Biomechanical Behavior of Dynamic vs. Static Distal Locking Intramedullary Nails in Subtrochanteric Femur Fractures
Abstract
:1. Introduction
2. Materials and Methods
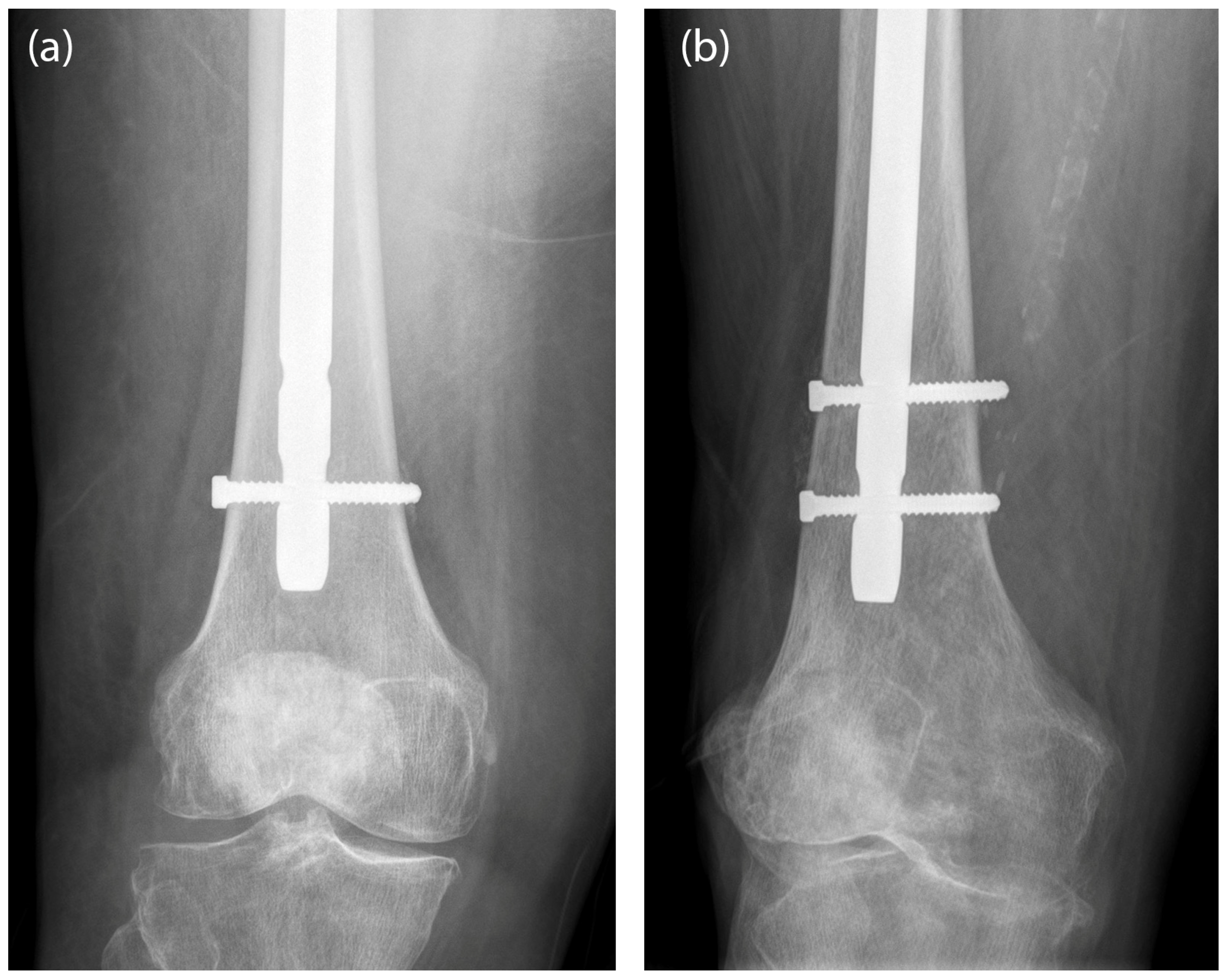
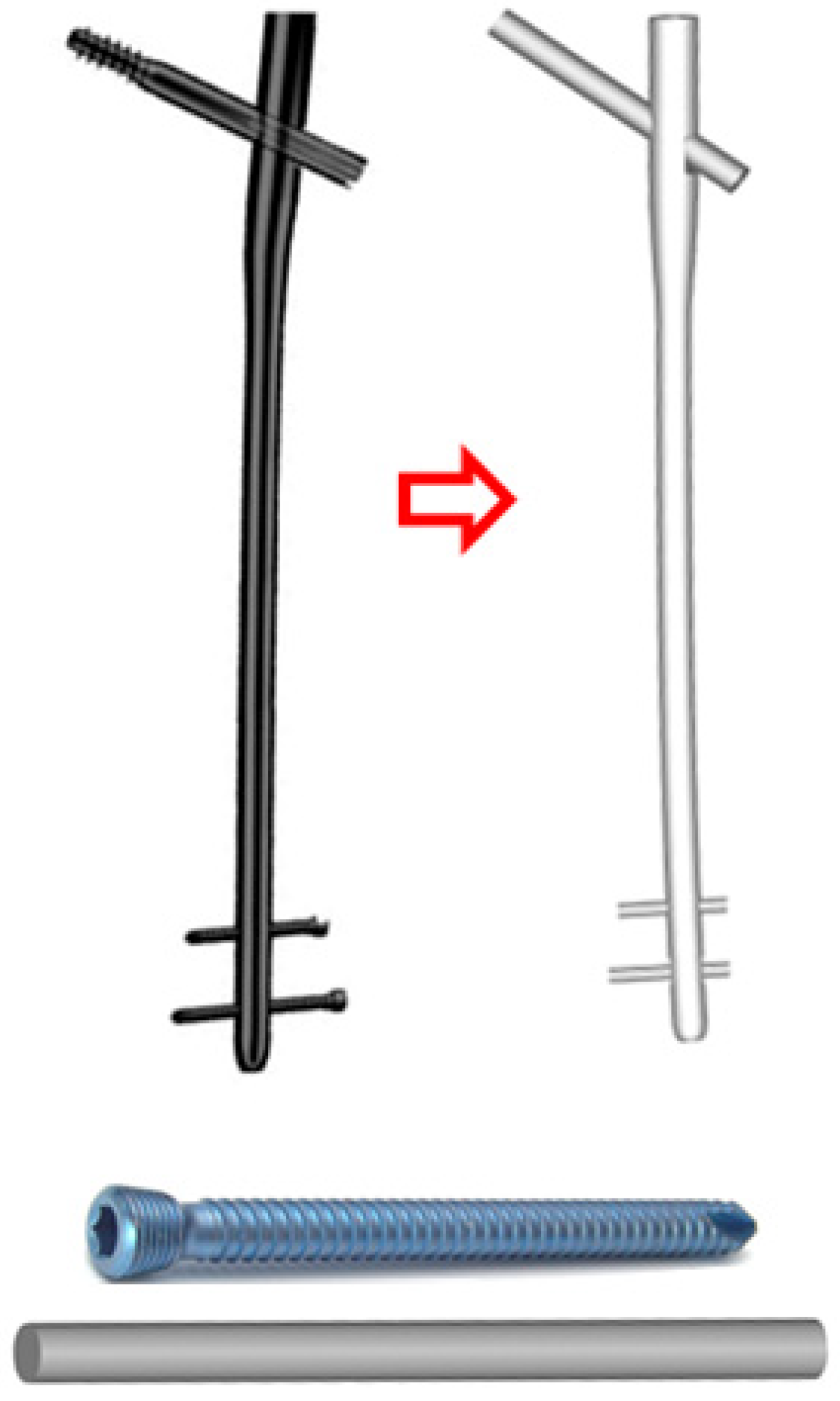
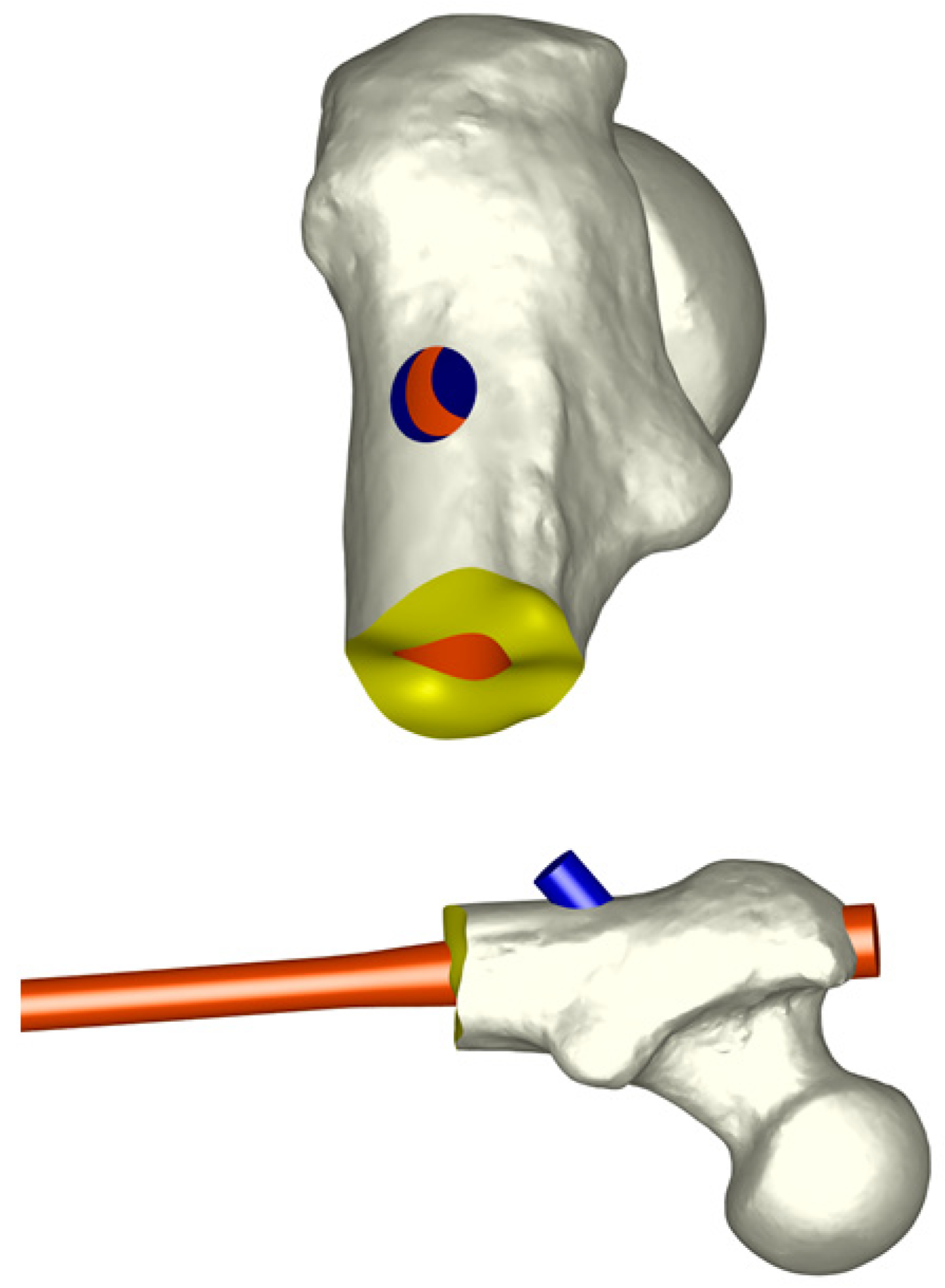
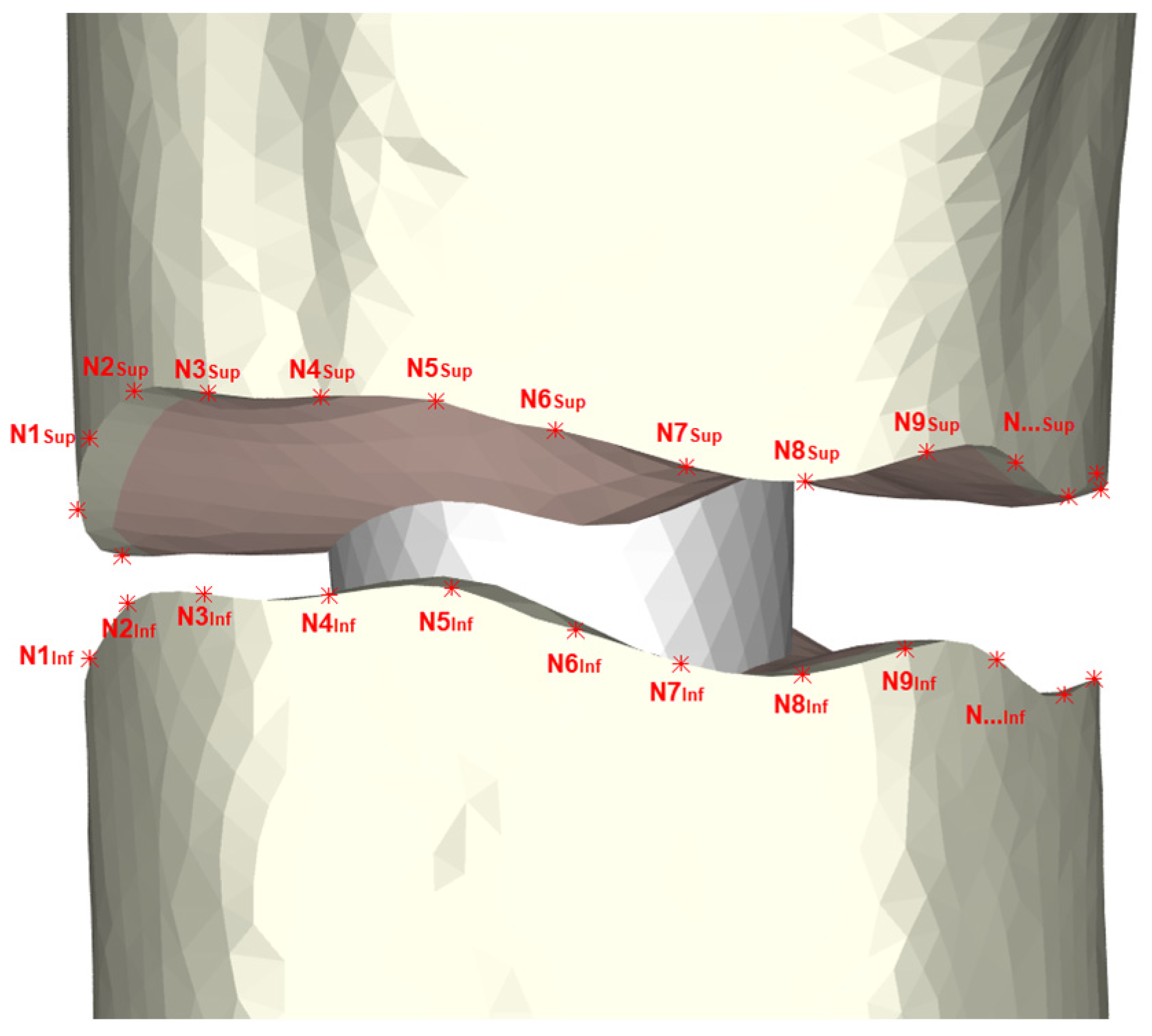
2.1. Model of the Femur and Implants
2.2. Material Properties
2.3. Contact Modeling
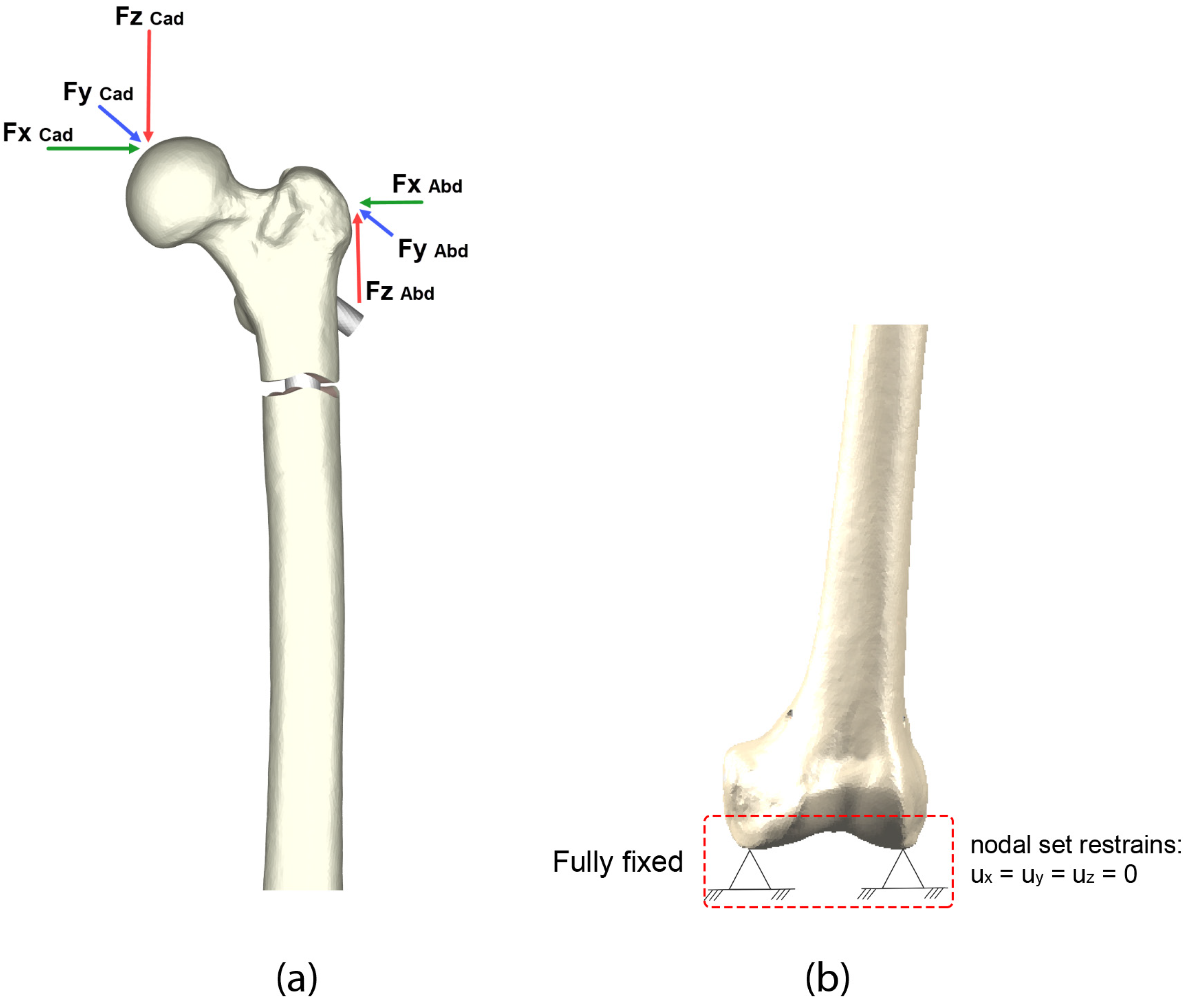
2.4. Loads and Boundary Conditions
3. Results
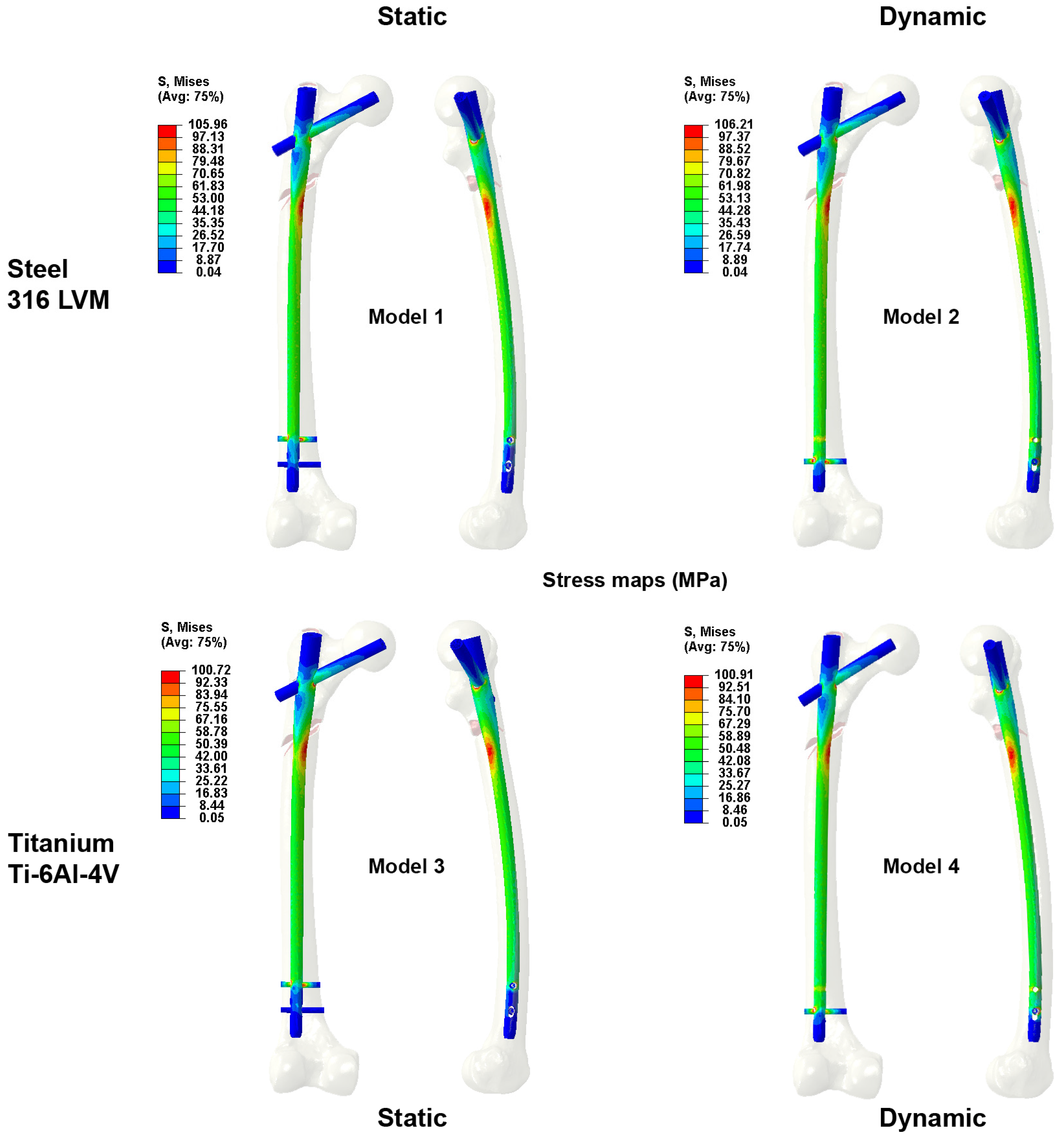
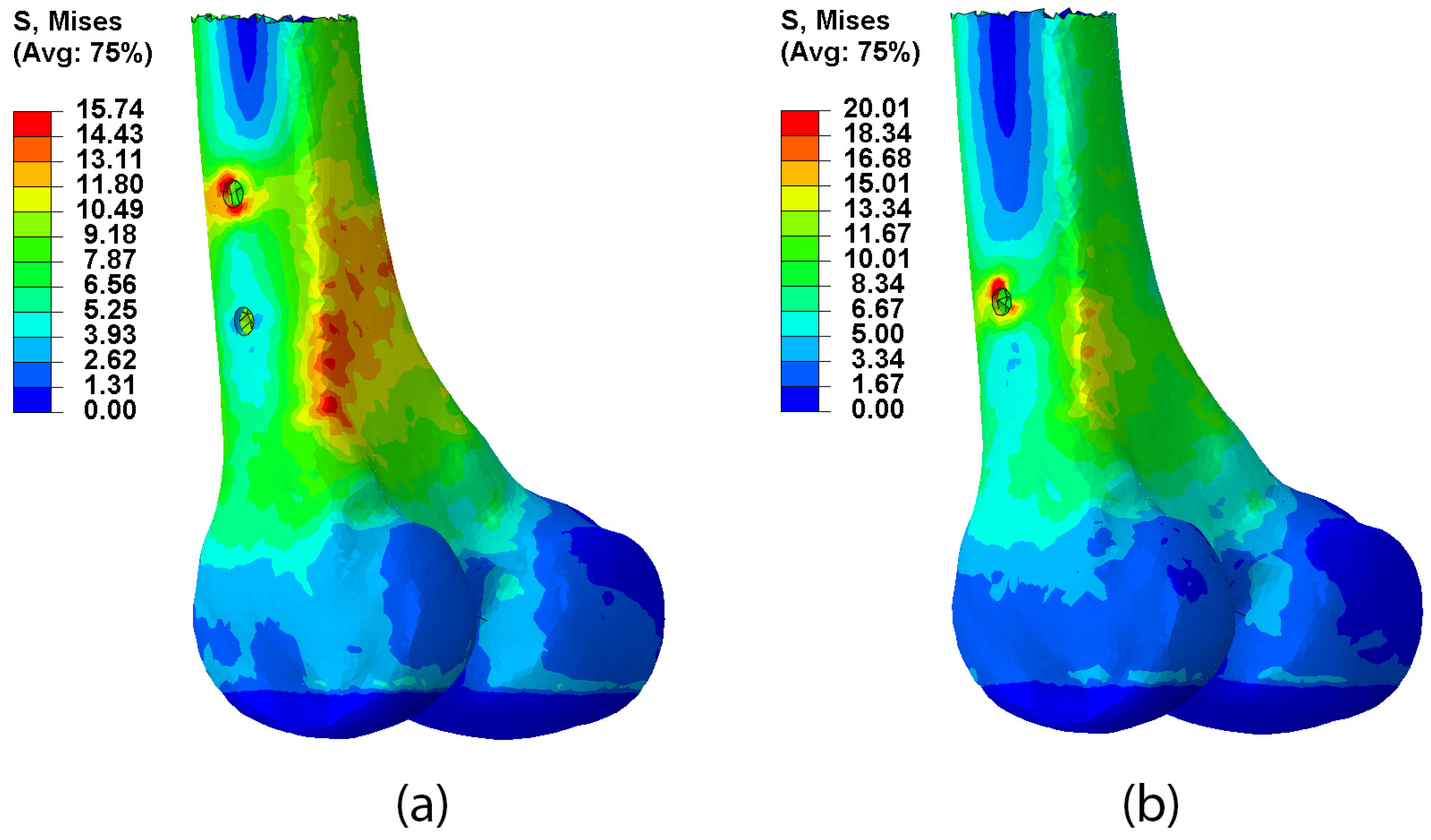
3.1. Type of Locking
3.2. Type of Material
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Brauer, C.A.; Coca-Perraillon, M.; Cutler, D.M.; Rosen, A.B. Incidence and Mortality of Hip Fractures in the United States. JAMA 2009, 302, 1573. [Google Scholar] [CrossRef] [PubMed]
- Svedbom, A.; Hernlund, E.; Ivergård, M.; Compston, J.; Cooper, C.; Stenmark, J.; McCloskey, E.V.; Jönsson, B.; Kanis, J.A.; EU Review Panel of the IOF. Osteoporosis in the European Union: A compendium of country-specific reports. Arch. Osteoporos. 2013, 8, 137. [Google Scholar] [CrossRef] [PubMed]
- Paaschburg Nielsen, B.; Jelnes, R.; Rasmussen, L.B.; Ebling, A. Trochanteric fractures treated by the McLaughlin nail and plate. Injury 1985, 16, 333–336. [Google Scholar] [CrossRef] [PubMed]
- Zickel, R.E. An intramedullary fixation device for the proximal part of the femur. J. Bone Jt. Surg. 1976, 58, 866–872. [Google Scholar] [CrossRef]
- Xie, H.; Xie, L.; Wang, J.; Chen, C.; Zhang, C.; Zheng, W. Intramedullary versus extramedullary fixation for treatment of subtrochanteric fracture: A systematic review and meta-analysis. Int. J. Surg. 2019, 63, 43–57. [Google Scholar] [CrossRef] [PubMed]
