Abstract
Probing the cortic ospinal tract integrity by transcranial magnetic stimulation (TMS) could help to understand the neurophysiological correlations of multiple sclerosis (MS) symptoms. Therefore, the study objective was, first, to investigate TMS measures (resting motor threshold-RMT, motor evoked potential (MEP) latency, and amplitude) of corticospinal tract integrity in people with relapsing-remitting MS (pwMS). Then, the study examined the conformity of TMS measures with clinical disease-related (Expanded Disability Status Scale—EDSS) and magnetic resonance imaging (MRI) results (lesion count) in pwMS. The e-field navigated TMS, MRI, and EDSS data were collected in 23 pwMS and compared to non-clinical samples. The results show that pwMS differed from non-clinical samples in MEP latency for upper and lower extremity muscles. Also, pwMS with altered MEP latency (prolonged or absent MEP response) had higher EDSS, general and pyramidal, functional scores than pwMS with normal MEP latency finding. Furthermore, the RMT intensity for lower extremity muscles was predictive of EDSS functional pyramidal scores. TMS/MEP latency findings classified pwMS as the same as EDSS functional pyramidal scores in 70–83% of cases and were similar to the MRI results, corresponding to EDSS functional pyramidal scores in 57–65% of cases. PwMS with altered MEP latency differed from pwMS with normal MEP latency in the total number of lesions in the brain corticospinal and cervical corticospinal tract. The study provides preliminary results on the correspondence of MRI and TMS corticospinal tract evaluation results with EDSS functional pyramidal score results in MS.
1. Introduction
Multiple sclerosis (MS) is an inflammatory autoimmune-mediated disease of the central nervous system (CNS) characterized by white matter demyelinating lesions and neuronal degeneration. The primary pathological event is demyelination, with destruction and loss of axons correlating with a permanent functional deficit [1,2,3,4]. However, pathophysiological correlates and their relation with clinical findings and symptoms are still not elucidated. Therefore, this suggests a need to detect subclinical markers, such as neurophysiological markers, that could identify pathological events involved in individuals with MS at different stages of the disease [5,6,7].
Using navigated transcranial magnetic stimulation (TMS) in probing corticospinal excitability as a marker of functional integrity of the primary motor cortex (M1), corticospinal axonal pathway, and peripheral signaling function to target muscles could help in further understanding the underlying pathophysiological mechanisms of MS. Recent findings proposed that applying TMS as an adjuvant para-clinical instrument could help to identify biomarkers of the MS disease [8], serving as a biomarker of MS disability [9]. An association between the pathophysiological mechanisms of MS (demyelination and axonal loss) and TMS measures (e.g., low amplitudes and prolonged latencies of motor evoked potentials (MEP), increased resting motor threshold (RMT), and increased central motor conduction time) have been reported [6]. Alterations in cortical excitatory and inhibitory processes in MS assessed with TMS are noticeable early in the disease progress, during relapses, and later during the disease progression [6,7,10]. Also, [6,9], from the clinical point of view, diverse quantitative magnetic resonance imaging (MRI) indices (i.e., lesion volume, T2WI value) have been proposed as structural biomarkers of MS. However, the correlations between individual MRI measures and the EDSS have been modest and varying.
The present study aims to (1) investigate TMS measures (resting motor threshold-RMT, motor evoked potential (MEP) latency, MEP amplitude) of corticospinal tract integrity in people with relapsing-remitting MS (pwMS), and (2) to preliminarily assess the conformity of TMS measures with clinical disease-related status (EDSS score) and magnetic resonance imaging (MRI) results (lesion count) in pwMS [11,12,13]. The following hypotheses were settled: (1) pwMS with altered (prolonged or absent) MEP latency will have higher EDSS scores compared to non-clinical samples, (2) pwMS with altered MEP latency will differ from non-clinical samples in the total number of lesions in the brain cortico-spinal and cervical corticospinal tract, and (3) the study will provide preliminary results on correspondence between TMS corticospinal integrity measures (MEP latency findings) and MRI corticospinal tract evaluation (lesion count) with EDSS functional pyramidal scores.
2. Materials and Methods
2.1. Participants and Study Design
This is a cross-sectional study of 23 pwMS treated with teriflunomide (Aubagio) medication for ≥12 months. None of the pwMS experienced a relapse 3 months before participating in this study. Non-clinical samples from previous studies were used as a control for comparison with pwMS on TMS [14,15,16,17,18,19]. Also, the following exclusion criteria were applied: immunomodulatory drug intake other than teriflunomide, history of diseases of the central or peripheral nervous system (other than relapsing-remitting MS), history of psychiatric diseases, drug or alcohol abuse, and using a TMS screening questionnaire, presence of any contraindication for TMS, for which the safety screening was applied [20].
