc. Rev. 2011, 19, 194–201. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.H.; Do, H.K.; Lee, J.H.; Kim, B.R.; Noh, J.H.; Choi, S.H.; Chung, S.G.; Lee, S.U.; Choi, J.E.; Kim, S.; et al. Clinical Outcomes of Conservative Treatment and Arthroscopic Repair of Rotator Cuff Tears: A Retrospective Observational Study. Ann. Rehabil. Med. 2016, 40, 252–262. [Google Scholar] [CrossRef] [PubMed]
- Osborne, J.D.; Gowda, A.L.; Wiater, B.; Wiater, J.M. Rotator cuff rehabilitation: Current theories and practice. Phys. Sport. 2016, 44, 85–92. [Google Scholar] [CrossRef]
- Pekyavas, N.O.; Ergun, N. Comparison of virtual reality exergaming and home exercise programs in patients with subacromial impingement syndrome and scapular dyskinesis: Short term effect. Acta Orthop. Traumatol. Turc. 2017, 51, 238–242. [Google Scholar] [CrossRef]
- Chang, W.K.; Lee, J.I.; Hwang, J.H.; Lim, J.Y. Post-operative rehabilitation using a digital healthcare system in patients who had undergone rotator cuff repair: Protocol for a single-center randomized controlled trial. Trials 2022, 23, 667. [Google Scholar] [CrossRef]
- Menek, B.; Tarakci, D.; Tarakci, E.; Menek, M.Y. Investigation on the Efficiency of the Closed Kinetic Chain and Video-Based Game Exercise Programs in the Rotator Cuff Rupture: A Randomized Trial. Games Health J. 2022, 11, 298–306. [Google Scholar] [CrossRef]
- Wochatz, M.; Rabe, S.; Engel, T.; Mueller, S.; Mayer, F. Scapular kinematics during unloaded and maximal loaded isokinetic concentric and eccentric shoulder flexion and extension movements. J. Electromyogr. Kinesiol. 2021, 57, 102517. [Google Scholar] [CrossRef]
- Menek, B.; Tarakci, D.; Algun, Z.C. The effect of Mulligan mobilization on pain and life quality of patients with Rotator cuff syndrome: A randomized controlled trial. J. Back. Musculoskelet. Rehabil. 2019, 32, 171–178. [Google Scholar] [CrossRef] [PubMed]
- Baldominos, A.; Saez, Y.; Pozo, C.G.d. An Approach to Physical Rehabilitation Using State-of-the-art Virtual Reality and Motion Tracking Technologies. Procedia Comput. Sci. 2015, 64, 10–16. [Google Scholar] [CrossRef]
- Thigpen, C.A.; Shaffer, M.A.; Gaunt, B.W.; Leggin, B.G.; Williams, G.R.; Wilcox, R.B., 3rd. The American Society of Shoulder and Elbow Therapists’ consensus statement on rehabilitation following arthroscopic rotator cuff repair. J. Shoulder Elb. Surg. 2016, 25, 521–535. [Google Scholar] [CrossRef] [PubMed]
- Wu, G.; van der Helm, F.C.; Veeger, H.E.; Makhsous, M.; Van Roy, P.; Anglin, C.; Nagels, J.; Karduna, A.R.; McQuade, K.; Wang, X.; et al. ISB recommendation on definitions of joint coordinate systems of various joints for the reporting of human joint motion--Part II: Shoulder, elbow, wrist and hand. J. Biomech. 2005, 38, 981–992. [Google Scholar] [CrossRef] [PubMed]
- Meskers, C.G.M.; Van der Helm, F.C.T.; Rozendaal, L.A.; Rozing, P.M. In vivo estimation of the glenohumeral joint rotation center from scapular bony landmarks by linear regression. J. Biomech. 1997, 31, 93–96. [Google Scholar] [CrossRef]
