A Lurking Threat of Community-Acquired Acinetobacter Meningitis—A Rare Case Report from Punjab, India
Abstract
:1. Introduction
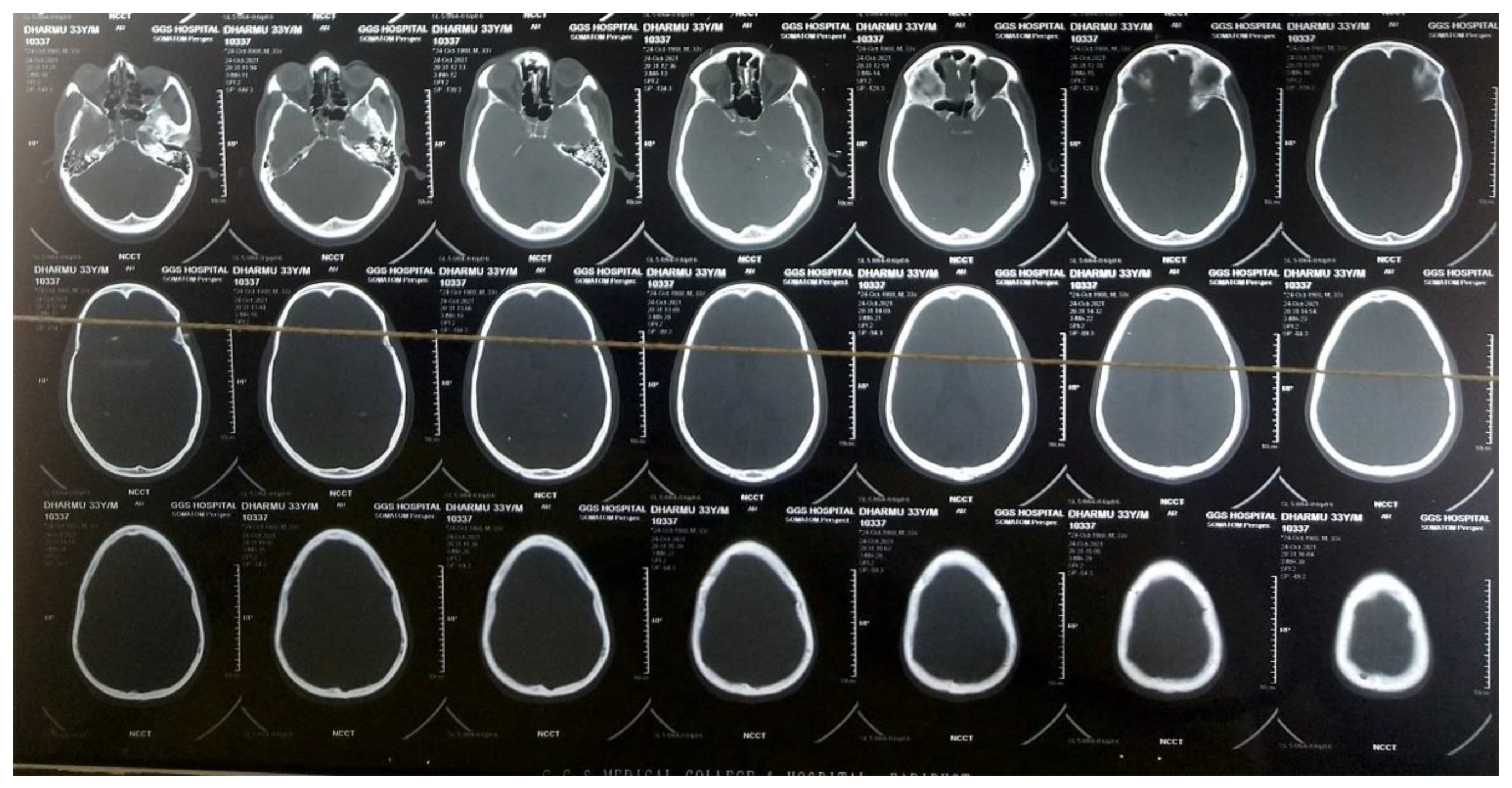
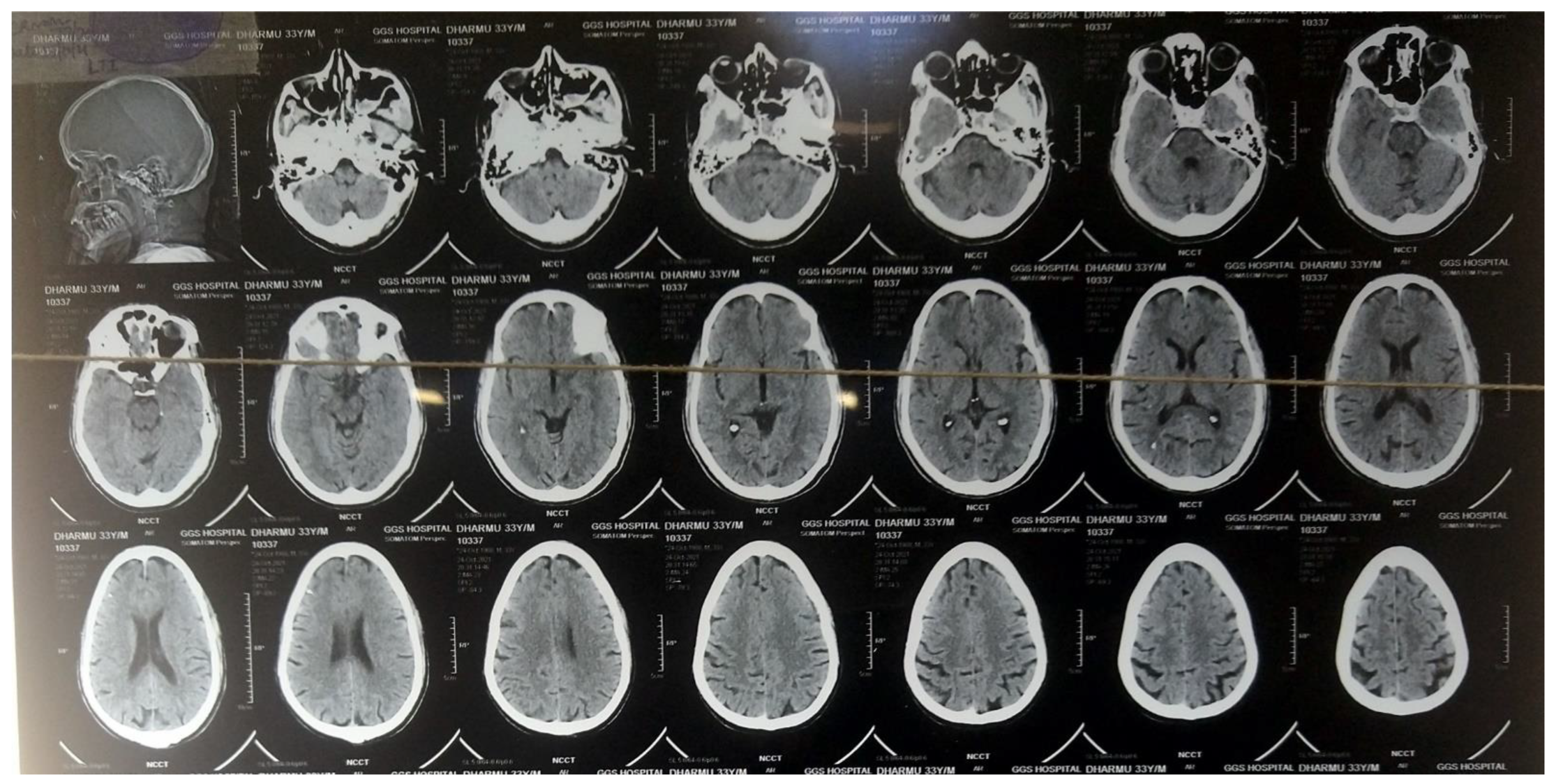
2. Case Presentation
3. Investigations
4. Treatment
5. Outcome and Follow-Up
6. Discussion
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Ethics Statement
References
- Falagas, M.E.; Karveli, E.A.; Kelesidis, I.; Kelesidis, T. Community-acquired Acinetobacter infections. Eur. J. Clin. Microbiol. Infect. Dis. Off. Publ. Eur. Soc. Clin. Microbiol. 2007, 26, 857–868. [Google Scholar] [CrossRef]
- Ramirez, M.S.; Bonomo, R.A.; Tolmasky, M.E. Carbapenemases: Transforming Acinetobacter baumannii into a yet more dangerous menace. Biomolecules 2020, 10, 720. [Google Scholar] [CrossRef] [PubMed]
- Mulani, M.S.; Kamble, E.E.; Kumkar, S.N.; Tawre, M.S.; Pardesi, K.R. Emerging strategies to combat ESKAPE pathogens in the era of antimicrobial resistance: A review. Front. Microbiol. 2019, 10, 539. [Google Scholar] [CrossRef] [PubMed]
- Nau, R.; Sörgel, F.; Eiffert, H. Penetration of drugs through the blood-cerebrospinal fluid/blood-brain barrier for treatment of central nervous system infections. Clin. Microbiol. Rev. 2010, 23, 858–883. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing; 29th Informational Supplement. CLSI Document M100-S29; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2020. [Google Scholar]