2.2. Clinical Disease-Related Assessment Measures
Neurological examination and medical history included the following measures: the EDSS score and EDSS functional pyramidal score total and for right and left upper and lower extremities [21], MS disease duration, age at onset of MS, drug intake duration, and comorbidities other than MS.
The electroneurographic (ENG) assessment was performed as an additional tool to exclude possible peripheral neurological events in pwMS using the Medelec-Synergy instrument (Oxford Instrument Co., Surrey, UK) [22]. ENG assessment of lower and upper extremities included the following measures for motor nerves (n. medianus, n. ulnaris, n. peroneus, n. tibialis): distal motor latency, compound muscle action potential amplitude, conduction velocity, and F-wave latency; and for sensory nerves (n. medianus, n. ulnaris, n. suralis): sensory nerve action potential amplitude, sensory nerve action potential latency, and conduction velocity.
2.3. Radiological Magnetic Resonance Imaging (MRI) Assessment and Image Evaluation
Scans were acquired on a MR 1.5T system (Avanto, Siemens, Medical Systems, Best, Germany) using a 12-channel phased array head coil. The sequences included in the brain scan protocol were 3D T1-weighted images, axial T2-weighted images, and fluid-attenuated inversion recovery (FLAIR) images in the axial and sagittal plane, all used to identify brain lesions. Spinal cord sequences included sagittal T2-weighted images, sagittal turbo inversion recovery magnitude (TIRM) images, and axial T2 med images from C1 to C7 vertebral levels. MRIs were analyzed using Syngo.via software (Siemens Healthcare, Forchheim, Germany) equipped with a screen (1600 × 1200 pixel resolution). MRIs were analyzed by a senior radiology resident (AB) and supervised by an experienced neuroradiologist (KD) with 15 years of experience. Both were blinded to the TMS and EDSS results. Using the T2, FLAIR, TIRM, and T2 med images, specific locations of the corticospinal tract (CST) were visually examined, including subcortical white matter in the primary motor cortex (CST-M1), capsula interna, cerebral peduncles and ventral parts of the midbrain and pons (CST-M2) and ventral and lateral parts of the cervical spinal cord (CST-M3). For each subject, it was checked whether they had a lesion in any listed locations (CST-M1, CST-M2, CST-M3), the number of lesions, and whether the lesion was located on the left or right side. The McDonald’s criteria were consulted for the lesion count for the individual subject [11,12,13]. MRI images were used for the 3D reconstruction of individual brain anatomy (3D optical tracking unit of the manufacturer Polaris ® Vicra) with TMS (Nexstim NBS System 4 of the manufacturer Nexstim Plc., Helsinki, Finland).
2.4. Navigated Transcranial Magnetic Stimulation (TMS) Procedure
The magnetic stimulation was delivered using a biphasic single magnetic coil generating a biphasic pulse of a length of 289 µs. The eight-shaped coil with an inner winding diameter of 50 mm and an outer winding diameter of 70 mm was placed tangentially to the subject’s skull over the primary motor cortex (M1). The motor evoked potentials (MEPs) were recorded from the upper extremity muscles (abductor pollicis brevis—APB, abductor digiti minimi—ADM) and lower extremity muscles (tibialis anterior—TA, abductor hallucis—AH) with a pair of self-adhesive surface electrodes (Ambu ® Blue Sensor BR, BR-50-K/12 of manufacturer Ambu A/S) in a belly-tendon montage. Electrodes were attached to the electrode cable of the Nexstim electromyography (EMG) system with a 1.5 mm touch-proof female safety connector (DIN 42-802) and connected to a 6-channel EMG and one common ground EMG amplifier (external module) with TMS-artefact rejection circuitry. The coil was positioned tangentially to the central sulcus to ensure a posterior–anterior current direction over the primary motor cortex (M1). The lowest stimulation intensity used to elicit at least five positive MEP responses out of 10 trials, having peak-to-peak amplitudes larger than 50 µV, was defined as the resting motor threshold (RMT) intensity. When mapping lower extremity muscles (TA, AH) and applying 100% intensity of maximal stimulator output to obtain reliable MEPs, the MEPs with amplitudes slightly lower than 50 µV were collected for the analysis (10 trials). MEP latency and amplitude estimation were performed by a custom-made MATLAB script (R2021a) using an automatic algorithm developed by our research group [23].
2.5. Statistical Analysis
Statistical analyses were conducted using Excel 2013 and IBM SPSS Statistics Version 25. Participants’ characteristics were analyzed using descriptive statistics. Since skewness and kurtosis parameters did not indicate significant deviations from a normal distribution for most variables, the parametric statistic was used, except for EDSS, for which we used nonparametric statistics (stated in brackets). Groups were compared with Welch t-tests suitable for heterogeneous variances (Mann–Whitney U test). These included comparisons of pwMS to non-clinical samples from previous research [14,15,16,17,18,19] and of pwMS with altered MEP latency (prolonged MEP latency or absent MEP latency) with non-altered MEP latency findings (MEP response elicited and non-alterations in MEP observed). Further, correlation analyses were conducted on the whole pwMS sample using Pearson’s r coefficient (or Spearman rank-order correlation ρ). Also, correspondence in classification was tested with McNemar’s test. Finally, a p < 0.05 value for the significance was set and considered statistically significant.
