Post-Traumatic-Related Technical Errors in Orthopantomographic Imaging
Abstract
1. Introduction
2. Materials and Methods
Selection and Description of Participants
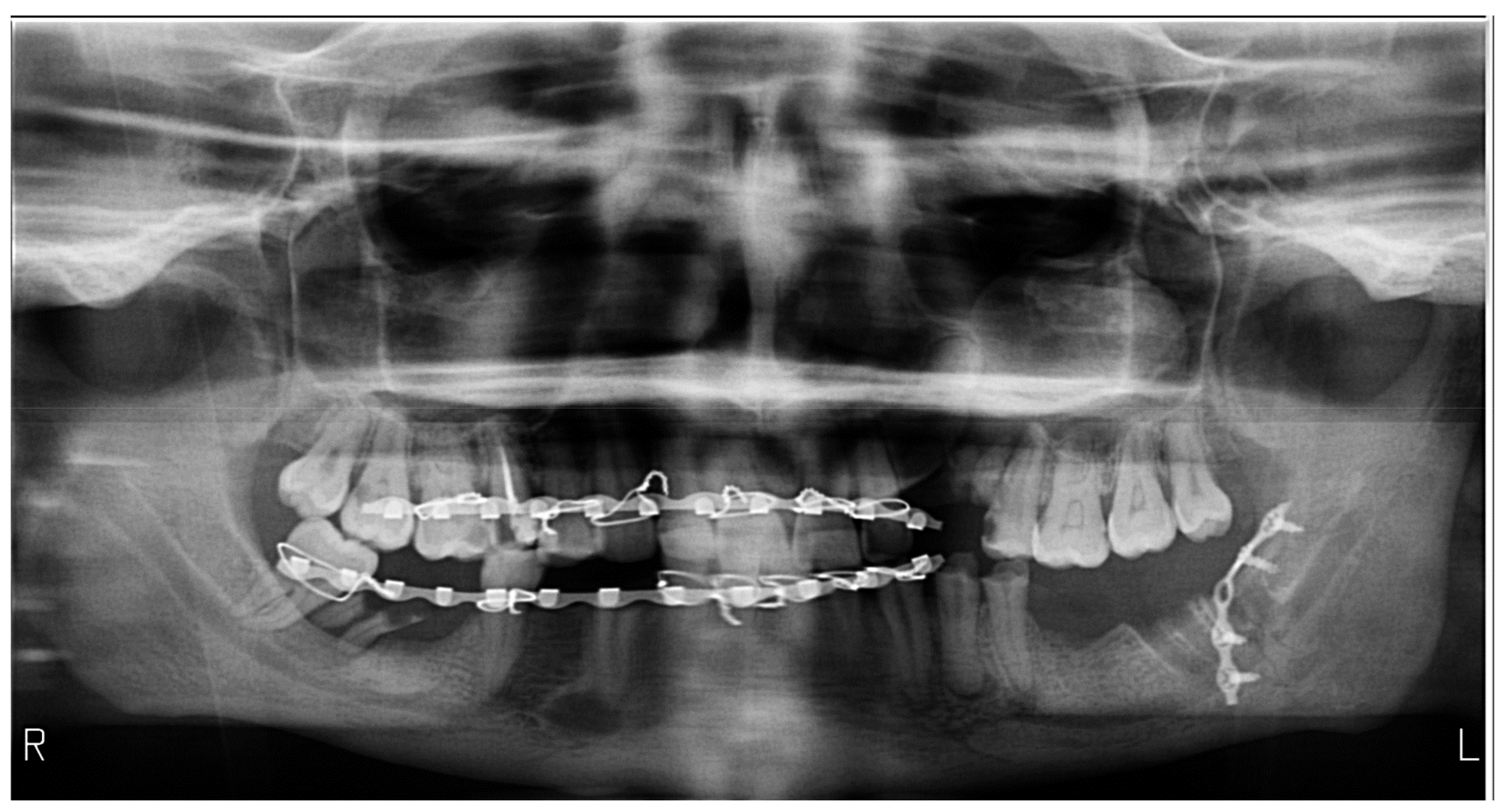
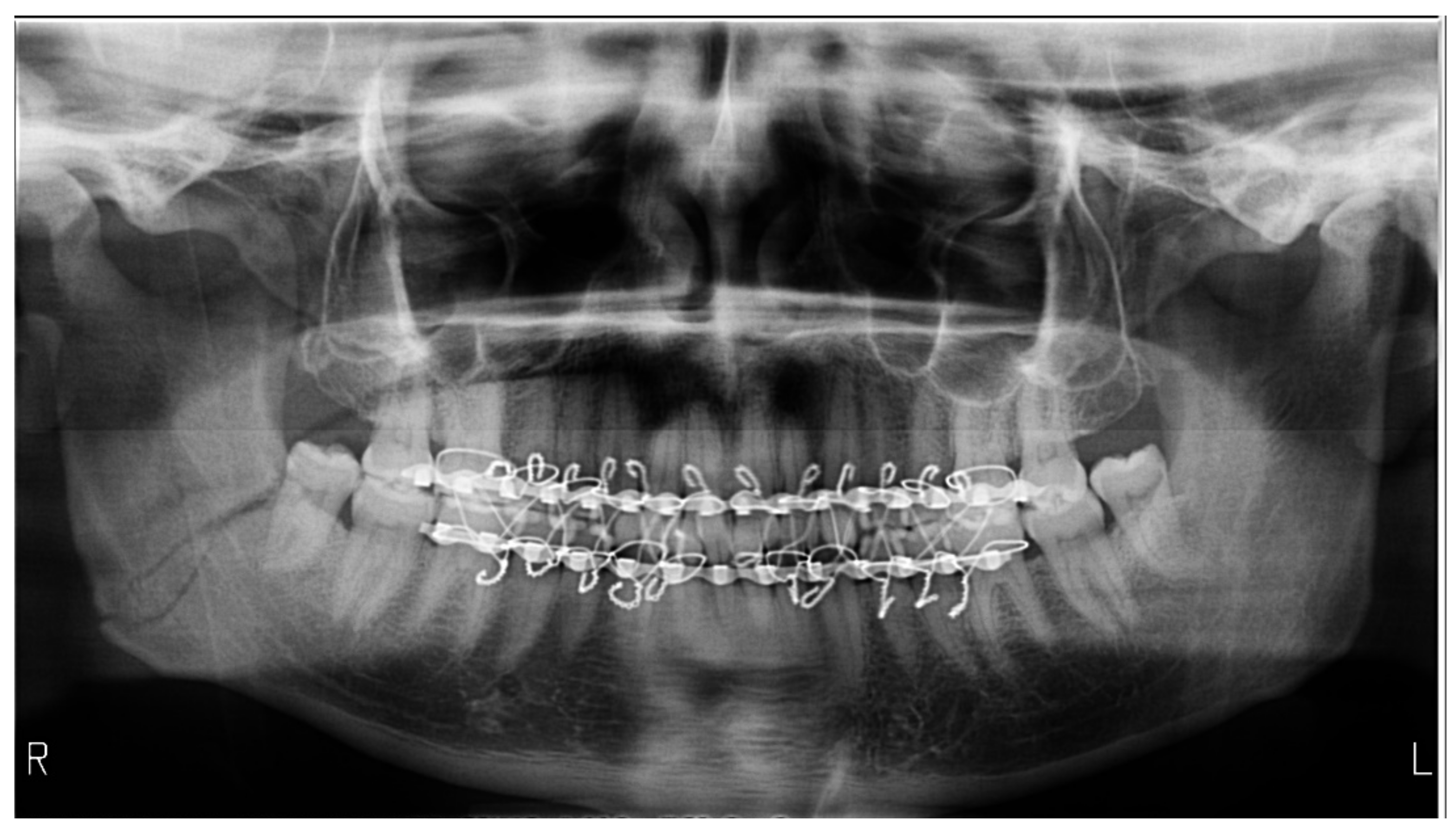
3. Results
4. Discussion
4.1. Strengths and Limitations
4.2. Implications for Practice and Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Khator, A.M.; Motwani, M.B.; Choudhary, A.B. A Study for Determination of Various Positioning Errors in Digital Panoramic Radiography for Evaluation of Diagnostic Image Quality. Indian J. Dent. Res. 2017, 28, 666–670. [Google Scholar] [CrossRef] [PubMed]
- Rondon, R.H.N.; Pereira, Y.C.L.; do Nascimento, G.C. Common Positioning Errors in Panoramic Radiography: A Review. Imaging Sci. Dent. 2014, 44, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Scott, A.M.; Reed, W.M. Panoramic Radiography and Patients with Disability: A New Simple Breathing Technique to Reduce Common Airspace Error. J. Med. Radiat. Sci. 2022, 69, 261–266. [Google Scholar] [CrossRef] [PubMed]
- Wenzel, A.; Matzen, L.H.; Spin-Neto, R.; Schropp, L. Effect of Computer-Assisted-Learning and Simulation Clinics on Dental Students’ Cognitive and Performance Skills: Panoramic Image Errors Related to Patient’s Head Position. Dentomaxillofac. Radiol. 2020, 49, 20200154. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Badal, A. A Review of Doses for Dental Imaging in 2010–2020 and Development of a Web Dose Calculator. Radiol. Res. Pract. 2021, 2021, 6924314. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.-W. Assessment of Panoramic Radiography as a National Oral Examination Tool: Review of the Literature. Imaging Sci. Dent. 2011, 41, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Masthoff, M.; Gerwing, M.; Masthoff, M.; Timme, M.; Kleinheinz, J.; Berninger, M.; Heindel, W.; Wildgruber, M.; Schülke, C. Dental Imaging—A Basic Guide for the Radiologist. Rofo 2019, 191, 192–198. [Google Scholar] [CrossRef] [PubMed]
