A Scientometric Analysis and Visualization of Prosthetic Foot Research Work: 2000 to 2022
Abstract
1. Introduction
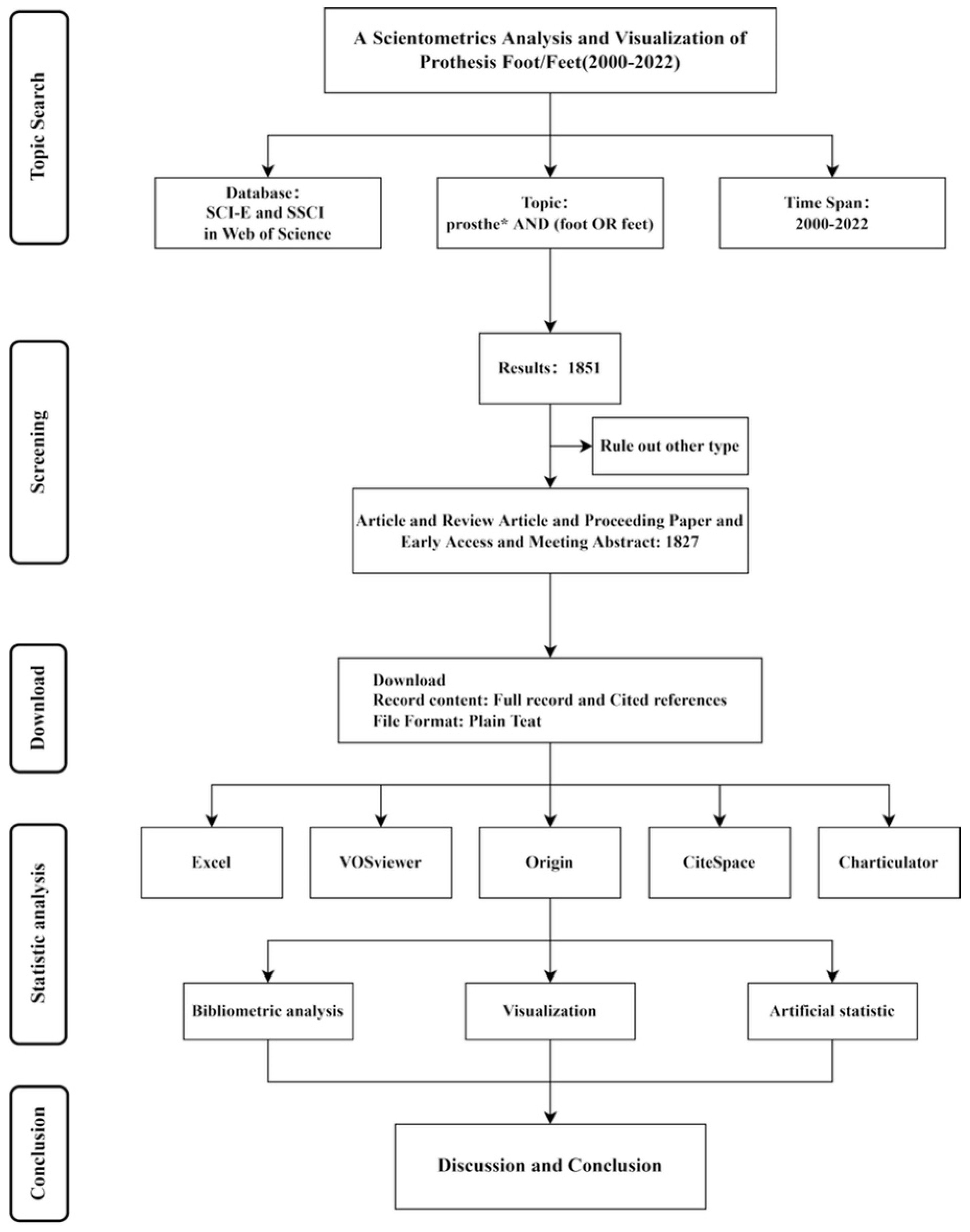
2. Methods
2.1. Data Acquisition and Search Strategy
2.2. Data Extraction and Analysis
3. Results
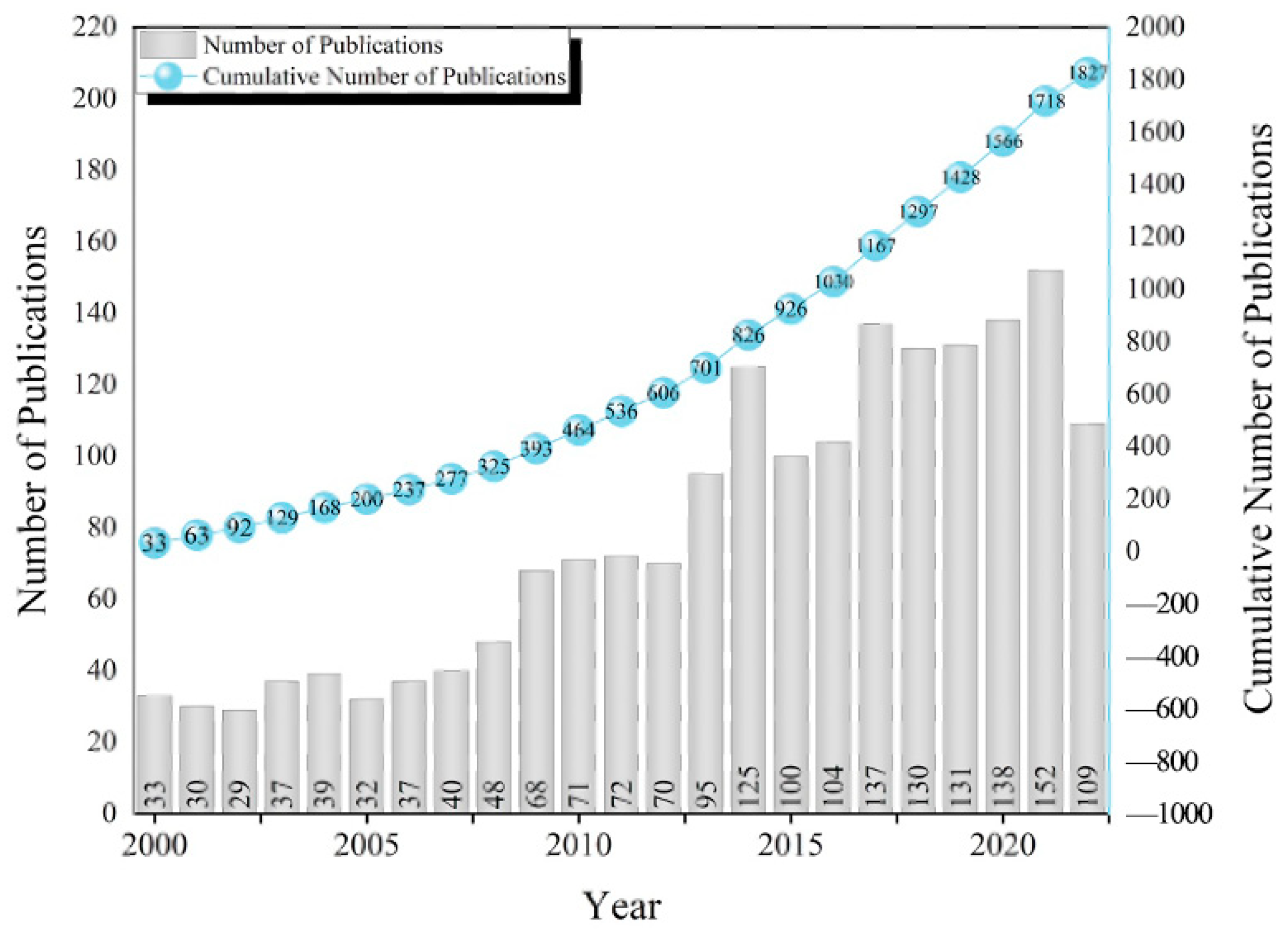
3.1. Publication Outputs
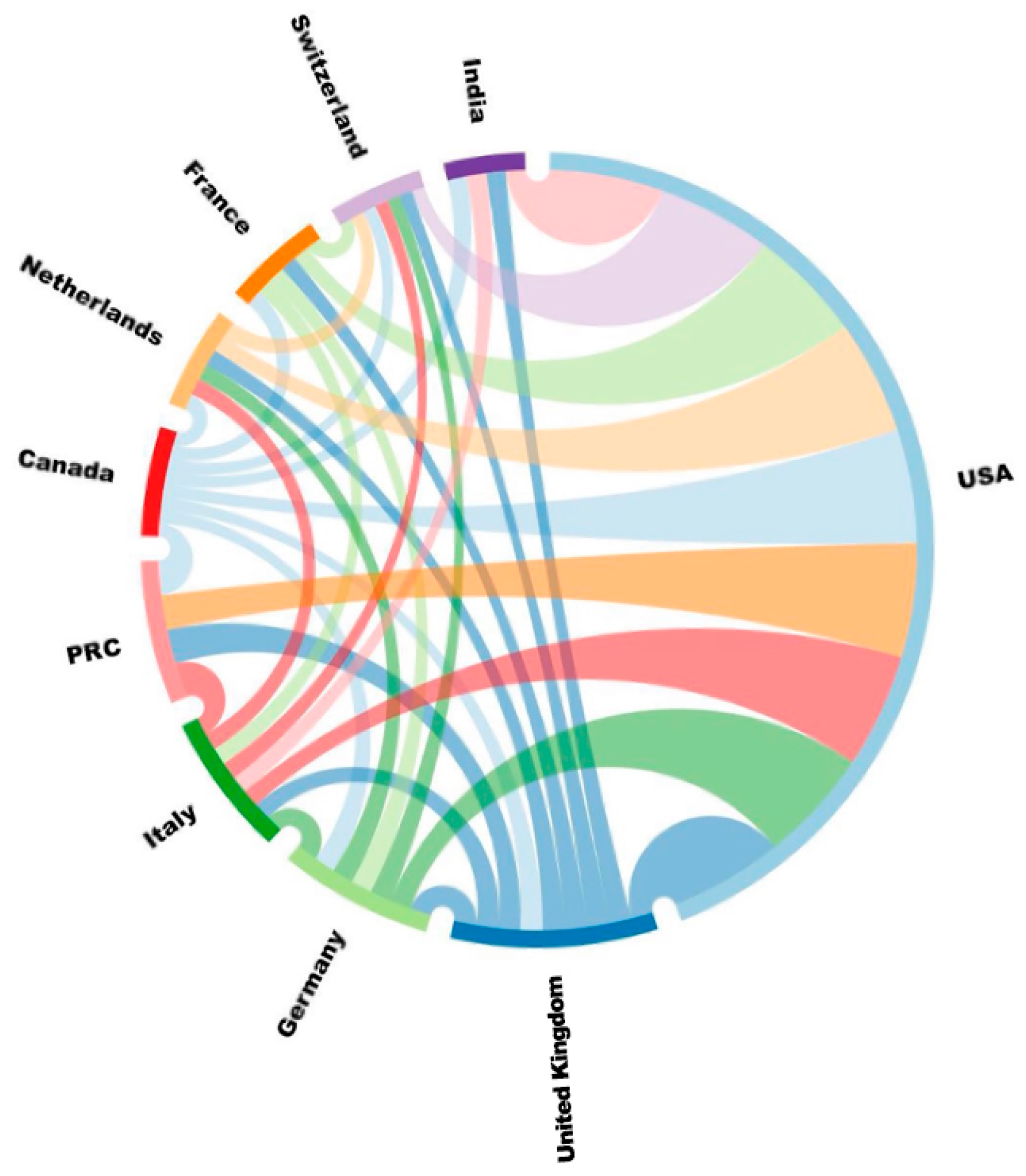
3.2. Distribution by Country and Institution
3.3. Distribution by Journal
3.4. Analysis of References
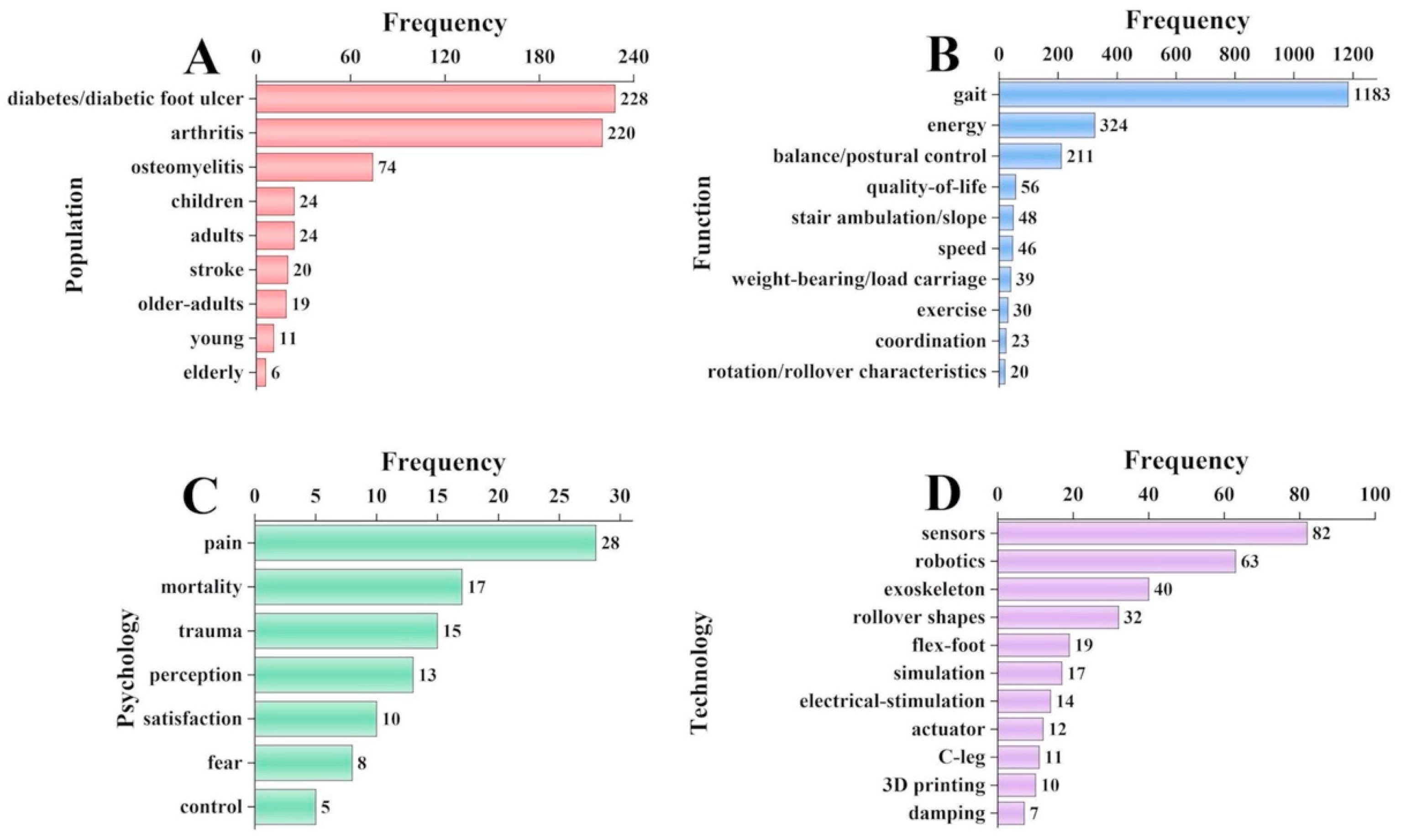
3.5. Analysis of Keywords
4. Discussion
4.1. Main Findings
4.2. Population
4.3. Function
4.4. Psychology
4.5. Technology
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- McDonald, C.L.; Westcott-McCoy, S.; Weaver, M.R.; Haagsma, J.; Kartin, D. Global prevalence of traumatic non-fatal limb amputation. Prosthet. Orthot. Int. 2021, 0309364620972258. [Google Scholar] [CrossRef] [PubMed]
- Molina, C.S.; Faulk, J. Lower Extremity Amputation. In StatPearls; StatPearls Publishing Copyright© 2022; StatPearls Publishing LLC.: Treasure Island, FL, USA, 2022. [Google Scholar]
- Ziegler-Graham, K.; MacKenzie, E.J.; Ephraim, P.L.; Travison, T.G.; Brookmeyer, R. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Arch. Phys. Med. Rehabil. 2008, 89, 422–429. [Google Scholar] [CrossRef] [PubMed]
- Price, M.A.; Beckerle, P.; Sup, F.C. Design optimization in lower limb prostheses: A review. IEEE Trans. Neural Syst. Rehabil. Eng. 2019, 27, 1574–1588. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Xu, X.; Liu, Y.; Zhong, K.; Zhang, H. Design of bionic active–passive hybrid-driven prosthesis based on gait analysis and simulation of compound control method. BioMed. Eng. OnLine 2021, 20, 126. [Google Scholar] [CrossRef] [PubMed]