- Collinge, C.A.; Hymes, R.; Archdeacon, M.; Streubel, P.; Obremskey, W.; Weber, T.; Watson, J.T.; Lowenberg, D. Members of the Proximal Femur Working Group of the Southeast Trauma Consortium. Unstable proximal femur fractures treated with proximal femoral locking plates: A retrospective, multicenter study of 111 cases. J. Orthop. Trauma 2016, 30, 489–495. [Google Scholar] [CrossRef] [PubMed]
- Panteli, M.; Mauffrey, C.; Giannoudis, P.V. Subtrochanteric fractures: Issues and challenges. Injury 2017, 48, 2023–2026. [Google Scholar] [CrossRef] [PubMed]
- Kumar, M.; Akshat, V.; Kanwariya, A.; Gandhi, M. A Prospective Study to Evaluate the Management of Sub-trochanteric Femur Fractures with Long Proximal Femoral Nail. Malays. Orthop. J. 2017, 11, 36–41. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Z.B.; Chen, S.; Gao, Y.S.; Sun, Y.Q.; Zhang, C.Q.; Jiang, Y. Subtrochanteric femur fracture treated by intramedullary fixation. Chin. J. Traumatol. 2015, 18, 336–341. [Google Scholar] [CrossRef]
- Herrera, A.; Ibarz, E.; Cegoñino, J.; Lobo-Escolar, A.; Puértolas, S.; López, E.; Mateo, J.; Gracia, L. Applications of finite element simulation in orthopedic and trauma surgery. World J. Orthop. 2012, 3, 25–41. [Google Scholar] [CrossRef]
- Herrera, A.; Panisello, J.J.; Ibarz, E.; Cegoñino, J.; Puértolas, J.A.; Gracia, L. Long-term study of bone remodelling after femoral stem: A comparison between dexa and finite element simulation. J. Biomech. 2007, 40, 3615–3625. [Google Scholar] [CrossRef]
- Larrainzar-Garijo, R.; Caeiro, J.R.; Marco, M.; Giner, E.; Miguélez, M.H. Validación experimental de un modelo de análisis de elementos finitos en fractura de cadera y su aplicabilidad clínica. Rev. Esp. Cir. Ortopédica Traumatol. 2019, 63, 146–154. [Google Scholar] [CrossRef]
- Cristofolini, L.; Juszczyk, M.; Martelli, S.; Taddei, F.; Viceconti, M. In vitro replication of spontaneous fractures of the proximal human femur. J. Biomech. 2007, 40, 2837–2845. [Google Scholar] [CrossRef]