3. Results
3.1. Patient Characteristics
Demographic, clinical, and disease-related characteristics of pwMS are summarized in Table 1. The study sample included 23 pwMS with a mean age of 41.65 (SD = 8.89) years. Most pwMS were women (60.87%), right-handed (91.3%), and with high school education (73.9%). The mean disease duration was 9.39 (SD = 5.73) years, and the median EDSS score was 2.5 (range 0–4). The average duration of immunomodulatory teriflunomide drug intake was 3.6 (SD = 1.66) years. In total, 43.5% of pwMS suffered from other chronic diseases. Average ENG values were in accordance with the referent values indicating no peripheral neurological events [22].

Table 1.
Demographic, clinical and disease-related characteristics.
3.2. TMS Measures
Fifteen out of 23 pwMS had altered MEP latency (prolonged or absent MEP) (65.2%), and eight subjects had normal MEP latency findings (MEP responses were elicited/present). Table 2 presents TMS measures (RMT, MEP latency, and MEP amplitude) for upper and lower extremity muscles. It can be observed that a significant difference was found for RMT between left and right hemisphere stimulation of APB (t(22) = 2.87, p = 0.009), which was higher for the right hemisphere (Mright = 47.00, Mleft = 40.26). The results of TMS measures (RMT, MEP latency, and MEP amplitude) for upper and lower extremity muscles for individual pwMS subjects divided into pwMS samples with altered MEP findings and pwMS with normal (non-altered) MEP findings are presented in Supplementary Table S1. When comparing TMS measures of the pwMS sample in the present study and non-clinical samples (Table 3) [14,15,16,17,18,19], significantly prolonged MEP latencies were found for all muscles (left: tAPB(23) = 4.94, p < 0.001; tADM(24) = 6.34, p < 0.001; tTA(16) = 6.12, p < 0.001; tAH(32) = 6.52, p < 0.001; right: tAPB(23) = 6.14, p < 0.001; tADM(24) = 7.15, p < 0.001; tTA(15) = 7.64, p < 0.001; tAH(30) = 4.96, p < 0.001) in the pwMS sample in the current study. Further, significantly prolonged MEP latencies were also found for all muscles when comparing non-clinical samples with pwMS with altered MEP latency findings (Table 3). Figure 1 presents single trial MEP latencies from upper and lower extremity muscles for an MS subject (No. 3) having four lesions in the corticospinal pathway (CST-M3), two lesions on the left and two lesions on the right with the positioning of positive, stimulating spots over the M1 for the representation of the upper (Figure 1A, C) and lower extremities (Figure 1B, D). Figure 2 presents all MEP latency trials from upper and lower extremity muscles for subject No. 3. Figure 3 depicts MEP responses from upper extremity muscles, and Figure 4 presents MEP responses from lower extremity muscles for all pwMS with altered MEP findings.

Table 2.
Results of TMS measures (RMT, MEP latency, and MEP amplitude) for upper and lower extremity muscles.

Table 3.
Comparison of results of TMS measures between pwMS in the present study and non-clinical samples.
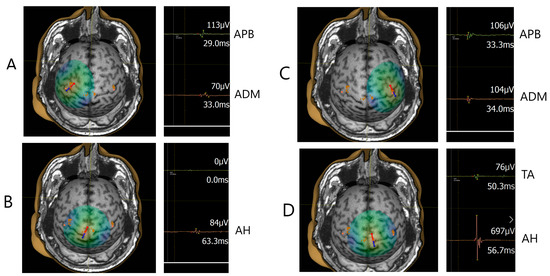
Figure 1.
Mapping of the M1 for the representation of the upper (A,C) and lower extremities (B,D) and registration of single trial MEP response from the muscles of the upper (APB, ADM) and lower extremities (TA, AH) in the male subject (No. 3). The arrow indicates the position of the coil perpendicular to the central sulcus and point of stimulation. Values of the MEP peak-to-peak amplitude (µV) and MEP latency (ms) are indicated for each MEP trial.
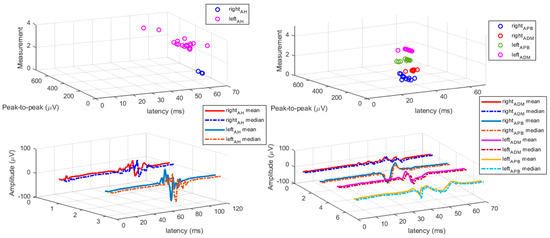
Figure 2.