- Gailey, R.; Allen, K.; Castles, J.; Kucharik, J.; Roeder, M. Review of secondary physical conditions associated with lower-limb amputation and long-term prosthesis use. J. Rehabil. Res. Dev. 2008, 45, 15. [Google Scholar] [CrossRef]
- Mellema, M.; Gjøvaag, T. Reported Outcome Measures in Studies of Real-World Ambulation in People with a Lower Limb Amputation: A Scoping Review. Sensors 2022, 22, 2243. [Google Scholar] [CrossRef]
- Kumar, P.K.; Charan, M.; Kanagaraj, S. Trends and challenges in lower limb prosthesis. IEEE Potentials 2017, 36, 19–23. [Google Scholar] [CrossRef]
- Rajťúková, V.; Michalíková, M.; Bednarčíková, L.; Balogová, A.; Živčák, J. Biomechanics of lower limb prostheses. Procedia Eng. 2014, 96, 382–391. [Google Scholar] [CrossRef]
- Condie, E.; Scott, H.; Treweek, S. Lower limb prosthetic outcome measures: A review of the literature 1995 to 2005. JPO J. Prosthet. Orthot. 2006, 18, P13–P45. [Google Scholar] [CrossRef]
- Gard, S.A. Use of quantitative gait analysis for the evaluation of prosthetic walking performance. JPO J. Prosthet. Orthot. 2006, 18, P93–P104. [Google Scholar] [CrossRef]
- Balk, E.M.; Gazula, A.; Markozannes, G.; Kimmel, H.J.; Saldanha, I.J.; Resnik, L.J.; Trikalinos, T.A. Lower Limb Prostheses: Measurement Instruments, Comparison of Component Effects by Subgroups, and Long-Term Outcomes [Internet]. 2018. Available online: https://europepmc.org/article/NBK/nbk531523: (accessed on 31 October 2022).