- Chen, S.H.; Yu, T.C.; Chang, C.H.; Lu, Y.C. Biomechanical analysis of retrograde intramedullary nail fixation in distal femoral fractures. Knee 2008, 15, 384–389. [Google Scholar] [CrossRef] [PubMed]
- Herrera, A.; Rosell, J.; Ibarz, E.; Albareda, J.; Gabarre, S.; Mateo, J.; Gracia, L. Biomechanical analysis of the stability of anterograde reamed intramedullary nails in femoral spiral fractures. Injury 2020, 51, 74–79. [Google Scholar] [CrossRef] [PubMed]
- Gabarre, S.; Albareda, J.; Gracia, L.; Puértolas, S.; Ibarz, E.; Herrera, A. Influence of gap size, screw configuration, and nail materials in the stability of anterograde reamed intramedullary nail in femoral transverse fractures. Injury 2017, 48 (Suppl. 6), 40–46. [Google Scholar] [CrossRef] [PubMed]
- Gabarre, S.; Albareda, J.; Gracia, L.; Puértolas, S.; Ibarz, E.; Herrera, A. Influence of screw combination and nail materials in the stability of anterograde reamed intramedullary nail in distal femoral fractures. Injury 2017, 48 (Suppl. 6), 47–53. [Google Scholar] [CrossRef]
- Kwak, D.K.; Bang, S.H.; Kim, W.H.; Lee, S.J.; Lee, S.; Yoo, J.H. Biomechanics of subtrochanteric fracture fixation using short cephalomedullary nails: A finite element analysis. PLoS ONE 2021, 16, e0253862. [Google Scholar] [CrossRef]
- Jang, C.Y.; Bang, S.H.; Kim, W.H.; Lee, S.J.; Lee, H.M.; Kwak, D.K.; Yoo, J.H. Effect of fracture levels on the strength of bone-implant constructs in subtrochanteric fracture models fixed using short cephalomedullary nails: A finite element analysis. Injury 2019, 50, 1883–1888. [Google Scholar] [CrossRef]
- Lee, W.C.; Chou, S.M.; Tan, C.W.; Chng, L.S.; Yam, G.J.M.; Chua, T.H.I. Intertrochanteric fracture with distal extension: When is the short proximal femoral nail antirotation too short? Injury 2021, 52, 926–932. [Google Scholar] [CrossRef]
- Chantarapanich, N.; Riansuwan, K. Biomechanical performance of short and long cephalomedullary nail constructs for stabilizing different levels of subtrochanteric fracture. Injury 2022, 53, 323–333. [Google Scholar] [CrossRef] [PubMed]