- Boser, Q.A.; Valevicius, A.M.; Lavoie, E.B.; Chapman, C.S.; Pilarski, P.M.; Hebert, J.S.; Vette, A.H. Cluster-based upper body marker models for three-dimensional kinematic analysis: Comparison with an anatomical model and reliability analysis. J. Biomech. 2018, 72, 228–234. [Google Scholar] [CrossRef]
- Kontaxis, A.; Cutti, A.G.; Johnson, G.R.; Veeger, H.E. A framework for the definition of standardized protocols for measuring upper-extremity kinematics. Clin. Biomech. 2009, 24, 246–253. [Google Scholar] [CrossRef]
- Cutti, A.G.; Parel, I.; Raggi, M.; Petracci, E.; Pellegrini, A.; Accardo, A.P.; Sacchetti, R.; Porcellini, G. Prediction bands and intervals for the scapulo-humeral coordination based on the Bootstrap and two Gaussian methods. J. Biomech. 2014, 47, 1035–1044. [Google Scholar] [CrossRef]
- Cunha, B.; Ferreira, R.; Sousa, A.S.P. Home-Based Rehabilitation of the Shoulder Using Auxiliary Systems and Artificial Intelligence: An Overview. Sensors 2023, 23, 7100. [Google Scholar] [CrossRef]
- Chen, K.; Chen, K.B. Task-Oriented and Imitation-Oriented Movements in Virtual Reality Exercise Performance and Design. Hum. Factors 2023, 65, 125–136. [Google Scholar] [CrossRef]


| Level | Flexion 1 | Flexion 2 | Abduction | External Rotation | Internal Rotation | |
|---|---|---|---|---|---|---|
| L1 | Repetitions | 10 | 10 | 10 | 8 | - |
| ROM | 60°–90° | 60°–90° | ≤45° | ≤20° | – | |
| L2 | Repetitions | 10 | 10 | 10 | 8 | 8 |
| ROM | 90°–120° | 90°–120° | 45°–80° | 20°–30° | ≤20° | |
| L3 | Repetitions | 10 | 10 | 10 | 10 | 10 |
| ROM | 130°–155° | 130°–155° | 80°–120° | 30°–45° | 20°–50° | |
| L4 | Repetitions | 12 | 12 | 12 | 12 | 12 |
| ROM | ≥140° | ≥140° | ≥120° | ≥45° | ≥50° | |
| Level | Volunteer | MAEinf | Ninf | MAETOT,inf | MAEsup | Nsup | MAETOT,sup |
|---|---|---|---|---|---|---|---|
| L1 | V1 | 1.0 | 8 | 6.4 | ✔ | 5 | 2.9 |
| V2 | 3.3 | ✔ | |||||
| V3 | 2.7 | 3.4 | |||||
| V4 | ✔ | 2.6 | |||||
| V5 | 10.2 | ✔ | |||||
| L2 | V1 | 2.3 | 15 | 5.1 | ✔ | 0 | ✔ |
| V2 | 5.5 | ✔ | |||||
| V3 | 2.6 | ✔ | |||||
| V4 | 2.8 | ✔ | |||||
| V5 | 7.9 | ✔ | |||||
| L3 | V1 | ✔ | 4 | 1.3 | ✔ | 3 | 8.6 |
| V2 | ✔ | ✔ | |||||
| V3 | 0.9 | ✔ | |||||
| V4 | 1.7 | ✔ | |||||
| V5 | ✔ | 8.6 | |||||
| L4 | V1 | ✔ | 1 | 0.8 | - | - | - |
| V2 | ✔ | - | |||||
| V3 | 0.8 | - | |||||
| V4 | ✔ | - | |||||
| V5 | ✔ | - |
| Level | Volunteer | MAEinf | Ninf | MAETOT,inf | MAEsup | Nsup | MAETOT,sup |
|---|---|---|---|---|---|---|---|
| L1 | V1 | 6.8 | 6 | 4.6 | ✔ | 6 | 10.5 |
| V2 | 2.8 | ✔ | |||||
| V3 | ✔ | ✔ | |||||
| V4 | ✔ | 10.5 | |||||
| V5 | 2.3 | ✔ | |||||
| L2 | V1 | 8.0 | 8 | 12.3 | ✔ | 7 | |
| V2 | 15.4 | ✔ | |||||
| V3 | ✔ | ✔ | 9.2 | ||||
| V4 | ✔ | 9.2 | |||||
| V5 | 13 | ✔ | |||||
| L3 | V1 | ✔ | 2 | 4.8 | ✔ | 2 | 2.1 |
| V2 | 7.9 | ✔ | |||||
| V3 | ✔ | ✔ | |||||
| V4 | 1.7 | ✔ | |||||
| V5 | ✔ | 2.1 | |||||
| L4 | V1 | ✔ | 8 | 2.6 | - | - | - |
| V2 | 2.6 | - | |||||
| V3 | ✔ | - | |||||
| V4 | ✔ | - | |||||
| V5 | ✔ | - |
| Level | Volunteer | MAEinf | Ninf | MAETOT,inf | MAEsup | Nsup | MAETOT,sup |