- Ghillebert, J.; De Bock, S.; Flynn, L.; Geeroms, J.; Tassignon, B.; Roelands, B.; Lefeber, D.; Vanderborght, B.; Meeusen, R.; De Pauw, K. Guidelines and recommendations to investigate the efficacy of a lower-limb prosthetic device: A systematic review. IEEE Trans. Med. Robot. Bionics 2019, 1, 279–296. [Google Scholar] [CrossRef]
- Moore, R. Patient evaluation of a novel prosthetic foot with hydraulic ankle aimed at persons with amputation with lower activity levels. JPO J. Prosthet. Orthot. 2017, 29, 44–47. [Google Scholar] [CrossRef]
- Vu, H.T.T.; Dong, D.; Cao, H.-L.; Verstraten, T.; Lefeber, D.; Vanderborght, B.; Geeroms, J. A review of gait phase detection algorithms for lower limb prostheses. Sensors 2020, 20, 3972. [Google Scholar] [CrossRef] [PubMed]
- Samuelsson, K.A.; Töytäri, O.; Salminen, A.-L.; Brandt, Å. Effects of lower limb prosthesis on activity, participation, and quality of life: A systematic review. Prosthet. Orthot. Int. 2012, 36, 145–158. [Google Scholar] [CrossRef]
- Safari, R. Lower limb prosthetic interfaces: Clinical and technological advancement and potential future direction. Prosthet. Orthot. Int. 2020, 44, 384–401. [Google Scholar] [CrossRef]
- Voloshina, A.; Collins, S. A Review of Design and Control Approaches in Lower-Limb Prosthetic Devices. Biology 2019. [Google Scholar]
- Andrysek, J. Lower-limb prosthetic technologies in the developing world: A review of literature from 1994–2010. Prosthet. Orthot. Int. 2010, 34, 378–398. [Google Scholar] [CrossRef]
- Xu, D.; Wang, Y.-L.; Wang, K.-T.; Wang, Y.; Dong, X.-R.; Tang, J.; Cui, Y.-L. A scientometrics analysis and visualization of depressive disorder. Curr. Neuropharmacol. 2021, 19, 766–786. [Google Scholar] [CrossRef]
- Xu, G.; Jin, B.; Xian, X.; Yang, H.; Zhao, H.; Du, S.; Makuuchi, M.; Pawlik, T.M.; Mao, Y. Evolutions in the management of hepatocellular carcinoma over last 4 decades: An analysis from the 100 most influential articles in the field. Liver Cancer 2021, 10, 137–150. [Google Scholar] [CrossRef]
- Stout, N.L.; Alfano, C.M.; Belter, C.W.; Nitkin, R.; Cernich, A.; Lohmann Siegel, K.; Chan, L. A bibliometric analysis of the landscape of cancer rehabilitation research (1992–2016). JNCI J. Natl. Cancer Inst. 2018, 110, 815–824. [Google Scholar] [CrossRef]
- Yan, W.; Zheng, K.; Weng, L.; Chen, C.; Kiartivich, S.; Jiang, X.; Su, X.; Wang, Y.; Wang, X. Bibliometric evaluation of 2000–2019 publications on functional near-infrared spectroscopy. NeuroImage 2020, 220, 117121. [Google Scholar] [CrossRef] [PubMed]
- Cruz Gonzalez, P.; Fong, K.N.; Chung, R.C.; Ting, K.-H.; Law, L.L.; Brown, T. Can transcranial direct-current stimulation alone or combined with cognitive training be used as a clinical intervention to improve cognitive functioning in persons with mild cognitive impairment and dementia? A systematic review and meta-analysis. Front. Hum. Neurosci. 2018, 12, 416. [Google Scholar] [CrossRef] [PubMed]
- Toh, S.F.M.; Fong, K.N.; Gonzalez, P.C.; Tang, Y.M. Application of home-based wearable technologies in physical rehabilitation for stroke: A scoping review. IEEE Trans. Neural Syst. Rehabil. Eng. 2023, 31, 1614–1623. [Google Scholar] [CrossRef] [PubMed]
- Synnestvedt, M.B.; Chen, C.; Holmes, J.H. CiteSpace II: Visualization and knowledge discovery in bibliographic databases. In Proceedings of the AMIA Annual Symposium Proceedings, Washington, DC, USA, 22–26 October 2005; p. 724. [Google Scholar]
- Liang, Y.-D.; Li, Y.; Zhao, J.; Wang, X.-Y.; Zhu, H.-Z.; Chen, X.-H. Study of acupuncture for low back pain in recent 20 years: A bibliometric analysis via CiteSpace. J. Pain Res. 2017, 10, 951. [Google Scholar] [CrossRef] [PubMed]
- Sun, W.; Song, J.; Dong, X.; Kang, X.; He, B.; Zhao, W.; Li, Z.; Feng, Z.; Chen, X. Bibliometric and visual analysis of transcranial direct current stimulation in the web of science database from 2000 to 2022 via CiteSpace. Front. Hum. Neurosci. 2022, 16, 1049572. [Google Scholar] [CrossRef]
- Özgür, A.; Vu, T.; Erkan, G.; Radev, D.R. Identifying gene-disease associations using centrality on a literature mined gene-interaction network. Bioinformatics 2008, 24, i277–i285. [Google Scholar] [CrossRef]
- Geiss, L.S.; Li, Y.; Hora, I.; Albright, A.; Rolka, D.; Gregg, E.W. Resurgence of diabetes-related nontraumatic lower-extremity amputation in the young and middle-aged adult US population. Diabetes Care 2019, 42, 50–54. [Google Scholar] [CrossRef]
- Wu, H.; Yang, A.; Lau, E.S.; Ma, R.C.; Kong, A.P.; Chow, E.; So, W.-Y.; Chan, J.C.; Luk, A.O. Secular trends in rates of hospitalisation for lower extremity amputation and 1 year mortality in people with diabetes in Hong Kong, 2001–2016: A retrospective cohort study. Diabetologia 2020, 63, 2689–2698. [Google Scholar] [CrossRef]
- Lazzarini, P.A.; Gurr, J.M.; Rogers, J.R.; Schox, A.; Bergin, S.M. Diabetes foot disease: The Cinderella of Australian diabetes management? J. Foot Ankle Res. 2012, 5, 24. [Google Scholar] [CrossRef]
- Wong, M.W. Lower extremity amputation in Hong Kong. Hong Kong Med. J. 2005, 11, 147–152. [Google Scholar]
- Riandini, T.; Pang, D.; Toh, M.P.; Tan, C.S.; Choong, A.M.; Lo, Z.J.; Chandrasekar, S.; Tai, E.S.; Tan, K.B.; Venkataraman, K. National rates of lower extremity amputation in people with and without diabetes in a multi-ethnic Asian population: A ten year study in Singapore. Eur. J. Vasc. Endovasc. Surg. 2022, 63, 147–155. [Google Scholar] [CrossRef] [PubMed]
- Kannan, K. Evaluation of Nerve Conduction Abnormalities and Brainstem Auditory Evoked Potentials in Type 2 Diabetes Mellitus; Madras Medical College: Chennai, India, 2011. [Google Scholar]
- Shi, Q.Q.; Li, P.L.; Yick, K.-L.; Li, N.-W.; Jiao, J. Effects of contoured insoles with different materials on plantar pressure offloading in diabetic elderly during gait. Sci. Rep. 2022, 12, 15395. [Google Scholar] [CrossRef] [PubMed]
- Shi, Q.-Q.; Li, P.-L.; Yick, K.-L.; Jiao, J.; Liu, Q.-L. Influence of Contoured Insoles with Different Materials on Kinematics and Kinetics Changes in Diabetic Elderly during Gait. Int. J. Environ. Res. Public Health 2022, 19, 12502. [Google Scholar] [CrossRef]
- Desveaux, L.; Goldstein, R.S.; Mathur, S.; Hassan, A.; Devlin, M.; Pauley, T.; Brooks, D. Physical activity in adults with diabetes following prosthetic rehabilitation. Can. J. Diabetes 2016, 40, 336–341. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.K.; Prasad, G. Long-term mortality after lower-limb amputation. Prosthet. Orthot. Int. 2016, 40, 545–551. [Google Scholar] [CrossRef] [PubMed]
- Movassaghi, K.; Wakefield, C.; Bohl, D.D.; Lee, S.; Lin, J.; Holmes Jr, G.B.; Hamid, K.S. Septic arthritis of the native ankle. JBJS Rev. 2019, 7, e6. [Google Scholar] [CrossRef]
- Simoni, G.; Maccauro, G.; Fenga, D.; De Santis, V.; Orani, R.; Centofanti, F.; Rosa, M. Arthrodesis of the ankle joint in septic osteoarthritis: Six years long term outcomes in authors’ personal experience. Eur. Rev. Med. Pharmacol. Sci. 2019, 23, 139–144. [Google Scholar]
- Wang, S.; Li, B.; Yu, X.; Wu, H.; Liu, L. Is Ankle Arthrodesis With an Ilizarov External Fixator an Effective Treatment for Septic Ankle Arthritis? A Study With a Minimum of 6 Years of Follow-up. Clin. Orthop. Relat. Res.® 2022, 481, 717–725. [Google Scholar] [CrossRef]
- Atluri, G.; Karpatne, A.; Kumar, V. Spatio-temporal data mining: A survey of problems and methods. ACM Comput. Surv. (CSUR) 2018, 51, 1–41. [Google Scholar] [CrossRef]
- Abouhossein, A.; Awad, M.I.; Maqbool, H.F.; Crisp, C.; Stewart, T.D.; Messenger, N.; Richardson, R.C.; Dehghani-Sanij, A.A.; Bradley, D. Foot trajectories and loading rates in a transfemoral amputee for six different commercial prosthetic knees: An indication of adaptability. Med. Eng. Phys. 2019, 68, 46–56. [Google Scholar] [CrossRef]