All MEP responses from upper and lower extremity muscles for male subject No. 3. Left: MEP responses elicited for lower extremity AH muscle; left upper: MEP responses for left and right AH muscle; left below: mean and median for left and right MEPs for AH muscle. Right: MEP responses elicited for upper extremity APB and ADM muscle; right upper: MEP responses for left and right APB and ADM muscle; right below: mean and median for left and right MEPs for APB and ADM muscle. MEP peak-to-peak amplitude is expressed in microvolts (µV), and MEP latency in milliseconds (ms).
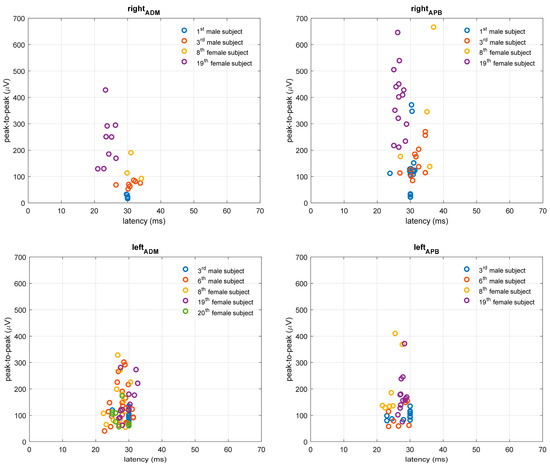
Figure 3.
MEP responses for upper extremity APB and ADM muscles in pwMS with altered TMS finding. MEP peak-to-peak amplitude is expressed in microvolts (µV), and latency in milliseconds (ms).
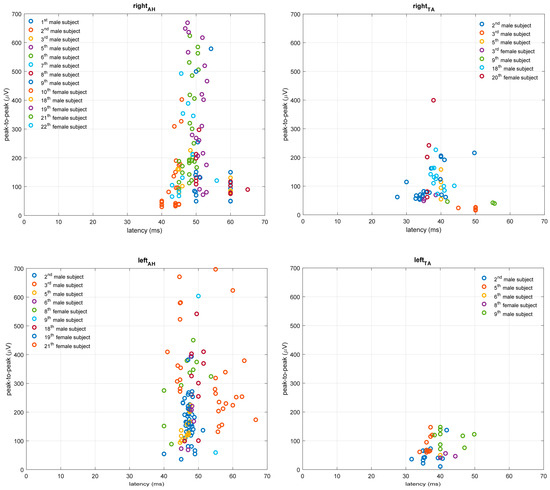
Figure 4.
MEP responses for lower extremity TA and AH muscles in pwMS with altered TMS finding. MEP peak-to-peak amplitude is expressed in microvolts (µV), and MEP latency in milliseconds (ms).
3.3. TMS, EDSS, and MRI Correspondence Results
PwMS with altered MEP finding (prolonged MEP latency or absent MEP) had higher EDSS score [Median TMS-A = 3.5 (range 0–4), Median TMS-N = 0.5(0–2.5), Mann–Whitney U = 19.5, p = 0.008] and EDSS functional pyramidal score [Median TMS-A = 3.0(0–3.5); Median TMS-N = 0.5(0–2) Mann–Whitney U = 18, p = 0.005], as well as for both lower extremities (right/left: Mann–Whitney U = 15.5/27, p = 0.002/0.034), but not upper extremities (right/left: Mann–Whitney U = 51/40, p = 0.591/0.213). Results indicate a significant correlation between MEP latency of lower extremity AH (ρ = 0.548, p < 0.01) and TA (ρ = 0.543, p < 0.05) muscle of the right leg and EDSS functional pyramidal score for the right leg. Also, a significant correlation was observed between RMT intensity for mapping representations for lower extremity TA and AH muscles over the right hemisphere and EDSS score (TA/AH, ρ = 0.615, p < 0.01; AH, ρ = 0.642, p < 0.01), EDSS functional pyramidal score (TA, ρ = 0.593, p < 0.01; AH, ρ = 0.654, p < 0.01), EDSS functional pyramidal score for the right leg (TA, ρ = 0.509, p < 0.05; AH, ρ = 0.560, p < 0.01) and EDSS functional pyramidal score for the left leg (TA, ρ = 0.615, p < 0.01; AH, ρ = 0.578, p < 0.01). Next, a significant correlation was observed between RMT intensity for mapping representations for AH muscle over the left hemisphere and EDSS score (ρ = 0.462, p < 0.05), EDSS functional pyramidal score (ρ = 0.480, p < 0.05), and EDSS functional pyramidal score for the right leg (ρ = 0.514, p < 0.05). PwMS with altered MEP latency differed from those with non-altered MEP latency finding on the total number of lesions in the brain corticospinal (t(11) = 3.05, p = 0.01) and in the cervical corticospinal (right: t(19) = 2.32, p = 0.03; left: t(19) = 2.23, p = 0.04) tract. A number of lesions in the right corticospinal tract (CST-M3) correlated with the EDSS functional pyramidal score for the right leg (ρ = 0.425, p < 0.05). Table 4 presents the lesion count according to McDonald’s criteria and MRI lesion evaluation of the corticospinal tract.