- Tsai, A.G.; Reich, M.S.; Bensusan, J.; Ashworth, T.; Marcus, R.E.; Akkus, O. A fatigue loading model for investigation of iatrogenic subtrochanteric fractures of the femur. Clin. Biomech. Bristol. Avon. 2013, 28, 981–987. [Google Scholar] [CrossRef] [PubMed]
- Lundy, D.W. Subtrochanteric femoral fractures. J. Am. Acad. Orthop. Surg 2007, 15, 663–671. [Google Scholar] [CrossRef] [PubMed]
- Omerovic, D.; Lazovic, F.; Hadzimehmedagic, A. Static or dynamic intramedullary nailing of femur and tibia. Med. Arch. 2015, 69, 110–113. [Google Scholar] [CrossRef]
- Hulshof, G.W.L.; van der Stelt, M.; Schutte, H.; van Koperen, P.J.; Timmers, T.K.; van Olden, G.D.J.; Kluijfhout, W.P. Locking in trochanteric fractures: A comparison of static versus dynamic locking using the Gamma3 nail. Eur. J. Orthop. Surg. Traumatol. 2023, 33, 1797–1804. [Google Scholar] [CrossRef]
- Kuzyk, P.R.; Shah, S.; Zdero, R.; Olsen, M.; Waddell, J.P.; Schemitsch, E.H. A biomechanical comparison of static versus dynamic lag screw modes for cephalomedullary nails used to fix unstable peritrochanteric fractures. J. Trauma Acute Care Surg. 2012, 72, 65–70. [Google Scholar] [CrossRef]
- Ciaffa, V.; Vicenti, G.; Mori, C.M.; Panella, A.; Conserva, V.; Corina, G.; Scialpi, L.; Speciale, M.; Fraccascia, A.; Picca, G.; et al. Unlocked versus dynamic and static distal locked femoral nails in stable and unstable intertrochanteric fractures. A prospective study. Injury 2018, 49 (Suppl. 3), 19–25. [Google Scholar] [CrossRef]
- Fang, C.; Shen, W.Y.; Wong, J.S.H.; Yee, D.K.; Yung, C.S.; Fang, E.; Lai, Y.S.; Woo, S.B.; Cheung, J.; Chau, J.Y.; et al. Should nails be locked dynamically or statically in atypical femoral fractures? A radiological analysis of time to union and reoperations in 236 displaced fractures with 4 years average follow-up. Injury 2023, 54, 110909. [Google Scholar] [CrossRef]