- Agrawal, V.; Gailey, R.S.; Gaunaurd, I.A.; O’Toole, C.; Finnieston, A.; Tolchin, R. Comparison of four different categories of prosthetic feet during ramp ambulation in unilateral transtibial amputees. Prosthet. Orthot. Int. 2015, 39, 380–389. [Google Scholar] [CrossRef] [PubMed]
- Aldridge, J.M.; Sturdy, J.T.; Wilken, J.M. Stair ascent kinematics and kinetics with a powered lower leg system following transtibial amputation. Gait Posture 2012, 36, 291–295. [Google Scholar] [CrossRef] [PubMed]
- Andrysek, J.; Wright, F.V.; Rotter, K.; Garcia, D.; Valdebenito, R.; Mitchell, C.A.; Rozbaczylo, C.; Cubillos, R. Long-term clinical evaluation of the automatic stance-phase lock-controlled prosthetic knee joint in young adults with unilateral above-knee amputation. Disabil. Rehabil. Assist. Technol. 2017, 12, 378–384. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Wensman, J.; Colabianchi, N.; Gates, D.H. The influence of powered prostheses on user perspectives, metabolics, and activity: A randomized crossover trial. J. Neuroeng. Rehabil. 2021, 18, 49. [Google Scholar] [CrossRef]
- Bai, X.; Ewins, D.; Crocombe, A.D.; Xu, W. Kinematic and biomimetic assessment of a hydraulic ankle/foot in level ground and camber walking. PLoS ONE 2017, 12, e0180836. [Google Scholar] [CrossRef]
- Bai, X.; Ewins, D.; Crocombe, A.D.; Xu, W. A biomechanical assessment of hydraulic ankle-foot devices with and without micro-processor control during slope ambulation in trans-femoral amputees. PLoS ONE 2018, 13, e0205093. [Google Scholar] [CrossRef]
- Barr, J.B.; Wutzke, C.J.; Threlkeld, A.J. Longitudinal gait analysis of a person with a transfemoral amputation using three different prosthetic knee/foot pairs. Physiother. Theory Pract. 2012, 28, 407–411. [Google Scholar] [CrossRef]
- Bellmann, M.; Schmalz, T.; Ludwigs, E.; Blumentritt, S. Immediate effects of a new microprocessor-controlled prosthetic knee joint: A comparative biomechanical evaluation. Arch. Phys. Med. Rehabil. 2012, 93, 541–549. [Google Scholar] [CrossRef]
- Burnfield, J.M.; Eberly, V.J.; Gronely, J.K.; Perry, J.; Yule, W.J.; Mulroy, S.J. Impact of stance phase microprocessor-controlled knee prosthesis on ramp negotiation and community walking function in K2 level transfemoral amputees. Prosthet. Orthot. Int. 2012, 36, 95–104. [Google Scholar] [CrossRef]
- Creylman, V.; Knippels, I.; Janssen, P.; Biesbrouck, E.; Lechler, K.; Peeraer, L. Assessment of transfemoral amputees using a passive microprocessor-controlled knee versus an active powered microprocessor-controlled knee for level walking. BioMed. Eng. OnLine 2016, 15, 53–63. [Google Scholar] [CrossRef]
- De Asha, A.R.; Munjal, R.; Kulkarni, J.; Buckley, J.G. Impact on the biomechanics of overground gait of using an ‘Echelon’hydraulic ankle–foot device in unilateral trans-tibial and trans-femoral amputees. Clin. Biomech. 2014, 29, 728–734. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Eberly, V.J.; Mulroy, S.J.; Gronley, J.K.; Perry, J.; Yule, W.J.; Burnfield, J.M. Impact of a stance phase microprocessor-controlled knee prosthesis on level walking in lower functioning individuals with a transfemoral amputation. Prosthet. Orthot. Int. 2014, 38, 447–455. [Google Scholar] [CrossRef] [PubMed]
- Russell Esposito, E.; Schmidtbauer, K.A.; Wilken, J.M. Experimental comparisons of passive and powered ankle-foot orthoses in individuals with limb reconstruction. J. Neuroeng. Rehabil. 2018, 15, 111. [Google Scholar] [CrossRef]
- Ferris, A.E.; Aldridge, J.M.; Rábago, C.A.; Wilken, J.M. Evaluation of a powered ankle-foot prosthetic system during walking. Arch. Phys. Med. Rehabil. 2012, 93, 1911–1918. [Google Scholar] [CrossRef]
- Fradet, L.; Alimusaj, M.; Braatz, F.; Wolf, S.I. Biomechanical analysis of ramp ambulation of transtibial amputees with an adaptive ankle foot system. Gait Posture 2010, 32, 191–198. [Google Scholar] [CrossRef]
- Gailey, R.S.; Gaunaurd, I.; Agrawal, V.; Finnieston, A.; Tolchin, R. Application of self-report and performance-based outcome measures to determine functional differences between four categories of prosthetic feet. J. Rehabil. Res. Dev. 2012, 49, 597–612. [Google Scholar] [CrossRef]
- Hasenoehrl, T.; Schmalz, T.; Windhager, R.; Domayer, S.; Dana, S.; Ambrozy, C.; Palma, S.; Crevenna, R. Safety and function of a prototype microprocessor-controlled knee prosthesis for low active transfemoral amputees switching from a mechanic knee prosthesis: A pilot study. Disabil. Rehabil. Assist. Technol. 2018, 13, 157–165. [Google Scholar] [CrossRef] [PubMed]
- Highsmith, M.J.; Kahle, J.T.; Kaluf, B.; Miro, R.M.; Mengelkoch, L.J.; Klenow, T.D. Psychometric evaluation of the hill assessment index (HAI) and stair assessment index (SAI) in high-functioning transfemoral amputees. Technol. Innov. 2016, 18, 193–201. [Google Scholar] [CrossRef]
- Houdijk, H.; Wezenberg, D.; Hak, L.; Cutti, A.G. Energy storing and return prosthetic feet improve step length symmetry while preserving margins of stability in persons with transtibial amputation. J. NeuroEng. Rehabil. 2018, 15, 76. [Google Scholar] [CrossRef]
- Ingraham, K.A.; Fey, N.P.; Simon, A.M.; Hargrove, L.J. Assessing the relative contributions of active ankle and knee assistance to the walking mechanics of transfemoral amputees using a powered prosthesis. PLoS ONE 2016, 11, e0147661. [Google Scholar] [CrossRef]
- Johnson, L.; De Asha, A.R.; Munjal, R.; Kulkarni, J.; Buckley, J.G. Toe Clearance When Walking in People with Unilateral Transtibial Amputation: Effects of Passive Hydraulic Ankle. J. Rehabil. Res. 2014, 51, 429–438. [Google Scholar] [CrossRef] [PubMed]
- Kaufman, K.R.; Frittoli, S.; Frigo, C.A. Gait asymmetry of transfemoral amputees using mechanical and microprocessor-controlled prosthetic knees. Clin. Biomech. 2012, 27, 460–465. [Google Scholar] [CrossRef] [PubMed]
- Klodd, E.; Hansen, A.; Fatone, S.; Edwards, M. Effects of prosthetic foot forefoot flexibility on oxygen cost and subjective preference rankings of unilateral transtibial prosthesis users. J. Rehabil. Res. Dev. 2010, 47, 543–552. [Google Scholar] [CrossRef] [PubMed]
- Koehler-McNicholas, S.R.; Savvas Slater, B.C.; Koester, K.; Nickel, E.A.; Ferguson, J.E.; Hansen, A.H. Bimodal ankle-foot prosthesis for enhanced standing stability. PLoS ONE 2018, 13, e0204512. [Google Scholar] [CrossRef]
- Lura, D.J.; Wernke, M.M.; Carey, S.L.; Kahle, J.T.; Miro, R.M.; Highsmith, M.J. Differences in knee flexion between the Genium and C-Leg microprocessor knees while walking on level ground and ramps. Clin. Biomech. 2015, 30, 175–181. [Google Scholar] [CrossRef]
- Major, M.; Twiste, M.; Kenney, L.; Howard, D. The effects of prosthetic ankle stiffness on stability of gait in people with trans-tibial amputation. J. Rehabil. Res. Dev. 2016, 53, 839–852. [Google Scholar] [CrossRef]
- McGrath, M.; Laszczak, P.; Zahedi, S.; Moser, D. The influence of a microprocessor-controlled hydraulic ankle on the kinetic symmetry of trans-tibial amputees during ramp walking: A case series. J. Rehabil. Assist. Technol. Eng. 2018, 5, 2055668318790650. [Google Scholar] [CrossRef]
- Martinez-Villalpando, E.C.; Mooney, L.; Elliott, G.; Herr, H. Antagonistic active knee prosthesis. A metabolic cost of walking comparison with a variable-damping prosthetic knee. In Proceedings of the 2011 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Boston, MA, USA, 30 August–3 September 2011; pp. 8519–8522. [Google Scholar]
- McDonald, C.L.; Kramer, P.A.; Morgan, S.J.; Halsne, E.G.; Cheever, S.M.; Hafner, B.J. Energy expenditure in people with transtibial amputation walking with crossover and energy storing prosthetic feet: A randomized within-subject study. Gait Posture 2018, 62, 349–354. [Google Scholar] [CrossRef]
- Mengelkoch, L.J.; Kahle, J.T.; Highsmith, M.J. Energy costs and performance of transfemoral amputees and non-amputees during walking and running: A pilot study. Prosthet. Orthot. Int. 2017, 41, 484–491. [Google Scholar] [CrossRef]