Table 4.
Number of lesions according to McDonald criteria and lesion evaluation of corticospinal tract.
The correspondence of EDSS pyramidal functional scoring of each extremity with classifications based on TMS corticospinal tract integrity and MRI on corticospinal tract evaluation is presented in Table 5. It can be observed that TMS findings classified pwMS as the same as EDSS pyramidal functional score in 70–83% of cases and MRI in 57–65% of cases. Moreover, McNemar’s test indicated TMS and MRI showed equal correspondence with the EDSS pyramidal functional score for the right arm’s muscles and for the lower extremity muscles. For the left arm muscles, McNemar’s test indicated significantly better correspondence of TMS (compared to MRI) with EDSS score (χ2 = 3.12, p = 0.047). Therefore, TMS was more accurate (83%) for the left arm in replicating the EDSS pyramidal functional score than MRI (57%). The correspondence of EDSS general/pyramidal with classifications based on TMS corticospinal tract integrity and MRI on corticospinal tract evaluation is presented in Table 6.

Table 5.
Correspondence of EDSS pyramidal functional score classifications with classifications based on TMS and MRI corticospinal tract results for lower and upper extremity muscles.

Table 6.
Correspondence of EDSS classifications (general and pyramid score) with classifications based on TMS and MRI corticospinal tract results.
4. Discussion
In this cross-sectional study, we found prolongations in MEP latency or absence of MEP response in lower and upper extremity muscles in 65.2% of pwMS. The study results correspond to previous findings on the correlation between EDSS scores and TMS measures (MEP latency and RMT intensity) [6,9]. The association between neurophysiological TMS measures of cortical excitability and clinical results (EDSS) could indicate a predominant role of white matter lesions in the pathogenesis of these changes, especially of the corticospinal pathway and corpus callosum [6]. Further, the present study provides preliminary results on correspondence between TMS corticospinal integrity measures (MEP latency findings) and MRI corticospinal tract evaluations (lesion count) with EDSS functional pyramidal scores.
From the clinical point of view, MRI is a sensitive test for diagnosing and assessing disease progression in pwMS and is often used to monitor therapeutic efficacy. However, the poor association between conventional MRI measures of tissue damage, such as T1-weighted or T2-weighted lesion load, and clinical disability measured with EDSS has been reported previously [24,25,26,27,28]. On the other hand, it is pointed out that TMS is not used as a standard technique in clinical assessment of pwMS and is currently recommended to monitor the integrity of the corticospinal tract in clinical follow-up [29]. The findings from the present study point to the practical value of TMS mapping of the corticospinal tract integrity and estimating the EDSS functional pyramidal score, in addition to the overall EDSS score.
Finally, there are limitations in the present study. The control data (non-clinical samples) from previous reports were used [14,15,16,17,18,19,30]. Due to the unavailability of diffusion tensor imaging (DTI) at our institution, fiber tractography, and automated atlases [31,32], we were limited in the identification and reconstruction of the corticospinal tract by applying MRI lesion count [28]. The MEP peak-to-peak amplitude and RMT could not be properly compared with non-clinical samples, since most of the studies reported MEP latency average results (including mean, standard deviation, and the number of subjects). Fourth, a larger sample would allow more power for our conclusions, i.e., less chance for so-called Type I error and additional statistical analyses. Furthermore, although MEP latency measures corresponded with clinical scores (EDSS), further validation of MEP measurements is needed regarding their validity, reliability, and sensitivity in longitudinal study before being routinely used in clinical trials in pwMS [33]. Also, EDSS is a standard tool for functional disability inspection applied by a physician and requires an in-person assessment and suffers from having high inter- and intra-rater variability, particularly at the lower disability levels [34]. In our study, the EDSS evaluation of pwMS was performed by an experienced physician for all patients to avoid interrater variability. Other functional tests like the 6 min walk-test (6MWT) or 10 m walk-test (10MWT), could be assessed with EDSS to evaluate clinically relevant disability status with TMS mapping of the corticospinal tract integrity in pwMS [5].
The advantage of the present study is the application of e-field navigated TMS in evaluating corticospinal tract integrity and its correspondence with the EDSS functional pyramidal score (general and for each extremity) in pwMS. Recent reports [35] suggest the use of e-field navigated TMS to improve the accuracy of corticospinal tract integrity testing by providing more objective correspondence of neurophysiological (e-field navigated TMS) and clinical (EDSS and MRI) classifications.