- Barrett, D.M.; Halbert, T.W.; Fiorillo, C.E.; Park, S.S.; Christophel, J.J. Cost-Based Decision Analysis of Postreduction Imaging in the Management of Mandibular Fractures. JAMA Facial Plast. Surg. 2015, 17, 28–32. [Google Scholar] [CrossRef] [PubMed]
- Tandogdu, E.; Ayali, A.; Caymaz, M.G. Comparison of the Efficacy of the Panoramic and Cone Beam Computed Tomography Imaging Methods in the Surgical Planning of the Maxillary All-On-4, M-4, and V-4. Biomed. Res. Int. 2022, 2022, 1553340. [Google Scholar] [CrossRef] [PubMed]
- Suskin, J.A.; Rao, V.; Crozier, J.W.; Yi, T.; Benz, E.; Woo, A.S. Re-Evaluating the Need for Orthopantomography in the Management of Mandibular Trauma: Is Computed Tomography Enough? Emerg. Radiol. 2022, 29, 663–670. [Google Scholar] [CrossRef] [PubMed]
- Riecke, B.; Friedrich, R.E.; Schulze, D.; Loos, C.; Blessmann, M.; Heiland, M.; Wikner, J. Impact of Malpositioning on Panoramic Radiography in Implant Dentistry. Clin. Oral Investig. 2015, 19, 781–790. [Google Scholar] [CrossRef] [PubMed]
- Ekströmer, K.; Hjalmarsson, L. Positioning Errors in Panoramic Images in General Dentistry in Sörmland County, Sweden. Swed. Dent. J. 2014, 38, 31–38. [Google Scholar] [PubMed]
- Kaviani, F.; Johari, M.; Esmaeili, F. Evaluation of Common Errors of Panoramic Radiographs in Tabriz Faculty of Dentistry. J. Dent. Res. Dent. Clin. Dent. Prospects 2008, 2, 99–101. [Google Scholar] [CrossRef] [PubMed]
- Dhillon, M.; Raju, S.M.; Verma, S.; Tomar, D.; Mohan, R.S.; Lakhanpal, M.; Krishnamoorthy, B. Positioning Errors and Quality Assessment in Panoramic Radiography. Imaging Sci. Dent. 2012, 42, 207–212. [Google Scholar] [CrossRef] [PubMed]