- Morgan, S.J.; Hafner, B.J.; Kelly, V.E. The effects of a concurrent task on walking in persons with transfemoral amputation compared to persons without limb loss. Prosthet. Orthot. Int. 2016, 40, 490–496. [Google Scholar] [CrossRef]
- Mulder, I.A.; Holtslag, H.R.; Beersma, L.F.; Koopman, B.F. Keep moving forward: A new energy returning prosthetic device with low installation height after Syme or Pirogoff amputation. Prosthet. Orthot. Int. 2014, 38, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Nickel, E. Passive prosthetic ankle-foot mechanism for automatic adaptation to sloped surfaces. J. Rehabil. Res. Dev. 2014, 51, 803. [Google Scholar] [CrossRef] [PubMed]
- Pew, C.; Klute, G.K. Pilot testing of a variable stiffness transverse plane adapter for lower limb amputees. Gait Posture 2017, 51, 104–108. [Google Scholar] [CrossRef]
- Pickle, N.T.; Wilken, J.M.; Whitehead, J.M.A.; Silverman, A.K. Whole-body angular momentum during sloped walking using passive and powered lower-limb prostheses. J. Biomech. 2016, 49, 3397–3406. [Google Scholar] [CrossRef]
- Prinsen, E.C.; Nederhand, M.J.; Sveinsdóttir, H.; Prins, M.; Van der Meer, F.; Koopman, H.F.; Rietman, J.S. The influence of a user-adaptive prosthetic knee across varying walking speeds: A randomized cross-over trial. Gait Posture 2017, 51, 254–260. [Google Scholar] [CrossRef] [PubMed]
- Quesada, R.E.; Caputo, J.M.; Collins, S.H. Increasing ankle push-off work with a powered prosthesis does not necessarily reduce metabolic rate for transtibial amputees. J. Biomech. 2016, 49, 3452–3459. [Google Scholar] [CrossRef]
- Rosenblatt, N.J.; Bauer, A.; Rotter, D.; Grabiner, M.D. Active dorsiflexing prostheses may reduce trip-related fall risk in people with transtibial amputation. J. Rehabil. Res. Dev. 2014, 51, 1229–1242. [Google Scholar] [CrossRef]
- Rock, C.G.; Wurdeman, S.R.; Stergiou, N.; Takahashi, K.Z. Stride-to-stride fluctuations in transtibial amputees are not affected by changes in push-off mechanics from using different prostheses. PLoS ONE 2018, 13, e0205098. [Google Scholar] [CrossRef]
- Roerdink, M.; Cutti, A.G.; Summa, A.; Monari, D.; Veronesi, D.; van Ooijen, M.W.; Beek, P.J. Gaitography applied to prosthetic walking. Med. Biol. Eng. Comput. 2014, 52, 963–969. [Google Scholar] [CrossRef]
- Schmalz, T.; Altenburg, B.; Ernst, M.; Bellmann, M.; Rosenbaum, D. Lower limb amputee gait characteristics on a specifically designed test ramp: Preliminary results of a biomechanical comparison of two prosthetic foot concepts. Gait Posture 2019, 68, 161–167. [Google Scholar] [CrossRef]
- Segal, A.D.; Zelik, K.E.; Klute, G.K.; Morgenroth, D.C.; Hahn, M.E.; Orendurff, M.S.; Adamczyk, P.G.; Collins, S.H.; Kuo, A.D.; Czerniecki, J.M. The effects of a controlled energy storage and return prototype prosthetic foot on transtibial amputee ambulation. Hum. Mov. Sci. 2012, 31, 918–931. [Google Scholar] [CrossRef] [PubMed]
- Shepherd, M.K.; Rouse, E.J. The VSPA foot: A quasi-passive ankle-foot prosthesis with continuously variable stiffness. IEEE Trans. Neural Syst. Rehabil. Eng. 2017, 25, 2375–2386. [Google Scholar] [CrossRef] [PubMed]
- Shultz, A.H.; Goldfarb, M. A unified controller for walking on even and uneven terrain with a powered ankle prosthesis. IEEE Trans. Neural Syst. Rehabil. Eng. 2018, 26, 788–797. [Google Scholar] [CrossRef]
- Takahashi, K.Z.; Horne, J.R.; Stanhope, S.J. Comparison of mechanical energy profiles of passive and active below-knee prostheses: A case study. Prosthet. Orthot. Int. 2015, 39, 150–156. [Google Scholar] [CrossRef] [PubMed]
- Thiele, J.; Westebbe, B.; Bellmann, M.; Kraft, M. Designs and performance of microprocessor-controlled knee joints. Biomed. Tech./Biomed. Eng. 2014, 59, 65–77. [Google Scholar] [CrossRef] [PubMed]
- Thiele, J.; Schöllig, C.; Bellmann, M.; Kraft, M. Designs and performance of three new microprocessor-controlled knee joints. Biomed. Eng./Biomed. Tech. 2019, 64, 119–126. [Google Scholar] [CrossRef]
- Wezenberg, D.; Cutti, A.G.; Bruno, A.; Houdijk, H. Differentiation between solid-ankle cushioned heel and energy storage and return prosthetic foot based on step-to-step transition cost. J. Rehabil. Res. Dev. 2014, 51, 1579–1590. [Google Scholar] [CrossRef]
- Wolf, E.J.; Everding, V.Q.; Linberg, A.L.; Schnall, B.L.; Czerniecki, J.M.; Gambel, J.M. Assessment of transfemoral amputees using C-Leg and Power Knee for ascending and descending inclines and steps. J. Rehabil. Res. Dev. 2012, 49, 831–842. [Google Scholar] [CrossRef]
- Aldridge Whitehead, J.M.; Wolf, E.J.; Scoville, C.R.; Wilken, J.M. Does a microprocessor-controlled prosthetic knee affect stair ascent strategies in persons with transfemoral amputation? Clin. Orthop. Relat. Res.® 2014, 472, 3093–3101. [Google Scholar] [CrossRef][Green Version]
- Knaepen, K.; Marusic, U.; Crea, S.; Guerrero, C.D.R.; Vitiello, N.; Pattyn, N.; Mairesse, O.; Lefeber, D.; Meeusen, R. Psychophysiological response to cognitive workload during symmetrical, asymmetrical and dual-task walking. Hum. Mov. Sci. 2015, 40, 248–263. [Google Scholar] [CrossRef]
- Mâaref, K.; Martinet, N.; Grumillier, C.; Ghannouchi, S.; André, J.M.; Paysant, J. Kinematics in the terminal swing phase of unilateral transfemoral amputees: Microprocessor-controlled versus swing-phase control prosthetic knees. Arch. Phys. Med. Rehabil. 2010, 91, 919–925. [Google Scholar] [CrossRef]
- Portnoy, S.; Kristal, A.; Gefen, A.; Siev-Ner, I. Outdoor dynamic subject-specific evaluation of internal stresses in the residual limb: Hydraulic energy-stored prosthetic foot compared to conventional energy-stored prosthetic feet. Gait Posture 2012, 35, 121–125. [Google Scholar] [CrossRef]
- Raschke, S.U.; Orendurff, M.S.; Mattie, J.L.; Kenyon, D.E.; Jones, O.Y.; Moe, D.; Winder, L.; Wong, A.S.; Moreno-Hernández, A.; Highsmith, M.J. Biomechanical characteristics, patient preference and activity level with different prosthetic feet: A randomized double blind trial with laboratory and community testing. J. Biomech. 2015, 48, 146–152. [Google Scholar] [CrossRef]
- Brandt, A.; Wen, Y.; Liu, M.; Stallings, J.; Huang, H.H. Interactions between transfemoral amputees and a powered knee prosthesis during load carriage. Sci. Rep. 2017, 7, 14480. [Google Scholar] [CrossRef]
- Hood, S.A.; Lenzi, T. Preliminary analysis of positive knee energy injection in a transfemoral amputee walking with a powered prosthesis. In Proceedings of the 2018 40th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Honolulu, HI, USA, 18–21 July 2018; pp. 1821–1824. [Google Scholar]
- Ray, S.F.; Wurdeman, S.R.; Takahashi, K.Z. Prosthetic energy return during walking increases after 3 weeks of adaptation to a new device. J. Neuroeng. Rehabil. 2018, 15, 6. [Google Scholar] [CrossRef] [PubMed]
- Bell, E.M.; Pruziner, A.L.; Wilken, J.M.; Wolf, E.J. Performance of conventional and X2® prosthetic knees during slope descent. Clin. Biomech. 2016, 33, 26–31. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Gjovaag, T.; Starholm, I.M.; Mirtaheri, P.; Hegge, F.W.; Skjetne, K. Assessment of aerobic capacity and walking economy of unilateral transfemoral amputees. Prosthet. Orthot. Int. 2014, 38, 140–147. [Google Scholar] [CrossRef]
- Grimmer, M.; Holgate, M.; Ward, J.; Boehler, A.; Seyfarth, A. Feasibility study of transtibial amputee walking using a powered prosthetic foot. In Proceedings of the 2017 International Conference on Rehabilitation Robotics (ICORR), London, UK, 17–20 July 2017; pp. 1118–1123. [Google Scholar]
- Howard, C.L.; Perry, B.; Chow, J.W.; Wallace, C.; Stokic, D.S. Increased alertness, better than posture prioritization, explains dual-task performance in prosthesis users and controls under increasing postural and cognitive challenge. Exp. Brain Res. 2017, 235, 3527–3539. [Google Scholar] [CrossRef] [PubMed]