- Siemens, I-Deas®11 NXSeries PLM Software. 2023. Available online: https://www.plm.automation.siemens.com/global/es/ (accessed on 12 September 2023 ).
- Dassault Systemes, Simulia Products, Abaqus Unified FEA. 2023. Available online: https://www.3ds.com/es/ (accessed on 12 September 2023).
- Weinans, H.; Huiskes, R.; Grootenboer, H.J. Effects of fit and bonding characteristics of femoral stems on adaptive bone remodeling. J Biomech Eng. 1994, 116, 393–400. [Google Scholar] [CrossRef]
- OrthoLoad [Internet]. Available online: https://orthoload.com/ (accessed on 29 September 2023).
- Henschel, J.; Eberle, S.; Augat, P. Load distribution between cephalic screws in a dual lag screw trochanteric nail. J. Orthop. Surg. 2016, 11, 41. [Google Scholar] [CrossRef]
- Loh, A.J.; Onggo, J.R.; Hockings, J.; Damasena, I. Comparison of dynamic versus static fixation of intramedullary nailing in tibial diaphyseal fractures: A systematic review and meta-analysis. J. Clin. Orthop. Trauma 2022, 32, 101941. [Google Scholar] [CrossRef]
- Hwang, J.; Cannady, D.F.; Nino, S.; Koval, K.J.; Langford, J.R.; Parry, J.A. Comparison of standard versus reconstruction proximal interlocking screw configurations for antegrade intramedullary nail fixation of femoral shaft fractures. J. Clin. Orthop. Trauma 2021, 17, 94–98. [Google Scholar] [CrossRef] [PubMed]
- Brumback, R.J.; Toal, T.R.; Murphy-Zane, M.S.; Novak, V.P.; Belkoff, S.M. Immediate weight-bearing after treatment of a comminuted fracture of the femoral shaft with a statically locked intramedullary nail. J. Bone Joint Surg. Am. 1999, 81, 1538–1544. [Google Scholar] [CrossRef]
- Brumback, R.J.; Uwagie-Ero, S.; Lakatos, R.P.; Poka, A.; Bathon, G.H.; Burgess, A.R. Intramedullary nailing of femoral shaft fractures. Part II: Fracture-healing with static interlocking fixation. J. Bone Joint Surg. Am. 1988, 70, 1453–1462. [Google Scholar] [CrossRef]