- Srinivasan, R.; Karaoz, U.; Volegova, M.; MacKichan, J.; Kato-Maeda, M.; Miller, S.; Nadarajan, R.; Brodie, E.L.; Lynch, S.V. Use of 16S rRNA gene for identification of a broad range of clinically relevant bacterial pathogens. PLoS ONE 2015, 10, e0117617. [Google Scholar] [CrossRef] [PubMed]
- Van de Beek, D.; Cabellos, C.; Dzupova, O.; Esposito, S.; Klein, M.; Kloek, A.T.; Leib, S.L.; Mourvillier, B.; Ostergaard, C.; Pagliano, P.; et al. ESCMID guideline: Diagnosis and treatment of acute bacterial meningitis. Clin. Microbiol. Infect. Off. Publ. Eur. Soc. Clin. Microbiol. Infect. Dis. 2016, 22 (Suppl. 3), S37–S62. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lu, C.-H.; Huang, C.-R.; Chang, W.-N.; Chang, C.-J.; Cheng, B.-C.; Lee, P.-Y.; Lin, M.-W.; Chang, H.-W. Community-acquired bacterial meningitis in adults: The epidemiology, timing of appropriate antimicrobial therapy, and prognostic factors. Clin. Neurol. Neurosurg. 2002, 104, 352–358. [Google Scholar] [CrossRef]
- Leung, W.-S.; Chu, C.-M.; Tsang, K.-Y.; Lo, F.-H.; Lo, K.-F.; Ho, P.-L. Fulminant community-acquired Acinetobacter baumannii pneumonia as a distinct clinical syndrome. Chest 2006, 129, 102–109. [Google Scholar] [CrossRef] [PubMed]
- Chang, W.N.; Lu, C.H.; Huang, C.R.; Chuang, Y.C. Community-acquired Acinetobacter meningitis in adults. Infection 2000, 28, 395–397. [Google Scholar] [CrossRef] [PubMed]
- Lowman, W.; Kalk, T.; Menezes, C.N.; John, M.A.; Grobusch, M.P. A case of community-acquired Acinetobacter baumannii meningitis—Has the threat moved beyond the hospital? J. Med. Microbiol. 2008, 57, 676–678. [Google Scholar] [CrossRef] [PubMed]