- Williams, M.R.; D’Andrea, S.; Herr, H.M. Impact on gait biomechanics of using an active variable impedance prosthetic knee. J. Neuroeng. Rehabil. 2016, 13, 54. [Google Scholar] [CrossRef] [PubMed]
- Prinsen, E.C.; Nederhand, M.J.; Koopman, B.F.; Rietman, J.S. The influence of a user-adaptive prosthetic knee on planned gait termination. In Proceedings of the 2017 International Conference on Rehabilitation Robotics (ICORR), London, UK, 17–20 July 2017; pp. 1254–1259. [Google Scholar]
- Bellmann, M.; Köhler, T.M.; Schmalz, T. Comparative biomechanical evaluation of two technologically different microprocessor-controlled prosthetic knee joints in safety-relevant daily-life situations. Biomed. Eng./Biomed. Tech. 2019, 64, 407–420. [Google Scholar] [CrossRef]
- Feng, Y.; Wang, Q. Combining push-off power and nonlinear damping behaviors for a lightweight motor-driven transtibial prosthesis. IEEE/ASME Trans. Mechatron. 2017, 22, 2512–2523. [Google Scholar] [CrossRef]
- Kendell, C.; Lemaire, E.D.; Kofman, J.; Dudek, N. Gait adaptations of transfemoral prosthesis users across multiple walking tasks. Prosthet. Orthot. Int. 2016, 40, 89–95. [Google Scholar] [CrossRef] [PubMed]
- Mishra, P.; Singh, S.; Ranjan, V.; Singh, S.; Vidyarthi, A. Performance evaluation of Jaipur knee joint through kinematics and kinetics gait symmetry with unilateral transfemoral indian amputees. J. Med. Syst. 2019, 43, 55. [Google Scholar] [CrossRef]
- Struchkov, V.; Buckley, J.G. Biomechanics of ramp descent in unilateral trans-tibial amputees: Comparison of a microprocessor controlled foot with conventional ankle–foot mechanisms. Clin. Biomech. 2016, 32, 164–170. [Google Scholar] [CrossRef] [PubMed]
- Svoboda, Z.; Janura, M.; Cabell, L.; Elfmark, M. Variability of kinetic variables during gait in unilateral transtibial amputees. Prosthet. Orthot. Int. 2012, 36, 225–230. [Google Scholar] [CrossRef]
- Simon, A.M.; Fey, N.P.; Finucane, S.B.; Lipschutz, R.D.; Hargrove, L.J. Strategies to reduce the configuration time for a powered knee and ankle prosthesis across multiple ambulation modes. In Proceedings of the 2013 IEEE 13th International Conference on Rehabilitation Robotics (ICORR), Seattle, WA, USA, 24–26 June 2013; pp. 1–6. [Google Scholar]
- Simon, A.M.; Ingraham, K.A.; Fey, N.P.; Finucane, S.B.; Lipschutz, R.D.; Young, A.J.; Hargrove, L.J. Configuring a powered knee and ankle prosthesis for transfemoral amputees within five specific ambulation modes. PLoS ONE 2014, 9, e99387. [Google Scholar] [CrossRef] [PubMed]
- Adamczyk, P.G.; Roland, M.; Hahn, M.E. Sensitivity of biomechanical outcomes to independent variations of hindfoot and forefoot stiffness in foot prostheses. Hum. Mov. Sci. 2017, 54, 154–171. [Google Scholar] [CrossRef]
- Culver, S.; Bartlett, H.; Shultz, A.; Goldfarb, M. A stair ascent and descent controller for a powered ankle prosthesis. IEEE Trans. Neural Syst. Rehabil. Eng. 2018, 26, 993–1002. [Google Scholar] [CrossRef]
- Fey, N.P.; Klute, G.K.; Neptune, R.R. The influence of energy storage and return foot stiffness on walking mechanics and muscle activity in below-knee amputees. Clin. Biomech. 2011, 26, 1025–1032. [Google Scholar] [CrossRef]
- Hansen, A.; Nickel, E.; Medvec, J.; Brielmaier, S.; Pike, A.; Weber, M. Effects of a flat prosthetic foot rocker section on balance and mobility. J. Rehabil. Res. Dev. 2014, 51, 137–148. [Google Scholar] [CrossRef]
- Highsmith, M.J.; Kahle, J.T.; Carey, S.L.; Lura, D.J.; Dubey, R.V.; Csavina, K.R.; Quillen, W.S. Kinetic asymmetry in transfemoral amputees while performing sit to stand and stand to sit movements. Gait Posture 2011, 34, 86–91. [Google Scholar] [CrossRef] [PubMed]
- Huang, S.; Wensman, J.P.; Ferris, D.P. Locomotor adaptation by transtibial amputees walking with an experimental powered prosthesis under continuous myoelectric control. IEEE Trans. Neural Syst. Rehabil. Eng. 2015, 24, 573–581. [Google Scholar] [CrossRef] [PubMed]
- Kark, L.; Simmons, A. Patient satisfaction following lower-limb amputation: The role of gait deviation. Prosthet. Orthot. Int. 2011, 35, 225–233. [Google Scholar] [CrossRef] [PubMed]
- Ledoux, E.D.; Goldfarb, M. Control and evaluation of a powered transfemoral prosthesis for stair ascent. IEEE Trans. Neural Syst. Rehabil. Eng. 2017, 25, 917–924. [Google Scholar] [CrossRef]
- Lura, D.J.; Wernke, M.W.; Carey, S.L.; Kahle, J.T.; Miro, R.M.; Highsmith, M.J. Crossover study of amputee stair ascent and descent biomechanics using Genium and C-Leg prostheses with comparison to non-amputee control. Gait Posture 2017, 58, 103–107. [Google Scholar] [CrossRef]
- Wu, M.; Haque, M.R.; Shen, X. Obtaining natural sit-to-stand motion with a biomimetic controller for powered knee prostheses. J. Healthc. Eng. 2017, 2017, 3850351. [Google Scholar] [CrossRef]
- Pickle, N.T.; Wilken, J.M.; Aldridge, J.M.; Neptune, R.R.; Silverman, A.K. Whole-body angular momentum during stair walking using passive and powered lower-limb prostheses. J. Biomech. 2014, 47, 3380–3389. [Google Scholar] [CrossRef]
- Turcot, K.; Sagawa Jr, Y.; Lacraz, A.; Lenoir, J.; Assal, M.; Armand, S. Comparison of the International Committee of the Red Cross foot with the solid ankle cushion heel foot during gait: A randomized double-blind study. Arch. Phys. Med. Rehabil. 2013, 94, 1490–1497. [Google Scholar] [CrossRef]
- Ventura, J.D.; Klute, G.K.; Neptune, R.R. The effects of prosthetic ankle dorsiflexion and energy return on below-knee amputee leg loading. Clin. Biomech. 2011, 26, 298–303. [Google Scholar] [CrossRef]
- Zelik, K.E.; Collins, S.H.; Adamczyk, P.G.; Segal, A.D.; Klute, G.K.; Morgenroth, D.C.; Hahn, M.E.; Orendurff, M.S.; Czerniecki, J.M.; Kuo, A.D. Systematic variation of prosthetic foot spring affects center-of-mass mechanics and metabolic cost during walking. IEEE Trans. Neural Syst. Rehabil. Eng. 2011, 19, 411–419. [Google Scholar] [CrossRef]
- Shultz, A.H.; Lawson, B.E.; Goldfarb, M. Variable cadence walking and ground adaptive standing with a powered ankle prosthesis. IEEE Trans. Neural Syst. Rehabil. Eng. 2015, 24, 495–505. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Montgomery, J.R.; Grabowski, A.M. Use of a powered ankle–foot prosthesis reduces the metabolic cost of uphill walking and improves leg work symmetry in people with transtibial amputations. J. R. Soc. Interface 2018, 15, 20180442. [Google Scholar] [CrossRef] [PubMed]
- Grabowski, A.M.; D’Andrea, S. Effects of a powered ankle-foot prosthesis on kinetic loading of the unaffected leg during level-ground walking. J. Neuroeng. Rehabil. 2013, 10, 49. [Google Scholar] [CrossRef] [PubMed]
- Inoue, K.; Hobara, H.; Wada, T. Effects of inertial properties of transfemoral prosthesis on leg swing motion during stair ascent. In Proceedings of the 2013 35th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Osaka, Japan, 3–7 July 2013; pp. 1591–1594. [Google Scholar]
- Delussu, A.S.; Brunelli, S.; Paradisi, F.; Iosa, M.; Pellegrini, R.; Zenardi, D.; Traballesi, M. Assessment of the effects of carbon fiber and bionic foot during overground and treadmill walking in transtibial amputees. Gait Posture 2013, 38, 876–882. [Google Scholar] [CrossRef]
- Srisuwan, B.; Klute, G.K. Locomotor activities of individuals with lower-limb amputation. Prosthet. Orthot. Int. 2021, 45, 191–197. [Google Scholar] [CrossRef]
- Czerniecki, J.M.; Morgenroth, D.C. Metabolic energy expenditure of ambulation in lower extremity amputees: What have we learned and what are the next steps? Disabil. Rehabil. 2017, 39, 143–151. [Google Scholar] [CrossRef]
- Sadeghi, H.; Allard, P.; Duhaime, M. Muscle power compensatory mechanisms in below-knee amputee gait. Am. J. Phys. Med. Rehabil. 2001, 80, 25–32. [Google Scholar] [CrossRef]
- Ibarra Aguila, S.; Sánchez, G.J.; Sauvain, E.E.; Alemon, B.; Fuentes-Aguilar, R.Q.; Huegel, J.C. Interface pressure system to compare the functional performance of prosthetic sockets during the gait in people with trans-tibial amputation. Sensors 2020, 20, 7043. [Google Scholar] [CrossRef]