- George, C.J.; Lindsey, R.W.; Noble, P.C.; Alexander, J.W.; Kamaric, E. Optimal location of a single distal interlocking screw in intramedullary nailing of distal third femoral shaft fractures. J. Orthop. Trauma 1998, 12, 267–272. [Google Scholar] [CrossRef] [PubMed]
- Grover, J.; Wiss, D.A. A prospective study of fractures of the femoral shaft treated with a static, intramedullary, interlocking nail comparing one versus two distal screws. Orthop. Clin. North Am. 1995, 26, 139–146. [Google Scholar] [CrossRef]
- Hajek, P.D.; Bicknell, H.R.; Bronson, W.E.; Albright, J.A.; Saha, S. The use of one compared with two distal screws in the treatment of femoral shaft fractures with interlocking intramedullary nailing. A clinical and biomechanical analysis. J. Bone Joint Surg. Am. 1993, 75, 519–525. [Google Scholar] [CrossRef]
- Arazi, M.; Oğün, T.C.; Oktar, M.N.; Memik, R.; Kutlu, A. Early weight-bearing after statically locked reamed intramedullary nailing of comminuted femoral fractures: Is it a safe procedure? J. Trauma 2001, 50, 711–716. [Google Scholar] [CrossRef] [PubMed]
- Hussain, M.; Askari Rizvi, S.H.; Abbas, N.; Sajjad, U.; Shad, M.R.; Badshah, M.A.; Malik, A.I. Recent Developments in Coatings for Orthopedic Metallic Implants. Coatings 2021, 11, 791. [Google Scholar] [CrossRef]
- Simon, U.; Augat, P.; Utz, M.; Claes, L. A numerical model of the fracture healing process that describes tissue development and revascularisation. Comput. Methods Biomech. Biomed. Engin. 2011, 14, 79–793. [Google Scholar] [CrossRef]
- Ramos-Maza, E.; Chávez-Cobarrubias, G.; García-Estrada, F.; Buffo-Sequeira, I.; Dominguez-Barrios, C.; Meza-Reyes, G. Biomecánica de la estabilidad. Acta Ortop. Mex. 2016, 30, 9–13. [Google Scholar]
- Lipphaus, A.; Witzel, U. Finite-Element Syntheses of Callus and Bone Remodeling: Biomechanical Study of Fracture Healing in Long Bones. Anat. Rec. 2018, 301, 2112–2121. [Google Scholar] [CrossRef] [PubMed]
