Seasonal Changes in Continuous Sedentary Behavior in Community—Dwelling Japanese Adults: A Pilot Study
Abstract
1. Introduction
2. Subjects and Methods
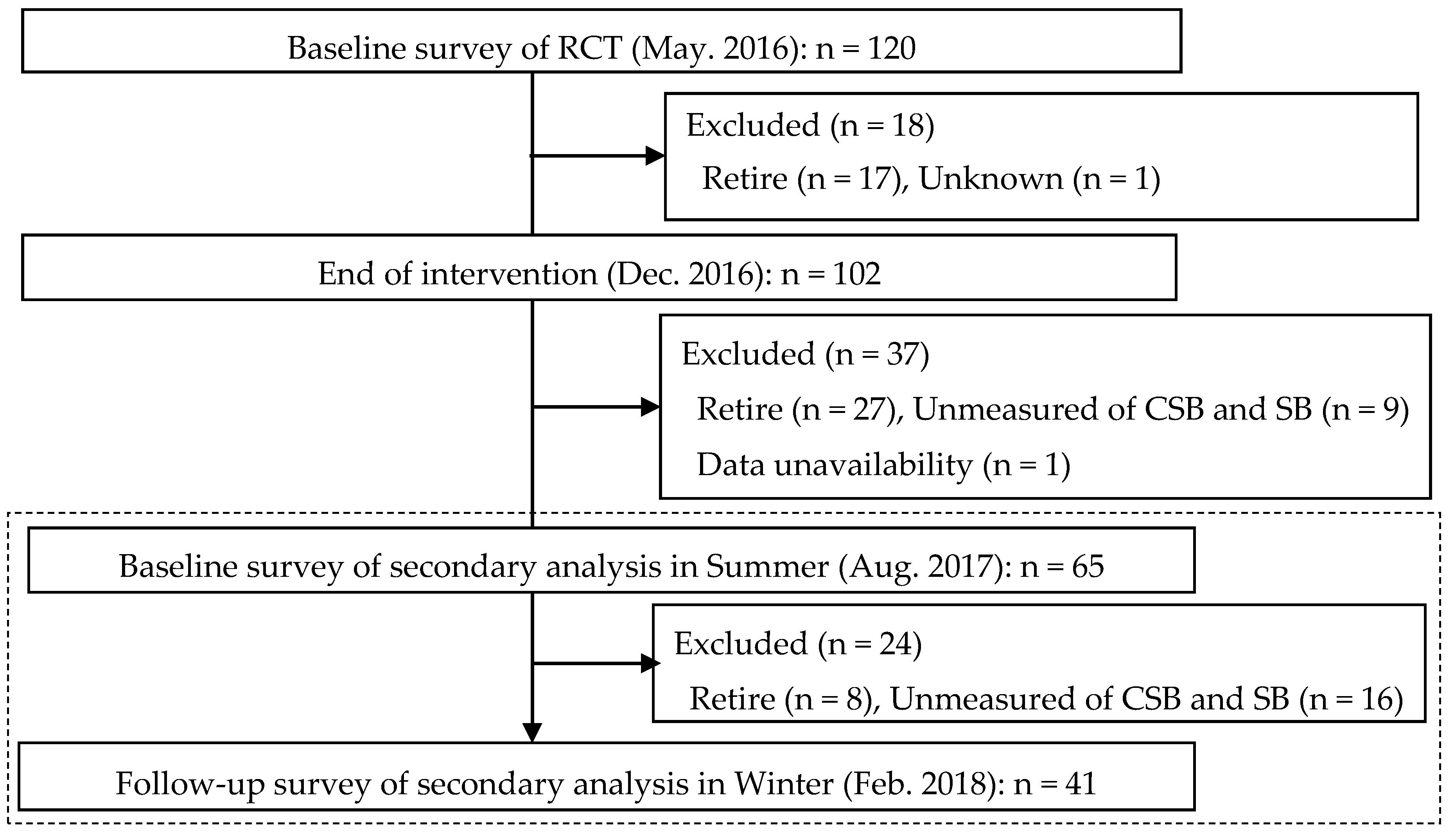
2.1. Subjects
2.2. Clinical Parameters
2.3. Tri-Accelerometer Measurements
2.4. Metrological Parameters
2.5. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- Tremblay, M.S.; Aubert, S.; Barnes, J.D.; Saunders, T.J.; Carson, V.; Latimer-Cheung, A.E.; Chastin, S.F.M.; Altenburg, T.M.; Chinapaw, M.J.M. Sedentary behavior research network (SBRN)-Terminology consensus project process and outcome. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 75. [Google Scholar] [CrossRef]
- Figueiró, T.H.; Arins, G.C.B.; Santos, C.E.S.D.; Cembranel, F.; Medeiros, P.A.; d’Orsi, E.; Rech, C.R. Association of objectively measured sedentary behavior and physical activity with cardiometabolic risk markers in older adults. PLoS ONE 2019, 14, e0210861. [Google Scholar] [CrossRef] [PubMed]
- Diaz, K.M.; Howard, V.J.; Hutto, B.; Colabianchi, N.; Vena, J.E.; Safford, M.M.; Blair, S.N.; Hooker, S.P. Patterns of sedentary behavior and mortality in U.S. Middle-aged and older adults: A national cohort study. Ann. Intern. Med. 2017, 167, 465–475. [Google Scholar] [CrossRef] [PubMed]
- Biswas, A.; Oh, P.I.; Faulkner, G.E.; Bajaj, R.R.; Silver, M.A.; Mitchell, M.S.; Alter, D.A. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: A systematic review and meta-analysis. Ann. Intern. Med. 2015, 162, 123–132. [Google Scholar] [CrossRef] [PubMed]
- Hishii, S.; Miyatake, N.; Nishi, H.; Katayama, A.; Ujike, K.; Koumoto, K.; Hashimoto, H. Relationship between sedentary behavior and health-related quality of life in patients on chronic hemodialysis. Acta. Med. Okayama 2018, 72, 395–400. [Google Scholar] [PubMed]
- Hishii, S.; Miyatake, N.; Nishi, H.; Katayama, A.; Ujike, K.; Koumoto, K.; Suzuki, H.; Hashimoto, H. Relationship between sedentary behavior and all-cause mortality in Japanese chronic hemodialysis patients: A prospective cohort study. Acta. Med. Okayama 2019, 73, 419–425. [Google Scholar]
- Dunstan, D.W.; Howard, B.; Healy, G.N.; Owen, N. Too much sitting-a health hazard. Diabetes Res. Clin. Pract. 2012, 97, 368–376. [Google Scholar] [CrossRef]
- Ng, S.W.; Popkin, B.M. Time use and physical activity: A shift away from movement across the globe. Obes. Rev. 2012, 13, 659–680. [Google Scholar] [CrossRef]
- Bauman, A.; Ainsworth, B.E.; Sallis, J.F.; Hagstromer, M.; Craig, C.L.; Bull, F.C.; Pratt, M.; Venugopal, K.; Chau, J.; Sjostrom, M.; et al. The descriptive epidemiology of sitting. A 20-country comparison using the international physical activity questionnaire (IPAQ). Am. J. Prev. Med. 2011, 41, 228–235. [Google Scholar] [CrossRef]