5. Conclusions
PwMS with prolonged or absent MEP response had higher EDSS, general and pyramidal, functional scores than pwMS with normal MEP latency findings. Further, RMT intensity for lower extremity muscles was predictive of EDSS functional pyramidal scores. The present study provides preliminary findings on the similar correspondence of TMS and MRI evaluations of corticospinal tract integrity results with EDSS pyramidal functional score classifications. The study findings point to the clinical value of the neurophysiological TMS methodology in evaluating corticospinal tract integrity as an additional armamentarium to EDSS, a standard clinical, functional disability instrument. Ultimately, TMS has the potential advantage of being a continuous variable compared to the discrete nature of EDSS; however, the usefulness of TMS mapping of corticospinal tract integrity in this regard can only be determined through longitudinal studies.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/bioengineering10101118/s1, Table S1: TMS measures (RMT, MEP latency, and MEP amplitude) for individual pwMS subjects.
Author Contributions
Conceptualization, M.R.V., N.R.M., A.M. (Anita Markotić), S.P., A.B. and A.Ć.K.; methodology, A.Ć.K., S.P., A.B., U.M., K.D. and A.B.; software, A.J., U.M. and J.Š.; validation, U.M. and A.J.; formal analysis, M.R.V., U.M., A.J. and A.Ć.K.; investigation, M.R.V., N.R.M., A.M. (Angela Mastelić), A.B., S.P., K.D. and A.Ć.K.; resources, A.M. (Anita Markotić), N.R.M. and Z.Đ.; data curation, M.R.V., A.Ć.K. and A.M. (Angela Mastelić); writing—original draft preparation, M.R.V. and A.Ć.K.; writing—review and editing, A.Ć.K., S.P., A.B., U.M., J.Š., A.J., A.M. (Angela Mastelić), K.D., A.M. (Anita Markotić), N.R.M. and Z.Đ.; visualization, M.R.V., J.Š., U.M. and A.J.; supervision, A.M. (Anita Markotić), Z.Đ., J.Š. and K.D.; project administration, M.R.V., Z.Đ. and A.M. (Angela Mastelić); funding acquisition, A.M. (Anita Markotić) and N.R.M. All authors have read and agreed to the published version of the manuscript.
Funding
This work is supported by Program funding of science for universities in the Republic of Croatia, the University of Split, Croatia.
Institutional Review Board Statement
The study procedure was approved by the University of Split, and University Hospital of Split research ethical committee board (Class: 003-08/21-03/0003, No: 2181-198-03-04-21-0039- April 2021 annex, and second annex Class: 003-08/22-03/003, No: 2181-198-03-04-22-0021) approved all aspects of the study protocol. The cross-sectional study registry name: “Biomarkers in Relapsing-Remitting Multiple Sclerosis (BioMS) URL (accessed on 1 July 2023): https://www.clinicaltrials.gov/ct2/show/NCT04604041?cond=Multiple+Sclerosis&cntry=HR&draw=2&rank=1, registration number (ClinicalTrials.gov Identifier: NCT04604041).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data are available with a granted proposal upon reasonable request.
Acknowledgments
We thank Meri Matijaca for her helpful advice and significant contribution to the manuscript’s preparation. The authors thank all participants for participating in the study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Lassmann, H.; Brück, W.; Lucchinetti, C. Heterogeneity of multiple sclerosis pathogenesis: Implications for diagnosis and therapy. Trends Mol. Med. 2001, 7, 115–121. [Google Scholar] [CrossRef]
- Pitteri, M.; Romualdi, C.; Magliozzi, R.; Monaco, S.; Calabrese, M. Cognitive impairment predicts disability progression and cortical thinning in MS: An 8-year study. Mult. Scler. J. 2017, 23, 848–854. [Google Scholar] [CrossRef] [PubMed]
- Filippi, M.; Brück, W.; Chard, D.; Fazekas, F.; Geurts, J.J.; Enzinger, C.; Hametner, S.; Kuhlmann, T.; Preziosa, P.; Rovira, A.; et al. Association between pathological and MRI findings in multiple sclerosis. Lancet Neurol. 2019, 18, 198–210. [Google Scholar] [CrossRef] [PubMed]