- Yamaji, T.; Ando, K.; Wolf, S.; Augat, P.; Claes, L. The effect of micromovement on callus formation. J. Orthop. Sci. Off. J. Jpn. Orthop. Assoc. 2001, 6, 571–575. [Google Scholar] [CrossRef]
- Epari, D.R.; Kassi, J.P.; Schell, H.; Duda, G.N. Timely fracture-healing requires optimization of axial fixation stability. J. Bone Joint Surg. Am. 2007, 89, 1575–1585. [Google Scholar] [CrossRef] [PubMed]
- Hussain, M.; Khan, S.M.; Al-Khaled, K.; Ayadi, M.; Abbas, N.; Chammam, W. Performance analysis of biodegradable materials for orthopedic applications. Mater. Today Commun. 2022, 31, 103167. [Google Scholar] [CrossRef]
- Di, T.; Xu, Y.; Liu, D.; Sun, X. Microstructure, Mechanical Performance and Anti-Bacterial Activity of Degradable Zn-Cu-Ag Alloy. Metals 2022, 12, 1444. [Google Scholar] [CrossRef]
- Hussain, M.; Ullah, S.; Raza, M.R.; Abbas, N.; Ali, A. Recent Developments in Zn-Based Biodegradable Materials for Biomedical Applications. J. Funct. Biomater. 2023, 14, 1. [Google Scholar] [CrossRef] [PubMed]
- Sha, M.; Guo, Z.; Fu, J.; Li, J.; Fan Yuan, C.; Shi, L.; Jun Li, S. The effects of nail rigidity on fracture healing in rats with osteoporosis. Acta Orthop. 2009, 80, 135–138. [Google Scholar] [CrossRef]
| Material | Young Modulus (MPa) | Poisson Ratio | Tensile Strength, Yield (MPa) | Tensile Strength, Ultimate (MPa) |
|---|---|---|---|---|
| Cortical bone | 20,000 | 0.30 | ||
| Cancellous bone | 959 | 0.12 | ||
| Steel 316 LVM | 192,360 | 0.30 | 690 | 860 |
| TitaniumTi-6Al-4V | 113,760 | 0.34 | 785 | 896 |
| Type of Fracture | Fracture Location | Distal Locking | Nail Material | |
|---|---|---|---|---|
| Model 1 | Inverse | Subtrochanteric | Static | Steel |
| Model 2 | Dynamic | |||
| Model 3 | Inverse | Subtrochanteric | Static | Titanium |
| Model 4 | Dynamic |
| Distal Locking | Dynamic/Static (%) | ||
|---|---|---|---|
| Dynamic | Static | ||