- Healy, G.N.; Matthews, C.E.; Dunstan, D.W.; Winkler, E.A.; Owen, N. Sedentary time and cardio-metabolic biomarkers in US Adults: NHANES 2003–06. Eur. Heart J. 2011, 32, 590–597. [Google Scholar] [CrossRef]
- Peddie, M.C.; Bone, J.L.; Rehrer, N.J.; Skeaff, C.M.; Gray, A.R.; Perry, T.L. Breaking prolonged sitting reduces postprandial glycemia in healthy, normal-weight adults: A randomized crossover trial. Am. J. Clin. Nutr. 2013, 98, 358–366. [Google Scholar] [CrossRef] [PubMed]
- Honda, T.; Chen, S.; Yonemoto, K.; Kishimoto, H.; Chen, T.; Narazaki, K.; Haeuchi, Y.; Kumagai, S. Sedentary bout durations and metabolic symdrome among working adults: A prospective cohort study. BMC Publ. Health 2016, 16, 888. [Google Scholar] [CrossRef] [PubMed]
- Owari, Y.; Miyatake, N. Long-term relationship between psychological distress and continuous sedentary behavior in healthy older adults: A three panel study. Medicina 2019, 55, 324. [Google Scholar] [CrossRef]
- Yamamoto, Y.; Suzuki, H.; Owari, Y.; Miyatake, N. Relationships between physical activity, sleeping time, and psychological distress in community-dwelling elderly Japanese. Medicina 2019, 55, 318. [Google Scholar] [CrossRef] [PubMed]
- Van der Berg, J.D.; Bosma, H.; Caserotti, P.; Eiriksdottir, G.; Arnardottir, N.Y.; Martin, K.R.; Brychta, R.J.; Chen, K.Y.; Sveinsson, T.; Johannsson, E.; et al. Midlife determinants associated with sedentary behavior in old age. Med. Sci. Sports Exerc. 2014, 46, 1359–1365. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.; Kishimoto, H.; Honda, T.; Hata, J.; Yoshida, D.; Mukai, N.; Shibata, M.; Ninomiya, T.; Kumagai, S. Patterns and levels of sedentary behavior and physical activity in a general Japanese population: The hisayama study. J. Epidemiol. 2018, 28, 260–265. [Google Scholar] [CrossRef]
- Chen, T.; Narazaki, K.; Honda, T.; Chen, S.; Haeuchi, Y.; Nofuji, Y.Y.; Matsuo, E.; Kumagai, S. Tri-axial accelerometer-determined daily physical activity and sedentary behavior of suburban community-Dwelling older Japanese adults. J. Sports Sci. Med. 2015, 14, 507–514. [Google Scholar]
- Van Nassau, F.; Mackenbach, J.D.; Compermolle, S.; de Bourdeaudhuij, I.; Lakerveld, J.; van der Ploeg, H.P. Individual and environmental correlates of objectively measured sedentary time in Dutch and Belgian adults. PLoS ONE 2017, 12, e0186538. [Google Scholar] [CrossRef]