- Bar-Or, A.; Li, R. Cellular immunology of relapsing multiple sclerosis: Interactions, checks, and balances. Lancet Neurol. 2021, 20, 470–483. [Google Scholar] [CrossRef]
- Pisa, M.; Chieffo, R.; Giordano, A.; Gelibter, S.; Comola, M.; Comi, G.; Leocani, L. Upper limb motor evoked potentials as outcome measure in progressive multiple sclerosis. Clin. Neurophysiol. 2020, 131, 401–405. [Google Scholar] [CrossRef]
- Stampanoni Bassi, M.; Buttari, F.; Gilio, L.; Paolis, N.; Fresegna, D.; Centonze, D.; Lezzi, E. Inflammation and Corticospinal Functioning in Multiple Sclerosis: A TMS Perspective. Front. Neurol. 2020, 11, 566. [Google Scholar] [CrossRef]
- Hardmeier, M.; Schindler, C.; Kuhle, J.; Fuhr, P. Validation of Quantitative Scores Derived From Motor Evoked Potentials in the Assessment of Primary Progressive Multiple Sclerosis: A Longitudinal Study. Front. Neurol. 2020, 11, 735. [Google Scholar] [CrossRef] [PubMed]
- Chalah, M.A.; Palm, U.; Ayache, S.S. Editorial: Corticospinal Excitability in Patients With Multiple Sclerosis. Front. Neurol. 2021, 11, 635612. [Google Scholar] [CrossRef] [PubMed]
- Neva, J.L.; Lakhani, B.; Brown, K.E.; Wadden, K.P.; Mang, C.S.; Ledwell, N.H.M.; Borich, M.R.; Vavasour, I.M.; Laule, C.; Traboulsee, A.L.; et al. Multiple measures of corticospinal excitability are associated with clinical features of multiple sclerosis. Behav. Brain Res. 2016, 297, 187–195. [Google Scholar] [CrossRef] [PubMed]
- Mamoei, S.; Hvid, L.G.; Boye Jensen, H.; Zijdewind, I.; Stenager, E.; Dalgas, U. Neurophysiological impairments in multiple sclerosis-Central and peripheral motor pathways. Acta Neurol. Scand. 2020, 142, 401–417. [Google Scholar] [CrossRef]
- Filippi, M.; Rocca, M.A.; Ciccarelli, O.; De Stefano, N.; Evangelou, N.; Kappos, L.; Rovira, A.; Sastre-Garriga, J.; Tintorè, M.; Frederiksenet, J.L.; et al. MRI criteria for the diagnosis of multiple sclerosis: MAGNIMS consensus guidelines. Lancet Neurol. 2016, 15, 292–303. [Google Scholar] [CrossRef]
- Thompson, A.J.; Banwell, B.L.; Barkhof, F.; Carroll, W.M.; Coetzee, T.; Comi, G.; Correale, J.; Fazekas, F.; Filippi, M.; Freedman, M.S.; et al. Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol. 2018, 17, 162–173. [Google Scholar] [CrossRef] [PubMed]
- Wattjes, M.P.; Ciccarelli, O.; Reich, D.S.; Banwell, B.; de Stefano, N.; Enzinger, C.; Fazekas, F.; Filippi, M.; Frederiksen, J.; Gasperini, C.; et al. 2021 MAGNIMS-CMSC-NAIMS consensus recommendations on the use of MRI in patients with multiple sclerosis. Lancet Neurol. 2021, 20, 653–670. [Google Scholar] [CrossRef] [PubMed]
- Triggs, W.J.; Calvanio, R.; Macdonell, R.A.; Cros, D.; Chiappa, K.H. Physiological motor asymmetry in human handedness: Evidence from transcranial magnetic stimulation. Brain Res. 1994, 636, 270–276. [Google Scholar] [CrossRef]
- Eisen, A.A.; Shtybel, W. Clinical experience with transcranial magnetic stimulation. Muscle Nerve 1990, 13, 995–1011. [Google Scholar] [CrossRef] [PubMed]
- Macdonell, R.A.; Donnan, G.A. Magnetic cortical stimulation in acute spinal cord injury. Neurology 1995, 45, 303–306. [Google Scholar] [CrossRef]
- Claus, D. Central motor conduction: Method and normal results. Muscle Nerve 1990, 13, 1125–1132. [Google Scholar] [CrossRef]
- Cantone, M.; Lanza, G.; Vinciguerra, L.; Puglisi, V.; Ricceri, R.; Fisicaro, F.; Vagli, C.; Bella, R.; Ferri, R.; Pennisi, G.; et al. Age, Height, and Sex on Motor Evoked Potentials: Translational Data From a Large Italian Cohort in a Clinical Environment. Front. Hum. Neurosci. 2019, 13, 185. [Google Scholar] [CrossRef] [PubMed]
- Osei-Lah, A.D.; Mills, K.R. Optimising the detection of upper motor neuron function dysfunction in amyotrophic lateral sclerosis-a transcranial magnetic stimulation study. J. Neurol. 2004, 251, 1364–1369. [Google Scholar] [CrossRef] [PubMed]