| Maximum displacement in the femoral head (mm) | 3.97 | 3.84 | 3.36 |
| Mobility at the fracture site (µm) | 340 | 305 | 11.46 |
| Maximum stress in the nail at fracture site (MPa) | 106.21 | 105.96 | 0.24 |
| Maximum stress in the cortical bone at the level of the distal screws (MPa) | 20.01 | 15.74 | 27.16 |
| Type of Material | Titanium/Steel (%) | ||
|---|---|---|---|
| Steel | Titanium | ||
| Maximum displacement in the femoral head (mm) | 3.97 | 5.32 | 34.00 |
| Mobility at the fracture site (µm) | 340 | 535 | 57.35 |
| Maximum stress in the nail at fracture site (MPa) | 106.21 | 100.91 | −4.99 |
| Maximum stress in the cortical bone at the level of the distal screws (MPa) | 20.01 | 19.19 | −0.41 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martínez-Aznar, C.; Mateo, J.; Ibarz, E.; Gracia, L.; Rosell, J.; Puértolas, S. Biomechanical Behavior of Dynamic vs. Static Distal Locking Intramedullary Nails in Subtrochanteric Femur Fractures. Bioengineering 2023, 10, 1179. https://doi.org/10.3390/bioengineering10101179
Martínez-Aznar C, Mateo J, Ibarz E, Gracia L, Rosell J, Puértolas S. Biomechanical Behavior of Dynamic vs. Static Distal Locking Intramedullary Nails in Subtrochanteric Femur Fractures. Bioengineering. 2023; 10(10):1179. https://doi.org/10.3390/bioengineering10101179
Chicago/Turabian StyleMartínez-Aznar, Carmen, Jesús Mateo, Elena Ibarz, Luis Gracia, Jorge Rosell, and Sergio Puértolas. 2023. "Biomechanical Behavior of Dynamic vs. Static Distal Locking Intramedullary Nails in Subtrochanteric Femur Fractures" Bioengineering 10, no. 10: 1179. https://doi.org/10.3390/bioengineering10101179
APA StyleMartínez-Aznar, C., Mateo, J., Ibarz, E., Gracia, L., Rosell, J., & Puértolas, S. (2023). Biomechanical Behavior of Dynamic vs. Static Distal Locking Intramedullary Nails in Subtrochanteric Femur Fractures. Bioengineering, 10(10), 1179. https://doi.org/10.3390/bioengineering10101179