- Glass, B.J.; Seals, R.R.; Williams, E.O. Common Errors in Panoramic Radiography of Edentulous Patients. J. Prosthodont. 1994, 3, 68–73. [Google Scholar] [CrossRef] [PubMed]
- Loughlin, A.; Drage, N.; Greenall, C.; Farnell, D.J.J. An Investigation in to the Impact of Acquisition Location on Error Type and Rate When Undertaking Panoramic Radiography. Radiography 2017, 23, 305–309. [Google Scholar] [CrossRef] [PubMed]
- Cordesmeyer, R.; Engelke, W.; Sömmer, C.; Kauffmann, P. Can Tongue Shadow in Panoramic Radiographs Be Avoided by Using the Tongue Repositioning Maneuver? Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2016, 121, e175–e180. [Google Scholar] [CrossRef] [PubMed]
- Gross, H.; Nilsson, M.; Hellén-Halme, K. Detectability of Normal Anatomy in Digital Panoramic Radiographs. Swed. Dent. J. 2014, 38, 179–185. [Google Scholar] [PubMed]
- Bissoon, A.K.; Whaites, E.; Moze, K.; Naidu, R. Evaluation of Common Operator Errors in Panoramic Radiography in Trinidad and Tobago: A Comparison of Formally vs Informally Trained Operators. West Indian Med. J. 2012, 61, 733–738. [Google Scholar] [PubMed]



| Number of Errors on a Single OPG | Total Errors (n) | Relative Frequency (%) | Relative Frequency (CI95%) |
|---|---|---|---|
| 2 | 3 | 6.6 | [01.85–21.32] |
| 3 | 12 | 40 | [24.59–57.68] |
| 4 | 10 | 33.33 | [19.23–5122] |
| 5 | 4 | 13.33 | [05.31–29.68] |
| 6 | 1 | 03.33 | [00.59–16.67] |
| Diagnostic | Total Errors (n) | Error Frequency on Images (%) | Relative Error Frequency (%) | Frequency on Images (CI95%) |
|---|---|---|---|---|
| Exposure errors | 24 | 80 | 53.33 | [62.69–90.49] |
| Palatoglossal air | 20 | 66.66 | 52.63 | [48.78–80.77] |
| Head in flexion | 11 | 36.66 | 39.28 | [21.87–54.49] |
| Head in extension | 8 | 26.66 | 44.44 | [14.18–44.45] |