|---|---|---|---|---|---|---|---|
| L1 | V1 | - | - | - | 5.9 | 14 | 6.1 |
| V2 | - | 7.8 | |||||
| V3 | - | ✔ | |||||
| V4 | - | ✔ | |||||
| V5 | - | 1.2 | |||||
| L2 | V1 | ✔ | 0 | ✔ | ✔ | 4 | |
| V2 | ✔ | 4.7 | |||||
| V3 | ✔ | ✔ | 4.7 | ||||
| V4 | ✔ | ✔ | |||||
| V5 | ✔ | ✔ | |||||
| L3 | V1 | 4.0 | 15 | 8.6 | ✔ | 0 | ✔ |
| V2 | ✔ | ✔ | |||||
| V3 | 11.4 | ✔ | |||||
| V4 | 8.2 | ✔ | |||||
| V5 | 8.0 | ✔ | |||||
| L4 | V1 | 6.6 | 22 | 6.6 | - | - | - |
| V2 | 5.8 | - | |||||
| V3 | 5.9 | - | |||||
| V4 | 10.8 | - | |||||
| V5 | 7.0 | - |
| Level | Volunteer | MAEinf | Ninf | MAETOT,inf | MAEsup | Nsup | MAETOT,sup |
|---|---|---|---|---|---|---|---|
| L1 | V1 | - | - | - | 11.5 | 32 | 6.5 |
| V2 | - | 3.4 | |||||
| V3 | - | 1.9 | |||||
| V4 | - | 5.7 | |||||
| V5 | - | 7.9 | |||||
| L2 | V1 | ✔ | 1 | 2.3 | 2.9 | 12 | |
| V2 | ✔ | 1.7 | |||||
| V3 | ✔ | ✔ | 2.6 | ||||
| V4 | 2.3 | ✔ | |||||
| V5 | ✔ | 2.6 | |||||
| L3 | V1 | ✔ | 16 | 6.3 | 2.6 | 5 | 2.6 |
| V2 | ✔ | ✔ | |||||
| V3 | 1.3 | ✔ | |||||
| V4 | 10.3 | ✔ | |||||
| V5 | 0.1 | ✔ | |||||
| L4 | V1 | 1.1 | 26 | 19.6 | - | - | - |
| V2 | ✔ | - | |||||
| V3 | 15.8 | - | |||||
| V4 | 26.6 | - | |||||
| V5 | ✔ | - |
| Level | Volunteer | MAEinf | Ninf | MAETOT,inf | MAEsup | Nsup | MAETOT,sup |
|---|---|---|---|---|---|---|---|
| L2 | V1 | - | - | - | 17.3 | 33 | 9.8 |
| V2 | - | 2.8 | |||||
| V3 | - | 8.0 | |||||
| V4 | - | 0.2 | |||||
| V5 | - | 12.4 | |||||
| L3 | V1 | ✔ | 6 | 2.0 | ✔ | 0 | ✔ |
| V2 | 1.9 | ✔ | |||||
| V3 | ✔ | ✔ | |||||
| V4 | 2.2 | ✔ | |||||
| V5 | ✔ | ✔ | |||||
| L4 | V1 | ✔ | 30 | 8.0 | - | - | - |
| V2 | 4.3 | - | |||||
| V3 | 7.6 | - | |||||
| V4 | 10.7 | - | |||||
| V5 | 3.1 | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carnevale, A.; Mannocchi, I.; Schena, E.; Carli, M.; Sassi, M.S.H.; Marino, M.; Longo, U.G. Performance Evaluation of an Immersive Virtual Reality Application for Rehabilitation after Arthroscopic Rotator Cuff Repair. Bioengineering 2023, 10, 1305. https://doi.org/10.3390/bioengineering10111305
Carnevale A, Mannocchi I, Schena E, Carli M, Sassi MSH, Marino M, Longo UG. Performance Evaluation of an Immersive Virtual Reality Application for Rehabilitation after Arthroscopic Rotator Cuff Repair. Bioengineering. 2023; 10(11):1305. https://doi.org/10.3390/bioengineering10111305
Chicago/Turabian StyleCarnevale, Arianna, Ilaria Mannocchi, Emiliano Schena, Marco Carli, Mohamed Saifeddine Hadj Sassi, Martina Marino, and Umile Giuseppe Longo. 2023. "Performance Evaluation of an Immersive Virtual Reality Application for Rehabilitation after Arthroscopic Rotator Cuff Repair" Bioengineering 10, no. 11: 1305. https://doi.org/10.3390/bioengineering10111305
APA StyleCarnevale, A., Mannocchi, I., Schena, E., Carli, M., Sassi, M. S. H., Marino, M., & Longo, U. G. (2023). Performance Evaluation of an Immersive Virtual Reality Application for Rehabilitation after Arthroscopic Rotator Cuff Repair. Bioengineering, 10(11), 1305. https://doi.org/10.3390/bioengineering10111305