- Starholm, I.-M.; Gjovaag, T.; Mengshoel, A.M. Energy expenditure of transfemoral amputees walking on a horizontal and tilted treadmill simulating different outdoor walking conditions. Prosthet. Orthot. Int. 2010, 34, 184–194. [Google Scholar] [CrossRef]
- De Pauw, K.; Cherelle, P.; Roelands, B.; Lefeber, D.; Meeusen, R. The efficacy of the Ankle Mimicking Prosthetic Foot prototype 4.0 during walking: Physiological determinants. Prosthet. Orthot. Int. 2018, 42, 504–510. [Google Scholar] [CrossRef]
- Meier, M.R.; Hansen, A.H.; Gard, S.A.; McFadyen, A.K. Obstacle course: Users’ maneuverability and movement efficiency when using Otto Bock C-Leg, Otto Bock 3R60, and CaTech SNS prosthetic knee joints. J. Rehabil. Res. Res. Dev. 2012, 49, 583–596. [Google Scholar] [CrossRef] [PubMed]
- Lacraz, A.; Armand, S.; Turcot, K.; Carmona, G.; Stern, R.; Borens, O.; Assal, M. Comparison of the Otto Bock solid ankle cushion heel foot with wooden keel to the low-cost CR-Equipements™ solid ankle cushion heel foot with polypropylene keel: A randomized prospective double-blind crossover study assessing patient satisfaction and energy expenditure. Prosthet. Orthot. Int. 2017, 41, 258–265. [Google Scholar] [PubMed]
- Neptune, R.R.; Kautz, S.A.; Zajac, F.E. Contributions of the individual ankle plantar flexors to support, forward progression and swing initiation during walking. J. Biomech. 2001, 34, 1387–1398. [Google Scholar] [CrossRef]
- Zajac, F.E. Understanding muscle coordination of the human leg with dynamical simulations. J. Biomech. 2002, 35, 1011–1018. [Google Scholar] [CrossRef]
- Hubley-Kozey, C.; Deluzio, K.; Dunbar, M. Muscle co-activation patterns during walking in those with severe knee osteoarthritis. Clin. Biomech. 2008, 23, 71–80. [Google Scholar] [CrossRef]
- Wong, C.K.; Gibbs, W.; Chen, E.S. Use of the Houghton scale to classify community and household walking ability in people with lower-limb amputation: Criterion-related validity. Arch. Phys. Med. Rehabil. 2016, 97, 1130–1136. [Google Scholar] [CrossRef]
- Devlin, M.; Pauley, T.; Head, K.; Garfinkel, S. Houghton scale of prosthetic use in people with lower-extremity amputations: Reliability, validity, and responsiveness to change. Arch. Phys. Med. Rehabil. 2004, 85, 1339–1344. [Google Scholar] [CrossRef]
- Franchignoni, F.; Orlandini, D.; Ferriero, G.; Moscato, T.A. Reliability, validity, and responsiveness of the locomotor capabilities index in adults with lower-limb amputation undergoing prosthetic training. Arch. Phys. Med. Rehabil. 2004, 85, 743–748. [Google Scholar] [CrossRef] [PubMed]
- Salavati, M.; Mazaheri, M.; Khosrozadeh, F.; Mousavi, S.M.E.; Negahban, H.; Shojaei, H. The Persian version of locomotor capabilities index: Translation, reliability and validity in individuals with lower limb amputation. Qual. Life Res. 2011, 20, 1–7. [Google Scholar] [CrossRef]
- Ranker, A.; Gutenbrunner, C.; Eckhardt, I.; Giordano, A.; Burger, H.; Franchignoni, F. Rasch validation and comparison of the German versions of the Locomotor Capabilities Index-5 and Prosthetic Mobility Questionnaire 2.0 in lower-limb prosthesis users. Int. J. Rehabil. Res. 2021, 44, 233–240. [Google Scholar] [CrossRef]
- Franchignoni, F.; Giordano, A.; Ferriero, G.; Orlandini, D.; Amoresano, A.; Perucca, L. Measuring mobility in people with lower limb amputation: Rasch analysis of the mobility section of the prosthesis evaluation questionnaire. J. Rehabil. Med. 2007, 39, 138–144. [Google Scholar] [CrossRef] [PubMed]
- Kahle, J.T.; Highsmith, M.J.; Hubbard, S.L. Comparison of nonmicroprocessor knee mechanism versus C-Leg on Prosthesis Evaluation Questionnaire, stumbles, falls, walking tests, stair descent, and knee preference. J. Rehabil. Res. Dev. 2008, 45, 1. [Google Scholar] [CrossRef] [PubMed]
- Coleman, K.L.; Boone, D.A.; Laing, L.S.; Mathews, D.E.; Smith, D.G. Quantification of prosthetic outcomes: Elastomeric gel liner with locking pin suspension versus polyethylene foam liner with neoprene sleeve suspension. J. Rehabil. Res. Dev. 2004, 41, 591–602. [Google Scholar] [CrossRef] [PubMed]
- Baars, E.C.; Schrier, E.; Dijkstra, P.U.; Geertzen, J.H. Prosthesis satisfaction in lower limb amputees: A systematic review of associated factors and questionnaires. Medicine 2018, 97, e12296. [Google Scholar] [CrossRef]
- Berke, G.M.; CP, F.; L-CPO, J.H.; Nguyen, V. Comparison of satisfaction with current prosthetic care in veterans and servicemembers from Vietnam and OIF/OEF conflicts with major traumatic limb loss. J. Rehabil. Res. Dev. 2010, 47, 361. [Google Scholar] [CrossRef]
- Dillingham, T.R.; Pezzin, L.E.; MacKenzie, E.J.; Burgess, A.R. Use and satisfaction with prosthetic devices among persons with trauma-related amputations: A long-term outcome study. Am. J. Phys. Med. Rehabil. 2001, 80, 563–571. [Google Scholar] [CrossRef]
- Miller, M.J.; Morris, M.A.; Magnusson, D.M.; Putnam, K.; Cook, P.F.; Schenkman, M.L.; Christiansen, C.L. Psychosocial factors influence physical activity after dysvascular amputation: A convergent mixed-methods study. PMR 2021, 13, 737–745. [Google Scholar] [CrossRef]
- Bunce, D.J.; Breakey, J.W. The impact of C-Leg® on the physical and psychological adjustment to transfemoral amputation. JPO J. Prosthet. Orthot. 2007, 19, 7–14. [Google Scholar] [CrossRef]
- Buis, A.W.; Dumbleton, T.; Murray, K.D.; McHugh, B.F.; McKay, G.; Sexton, S. Measuring the daily stepping activity of people with transtibial amputation using the ActivPAL™ activity monitor. JPO J. Prosthet. Orthot. 2014, 26, 43–47. [Google Scholar] [CrossRef]
- Beisheim, E.H.; Arch, E.S.; Horne, J.R.; Sions, J.M. Performance-based outcome measures are associated with cadence variability during community ambulation among individuals with a transtibial amputation. Prosthet. Orthot. Int. 2020, 44, 215–224. [Google Scholar] [CrossRef]
- Fleming, A.; Stafford, N.; Huang, S.; Hu, X.; Ferris, D.P.; Huang, H.H. Myoelectric control of robotic lower limb prostheses: A review of electromyography interfaces, control paradigms, challenges and future directions. J. Neural Eng. 2021, 18, 041004. [Google Scholar] [CrossRef] [PubMed]
- Brown, B.J.; Iorio, M.L.; Klement, M.; Conti Mica, M.R.; El-Amraoui, A.; O’Halloran, P.; Attinger, C.E. Outcomes after 294 transtibial amputations with the posterior myocutaneous flap. Int. J. Low. Extrem. Wounds 2014, 13, 33–40. [Google Scholar] [CrossRef] [PubMed]
- Huang, S.; Huang, H. Voluntary control of residual antagonistic muscles in transtibial amputees: Feedforward ballistic contractions and implications for direct neural control of powered lower limb prostheses. IEEE Trans. Neural Syst. Rehabil. Eng. 2018, 26, 894–903. [Google Scholar] [CrossRef]
- Ha, K.H.; Varol, H.A.; Goldfarb, M. Volitional control of a prosthetic knee using surface electromyography. IEEE Trans. Biomed. Eng. 2010, 58, 144–151. [Google Scholar] [CrossRef]
- Huang, H.; Zhang, F.; Hargrove, L.J.; Dou, Z.; Rogers, D.R.; Englehart, K.B. Continuous locomotion-mode identification for prosthetic legs based on neuromuscular–mechanical fusion. IEEE Trans. Biomed. Eng. 2011, 58, 2867–2875. [Google Scholar] [CrossRef]
- Miller, J.D.; Beazer, M.S.; Hahn, M.E. Myoelectric walking mode classification for transtibial amputees. IEEE Trans. Biomed. Eng. 2013, 60, 2745–2750. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.-H.; Oh, J.-H. Development of an above knee prosthesis using MR damper and leg simulator. In Proceedings of the Proceedings 2001 ICRA. IEEE International Conference on Robotics and Automation (Cat. No. 01CH37164), Seoul, Republic of Korea, 21–26 May 2001; pp. 3686–3691. [Google Scholar]
- Underwood, H.A.; Tokuno, C.D.; Eng, J.J. A comparison of two prosthetic feet on the multi-joint and multi-plane kinetic gait compensations in individuals with a unilateral trans-tibial amputation. Clin. Biomech. 2004, 19, 609–616. [Google Scholar] [CrossRef]