| Antimicrobials | Interpretation |
|---|---|
| Gentamycin | R |
| Cephalaxin | R |
| Amikacin | R |
| Ciprofloxacin | R |
| Netilmycin | R |
| Cefotaxime | R |
| Ceftazidime + Sulbactam | R |
| Ofloxacin | IM |
| Cefoperazone + Sulbactam | S |
| Augmantin | R |
| Cotrimoxazole | R |
| Meropenem | S |
| Pipercillin/Tazobactum | S |
| Gatifloxacin | S |
| Cefuroxime | R |
| Cefixime | R |
| Cefepime | R |
| Cefprozil | R |
| Ceftrixone + Sulbactam | S |
| Imipenem | IM |
| Colistin | S |
| Ertapenem | R |
| Elores | S |
| Levofloxacin | S |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jindal, N.; Jain, S.; Bhowmick, A.; Bhargava, V. A Lurking Threat of Community-Acquired Acinetobacter Meningitis—A Rare Case Report from Punjab, India. Medicines 2022, 9, 27. https://doi.org/10.3390/medicines9040027
Jindal N, Jain S, Bhowmick A, Bhargava V. A Lurking Threat of Community-Acquired Acinetobacter Meningitis—A Rare Case Report from Punjab, India. Medicines. 2022; 9(4):27. https://doi.org/10.3390/medicines9040027
Chicago/Turabian StyleJindal, Navodhya, Sonia Jain, Arghya Bhowmick, and Vyom Bhargava. 2022. "A Lurking Threat of Community-Acquired Acinetobacter Meningitis—A Rare Case Report from Punjab, India" Medicines 9, no. 4: 27. https://doi.org/10.3390/medicines9040027
APA StyleJindal, N., Jain, S., Bhowmick, A., & Bhargava, V. (2022). A Lurking Threat of Community-Acquired Acinetobacter Meningitis—A Rare Case Report from Punjab, India. Medicines, 9(4), 27. https://doi.org/10.3390/medicines9040027