- Kurita, S.; Shibata, A.; Ishii, K.; Koohsari, M.J.; Owen, N.; Oka, K. Patterns of objectively assessed sedentary time and physical activity among Japanese workers: A cross-sectional observational study. BMJ Open 2019, 9, e021690. [Google Scholar] [CrossRef]
- Schrempft, S.; Jackowska, M.; Hamer, M.; Steptoe, A. Associations between social isolation, loneliness, and objective physical activity in older men and women. BMC Publ. Health 2019, 19, 74. [Google Scholar] [CrossRef]
- Sartini, C.; Morris, R.W.; Whincup, P.H.; Wannamethee, S.G.; Ash, S.; Lennon, L.; Jefferis, B.J. Association of maximum temperature with sedentary time in older British men. J. Phys. Act. Health 2017, 14, 265–269. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Schepps, M.A.; Shiroma, E.J.; Kamada, M.; Harris, T.B.; Lee, I.M. Day length is associated with physical activity and sedentary behavior among older women. Sci. Rep. 2018, 8, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Arnardottir, N.Y.; Oskarsdottir, N.D.; Brychta, R.J.; Koster, A.; van Domelen, D.R.; Caserotti, P.; Eiriksdottir, G.; Sverrisdottir, J.E.; Johannsson, E.; Launer, L.J.; et al. Comparison of summer and winter objectively measured physical activity and sedentary behavior in older adults: Age, gene/environment susceptibility reykjavik study. Int. J. Environ. Res. Public Health. 2017, 14, 1268. [Google Scholar] [CrossRef] [PubMed]
- O’Connell, S.E.; Griffiths, P.L.; Clemes, S.A. Seasonal variation in physical activity, sedentary behavior and sleep in a sample of UK adults. Ann. Hum. Biol. 2014, 41, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, C.; Reilly, J.J.; Tanaka, M.; Tanaka, S. Seasonal changes in objectively measured sedentary behavior and physical activity in Japanese primary school children. BMC Publ. Health 2016, 16, 969. [Google Scholar] [CrossRef]
- Bando, M.; Miyatake, N.; Kataoka, H.; Kinoshita, H.; Tanaka, N.; Suzuki, H.; Katayama, A. Relationship between air temperature parameters and the number of deaths stratified by cause in gifu prefecture, Japan. Healthcare 2020, 8, 35. [Google Scholar] [CrossRef]
- Sakamoto, M.; Matsutani, D.; Minato, S.; Tsujimoto, Y.; Kayama, Y.; Takeda, N.; Ichikawa, S.; Horiuchi, R.; Utsunomiya, K.; Nishikawa, M.; et al. Seasonal variation in the achievement of guideline targets for HbA1c, blood pressure, and cholesterol among patients with type 2 diabetes: A nationwide population-based study (ABC Study: JDDM49). Diabetes Care 2019, 42, 816–823. [Google Scholar] [CrossRef]
- Aoyagi, Y.; Shephard, R.J. Habitual physical activity and health in the elderly: The nakanojo study. Geriatr. Gerontol. Lnt. 2010, 10, S236–S243. [Google Scholar] [CrossRef]