- Berry, D. Microprocessor prosthetic knees. Phys. Med. Rehabil. Clin. 2006, 17, 91–113. [Google Scholar] [CrossRef]
- Xu, L.; Wang, D.-H.; Fu, Q.; Yuan, G.; Hu, L.-Z. A novel four-bar linkage prosthetic knee based on magnetorheological effect: Principle, structure, simulation and control. Smart Mater. Struct. 2016, 25, 115007. [Google Scholar] [CrossRef]
- Rochlitz, B.; Pammer, D. Design and analysis of 3D printable foot prosthesis. Period. Polytech. Mech. Eng. 2017, 61, 282–287. [Google Scholar] [CrossRef]

| Number of Publications | Centrality | Country |
|---|---|---|
| 774 | 0.51 | USA |
| 150 | 0.22 | UNITED KINGDOM |
| 112 | 0.06 | GERMANY |
| 104 | 0.25 | ITALY |
| 104 | 0.05 | PRC |
| 79 | 0.15 | CANADA |
| 74 | 0.07 | THE NETHERLANDS |
| 73 | 0.10 | FRANCE |
| 69 | 0.05 | SWITZERLAND |
| 59 | 0.01 | INDIA |
| Number of Publications | Centrality | Name of Institution |
|---|---|---|
| 84 | 0.08 | Northwestern University |
| 60 | 0.05 | University of Washington |
| 31 | 0.01 | University of Michigan |
| 23 | 0.03 | Brooke Army Medical Center |
| 22 | 0.01 | Duke University |
| 20 | 0.00 | The University of Texas at Austin |
| 18 | 0.02 | Massachusetts Institute of Technology |
| 17 | 0.03 | Georgia Institute of Technology |
| 17 | 0.00 | Vrije Universiteit Brussel |
| 16 | 0.01 | Jesse Brown VA Medical Center |
| Rank | Journal | Number of Publications | % of Total Number of Publications | Country | Impact Factor (2022) | H-Index (2022) |
|---|---|---|---|---|---|---|
| 1 | Prosthetics and Orthotics International | 151 | 8.26 | UK | 1.672 | 55 |
| 2 | Foot and Ankle International | 85 | 4.65 | USA | 3.569 | 114 |
| 3 | Journal of Foot and Ankle Surgery | 67 | 3.67 | USA | 1.345 | 70 |
| 4 | Gait and Posture | 62 | 3.39 | Ireland | 2.746 | 156 |
| s | Journal of Biomechanics | 58 | 3.17 | UK | 2.789 | 208 |
| 6 | Journal of Rehabilitation Research and Development | 56 | 3.06 | USA | 1.277 | 108 |
| 7 | IEEE Transactions on Neural Systems and Rehabilitation Engineering | 53 | 2.90 | USA | 4.528 | 148 |
| 8 | Clinical Biomechanics | 48 | 2.63 | UK | 2.034 | 135 |
| 9 | PLoS ONE | 40 | 2.19 | USA | 3.752 | 367 |
| 10 | Foot and Ankle Surgery | 38 | 2.08 | UK | 2.840 | 43 |
| 11 | Journal of NeuroEngineering and Rehabilitation | 32 | 1.75 | UK | 5.208 | 102 |
| 12 | Journal of Bone and Joint Surgery American Volume | 31 | 1.70 | USA | 6.558 | 274 |
| 13 | Archives of Physical Medicine and Rehabilitation | 30 | 1.64 | USA | 4.060 | 197 |
| 14 | Journal of Biomechanical Engineering-Transactions of the ASME | 28 | 1.53 | USA | 1.899 | 131 |
| 15 | Sensors | 26 | 1.42 | Switzerland | 3.847 | 196 |
| References | Year | Strength | Begin | End | 2000–2022 |
|---|---|---|---|---|---|
| GITTER A, 1991, AM J PHYS MED REHAB, V70, P142, https://doi.org/10.1097/00002060-199106000-00006 | 1991 | 14.04 | 2000 | 2012 | ▃▃▃▃▃▃▃▃▃▃▃▃▃▂▂▂▂▂▂▂▂▂▂ |
| TORBURN L, 1990, JOURNAL OF REHABILITATION RESEARCH AND DEVELOPMENT, V27, P369, https://doi.org/10.1682/JRRD.1990.10.0369 | 1990 | 13.13 | 2000 | 2013 | ▃▃▃▃▃▃▃▃▃▃▃▃▃▃▂▂▂▂▂▂▂▂▂ |
| LEHMANN JF, 1993, ARCH PHYS MED REHAB, V74, P1225, https://doi.org/10.1016/S0003-9993(23)00022-9 | 1993 | 11.47 | 2000 | 2010 | ▃▃▃▃▃▃▃▃▃▃▃▂▂▂▂▂▂▂▂▂▂▂▂ |
| LEHMANN JF, 1993, ARCH PHYS MED REHAB, V74, P853, https://doi.org/10.1016/0003-9993(93)90013-Z | 1993 | 9.95 | 2000 | 2006 | ▃▃▃▃▃▃▃▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂ |
| POWERS CM, 1994, ARCH PHYS MED REHAB, V75, P825, https://doi.org/10.1016/0003-9993(94)90146-5 | 1994 | 9.86 | 2000 | 2012 | ▃▃▃▃▃▃▃▃▃▃▃▃▃▂▂▂▂▂▂▂▂▂▂ |
| SNYDER RD, 1995, J REHABIL RES DEV, V32, P309 | 1995 | 9.67 | 2000 | 2010 | ▃▃▃▃▃▃▃▃▃▃▃▂▂▂▂▂▂▂▂▂▂▂▂ |
| ARYA AP, 1995, PROSTHET ORTHOT INT, V19, P37, https://doi.org/10.3109/03093649509078230 | 1995 | 7.51 | 2000 | 2008 | ▃▃▃▃▃▃▃▃▃▂▂▂▂▂▂▂▂▂▂▂▂▂▂ |
| POSTEMA K, 1997, PROSTHET ORTHOT INT, V21, P28, https://doi.org/10.3109/03093649709164527 | 1997 | 7.37 | 2000 | 2004 | ▃▃▃▃▃▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂ |
| KADABA MP, 1990, J ORTHOP RES, V8, P383, https://doi.org/10.1002/jor.1100080310 | 1990 | 8.50 | 2004 | 2010 | ▂▂▂▂▃▃▃▃▃▃▃▂▂▂▂▂▂▂▂▂▂▂▂ |
| ANDERSON T, 2003, J BONE JOINT SURG AM, V85A, P1321, https://doi.org/10.2106/00004623-200307000-00019 | 2003 | 7.66 | 2006 | 2014 | ▂▂▂▂▂▂▃▃▃▃▃▃▃▃▃▂▂▂▂▂▂▂▂ |
| HANSEN AH, 2006, PROSTHET ORTHOT INT, V30, P286, https://doi.org/10.1080/03093640600816982 | 2006 | 10.62 | 2008 | 2012 | ▂▂▂▂▂▂▂▂▃▃▃▃▃▂▂▂▂▂▂▂▂▂▂ |
| BONNIN M, 2004, CLIN ORTHOP RELAT R, V0, PP6, https://doi.org/10.1097/01.blo.0000132407.75881.a0 | 2004 | 8.27 | 2009 | 2015 | ▂▂▂▂▂▂▂▂▂▃▃▃▃▃▃▃▂▂▂▂▂▂▂ |
| SILVERMAN AK, 2008, GAIT POSTURE, V28, P602, https://doi.org/10.1016/j.gaitpost.2008.04.005 | 2008 | 9.51 | 2011 | 2012 | ▂▂▂▂▂▂▂▂▂▂▂▃▃▂▂▂▂▂▂▂▂▂▂ |
| VALDERRABANO V, 2004, CLIN ORTHOP RELAT R, V0, PP47, https://doi.org/10.1097/01.blo.0000132245.18548.09 | 2004 | 8.03 | 2011 | 2015 | ▂▂▂▂▂▂▂▂▂▂▂▃▃▃▃▃▂▂▂▂▂▂▂ |
| HITT J, 2009, IND ROBOT, V36, P441, https://doi.org/10.1108/01439910910980169 | 2009 | 9.92 | 2013 | 2017 | ▂▂▂▂▂▂▂▂▂▂▂▂▂▃▃▃▃▃▂▂▂▂▂ |
| WINTER DA, 1983, CLIN ORTHOP RELAT R, V0, P147 | 1983 | 8.07 | 2013 | 2018 | ▂▂▂▂▂▂▂▂▂▂▂▂▂▃▃▃▃▃▃▂▂▂▂ |
| HSU MJ, 2006, ARCH PHYS MED REHAB, V87, P123, https://doi.org/10.1016/j.apmr.2005.07.310 | 2006 | 7.93 | 2013 | 2018 | ▂▂▂▂▂▂▂▂▂▂▂▂▂▃▃▃▃▃▃▂▂▂▂ |
| FEY NP, 2011, CLIN BIOMECH, V26, P1025, https://doi.org/10.1016/j.clinbiomech.2011.06.007 | 2011 | 7.80 | 2016 | 2020 | ▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▃▃▃▃▃▂▂ |
| QUESADA RE, 2016, J BIOMECH, V49, P3452, https://doi.org/10.1016/j.jbiomech.2016.09.015 | 2016 | 8.64 | 2017 | 2022 | ▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▃▃▃▃▃▃ |
| ADAMCZYK PG, 2017, HUM MOVEMENT SCI, V54, P154, https://doi.org/10.1016/j.humov.2017.04.005 | 2017 | 7.50 | 2018 | 2022 | ▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▃▃▃▃▃ |
| SHEPHERD MK, 2017, IEEE T NEUR SYS REH, V25, P2375, https://doi.org/10.1109/TNSRE.2017.2750113 | 2017 | 12.95 | 2019 | 2022 | ▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▃▃▃▃ |
| HUANG H, 2011, IEEE T BIO-MED ENG, V58, P2867, https://doi.org/10.1109/TBME.2011.2161671 | 2011 | 9.71 | 2019 | 2022 | ▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▃▃▃▃ |
| TUCKER MR, 2015, J NEUROENG REHABIL, V12, P0, https://doi.org/10.1186/1743-0003-12-1 | 2015 | 8.32 | 2019 | 2022 | ▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▃▃▃▃ |
| GLANZER EM, 2018, IEEE T NEUR SYS REH, V26, P2351, https://doi.org/10.1109/TNSRE.2018.2877962 | 2018 | 9.81 | 2020 | 2022 | ▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▃▃▃ |
| LAWSON BE, 2014, IEEE ROBOT AUTOM MAG, V21, P70, https://doi.org/10.1109/MRA.2014.2360303 | 2014 | 8.44 | 2020 | 2022 | ▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▂▃▃▃ |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shi, Q.-Q.; Yick, K.-L.; Wu, J.; Huang, X.; Tse, C.-Y.; Chan, M.-K. A Scientometric Analysis and Visualization of Prosthetic Foot Research Work: 2000 to 2022. Bioengineering 2023, 10, 1138. https://doi.org/10.3390/bioengineering10101138
Shi Q-Q, Yick K-L, Wu J, Huang X, Tse C-Y, Chan M-K. A Scientometric Analysis and Visualization of Prosthetic Foot Research Work: 2000 to 2022. Bioengineering. 2023; 10(10):1138. https://doi.org/10.3390/bioengineering10101138
Chicago/Turabian StyleShi, Qiu-Qiong, Kit-Lun Yick, Jinlong Wu, Xujia Huang, Chi-Yung Tse, and Mei-Ki Chan. 2023. "A Scientometric Analysis and Visualization of Prosthetic Foot Research Work: 2000 to 2022" Bioengineering 10, no. 10: 1138. https://doi.org/10.3390/bioengineering10101138
APA StyleShi, Q.-Q., Yick, K.-L., Wu, J., Huang, X., Tse, C.-Y., & Chan, M.-K. (2023). A Scientometric Analysis and Visualization of Prosthetic Foot Research Work: 2000 to 2022. Bioengineering, 10(10), 1138. https://doi.org/10.3390/bioengineering10101138