| Lateral head inclination | 18 | 60 | 45 | [42.32–75.41] |
| Lateral head deviation | 18 | 60 | 52.94 | [42.32–75.41] |
| Lateral head rotation | 11 | 36.66 | 73.33 | [21.87–54.49] |
| Absence of bite-block | 28 | 93.33 | 51.85 | [78.68–98.15] |
| Inappropriate bite | 2 | 6.66 | 66.66 | [01.85–21.32] |
| Positioning outside the focal plane | 21 | 70 | 46.66 | [52.12–83.34] |
| Radiographs with bimaxillary immobilization errors | 23 | 76.66 | 62.16 | [59.07–88.21] * |
| Presence of Bite-Block | Total Errors (n) % | Relative Frequency (CI95%) | Absence of Bite-Block (n) % | Relative Frequency (CI95%) |
|---|---|---|---|---|
| Lateral rotation | (3) 37.50 | [13.68–69.43] | (10) 45.45 | [26.92–65.34] |
| Lateral deviation | (2) 25.00 | [07.15–59.07] | (19) 86.36 | [66.67–95.25] * |
| Total | 8 | 22 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Almășan, O.; Roman, R.A.; Hedeşiu, M.; Bran, S.; Roman, S.; Petric, B.; Dinu, C. Post-Traumatic-Related Technical Errors in Orthopantomographic Imaging. Medicines 2022, 9, 63. https://doi.org/10.3390/medicines9120063
Almășan O, Roman RA, Hedeşiu M, Bran S, Roman S, Petric B, Dinu C. Post-Traumatic-Related Technical Errors in Orthopantomographic Imaging. Medicines. 2022; 9(12):63. https://doi.org/10.3390/medicines9120063
Chicago/Turabian StyleAlmășan, Oana, Raluca Ancuța Roman, Mihaela Hedeşiu, Simion Bran, Sara Roman, Bianca Petric, and Cristian Dinu. 2022. "Post-Traumatic-Related Technical Errors in Orthopantomographic Imaging" Medicines 9, no. 12: 63. https://doi.org/10.3390/medicines9120063
APA StyleAlmășan, O., Roman, R. A., Hedeşiu, M., Bran, S., Roman, S., Petric, B., & Dinu, C. (2022). Post-Traumatic-Related Technical Errors in Orthopantomographic Imaging. Medicines, 9(12), 63. https://doi.org/10.3390/medicines9120063