- Tucker, P.; Gilliland, J. The effect of season and weather on physical activity. A Public Health 2007, 121, 909–922. [Google Scholar] [CrossRef]
- Takashima, N.; Katayama, A.; Mochimasu, K.D.; Hishii, S.; Suzuki, H.; Miyatake, N. A pilot study of the relationship between diet and mental health in community dwelling Japanese women. Medicina 2019, 55, 513. [Google Scholar] [CrossRef]
- Katayama, A.; Miyatake, N.; Uchida, H. A randomized controlled trial of theeffectof exercise program in community dwelling elderly people. Abstract of the 20th of Annual Meeting of Japanese Association of Exercise Epidemiology 50. Available online: http://jaee.umin.jp/doc/meeting_20_presentation.pdf (accessed on 1 February 2020).
- Wang, Z.H.; Yang, Z.P.; Wang, X.J.; Dong, Y.H.; Ma, J. Comparative analysis of the multi-frequency bio-impedance and dual-energy X-ray absorptiometry on body composition in obese subjects. Biomed. Environ. Sci. 2018, 31, 72–75. [Google Scholar] [PubMed]
- Ohkawara, K.; Oshima, Y.; Hikihara, Y.; Ishikawa-Takata, K.; Tabata, I.; Tanaka, S. Real-time estimation of daily physical activity intensity by a triaxial accelerometer and a gravity-removal classification algorithm. Br. J. Nutr. 2011, 105, 1681–1691. [Google Scholar] [CrossRef] [PubMed]
- Oshima, Y.; Kawaguchi, K.; Tanaka, S.; Ohkawara, K.; Hikihara, Y.; Ishikawa-Takata, K.; Tabata, I. Classifying household and locomotive activities using a triaxial accelerometer. Gait Posture. 2010, 31, 370–374. [Google Scholar] [CrossRef] [PubMed]
- Kumagai, S.; Tanaka, S.; Kishimoto, H.; Naito, Y. Measurements of physical activity and sedentary behavior by tri-axial accelerometers and their application to epidemiological studies. Reseach Exerc. Epidemiol. 2015, 17, 90–103. (In Japanese) [Google Scholar]
- Sasaki, H. Assessing sedentary behavior using wearable devices: An overview and future directions. J. Phys. Fitness Sports Med. 2017, 6, 135–143. [Google Scholar] [CrossRef]
- Trost, S.G.; Mclver, K.L.; Pate, R.R. Conducting accelerometer-based activity assessments in field-based research. Med. Sci. Sports Exerc. 2005, 37, S531–S543. [Google Scholar] [CrossRef]
- Aoyama, T.; Miyatake, N.; Seki, A.; Hossaka, K.; Takimoto, H.; Tanaka, S. Does physical activity attenuate the association between birth weight and glycated hemoglobin in nondiabetic Japanese women? J. Dev. Orig. Health Dis. 2019, 18, 1–5. [Google Scholar] [CrossRef]
- Japan Meteorological Agency. Available online: http://www.data.jma.go.jp/obd/stats/etrn/index.php (accessed on 6 May 2020). (In Japanese).