- Rossi, S.; Hallett, M.; Rossini, P.M.; Pascual-Leone, A. Screening questionnaire before TMS: An update. Clin. Neurophysiol. 2011, 122, 1686. [Google Scholar] [CrossRef]
- Kurtzke, J.F. Rating neurologic impairment in multiple sclerosis: An expanded disability status scale (EDSS). Neurology 1983, 33, 1444–14452. [Google Scholar] [CrossRef]
- Preston, D.C.; Shapiro, B.E. Electromyography and Neuromuscular Disorders: Clinical-Electrophysiologic Correlations, 3rd ed.; Elsevier Inc.: Amsterdam, The Netherlands, 2013; ISBN 9781455726721. [Google Scholar]
- Šoda, J.; Rogić Vidaković, M.; Lorincz, J.; Jerković, A.; Vujović, I. Novel Latency Estimation Algorithm of Motor Evoked Potential Signals. IEEE Access 2020, 8, 193356–193374. [Google Scholar] [CrossRef]
- Chard, D.; Trip, S.A. Resolving the clinico-radiological paradox in multiple sclerosis. F1000Research 2017, 6, 1828. [Google Scholar] [CrossRef] [PubMed]
- Lapucci, C.; Schiavi, S.; Signori, A.; Sbragia, E.; Bommarito, G.; Cellerino, M.; Uccelli, A.; Inglese, M.; Roccatagliata, L.; Pardini, M. The role of disconnection in explaining disability in multiple sclerosis. Eur. Radiol. Exp. 2022, 6, 23. [Google Scholar] [CrossRef]
- McFarland, H.; Barkhof, F.; Antel, J.; Miller, D. The role of MRI as a surrogate outcome measure in multiple sclerosis. Mult. Scler. J. 2002, 8 (Suppl. 1), 40–51. [Google Scholar] [CrossRef] [PubMed]
- Boneschi, F.M.; Rovaris, M.; Comi, G.; Filippi, M. The use of magnetic resonance imaging in multiple sclerosis: Lessons learned from clinical trials. Mult. Scler. J. 2004, 10, 341–347. [Google Scholar] [CrossRef] [PubMed]
- Valizadeh, A.; Moassefi, M.; Elham Barati, E.; Ali Sahraian, M.; Aghajani, F.; Fattahi, M.R. Correlation between the clinical disability and T1 hypointense lesions’ volume in cerebral magnetic resonance imaging of multiple sclerosis patients: A systematic review and meta-analysis. CNS Neurosci. Ther. 2021, 27, 1268–1280. [Google Scholar] [CrossRef]
- Yperman, J.; Popescu, V.; Van Wijmeersch, B.; Becker, T.; Peeters, L.M. Motor evoked potentials for multiple sclerosis, a multiyear follow-up dataset. Sci. Data 2022, 9, 207. [Google Scholar] [CrossRef] [PubMed]
- Rossini, P.M.; Burke, D.; Chen, R.; Cohen, L.G.; Daskalakis, Z.; Di Iorio, R.; Di Lazzaro, V.; Ferreri, F.; Fitzgerald, P.B.; George, M.S.; et al. Non-invasive electrical and magnetic stimulation of the brain, spinal cord, roots and peripheral nerves: Basic principles and procedures for routine clinical and research application. An updated report from an I.F.C.N. Committee. Clin. Neurophysiol. 2015, 126, 1071–1107. [Google Scholar] [CrossRef]
- Pawlitzki, M.; Neumann, J.; Kaufmann, J.; Heidel, J.; Stadler, E.; Sweeney-Reed, C.; Sailer, M.; Schreiber, S. Loss of corticospinal tract integrity in early MS disease stages. Neurol. Neuroimmunol. Neuroinflamm. 2017, 4, e399. [Google Scholar] [CrossRef]
- Kerbrat, A.; Gros, C.; Badji, A.; Bannier, E.; Galassi, F.; Combès, B.; Chouteau, R.; Labauge, P.; Ayrignac, X.; Carra-Dalliere, C.; et al. Multiple sclerosis lesions in motor tracts from brain to cervical cord: Spatial distribution and correlation with disability. Brain 2020, 143, 2089–2105. [Google Scholar] [CrossRef] [PubMed]
- Victoria Fernández, V. The Use of Motor-Evoked Potentials in Clinical Trials in Multiple Sclerosis. J. Clin. Neurophysiol. 2021, 38, 166–170. [Google Scholar] [CrossRef] [PubMed]
- Collins, C.D.; Ivry, B.; Bowen, J.D.; Cheng, E.M.; Dobson, R.; Goodin, D.S.; Lechner-Scott, J.; Kappos, L.; Galea, I. A comparative analysis of Patient-Reported Expanded Disability Status Scale tools. Mult. Scler. J. 2016, 22, 1349–1358. [Google Scholar] [CrossRef] [PubMed]
- Šoda, J.; Pavelin, S.; Vujović, I.; Rogić Vidaković, M. Assessment of Motor Evoked Potentials in Multiple Sclerosis. Sensors 2023, 23, 497. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).