- Suzuki, H. The classification of Japanese climates. Geogr. Rev. Jap. 1962, 35, 205–211. (In Japanese) [Google Scholar] [CrossRef]
- Fishman, E.I.; Steeves, J.A.; Zipunnikov, V.; Koster, A.; Berrigan, D.; Harris, T.A.; Murphy, R. Association between objectively measured physical activity and mortality in NHANES. Med. Sci. Sports Exerc. 2016, 48, 1303–1311. [Google Scholar] [CrossRef]
- Parsons, T.J.; Sartini, C.; Ash, S.; Lennon, L.T.; Wannamethee, S.G.; Lee, I.M.; Whincup, P.H.; Jefferis, B.J. Objectively measured physical activity and kidney function in older men; A cross-sectional population-based study. Age Ageing 2017, 46, 1010–1014. [Google Scholar] [CrossRef]
- Baruth, M.; Sharpe, P.A.; Hutto, B.; Wilcox, S.; Warren, T.Y. Patterns of sedentary behavior in overweight and obese women. Ethn. Dis. 2013, 23, 336–342. [Google Scholar] [PubMed]
- Hamilton, S.L.; Clemes, S.A.; Griffiths, P.L. UK adults exhibit higher step counts in summer compared to winter months. Ann. Hum. Biol. 2008, 35, 154–169. [Google Scholar] [CrossRef] [PubMed]
- Hino, K.; Lee, J.S.; Asami, Y. Associations between seasonal meteorological conditions and the daily step count of adults in Yokohama, Japan: Results of year-round pedometer measurements in a large population. Prev. Med. Rep. 2017, 8, 15–17. [Google Scholar] [CrossRef] [PubMed]
- Sugiwara, H.; Akiyama, H. Social participation of older adults in the workplace and in the community-A comparison of Japan and the United States. Jpn. J. Labour Stud. 2001, 43, 20–30. (In Japanese) [Google Scholar]
| Total (n = 65) | Men (n = 7) | Women (n = 58) | ||||
|---|---|---|---|---|---|---|
| Age (years) | 69 | (50–78) b | 72.1 | ±5.3 a | 69 | (50–78) b |
| Height (cm) | 154.0 | (138.0–175.5) b | 166.6 | ±6.5 a | 153.5 | ±5.1 a |
| Body weight (dry weight) (kg) | 52.4 | (41.2–74.3) b | 58.4 | ±5.4 a | 51.9 | (41.2–74.3) b |
| BMI (kg/m2) | 22.0 | ±2.1 a | 20.6 | (20.1–21.9) b | 22.2 | ±2.2 a |
| Body fat percentage (%) | 26.8 | ±7.3 a | 13.1 | ±3.2 a | 28.4 | ±5.8 a |
| LBM (kg) | 37.4 | (29.0–60.4) b | 50.7 | ±5.0 a | 37.1 | ±2.6 a |
| Daily step counts (steps/day) | 6350.6 | ±2292.7 a | 8207.3 | ±1210.6 a | 6126.6 | ±2296.3 a |
| SB (%) | 54.0 | ±11.5 a | 55.6 | ±13.1 a | 53.8 | ±11.4 a |
| CSB (%) | 20.5 | (4.0–60.9) b | 25.0 | ±13.4 a | 20.3 | (4.0–60.9) b |
| LPA (%) | 40.1 | ±10.5 a | 34.9 | ±9.5 a | 40.8 | ±10.5 a |
| MVPA (%) | 6.1 | (1.3–25.5) b | 8.0 | (5.9–25.5) b | 5.6 | (1.3–17.8) b |
| Follow-Up (+) (n = 41) | Follow-Up (−) (n = 24) | p | p1 | |||
|---|---|---|---|---|---|---|
| Men/Women | 5/36 | 2/22 | ||||
| Age (years) | 68.7 | ±5.6 a | 67.9 | ±6.6 a | 0.577 c | |
| Height (cm) | 154.0 | (148.0–173.0) b | 153.6 | ±7.3 a | 0.475 d | |
| Body weight (dry weight) (kg) | 52.9 | ±5.0 a | 52.1 | (41.2–74.3) b | 0.519 d | |
| BMI (kg/m2) | 21.8 | ±1.9 a | 22.1 | (18.6–28.6) b | 0.624 d | |
| Body fat percentage (%) | 27.1 | (9.5–35.7) b | 28.1 | ±8.1 a | 0.373 d | |
| LBM (kg) | 38.0 | (32.5–53.6) b | 36.6 | (29.0–60.4) b | 0.093 d | |
| Daily step counts (steps/day) | 6491.8 | ±1892.8 a | 6109.4 | ±2880.8 a | 0.521 c | |
| SB (%) | 55.2 | ±11.2 a | 52.0 | ±11.9 a | 0.285 c | 0.397 |
| CSB (%) | 24.7 | ±12.2 a | 19.5 | (5.2–60.9) b | 0.209 d | 0.320 |
| LPA (%) | 39.3 | ±10.3 a | 41.5 | ±10.8 a | 0.408 c | |
| MVPA (%) | 6.1 | (1.3–15.3) b | 6.2 | (1.8–25.5) b | 0.573 d | |
| Baseline (Summer) | Follow-Up (Winter) | Difference | 95%CI | p | |||
|---|---|---|---|---|---|---|---|
| (Winter–Summer) | (Lower, Upper) | ||||||
| Daily step counts (steps/day) | 6491.8 | ±1892.8 a | 5751.5 | ±2768.4 a | −740.4 | (−1530.1, 49.4) | 0.065 c |
| SB (%) | 55.2 | ±11.2 a | 60.2 | ±10.4 a | 5.1 | (1.9, 8.3) | 0.003c |
| CSB (%) | 24.7 | ±12.2 a | 31.4 | ±14.7 a | 6.6 | (2.4, 10.8) | 0.003c |
| LPA (%) | 39.3 | ±10.3 a | 35.2 | ±9.7 a | −4.1 | (−6.9, −1.3) | 0.006c |
| MVPA (%) | 6.1 | (1.3–15.3) b | 4.9 | (0.8–13.9) b | −1.2 | (−2.0, −0.4) | 0.002d |
| ΔSB | ΔCSB | |||||||
|---|---|---|---|---|---|---|---|---|
| r | p | r1 | p1 | r | p | r1 | p1 | |
| Age (years) a | −0.034 | 0.832 | 0.166 | 0.299 | ||||
| Height (cm) a | −0.021 | 0.894 | −0.013 | 0.938 | ||||
| Body weight (dry weight) (kg) a | 0.398 | 0.010 | 0.434 | 0.005 | ||||
| BMI (kg/m2) b | 0.381 | 0.014 | 0.432 | 0.005 | 0.356 | 0.022 | 0.418 | 0.009 |
| Body fat percentage (%) b | 0.278 | 0.078 | 0.261 | 0.099 | ||||
| LBM (kg) a | 0.090 | 0.574 | 0.075 | 0.641 | ||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Uehara, C.; Miyatake, N.; Hishii, S.; Suzuki, H.; Katayama, A. Seasonal Changes in Continuous Sedentary Behavior in Community—Dwelling Japanese Adults: A Pilot Study. Medicines 2020, 7, 48. https://doi.org/10.3390/medicines7090048
Uehara C, Miyatake N, Hishii S, Suzuki H, Katayama A. Seasonal Changes in Continuous Sedentary Behavior in Community—Dwelling Japanese Adults: A Pilot Study. Medicines. 2020; 7(9):48. https://doi.org/10.3390/medicines7090048
Chicago/Turabian StyleUehara, Chiaki, Nobuyuki Miyatake, Shuhei Hishii, Hiromi Suzuki, and Akihiko Katayama. 2020. "Seasonal Changes in Continuous Sedentary Behavior in Community—Dwelling Japanese Adults: A Pilot Study" Medicines 7, no. 9: 48. https://doi.org/10.3390/medicines7090048
APA StyleUehara, C., Miyatake, N., Hishii, S., Suzuki, H., & Katayama, A. (2020). Seasonal Changes in Continuous Sedentary Behavior in Community—Dwelling Japanese Adults: A Pilot Study. Medicines, 7(9), 48. https://doi.org/10.3390/medicines7090048





